Abstract
Background:
Intestinal parasites are a cause of morbidity and mortality throughout the world particularly in developing countries and they are common health problems of children. This study determined the prevalence of intestinal parasites among primary school children, assessed risk factors predisposing to infection and the nutritional status with cognitive function of the pupils.
Materials and Methods:
It was a cross sectional study and 384 pupils from six public primary schools in Ile-Ife were enrolled. Anthropometric measurements were obtained using standard procedures. The intelligence quotients of the pupils were assessed using the Draw-a-person- test. Stool samples were collected and examined. Data was processed using SPSS Inc USA version 17. Statistical analysis was done using frequency, percentages, tables and Pearson’s chi-square was used to determine the association between intestinal parasites, nutritional status and cognitive function.
Results:
The prevalence of intestinal parasites in the study population was 24% with double infection occurring in 3.2%. Ascaris lumbricoides most prevalent 22.1%, Hookworm 3.4%, Hymenolepis nana 0.3%. Intestinal parasites were present in those that use bush and refuse dump for defeacation. The nutritional status of the pupils showed 95.8% normal weight, 3.6% underweight and 0.5% overweight. In terms of cognition, 65.4% mentally deficient, 14.3% mentally dull and 20.3% average.
Conclusion:
Intestinal parasites were prevalent among primary school children and use of bush or refuse dump for defeacation was a risk factor. There was no association between intestinal parasites, nutritional status and cognition.
Keywords: Intestinal parasites, Prevalence, School children, Nutritional status, Cognition, Risk factors
Introduction
Intestinal parasites are a cause of morbidity and mortality throughout the world particularly in developing countries and are common health problems of children especially school - age children between ages 5-10 years Reji et al., (2011). These infections are caused by both protozoal and helminthic organisms and majority are among the neglected tropical diseases. Estimates reveal that at least 400 million school children are chronically infected with Ascaris lumbricoides, Trichuris trichiura and the hook worms Damen et al., (2011). Severity of morbidity is directly linked to worm burden and children are susceptible to infection mostly at an age when they are both growing and learning. They suffer nutritional deficits, cognitive impairment and complications such as intestinal obstruction from ascariasis and iron deficiency anaemia from hookworm infection. (G/hiwot et al., 2014; Alum et al., 2010; Damen et al., 2011). In addition intestinal parasitic infections in school children have been associated with stunting of linear growth, physical weakness, low educational achievement Garba et al., (2010). The effect of intestinal parasites on the nutritional status and cognitive function of children affects their health adversely and unhealthy children cannot attain maximum educational achievement or make significant contributions to their communities. Consequently, this study set out to determine the prevalence of intestinal parasites and their associated risk factors among pupils in Ile-Ife, to assess the nutritional status of the pupils, to examine the cognitive function of the pupils by testing for their intelligence quotient, to document the association between intestinal parasitic infection, nutritional status and cognitive function of pupils in Ile-Ife.
Materials and Methods
Study design - It was a cross-sectional study.
Study area - The study area is Ile-Ife, a town in Osun state, Southwestern Nigeria between latitude 7°28’N and longitude 4°34’E and about 218 km northeast of Lagos.
Study population/duration - Primary school pupils in six public schools that were randomly selected in Ife Central Local Government were used for the study and the duration was for four months (April-July 2013).
Ethical approval – Approval was obtained from the research and ethical committee of OAUTHC, Ile-Ife for the study. Informed consent was also obtained from the parents of the subjects and the school authorities. “The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.”
Selection of subjects- Sixty-four responders were randomly selected from each school based on a sample size of three hundred and eighty-four. With the aid of questionnaire, relevant demographic information was obtained from these children.
Sample collection, processing and storage - Stool samples were collected from the pupils into clean, dry universal containers and transported to the laboratory for analysis. Direct examination of each stool sample was done with both saline and iodine mounts on clean grease-free slides and examined under the microscope first with x10 and then x40 objectives for ova and cysts of parasite. The stool samples that were negative by wet mounts were concentrated using the formol-ether concentration method. The worm burden was also determined by counting the number of eggs per gram of faeces using the Stoll egg counting technique on all positive stool samples.
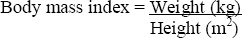
Assessment of Nutritional Status - Body mass index (BMI) was used to assess the nutritional status of these children as this is the most appropriate method for children older than 5 years. BMI was calculated using the following formula:
Weight was measured with a weighing scale to the nearest 0.1kg and height was measured with a stadiometer to the nearest 0.1 cm. The nutritional status of the study participants was determined by comparing the BMI of the pupils with the revised WHO BMI for age charts from Centre for Disease Control (CDC) as reference.
Assessment of Intelligence quotient - The intelligence quotient (IQ) of the children was assessed by the ‘Draw a person test’ according to Ziler. This test has been standardized and validated for use in Nigeria for assessing the intellectual and emotional state of children.
Data Analysis – Data were analyzed using frequency, proportion, percentages, tables and Pearson’s chi-square was used to determine the association between intestinal parasites, nutritional status and cognitive function
Results
Three hundred and eighty four primary school pupils aged 6-12 years participated in the study. The pupils were categorized into age groups 6-7 years (pupils in primaries 1 and 2); 8-9 years (pupils in primaries 3 and 4); 10-12 years (pupils in the exit classes, primaries 5 and 6). Table 1 shows the characteristics of the study population (age, sex, religion and family social class). There were no differences in the sex distribution of participants as 49.5% were males and 50.5% were females.
Table 1.
Characteristics of the Study Participants
| Variable | Frequency | Percent | |
|---|---|---|---|
| Age group* | 6 - 7 yrs | 80 | 20.8 |
| 8 - 9 yrs | 94 | 24.5 | |
| 10 - 12 yrs | 210 | 54.7 | |
| Sex | Male | 190 | 49.5 |
| Female | 194 | 50.5 | |
| Religion | Christianit | 232 | 60.4 |
| Islam | 151 | 39.3 | |
| No information | 1 | 0.3 | |
| Family social class | Upper class | 4 | 1.0 |
| Middle class | 47 | 12.2 | |
| Lower class | 333 | 86.7 | |
The overall prevalence of intestinal parasites in the study participants was 24% ranging from 15.6% to 31.3%.
Ascaris lumbricoides was the most prevalent intestinal parasite (22.1%) followed by hookworm (3.4%) and Hymenolepsis nana was (0.3%). Co-infection of Ascaris lumbricoides and hookworm had a prevalence of 1.6% among the study participants while Ascaris lumbricoides and Hymenolepsis nana co-infection had a rate of 0.3%. This is shown in Table 2.
Table 2.
Prevalence of Intestinal Parasites by Type in the Study Participants
| Variable | N | Prevalence % |
|---|---|---|
| Prevalence by parasite | ||
| Ascaris lumbricoides | 85 | 22.1 |
| Hookworm | 13 | 3.4 |
| Hymenolepis nana | 1 | 0.3 |
| Ascaris-Hookworm co-infection | 6 | 1.6 |
| Ascaris-Hymenolepis co-infection | 1 | 0.3 |
There was no associations between occurrence of intestinal parasites and age groups, sex, parent’s occupation, educational status of the parents and family social class. Table 3 shows the association between intestinal parasites and housing and amenities. There was significant association between toilet facility and intestinal parasites. Those who used bush or refuse dump were more likely to be infected with intestinal parasites (χ2 = 8.783, df = 3, p = 0.032). There were no associations between presence of intestinal parasites and other characteristics such as housing structure and number of co-residents and water source. There were no association between intestinal parasites and risk factors such as history of de-worming, walking barefooted. Hand washing was found to be a protective factor as shown in Table 4.
Table 3.
Association of Intestinal Parasites with Risk Factors in the Study Participants
| Variables | Intestinal Parasite | Total | χ2 | Df | P value | |
|---|---|---|---|---|---|---|
| Present | Absent | |||||
| (N = 92) | (N = 292) | (N = 384) | ||||
| House Structure | ||||||
| One room | 10 (20.4) | 39 (79.6) | 49 (100.0) | |||
| Two rooms | 36 (23.5) | 117 (76.5) | 153 (100.0) | |||
| Three rooms | 35 (26.5) | 97 (73.5) | 132 (100.0) | 1.324 | 4 | 0.857 |
| Four rooms | 5 (18.5) | 22 (81.5) | 27 (100.0) | |||
| Flat | 6 (26.1) | 17 (73.9) | 23 (100.0) | |||
| Number of co-residents | ||||||
| ≤ 5 persons | 14 (22.2) | 49 (77.8) | 63 (100.0) | |||
| 6 - 10 persons | 46 (24.9) | 139 (75.1) | 185 (100.0) | 0.180 | 2 | 0.914 |
| > 10 persons | 32 (24.1) | 101 (75.9) | 133 (100.0) | |||
| Toilet facility | ||||||
| Pit | 59 (25.2) | 175 (74.8) | 234 (100.0) | |||
| Water closet | 23 (20.7) | 88 (79.3) | 111 (100.0) | 8.783 | 3 | 0.032 |
| Bush, Refuse dump, etc | 10 (40.0) | 15 (60.0) | 25 (100.0) | |||
| ‘Shot put’ | 0 (0.0) | 14 (100.0) | 14 (100.0) | |||
| Water source | ||||||
| Well | 76 (24.1) | 239 (75.9) | 315 (100.0) | |||
| Tap | 16 (23.5) | 52 (76.5) | 68 (100.0) | 0.327 | 2 | 0.849 |
| River | 0 (0.0) | 1 (100.0) | 1 (100.0) | |||
| Ever dewormed | ||||||
| Yes | 43 (22.2) | 151 (77.8) | 194 (100.0) | 0.692 | 1 | 0.405 |
| No | 49 (25.8) | 141 (74.2) | 190 (100.0) | |||
| Last deworming | ||||||
| ≤ 1 year | 20 (19.6) | 82 (80.4) | 102 (100.0) | |||
| 2 years | 15 (28.8) | 37 (71.2) | 52 (100.0) | 1.841 | 2 | 0.398 |
| > 2 years | 8 (20.0) | 32 (80.0) | 40 (100.0) | |||
| Walks barefoot | ||||||
| Yes | 77 (25.2) | 228 (74.8) | 305 (100.0) | 1.231 | 1 | 0.267 |
| No | 15 (19.2) | 63 (80.8) | 78 (100.0) | |||
| Hand washing | ||||||
| Yes | 75 (22.6) | 257 (77.4) | 332 (100.0) | 2.518 | 1 | 0.113 |
| No | 17 (32.7) | 35 (67.3) | 52 (100.0) | |||
Table 4.
Binary logistic regression for predictors of intestinal parasite infection
| Variables | B | S.E. | OR (95% CI) | P value |
|---|---|---|---|---|
| Father’s education level | ||||
| None / Primary | 0.152 | 0.133 | 1.165 (0.898 - 1.511) | 0.251 |
| Secondary / Tertiary | 1 | |||
| Toilet facility | ||||
| Shot put / Bush | 0.081 | 0.165 | 1.084 (0.784 - 1.498) | 0.626 |
| Pit / water closet | 1 | |||
| Hand washing | ||||
| Yes | -0.671 | 0.318 | 0.511 (0.274 - 0.953) | 0.035 |
| No | 1 | |||
| Weight loss | ||||
| Present | 0.364 | 0.417 | 1.439 (0.636 - 3.257) | 0.383 |
| Absent | 1 | |||
| Abdominal pain | ||||
| Present | 0.181 | 0.282 | 1.198 (0.689 - 2.081) | 0.522 |
| Absent | ||||
| Nausea | ||||
| Present | 0.326 | 0.388 | 1.386 (0.648 - 2.963) | 0.400 |
| Absent | 1 | |||
| Vomiting | ||||
| Present | 0.183 | 0.428 | 1.200 (0.519 - 2.775) | 0.669 |
| Absent | 1 | |||
| Anorexia | ||||
| Present | 0.232 | 0.415 | 1.261 (0.559 - 2.847) | 0.576 |
| Absent | 1 | |||
| Meat/Fish containing diet | ||||
| < 4 - 5 times/week | 0.046 | 0.094 | 1.047 (0.871 - 1.260) | 0.623 |
| ≥ 4 - 5 times/week | 1 | |||
| Milk containing diet | ||||
| < 4 - 5 times/week | -0.021 | 0.075 | 0.979 (0.846 - 1.134) | 0.781 |
| ≥ 4 - 5 times/week | 1 | |||
| Intelligence Quotient | ||||
| Average / above average | -0.375 | 0.194 | 0.688 (0.470 - 1.006) | 0.054 |
| Mental deficiency / dullness | 1 | |||
| Constant | -1.732 | 1.597 | 0.177 | 0.275 |
Table 5 shows the anthropometric measurements of the study participants. The indices were reported as mean ± SD. The mean weight of the pupils was 27.33±6.20 kg. The mean height of the pupils was 1.28±0.11m and the mean BMI (Body mass index) was 16.56±1.73 kg/m2. The weight, height and BMI were not significantly associated with intestinal parasites (p = 0.517, p = 0.476, p = 0.878 respectively).
Table 5.
Intelligence Quotient by Age and Gender
| Variables | IQ categories, n (%) | Total | ||
|---|---|---|---|---|
| Average | Mental deficiency | Mental dullness | ||
| All Age groups | ||||
| 6 - 7 yrs | 31 (38.8) | 33 (41.2) | 16 (20.0) | 80 (100.0) |
| 8 - 9 yrs | 18 (19.1) | 65 (69.2) | 11 (11.7) | 94 (100.0) |
| 10 - 12 yrs | 29 (13.8) | 153 (72.9) | 28 (13.3) | 210 (100.0) |
| Total | 78 (20.3) | 251 (65.4) | 55 (14.3) | 384 (100.0) |
| χ2 = 29.344, df = 4; p <0.0001 | ||||
| Age group (Male) | ||||
| 6 - 7 yrs | 18 (40.9) | 15 (34.1) | 11 (25.0) | 44 (100.0) |
| 8 - 9 yrs | 7 (15.6) | 29 (64.4) | 9 (20.0) | 45 (100.0) |
| 10 - 12 yrs | 13 (12.9) | 74 (73.2) | 14 (13.9) | 101 (100.0) |
| Total | 38 (20.0) | 118 (62.1) | 34 (17.9) | 190 (100.0) |
| χ2 = 22.526, df = 4; p <0.0001 | ||||
| Age group (Female) | ||||
| 6 - 7 yrs | 13 (36.1) | 18 (50.0) | 5 (13.9) | 36 (100.0) |
| 8 - 9 yrs | 11 (22.4) | 36 (73.5) | 2 (4.1) | 49 (100.0) |
| 10 - 12 yrs | 16 (14.7) | 79 (72.5) | 14 (12.8) | 109 (100.0) |
| Total | 40 (20.6) | 133 (68.6) | 21 (10.8) | 194 (100.0) |
| χ2 = 11.142, df = 4; p = 0.025 | ||||
| Gender | ||||
| Male | 38 (20.0) | 118 (62.1) | 34 (17.9) | 190 (100.0) |
| Female | 40 (20.6) | 133 (68.6) | 21 (10.8) | 194 (100.0) |
| χ2 = 3.979, df = 2; p = 0.137 | ||||
The intelligence quotient of the pupils by age and gender is shown in Table 6. Mental dullness was significantly more prevalent among the 6-7 year group in all pupils together, in boys and in girls. There was however no difference between boys and girls for the different IQ categories.
Table 6.
Intestinal Parasites by Nutritional Status and Intelligence Quotient
| Variables | Intestinal Parasite | Total | χ2 | Df | P value | |
|---|---|---|---|---|---|---|
| Present | Absent | |||||
| (N = 92) | (N = 292) | (N = 384) | ||||
| Nutritional status | ||||||
| Normal weight | 88 (23.9) | 280 (76.1) | 368 (100.0) | |||
| Underweight | 4 (28.6) | 10 (71.4) | 14 (100.0) | 0.794 | 2 | 0.672 |
| Overweight | 0 (0.0) | 2 (100.0) | 2 (100.0) | |||
| Intelligence Quotient | ||||||
| Average | 14 (18.2) | 63 (81.8) | 77 (100.0) | 5.396 | 2 | 0.145 |
| Mental deficiency | 61 (24.3) | 190 (75.7) | 251 (100.0) | |||
| Mental dullness | 16 (29.1) | 39 (70.9) | 55 (100.0) | |||
There was no significant association between intestinal parasites, nutritional status and cognitive function in the study participants. This is shown in Table 6.
In this study 20.6% of the participants had light intensity infection (100-4100 epg of faeces) for Ascaris lumbricoides while 1.6% had moderate intensity infection (5300-12,600 epg of faeces) and none had heavy intensity infection. Only 3.4% of the pupils had light intensity infection (100-700 epg of faeces) for hookworm. Infection intensity was also not found to be associated with nutritional status and cognitive function.
Discussion
The prevalence of intestinal parasites in the study participants was 24%. This is in conformity with the report of Barazesh et al. (2017), who reported a prevalence of 25.1% for intestinal parasites among primary school children in Bushehr, Iran. Similarly Abah et al., (2015) in Rivers State, Nigeria reported a prevalence of 27.6% for intestinal parasitic infections among primary school children. However the prevalence rate obtained in this study is not in agreement with several other studies that reported higher prevalence rates for intestinal parasitic infections among school children. In Yemen, Alwabr et al., (2016) reported an overall prevalence of 90% for intestinal parasites from school children in Yemen. Adefioye et al., (2011) got a prevalence of 52% in a study carried out on school children in Southwest Nigeria. The differences in prevalence rates obtained from these various locations is most likely due to differences in the level of hygiene, environmental contamination and the different age groups used for the studies. Pupils in the age group 10-12 years had the highest prevalence while those in the age group 7-9 years had the lowest prevalence. This is similar to the findings of Sanchez et al., (2013) in which children more than 10 years old were found to be more infected than those in the age group 7-9 years. The finding in this study further emphasizes the importance of health education of school children through their school years as it is not only the younger children that are vulnerable to infection. The prevalence of intestinal parasites in the six schools that were used for the study was between 15.6% - 31.3%. A possible explanation for the varying prevalence rates in these schools could be attributed to the differences in the level of hygiene observed in the schools. There were no statistically significant differences in the rates obtained from these schools. The intestinal parasites obtained in the stool samples of the pupils were Ascaris lumbricoides, Hookworm and Hymenolepis nana. Ascaris lumbricoides had the highest overall infection rate of 22.1%. This is similar to findings from several studies, Adefioye et al., (2011), Nxasana et al., (2013); and Udensi et al., (2015). This was followed by hookworm 3.4% and Hymenolepis nana was the parasite with the lowest infection rate of 0.3%. In addition, Ascaris lumbricoides and Hookworm co-infection occurred in 1.6% of the study participants. Ascaris lumbricoides and Hymenolepsis nana co-infection was also observed in 0.3% of the pupils who participated in this study. In the six schools used for the study, Ascaris lumbricoides was the most prevalent parasite.
The presence of intestinal parasites was not found to be significantly associated with the sociodemographic characteristics of the study participants. This is similar to the findings of Reji et al., (2011) in Ethiopia in which sociodemographic characteristics were not found to be significantly associated with intestinal parasites. The housing amenities of the study participants were also assessed and pupils using bush and refuse dump were more likely to be infected with intestinal parasites compared to the other modes of toilet facilities. Risk factors like history of deworming, walking barefoot were not significantly associated with presence of intestinal parasites. Handwashing was however found to be a protective factor.
The intensity of intestinal parasitic infection in these pupils was also determined. According to the WHO Criteria for infection intensity for soil transmitted helminthes, 20.6% of the study population had light intensity infections for Ascaris lumbricoides and 1.6% had moderate intensity. This is similar to the findings of Ngonjo et al., (2016) where light to moderate intensity was reported for Ascaris lumbricoides. For Hookworm, 3.4% had light intensity infection.
The percentage of pupils that were underweight in this study is very low (3.6%), similar to the findings of Francis et al., (2012) in Uganda where 5.3% 0f the children studied were underweight. However, this is not in agreement with a study in Ethiopia, Reji et al., (2011) where a prevalence of 21.2% was reported for malnutrition. This is probably due to differences in the methods used in assessing the nutritional status of the pupils. Majority (95.8%) of the study participants were normal weight. This is possibly because almost all the participants (96.9%) eat meals provided by the Osun State Government and the meals are usually balanced and more than half of the pupils take breakfast before coming to school.
The Draw a Person Test has been used in some studies, Lobato et al., (2012); Ezenwosu et al., (2013) to assess the intelligence quotient of school children. The findings from this study is similar to the report of a study carried out in Malaysia, Al-Melkafi et al., (2011) in which the intelligence quotient was assessed and 67.6% of the school children were found to have poor intelligence quotient. A study carried out in the Phillipines, Amara et al., (2005) showed that helminthic infection negatively impaired different aspects of cognitive function like learning ability, verbal fluency and working memory using various tests. Surprisingly in the present study there was no association between intestinal parasites, nutritional status and cognitive function. This is not in agreement with some studies, Hesham et al., (2004); Garba et al., (2010) that have shown association between intestinal parasites and nutritional status. However, in this study there were light and moderate intensity infection rates for Ascaris lumbricoides and light intensity infection rate for hookworm but these were not significantly associated with nutritional status and cognitive function. Sakti et al., (1999) also reported an association between hookworm infection and impairment of cognitive function. This is because hookworm infection results in iron deficiency anaemia which affects working memory. However, the prevalence of hookworm infection in this study was very low and the infection intensity was also light. This may probably account for the lack of association between intestinal parasites, nutritional status and cognitive function obtained in this study.
In conclusion, primary school children are still a high risk group for infection. The age group with the highest prevalence of intestinal parasites was 10-12 years. The use of bush or refuse dump as a means of toilet facility was identified as a risk factor. Hand washing was found to be protective and should be encouraged among them. Surprisingly, nutritional status and cognitive function of the pupils were not significantly associated with the presence of intestinal parasites.
Abbreviations
- BMI:
Body Mass Index
- CDC:
Centre for Disease Control
- IQ:
Intelligence Quotient
- OAUTHC:
Obafemi Awolowo University Teaching Hospitals Complex
Acknowledgement
We thank very much the pupils we used for the study. We also appreciate the teachers in the schools and the parents of the pupils for their co-operation for this work. We also appreciate the resident doctors of the Department of Medical Microbiology/Parasitology, OAUTHC for the assistance they gave for this work.
“This research received no specific grant from any funding agency, commercial or not-for-profit sectors.”
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
References
- 1.Abah A.E, Arere F.O.I. Status of Intestinal Parasitic Infections among Primary School Children in Rivers State, Nigeria. Journal of Parasitology Research. 2015;7(3):208–211. doi: 10.1155/2015/937096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adefioye O.A, Efunshile A.M, Ojurongbe O, Akindele A.A, Adewuyi I.K, Bolaji O.S, Adedokun S.A, Adeyeba A.O. Intestinal helminthiasis among School Children in Ilie, Osun State, Southwest Nigeria. Sierraleone Journal of Biomedical Research. 2011;3(1):36–42. [Google Scholar]
- 3.Al-Melkafi H.M, Mahdy M.A, Sallam A.A, Ariffin W.A, Al-Melkafi A.M, Amran A.A, Surin J. Nutritional and Socioeconomic Determinants of Cognitive Function and Educational Achievment of Aboriginal School children in Rural Malaysia. British Journal of Nutrition. 2011;106:1100–1106. doi: 10.1017/S0007114511001449. [DOI] [PubMed] [Google Scholar]
- 4.Alwabr G.M.A, Al-Moayed E.E. Prevalence of Intestinal Parasitic Infections among School Children of Al-Mahweet Governorate, Yemen. European Journal of Biological Research. 2016;6(2):64–73. [Google Scholar]
- 5.Amara E.E, Jeniffer F.F, Luz P.A, David C.B, Gretchen C.L, Daria L.M, Remigio M.O, Jonathan D.K, Stephen T.M. Helminth Infection and Cognitive Impairment among Fillipino Children. American Journal of Tropical Medicine and Hygiene. 2005;72(5):540–548. [PMC free article] [PubMed] [Google Scholar]
- 6.Barazesh A, Fouladvand M, Tahmasebi R, Heydari A, Kooshesh F. Prevalence of Intestinal Parasitic Infections among Primary School Children in Bushehr, Iran, Avicenna. Journal of Clinical Microbiology and Infection. 2017;4(1):1–6. [Google Scholar]
- 7.Ezenwosu O.U, Emodi I.J, Ikefuna A.N, Chukwu B.F, Osuorah C.D. Determinants of Academic Perfomance in Children with Sickle Cell Anaemia. Biomedcentral Journal of Paediatrics. 2013;13:189. doi: 10.1186/1471-2431-13-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Francis L, Kirunda B.E, Orach C.G. Intestinal Helminth Infections and Nutritional Status of Children Attending Primary Schools in Wakiso district, Central Uganda. International Journal of Enviromental Research of Public Health. 2012;9:2910–2921. doi: 10.3390/ijerph9082910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Garba C.M.G, Mbofung C.M.F. Relationship between Malnutrition and Parasitic Infection among School Children in the Adamawa Region of Cameroon. Pakistan Journal of nutrition. 2010;9(11):1094–1099. [Google Scholar]
- 10.G/hiwot Y, Degarege A, Erko B. Prevalence of Intestinal Parasitic Infections among children less than 5 years of age with emphasis onSchistosoma mansoniin Wonji Shoa Sugar Estate, Ethiopia. PLoS ONE. 2014;9(10):e109793. doi: 10.1371/journal.pone.0109793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hesham M.S, Edariah A.B, Norhayati M. Intestinal Parasitic Infections and Micronutrient Deficiency:A Review. Medical Journal of Malaysia. 2004;59:284–292. [PubMed] [Google Scholar]
- 12.Lobato L, Miranda A, Faria I.M, Bethony J.M, Gazzinelli M.F. Development of Cognitive Abilities of Children infected with Helminths Through Health Education. Revista da Sociedade Brasileira de Medicina Tropical. 2012;45(4):514–519. doi: 10.1590/s0037-86822012000400020. [DOI] [PubMed] [Google Scholar]
- 13.Ngonjo T, Okoyo C, Andore C, Simiyu E, Lelo A.E, Kabiru E, Kihara J, Mwandawiro C. Current Status of Soil-transmitted Helminths among SchoolChildren in Kakamega County, Western Kenya. Journal of Parasitology Research. 2016:1–9. doi: 10.1155/2016/7680124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nxasana N, Baba K, Bhat V.G, Vasaikar S.D. Prevalence of Intestinal parasites in Primary School Children of Mthatha, Eastern Cape Province, South Africa. Annals of Medical and Health Sciences Research. 2013;3(4):511–516. doi: 10.4103/2141-9248.122064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reji P, Belay G, Erko B, Legesse M, Belay M. Intestinal Parasitic Infections and Malnutrition among First-cycle Primary School Children in Adama, Ethiopia. African Journal of Primary Health care and Family Medicine. 2011;3(1):1–5. [Google Scholar]
- 16.Sakti H, Nokes C, Subagio Hertanto W. Evidence for an Association between Hookworm Infection and Cognitive Function in Indonesian School Children. Tropical Medicine and International Health. 1999;4(5):322–324. doi: 10.1046/j.1365-3156.1999.00410.x. [DOI] [PubMed] [Google Scholar]
- 17.Sanchez A.L, Gabrie J.A, Usuanlele M-T, Raeda M.M, Canales M, Gyorkos T.W. Soil-transmitted Helminthic Infections and Nutritional Status in School-age Children from Rural Communities in Honduras. PLoS Neglected Tropical Diseases. 2013;7(8):1–9. doi: 10.1371/journal.pntd.0002378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Udensi U.J, Mgbemena I.C, Emeka-Nwabunnia I, Ugochukwu M.G, Awurum I.N. Prevalence of Intestinal Parasites among Primary School Children in Three Geopolitical Zones of Imo State, Nigeria. Science Journal of Public Health. 2015;3(5):25–28. [Google Scholar]


