Abstract.
Acute conjunctivitis follows a seasonal pattern. Although its clinical course is typically self-limited, conjunctivitis epidemics incur a substantial economic burden because of missed school and work days. This study investigated seasonal and temporal trends of childhood conjunctivitis in the entire country of Burkina Faso from 2013 to 2016, using routine monthly surveillance from 2,444 government health facilities. A total of 783,314 cases were reported over the 4-year period. Conjunctivitis followed a seasonal pattern throughout the country, with a peak in April. A nationwide conjunctivitis outbreak with a peak in September 2016 was noted (P < 0.001), with an excess number of cases first detected in June 2016. Nationwide passive surveillance was able to detect an epidemic 3 months before its peak, which may aide in allocation of resources for containment and mitigation of transmission in future outbreaks.
INTRODUCTION
Acute conjunctivitis has been shown to follow a seasonal pattern in many areas, including in the United States, which has a peak in cases in April and May.1–3 Bacterial and viral conjunctivitis is highly transmissible and thus is prone to outbreaks.4,5 Epidemic keratoconjunctivitis (EKC) is a common eye infection globally, and EKC outbreaks are reported regularly in the United States.6 Acute hemorrhagic conjunctivitis (AHC) has epidemic potential in tropical regions.7 Acute hemorrhagic conjunctivitis was first described in Ghana in 1969,8,9 and large outbreaks are regularly reported in tropical regions of the world.5,10,11 Although the course of conjunctivitis is typically self-limited, conjunctivitis can cause missed school or work time and represents a substantial economic burden.12 Routine surveillance for conjunctivitis may help identify patterns in conjunctivitis and detect outbreaks earlier, which may help with control measures, such as hygiene improvement and quarantine, and curb transmission.1,13,14 Here, we report temporal and seasonal trends in childhood conjunctivitis from routine countrywide surveillance via health facilities in Burkina Faso.
METHODS
Beginning in 2013, conjunctivitis was reported to the Ministry of Health in Burkina Faso as a count of the number of cases per month from each of 2,444 health facilities in the 13 administrative regions of the country. Each health facility uses a standardized form to record the number of conjunctivitis cases per calendar month, with separate counts for neonatal, child, and adult cases. Data are subsequently reported to the Ministry of Health on a monthly basis. We obtained monthly count data for each health facility in the entire country of Burkina Faso from the Ministère de la Santé in Ouagadougou. Here, we report monthly count outcomes for childhood conjunctivitis cases.
The total population in each region per year was extracted from the Institut National de la Statistique et de la Démographie in Burkina Faso, which published the total population per region per year until 2015. The population per region in 2016 was estimated based on the growth rate from 2014 to 2015. The number of cases per 10,000 population per region per year was calculated by dividing the number of cases per region per year by the total population estimated in the census. We used negative binominal regression to model the monthly case counts, using 1) cyclic splines to model variation over the course of a year and 2) a linear trend. Seasonal variation and linear trends were both allowed to vary for each of the 13 regions in Burkina Faso. The epidemic period was easily identified by a large residual variation during the months of mid-to-late 2016. We estimated the number of cases that would have occurred in the absence of an epidemic using a second regression in which an epidemic basis function was introduced during the period of maximum residual deviation. Analyses were conducted in R (version 3.3.1, The R Foundation for Statistical Computing, package MASS).
RESULTS
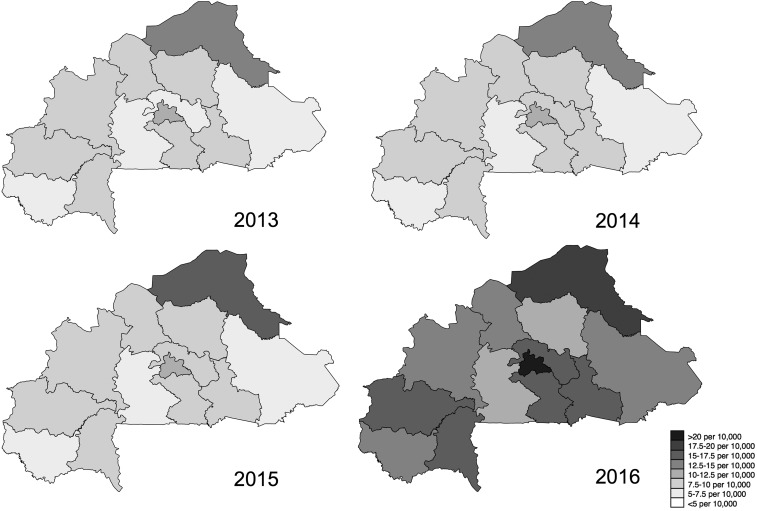
Data were available from January 2013 through December 2016. Nationwide, a total of 783,314 cases of conjunctivitis were reported over this period: 147,437 in 2013, 162,2499 in 2014, 170,665 in 2015, and 302,713 in 2016. Figure 1 shows the number of cases per 10,000 population per year. The case per 10,000 population rate was consistent from 2013 through 2015, and the rate roughly doubled in 2016. The Sahel region had the highest number of cases during the non-epidemic years, ranging from 13.1 to 16.2 per 10,000. In 2016, Center, the region in which the capital Ouagadougou is located, had the highest number of cases at 23.5 per 10,000.
Figure 1.
Cases per 10,000 population by region and year. Darker shades of gray indicate greater proportion of cases.
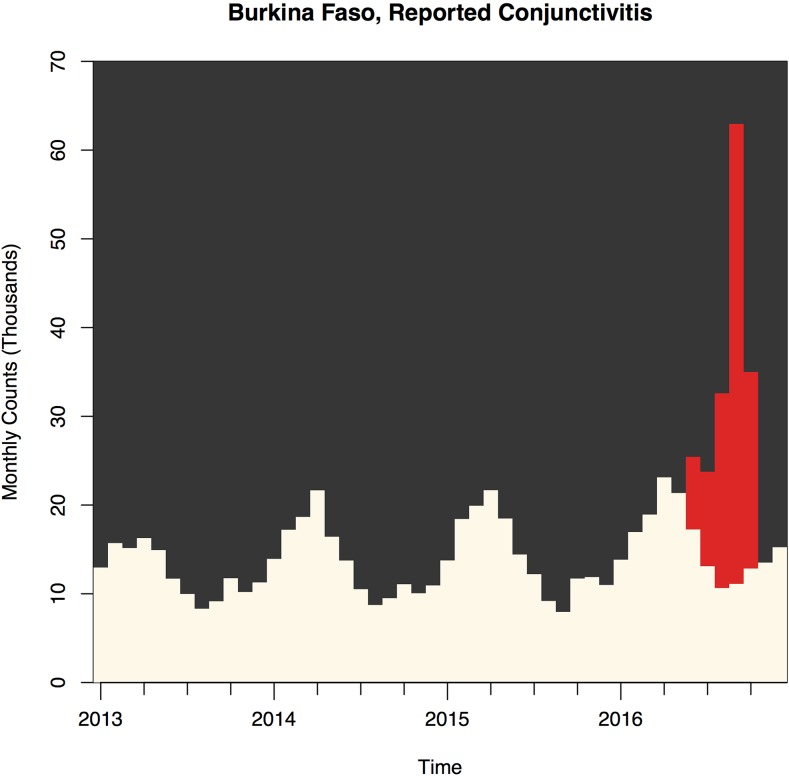
Figure 2 shows the distribution of conjunctivitis cases by month for the country from 2013 to 2016. There was a distinct seasonal pattern each year, with cases peaking in April each year (P < 0.001 for seasonal trend). An epidemic was detected in 2016 (P < 0.001 for difference in the number of cases compared with that expected based on previous years), with the first excess cases detected in June 2016 and peaking in September 2016. The number of cases returned to normal levels in November 2016. The government data did not break down conjunctivitis cases by etiology. However, a government ophthalmologist reviewed available medical records from 491 patients from August to October 2016 and found that 41% were AHC, 22% were bacterial, and 37% were allergic (A. Diarra, personal communication).
Figure 2.
Number of conjunctivitis cases reported by month and year nationwide. Red bars indicate excess cases over expected seasonal trends. Beige bars under the red bars indicate the number of cases that would have been expected based on trends in previous years. This figure appears in color at www.ajtmh.org.
DISCUSSION
A nationwide conjunctivitis epidemic occurred in Burkina Faso in the second half of 2016. The earliest time an excess number of cases could be detected was in June, 3 months before the peak of the epidemic. The number of cases returned to normal levels by November, 2 months after the spike. The epidemic did not coincide with the underlying seasonal pattern of conjunctivitis cases, which normally increases in April and subsides by June. In fact, the peak epidemic months of September and October are normally the nadir of the seasonality of conjunctivitis. Because the national surveillance mechanism does not report the etiology of conjunctivitis cases and because of the difficulty in determining etiology, it is unknown whether these cases were viral, bacterial, or allergic. It is likely that the cases were a mix of AHC, allergic, and bacterial.
The cause of the seasonal conjunctivitis pattern is unclear. The consistency of the pattern implicates environmental risk factors, and we hypothesize that seasonal allergies from pollen and other allergens may ultimately be responsible, although this remains a conjecture on our part. Of note, March through May is the hottest period of the year in Burkina Faso and is before the rainy season that normally begins in June and reaches peak intensity in August.15 Adenoviral epidemics in regions with poor access to potable water occur concurrent to the rainy season, possibly because of fecal contamination of drinking and bathing water from runoff of contaminated surface water. Consistent with our hypothesis, allergic conjunctivitis has been shown to correlate with increased temperature in China16 and peaks in April–May in the United States.1 However, seasonal patterns in nonallergic conjunctivitis have also been noted.1 A better understanding of the causes of seasonal variation in conjunctivitis would allow for a better public health response, which would differ depending on whether the underlying surge in cases was allergic versus infectious. If the former, interventions could focus on early treatment of children with known allergies and educating health providers about the normal timing of allergic conjunctivitis. If the latter, interventions could focus on improving hygiene and quarantining children from schools and day care centers during the spring swell in cases.
The region with the highest incidence of conjunctivitis was the Sahel. Currently, Sahel faces insecurity because of its proximity to Mali and is also the location of two camps for Malian refugees. Highly transmissible diseases such as conjunctivitis may spread rapidly in refugee settings because of overcrowding and hygiene concerns,17 which could contribute to the excess number of cases reported in the region. Although the Sahel region had the second highest rate of conjunctivitis during the epidemic (second to Center), it had the smallest increase in the number of cases from 2015 compared with any other region. This may be due to already high background rates or differences in epidemic dynamics in this region.
This analysis has several limitations. Using national-level surveillance data provides large numbers and data for all available health facilities in the country but is also subject to the constraints of administrative data. For example, the database did not include individual-level information on etiology or case definitions of the conjunctivitis cases, and even if it did, such data would be subject to misclassification error. We reported data on conjunctivitis etiology from a single ophthalmologist, although these data may not be generalizable to the entire country and could likewise be subject to misclassification error. It is highly likely that not all caregivers of children with conjunctivitis seek care for the condition, so the incidence estimates herein are almost certainly an underestimate of the true incidence of conjunctivitis in Burkina Faso. However, the overall trends should still be reflective of conjunctivitis epidemiology more generally in the country. Given the consistency in seasonal trends over time and the finding that epidemic cases returned to normal levels in November 2016, it is unlikely that temporal trends reported here are reflective of an increase in care seeking or reporting behavior. Finally, data are reported on a monthly basis, and data are currently collected via paper and thus data are not monitored in real time. Data entry and transmission time could be reduced with the introduction of electronic systems, which may allow for real-time monitoring and earlier detection of potential outbreaks.
In summary, we demonstrated consistent seasonal trends in reported conjunctivitis cases in Burkina Faso across the entire country, with a consistent increase in reported cases each April. Routine passive surveillance via clinic-based reports of conjunctivitis revealed a large epidemic in late 2016, which was experienced throughout the country. Nationwide clinic-based surveillance for conjunctivitis detected an epidemic 3 months before the peak in the epidemic. Early detection of epidemics may aide in allocation of resources for containment and prevention of transmission of potential outbreaks.
REFERENCES
- 1.Deiner MS, Lietman TM, McLeod SD, Chodosh J, Porco TC, 2016. Surveillance tools emerging from search engines and social media data for determining eye disease patterns. JAMA Ophthalmol 134: 1024–1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ramirez DA, Porco TC, Lietman TM, Keenan JD, 2017. The epidemiology of conjunctivitis in United States emergency departments: a population-based study. JAMA Ophthalmol 135: 1119–1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Deiner MS, McLeod SD, Chodosh J, Oldenburg CE, Fathy CA, Lietman TM, Porco TC, 2018. Clinical age-specific seasonal conjunctivitis patterns and their online detection in twitter, blog, forum, and comment social media posts. Invest Ophthalmol Vis Sci 59: 910–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang L, Zhao N, Sha J, Wang C, Jin X, Amer S, Liu S, 2016. Virology and epidemiology analyses of global adenovirus-associated conjunctivitis outbreaks, 1953–2013. Epidemiol Infect 144: 1661–1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patriarca PA, Onorato IM, Sklar VEF, Schonberger LB, Kaminski RM, Hatch MH, Morens DM, Forster RK, 1983. Acute hemorrhagic conjuctivitis: investigation of a large-scale community outbreak in Dade County, Florida. JAMA 249: 1283–1289. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC) , 2013. Adenovirus-associated epidemic keratoconjunctivitis outbreaks—four states, 2008–2010. MMWR Morb Mortal Wkly Rep 62: 637–641. [PMC free article] [PubMed] [Google Scholar]
- 7.Dawson CR, Whitcher JP, Schmidt NJ, 1974. Editorial: acute hemmorhagic conjunctivitis. JAMA 230: 727–728. [DOI] [PubMed] [Google Scholar]
- 8.Minami K, Otatsume S, Mingle JA, Afoakwa SN, Quarcoopome CO, Konno K, Uchida Y, Kurahashi H, Kono R, 1981. Seroepidemiologic studies of acute hemmorrhagic conjunctivitis virus (enterovirus type 70) in West Africa: I. Studies with human sera from Ghana collected eight years after the first outbreak. Am J Epidemiol 114: 267–273. [DOI] [PubMed] [Google Scholar]
- 9.Chatterjee S, Quarcoopome CO, Apenteng A, 1970. Unusual type of epidemic conjunctivitis. Brit J Opthal 54: 628–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Medina NH, Haro-Muñoz E, Pellini AC, Machado BC, Russo DH, Timenetsky MD, Carmona RC, 2016. Acute hemorrhagic conjunctivitis epidemic in São Paulo state, Brazil, 2011. Rev Panam Salud Publica 39: 137–141. [PubMed] [Google Scholar]
- 11.Chansaenroj J, Vongpunsawad S, Puenpa J, Theamboonlers A, Vuthitanachot V, Chattakul P, Areechokchai D, Poovorawan Y, 2015. Epidemic outbreak of acute haemorrhagic conjunctivitis caused by coxsackievirus A24 in Thailand, 2014. Epidemiol Infect 143: 3087–3093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smith AF, Waycaster C, 2009. Estimate of the direct and indirect annual cost of bacterial conjunctivitis in the United States. BMC Ophthalmol 9: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kuo IC, Espinosa C, Forman M, Valsamakis A, 2016. A polymerase chain reaction-based algorithm to detect and prevent transmission of adenoviral conjunctivitis in hospital employees. Am J Ophthalmol 163: 38–44. [DOI] [PubMed] [Google Scholar]
- 14.Imonikhe R, Flynn TH, Mearza AA, 2011. Determination of seasonal allergic conjunctivitis variation using internet search engine data. Eye (Lond) 25: 1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Diboulo E, Sié A, Rocklöv J, Niamba L, Yé M, Bagagnan C, Sauerborn R, 2012. Weather and mortality: a 10 year retrospective analysis of the Nouna health and demographic surveillance system, Burkina Faso. Glob Health Action 5: 32–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hong J, et al. 2016. Ambient air pollution, weather changes, and outpatient visits for allergic conjunctivitis: a retrospective registry study. Sci Rep 6: 23858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burki T, 2013. Infectious diseases in Malian and Syrian conflicts. Lancet Infect Dis 13: 296–297. [DOI] [PubMed] [Google Scholar]