Abstract.
Microsporidia are protists close to the kingdom of fungi that may cause eye infections. Most cases are reported in Asia and affect both immunocompromised and immunocompetent patients. Here, we report a rare case of microsporidial keratoconjunctivitis in an immunocompetent French patient 3 weeks after returning from India. In our patient, Weber trichrome staining of conjunctival scrapings revealed rounded elements approximately 1–3 μm in size. Conventional polymerase chain reaction analysis by ribosomal RNA subunit sequencing showed 100% identity with Vittaforma corneae. Treatment by corneal debridement combined with fluoroquinolone eye drops allowed complete resolution of the lesions. Although rare, ocular microsporidiosis should be investigated in a patient who is native to Asia or has returned from an endemic area and presents with keratoconjunctivitis of undetermined etiology.
INTRODUCTION
Microsporidia are eukaryotic, obligate microorganisms with intracellular tropism, closely related to the kingdom of fungi.1 Since their first discovery in 1857, approximately 1,300 species belonging to nearly 200 genera have been described.2,3 The organisms are ubiquitous in distribution and cause a wide spectrum of clinical infections in humans, including digestive, ocular, sinus, pulmonary, muscular, and renal infections, mainly involving immunosuppressed patients.4–6 Ocular disease is the second most common type of infection after digestive infection.7 Early published studies described two distinct clinical entities affecting the cornea which appear to be correlated to the immune status of the patient: superficial keratoconjunctivitis in immunosuppressed patients and punctate stromal keratitis in immunocompetent patients.8–10 However, over the past few years, the incidence of microsporidial keratoconjunctivitis has increased significantly in immunocompetent individuals in Asia.11
We report a case of ocular microsporidiosis diagnosed in France in an immunocompetent patient who had returned from a holiday in India. We also present a mini-review of the literature dealing with this subject.
CASE REPORT
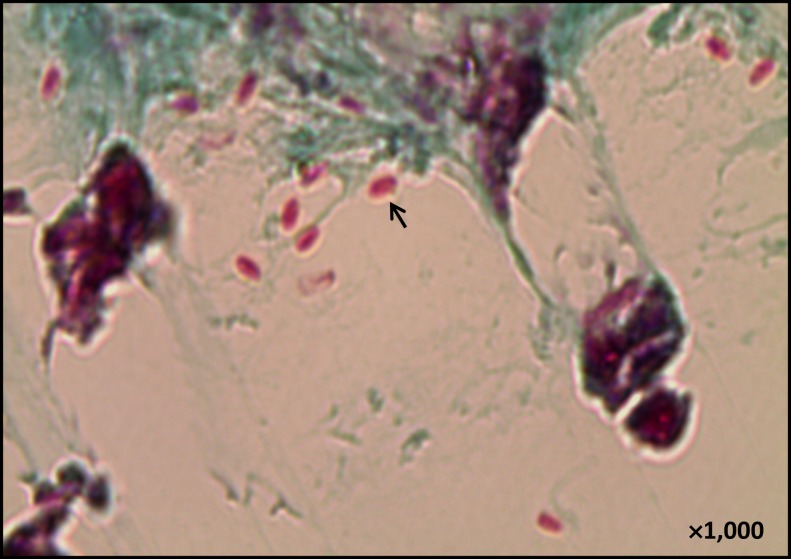
A 53-year-old male patient, living in France and without any previous medical history, presented at the end of September 2015 at the ophthalmology emergency department of Lille University Hospital with unilateral redness of the left eye associated with a decrease in visual acuity, despite the use of norfloxacin-based eye lotion (Chibroxine®; Théa Laboratoires, Clermont Ferrand, France) for several days. The patient reported that he had been in Rajasthan and Uttar Pradesh (India) for 3 weeks during the monsoon season (August) and had bathed in hotel swimming pools in Jaisalmer and New Delhi. Scraping of the eye lesion was performed. Gram’s stain did not reveal any bacteria. Different culture media (blood agar, PolyVitex chocolate agar, heart/brain broth, Lowenstein–Jensen medium, and Sabouraud agar) were sterile. Investigations for Acanthamoeba spp. were also negative. Many oval elements, 1–3 μm in size (Figure 1), were observed after staining with Weber’s modified trichrome. Investigations for Microsporidium spp. in corneal scrapings by conventional PCR targeting the small subunit rRNA gene (forward primer 5′-CAGGTTGATTCTGCCTGACG-3′ and reverse primer 5′-ATCTCTCAGGCTCCCTCTCC-3′) followed by sequencing of the PCR product showed 100% identity (GenBank accession number MG206087) with Vittaforma corneae sequences.12 The disease resolved within 15 days after corneal debridement and local treatment with eye lotion (Norfloxacin 0.3%).
Figure 1.
Corneal scraping stained with Weber’s modified trichrome (×1,000).
DISCUSSION
Microsporidiosis was first described in 1857 in silkworms by Carl Wihelm von Nägeli.2 The eukaryotic, unicellular, obligate intracellular parasites involved are ubiquitous and have a worldwide distribution.4,13 The term “microsporidia” is a designation without any taxonomic justification, currently used to designate organisms belonging to the phylum of Microspora included in the subkingdom of Protista.14 Phylogenetic analysis suggests that the Microsporidia are related to the Cryptomycota as a sister group to the fungi.15,17
Currently, 14 species of microsporidia have been implicated in human diseases.18 The species described in human ocular infections belong to seven distinct genera: Enterocytozoon, Encephalitozoon, Pleistophora, Traphipleistophora, Brachiola, Nosema, and Vittaforma.19 Cases have been described anecdotally in Europe, Africa, South America, and the United States.20,21 Although rare, most cases of ocular microsporidiosis are found in Asia. They have been reported in China, Malaysia, and Thailand, and an increasing number of cases are being reported in India and Singapore.22–24 Their prevalence varies depending on the region and the diagnostic methods available.21 In Asia, the prevalence of microsporidial keratoconjunctivitis varies between 0.4% and 19.7%,23,25 whereas the prevalence of stromal keratitis is lower.26 To date, 56 cases of Vittaforma corneae corneal lesions were reported in the Southeast Asia (Table 1).27–30
Table 1.
Cases of Vittaforma corneae corneal lesions reported in the Southeast Asia
| Country | Clinical form | Identification methods | Contamination | Number of cases | Treatment | Reference |
|---|---|---|---|---|---|---|
| India | Keratoconjunctivitis stromal keratitis | PCR (SSU-rRNA) | Water, insect, dust, trauma | 15 | NR | 57 |
| Singapore | Keratoconjunctivitis | PCR (SSU-rRNA) | Mud/soil | 11 | NR | 27 |
| Vietnam | Keratoconjunctivitis stromal keratitis | EM and PCR (SSU-rRNA) | Water | 1 | Penetrating keratoplasty | 28 |
| Taiwan | Keratoconjunctivitis | PCR (16S rRNA) | Water (hot springs) | 6 | Debridement, topical antibiotics | 36 |
| Taiwan | Keratoconjunctivitis | PCR (16S rRNA) | NR | 10 | Swabbing, topical antibiotics | 29 |
| Singapore | Keratoconjunctivitis | PCR (SSU-rRNA) | Mud/soil | 4 | Fluoroquinolone, topical antibiotics | 30 |
| India | Stromal keratitis | PCR (SSU-rRNA) | NR | 9 | NR | 9 |
EM = electronmicroscopy; NR = not reported; SSU = small subunit.
The sources and routes of ocular infection are less clear than those for digestive diseases.31 Although cases of zoonotic, aerial, alimentary, and interhuman infection have been described, water sources are probably the most important route of infection because most potentially pathogenic species to humans have been identified in water and are resistant to chlorine.2,32,33 Predisposing factors include the wearing of contact lenses and misuse of lens cleaning solutions, surgery or corneal transplant, corticosteroid eye lotion, trauma, bathing in thermal baths, and exposure to dirty water or soil.23,34–36 An epidemic has been reported in rugby players.10 Seasonal variation in infection has been observed in Singapore, India, and Thailand, with a peak in incidence of around 60% in the monsoon period, from July to October.11,23,37
Microsporidia are characterized by their spore. This structure is responsible for resistance to environmental changes and allows for dissemination.38 The spore length varies depending on the species and is generally between 2 and 8 μm, with variations from 1 to 30 μm.32 Microsporidia do not possess a peroxisome or mitochondria but have an organelle known as a mitosome.2 The cell wall of the spore is composed of a double envelope with an outer part (exospore) containing glycoproteins and an inner part (endospore) rich in chitin.5,39 The endospore conceals the plasma membrane delimiting the sporoplasm, the infectious element formed by the cytoplasm and one or two nuclei.40 Microsporidia can be distinguished from other unicellular organisms by the presence of an ejection apparatus known as the polar filament, which is involved in host cell invasion.13 Different stimuli can induce quasi-instantaneous extrusion of the polar filament, which ejects the sporoplasm into the cytoplasm of the host cell.39
Ocular microsporidiosis affects the cornea, with deep or superficial lesions, and/or the conjunctiva. The most frequently reported forms include punctate stromal keratitis and superficial keratoconjunctivitis. Scleritis and endophthalmia are rare (Table 2).19,21,41–43 The first case of ocular microsporidiosis was described in a child in Sri Lanka in 1973.44 It was only in the 1990s, during the acquired immune deficiency syndrome epidemic, that a much larger number of cases of keratoconjunctivitis were reported.45 Since early 2000, an increase in stromal keratitis and keratoconjunctivitis cases has been described in immunocompetent patients.21,46 As reported previously for our immunocompetent case, clinical symptoms include unilateral pain, conjunctival redness, photophobia, the sensation of a foreign body in the eye, and blurred vision.35,45 Progressive and significant decrease in visual acuity complicated by a perforated corneal ulcer in stromal keratitis was also reported.47 The clinical features of our case may mimic adenovirus or herpes keratoconjunctivitis. However, it appears that the infection is deeper and more extensive in ocular microsporidiosis.21,45,47 Recently, Herpes virus and microsporidia have been reported to coexist in granulomatous inflammation.48
Table 2.
Clinical details and isolated species of reported human cases with microsporidosis of the eye, according to the location of lesion
| Location | Characteristics of lesion | Immune status of patient most often reported | Main species | Treatment reported to be effective | References |
|---|---|---|---|---|---|
| Conjunctiva and cornea | Superficial lesions; keratoconjunctivitis | Immunosuppressed/immunocompetent | Encephalitozoon | Albendazole and/or topical fumidil B alternative: Fluoroquinolone | 10, 18, 56, 58, 61 |
| Deep lesions; punctate stromal keratitis | Immunocompetent | Nosema and Microsporidium | Penetrating keratoplasty | 10, 18, 62 | |
| Sclera | Scleritis | Immunocompetent (N = 1) | NR | NR | 41 |
| Interior eye | Endophthalmia | Immunosuppressed (N = 2) | NR | NR | 42, 43 |
| Immunocompetent (N = 1) |
NR = not reported.
Electron microscopy was formerly the reference technique for the identification of species based on studying the structural characteristics of the spore.49,50 However, this tedious and time-consuming technique has low sensitivity and is not available routinely.5 The diagnosis of microsporidiosis is generally made by optical microscopy. Different stains are used and a combination of stains can increase the sensitivity of microscopic examination.51 Using Weber’s modified trichrome stain,52 spores of microsporidia appear a brilliant pink against a blue or pale green background (Figure 1).51 Other stains used routinely, such as Gram or Giemsa stain, have very limited usefulness for ocular specimens. The spores stain strongly and oval, non-budding forms can be seen which can easily be confused with bacteria or yeasts.51,53 Fluorochromes Calcofluor white 2M (Merck, Darmstadt, Germany) and Uvitex 2B (Polysciences Inc. Warrington, PA) electively stain chitin in the cell wall of microsporidia spores. This technique has the advantage of being easy, rapid, and sensitive.49 Nevertheless, reading of slides is time consuming, requires an experienced eye, and does not allow species identification.14 Precise identification of the species involved is essential for determining the most effective treatment and risk of dissemination.25
Molecular identification has the advantage of being rapid and helps to identify most of the species implicated in ocular infections, including V. corneae, Encephalitozoon hellem, Encephalitozoon cuniculi, and Encephalitozoon intestinalis.14 PCR techniques specific for these species have been developed and described.12,14,54–56 A pan-species PCR, based on amplification of a fragment of 16S rRNA, was developed by an Indian group using conjunctival specimens and had a sensitivity of 83% and specificity of 98%.57 In our patient, V. corneae was identified using a similar molecular approach.
Medical treatment of ocular microsporidiosis has variable success. Its efficacy depends on the species involved and immune status of the patient.26 Albendazole and fumagillin have superior in vitro activity to other drugs used in the treatment of keratoconjunctivitis, whereas stromal keratitis appears to be refractory to a number of drugs.26,35,58 Albendazole has good activity against Encephalitozoon spp. but only weak activity against Enterocytozoon bieneusi.58 Fumagillin has been studied in in vitro and in vivo models and has been shown to be active against infections caused by E. hellem, E. cuniculi, E. intestinalis, E. bieneusi, and V. corneae.58–60 Topical use of fumidil B is recommended for the treatment of keratoconjunctivitis.35 Fluoroquinolone eyewashes have been used as an alternative in human cases.35,53,61 Surgical debridement does not appear to be superior to medical treatment and is not required in most of the patients with keratoconjunctivitis.62,63 Furthermore, a randomized study demonstrated complete cure, without recurrence, in the absence of medical treatment, reinforcing the idea that keratoconjunctivitis is an anatomically limited infection.26,64 Corticosteroids appear to be ineffective and may even make the disease worse.10 In our patient, corneal debridement and administration of fluoroquinolones resulted in definitive treatment. By contrast, stromal keratitis requires early surgical treatment by penetrating or deep anterior lamellar keratoplasty.65
Although rare, microsporidia are an emerging cause of ocular infection in immunocompetent patients. This etiology should be evoked in a patient with keratitis of undetermined origin originating or returning from Asia, particularly during the rainy season.
Acknowledgments:
We thank Jean-Michel Dewitte for his excellent technical assistance and Val Hopwood for editing the manuscript.
REFERENCES
- 1.Keeling P, 2009. Five questions about microsporidia. PLoS Pathog 5: e1000489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Didier ES, Stovall ME, Green LC, Brindley PJ, Sestak K, Didier PJ, 2004. Epidemiology of microsporidiosis: sources and modes of transmission. Vet Parasitol 126: 145–166. [DOI] [PubMed] [Google Scholar]
- 3.Vávra J, Lukeš J, 2013. Microsporidia and “the art of living together”. Adv Parasitol 82: 253–319. [DOI] [PubMed] [Google Scholar]
- 4.Franzen C, Müller A, 1999. Cryptosporidia and microsporidia—waterborne diseases in the immunocompromised host. Diagn Microbiol Infect Dis 34: 245–262. [DOI] [PubMed] [Google Scholar]
- 5.Didier ES, 2005. Microsporidiosis: an emerging and opportunistic infection in humans and animals. Acta Trop 94: 61–76. [DOI] [PubMed] [Google Scholar]
- 6.Anane S, Attouchi H, 2010. Microsporidiosis: epidemiology, clinical data and therapy. Gastroenterol Clin Biol 34: 450–464. [DOI] [PubMed] [Google Scholar]
- 7.Sharma S, Das S, Joseph J, Vemuganti GK, Murthy S, 2011. Microsporidial keratitis: need for increased awareness. Surv Ophthalmol 56: 1–22. [DOI] [PubMed] [Google Scholar]
- 8.Weber R, Bryan RT, 1994. Microsporidial infections in immunodeficient and immunocompetent patients. Clin Infect Dis 19: 517–521. [DOI] [PubMed] [Google Scholar]
- 9.Bharathi MJ, Murugan N, Kumar GR, Ramakrishnan R, Anitha V, Ramesh S, 2013. Vittaforma corneae keratitis in southern India: role of a novel duplex PCR. J Med Microbiol 62: 553–559. [DOI] [PubMed] [Google Scholar]
- 10.Kwok AKH, Tong JMK, Tang BSF, Poon RWS, Li WWT, Yuen KY, 2013. Outbreak of microsporidial keratoconjunctivitis with rugby sport due to soil exposure. Eye (Lond) 27: 747–754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thanathanee O, Athikulwongse R, Anutarapongpan O, Laummaunwai P, Maleewong W, Intapan PM, Suwan-Apichon O, 2016. Clinical features, risk factors, and treatments of microsporidial epithelial keratitis. Semin Ophthalmol 31: 266–270. [DOI] [PubMed] [Google Scholar]
- 12.Bart A, Wentink-Bonnema EM, Heddema ER, Buijs J, van Gool T, 2008. Frequent occurrence of human-associated microsporidia in fecal droppings of urban pigeons in Amsterdam, The Netherlands. Appl Environ Microbiol 74: 7056–7058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Franzen C, 2004. Microsporidia: how can they invade other cells? Trends Parasitol 20: 275–279. [DOI] [PubMed] [Google Scholar]
- 14.Franzen C, Müller A, 1999. Molecular techniques for detection, species differentiation, and phylogenetic analysis of microsporidia. Clin Microbiol Rev 12: 243–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Franzen C, 2008. Microsporidia: a review of 150 years of research. Open Parasitol J 2: 1–34. [Google Scholar]
- 16.Keeling PJ, 2014. Phylogenetic place of microsporidia in the tree of eukaryotes. Weiss LM, Becnel JJ, eds. Microsporidia Chichester, United Kingdom: John Wiley & Sons, Inc., 195–202. Available at: http://onlinelibrary.wiley.com/doi/10.1002/9781118395264.ch5/summary. Accessed April 12, 2016. [Google Scholar]
- 17.James TY, Pelin A, Bonen L, Ahrendt S, Sain D, Corradi N, Stajich JE, 2013. Shared signatures of parasitism and phylogenomics unite cryptomycota and microsporidia. Curr Biol 23: 1548–1553. [DOI] [PubMed] [Google Scholar]
- 18.Didier ES, Weiss LM, 2011. Microsporidiosis: not just in AIDS patients. Curr Opin Infect Dis 24: 490–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bhosale NK, Ganesan N, 2015. Microsporidial keratitis. J Bacteriol Parasitol 6: 248. [Google Scholar]
- 20.Friedberg DN, Stenson SM, Orenstein JM, Tierno PM, Charles NC, 1990. Microsporidial keratoconjunctivitis in acquired immunodeficiency syndrome. Arch Ophthalmol 108: 504–508. [DOI] [PubMed] [Google Scholar]
- 21.Garg P, 2013. Microsporidia infection of the cornea—a unique and challenging disease. Cornea 32 (Suppl 1): S33–S38. [DOI] [PubMed] [Google Scholar]
- 22.Vemuganti GK, Garg P, Sharma S, Joseph J, Gopinathan U, Singh S, 2005. Is microsporidial keratitis an emerging cause of stromal keratitis?—a case series study. BMC Ophthalmol 5: 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Loh RS, Chan CML, Ti SE, Lim L, Chan KS, Tan DTH, 2009. Emerging prevalence of microsporidial keratitis in Singapore: epidemiology, clinical features, and management. Ophthalmology 116: 2348–2353. [DOI] [PubMed] [Google Scholar]
- 24.Tung-Lien Quek D, Pan JC-H, Krishnan PU, Zhao PS, Teoh SCB, 2011. Microsporidial keratoconjunctivitis in the tropics: a case series. Open Ophthalmol J 5: 42–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Joseph J, Sridhar MS, Murthy S, Sharma S, 2006. Clinical and microbiological profile of microsporidial keratoconjunctivitis in southern India. Ophthalmology 113: 531–537. [DOI] [PubMed] [Google Scholar]
- 26.Sharma S, Balne PK, Das S, 2014, Ocular microsporidiosis. Weiss LM, Becnel JJ, eds. Microsporidia. Chichester, United Kingdom: John Wiley & Sons, Inc., 403–419. [Google Scholar]
- 27.Chan KS, Koh TH, 2008. Extraction of microsporidial DNA from modified trichrome-stained clinical slides and subsequent species identification using PCR sequencing. Parasitology 135: 701–703. [DOI] [PubMed] [Google Scholar]
- 28.Badenoch PR, Coster DJ, Sadlon TA, Klebe S, Stirling JW, Jaunzems AE, Mazierska JE, 2011. Deep microsporidial keratitis after keratoconjunctivitis. Clin Exp Ophthalmol 39: 577–580. [DOI] [PubMed] [Google Scholar]
- 29.Fan N-W, Lin P-Y, Chen T-L, Chen C-P, Lee S-M, 2012. Treatment of microsporidial keratoconjunctivitis with repeated corneal swabbing. Am J Ophthalmol 154: 927–933.e1. [DOI] [PubMed] [Google Scholar]
- 30.Tan J, et al. 2013. Microsporidial keratoconjunctivitis after rugby tournament, Singapore. Emerg Infect Dis 19: 1484–1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weiss LM, Becnel JJ, 2014. Microsporidia: Pathogens of Opportunity. Chichester, United Kingdom: John Wiley & Sons. [Google Scholar]
- 32.Stentiford GD, et al. 2016. Microsporidia—emergent pathogens in the global food chain. Trends Parasitol 32: 336–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen J-S, Hsu T-K, Hsu B-M, Huang T-Y, Huang Y-L, Shaio M-F, Ji D-D, 2017. Surveillance of Vittaforma corneae in hot springs by a small-volume procedure. Water Res 118: 208–216. [DOI] [PubMed] [Google Scholar]
- 34.Kakrania R, Joseph J, Vaddavalli PK, Gangopadhyay N, Sharma S, 2005. Microsporidia keratoconjunctivitis in a corneal graft. Eye (Lond) 20: 1314–1315. [DOI] [PubMed] [Google Scholar]
- 35.Tham AC, Sanjay S, 2012. Clinical spectrum of microsporidial keratoconjunctivitis. Clin Exp Ophthalmol 40: 512–518. [DOI] [PubMed] [Google Scholar]
- 36.Fan N-W, Wu C-C, Chen T-L, Yu W-K, Chen C-P, Lee S-M, Lin P-Y, 2012. Microsporidial keratitis in patients with hot springs exposure. J Clin Microbiol 50: 414–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Reddy AK, Balne PK, Garg P, Krishnaiah S, 2011. Is microsporidial keratitis a seasonal infection in India? Clin Microbiol Infect 17: 1114–1116. [DOI] [PubMed] [Google Scholar]
- 38.Vivarès CP, 1999. Les microsporidies: un regain d’intérêt pour ces curieux parasites. Annee Biol 38: 1–16. [Google Scholar]
- 39.Bigliardi E, Sacchi L, 2001. Cell biology and invasion of the microsporidia. Microbes Infect 3: 373–379. [DOI] [PubMed] [Google Scholar]
- 40.Keeling PJ, Fast NM, 2002. Microsporidia: biology and evolution of highly reduced intracellular parasites. Annu Rev Microbiol 56: 93–116. [DOI] [PubMed] [Google Scholar]
- 41.Mietz H, Franzen C, Hoppe T, Bartz-Schmidt KU, 2002. Microsporidia-induced sclerouveitis with retinal detachment. Arch Ophthalmol 120: 864–865. [PubMed] [Google Scholar]
- 42.Yoken J, Forbes B, Maguire AM, Prenner JL, Carpentieri D, 2002. Microsporidial endophthalmitis in a patient with acute myelogenous leukemia. Retina 22: 123–125. [DOI] [PubMed] [Google Scholar]
- 43.Sood AB, Debiec MR, Yeh S, Grossniklaus HE, Randleman JB, 2016. Microsporidial stromal keratitis and endophthalmitis in an immunocompetent patient. J Ophthalmic Inflamm Infect 6: 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ashton N, Wirasinha PA, 1973. Encephalitozoonosis (nosematosis) of the cornea. Br J Ophthalmol 57: 669–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sridhar U, Rahman AAU, Batra J, Sapra N, 2015. Ocular microsporidiosis—our experience in a tertiary care centre in north India. Open J Ophthalmol 5: 130. [Google Scholar]
- 46.Theng J, Chan C, Ling ML, Tan D, 2001. Microsporidial keratoconjunctivitis in a healthy contact lens wearer without human immunodeficiency virus infection. Ophthalmology 108: 976–978. [DOI] [PubMed] [Google Scholar]
- 47.Joseph J, Vemuganti GK, Sharma S, 2005. Microsporidia: emerging ocular pathogens. Indian J Med Microbiol 23: 80–91. [DOI] [PubMed] [Google Scholar]
- 48.Mittal R, Balne PK, Sahu S, Das S, Sharma S, 2017. Coexistence of herpes simplex virus infection in microsporidial stromal keratitis associated with granulomatous inflammation. Indian J Ophthalmol 65: 276–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Franzen C, Müller A, 2001. Microsporidiosis: human diseases and diagnosis. Microbes Infect 3: 389–400. [DOI] [PubMed] [Google Scholar]
- 50.Ghosh K, Schwartz D, Weiss LM, 2014. Laboratory diagnosis of microsporidia. Weiss LM, Becnel JJ, eds. Microsporidia. Chichester, United Kingdom: John Wiley & Sons, Inc., 421–456. [Google Scholar]
- 51.Garcia LS, 2002. Laboratory identification of the microsporidia. J Clin Microbiol 40: 1892–1901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Weber R, Bryan RT, Owen RL, Wilcox CM, Gorelkin L, Visvesvara GS, 1992. Improved light-microscopical detection of microsporidia spores in stool and duodenal aspirates. the enteric opportunistic infections working group. N Engl J Med 326: 161–166. [DOI] [PubMed] [Google Scholar]
- 53.Das S, Sharma S, Sahu SK, Nayak SS, Kar S, 2012. Diagnosis, clinical features and treatment outcome of microsporidial keratoconjunctivitis. Br J Ophthalmol 96: 793–795. [DOI] [PubMed] [Google Scholar]
- 54.Weiss LM, Vossbrinck CR, 1998. Microsporidiosis: molecular and diagnostic aspects. Adv Parasitol 40: 351–395. [DOI] [PubMed] [Google Scholar]
- 55.Notermans DW, Peek R, de Jong MD, Wentink-Bonnema EM, Boom R, van Gool T, 2005. Detection and identification of Enterocytozoon bieneusi and Encephalitozoon species in stool and urine specimens by PCR and differential hybridization. J Clin Microbiol 43: 610–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ghosh K, Weiss LM, 2009. Molecular diagnostic tests for microsporidia. Interdiscip Perspect Infect Dis 2009: 926521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Joseph J, Sharma S, Murthy SI, Krishna PV, Garg P, Nutheti R, Kenneth J, Balasubramanian D, 2006. Microsporidial keratitis in India: 16S rRNA gene-based PCR assay for diagnosis and species identification of microsporidia in clinical samples. Invest Ophthalmol Vis Sci 47: 4468–4473. [DOI] [PubMed] [Google Scholar]
- 58.Costa SF, Weiss LM, 2000. Drug treatment of microsporidiosis. Drug Resist Updat 3: 384–399. [DOI] [PubMed] [Google Scholar]
- 59.Conteas CN, Berlin OG, Ash LR, Pruthi JS, 2000. Therapy for human gastrointestinal microsporidiosis. Am J Trop Med Hyg 63: 121–127. [DOI] [PubMed] [Google Scholar]
- 60.Didier PJ, Phillips JN, Kuebler DJ, Nasr M, Brindley PJ, Stovall ME, Bowers LC, Didier ES, 2006. Antimicrosporidial activities of fumagillin, TNP-470, ovalicin, and ovalicin derivatives in vitro and in vivo. Antimicrob Agents Chemother 50: 2146–2155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Didier ES, Bowers L, Stovall ME, Kuebler D, Mittleider D, Brindley PJ, Didier PJ, 2005. Antimicrosporidial activity of (fluoro)quinolones in vitro and in vivo. Folia Parasitol (Praha) 52: 173–181. [DOI] [PubMed] [Google Scholar]
- 62.Das S, Wallang BS, Sharma S, Bhadange YV, Balne PK, Sahu SK, 2014. The efficacy of corneal debridement in the treatment of microsporidial keratoconjunctivitis: a prospective randomized clinical trial. Am J Ophthalmol 157: 1151–1155. [DOI] [PubMed] [Google Scholar]
- 63.Sharma S, Das S, Joseph J, Vemuganti GK, Murthy S, 2011. Microsporidial keratitis: need for increased awareness. Surv Ophthalmol 56: 1–22. [DOI] [PubMed] [Google Scholar]
- 64.Das S, Sahu SK, Sharma S, Nayak SS, Kar S, 2010. Clinical trial of 0.02% polyhexamethylene biguanide versus placebo in the treatment of microsporidial keratoconjunctivitis. Am J Ophthalmol 150: 110–115.e2. [DOI] [PubMed] [Google Scholar]
- 65.Font RL, Samaha AN, Keener MJ, Chevez-Barrios P, Goosey JD, 2000. Corneal microsporidiosis. report of case, including electron microscopic observations. Ophthalmology 107: 1769–1775. [DOI] [PubMed] [Google Scholar]