Abstract
Background:
Intravenous (IV) oxycodone has been used at induction to prevent an intubation reaction. The aims of the current study were to calculate the median effective dose (ED50) and the 95% effective dose (ED95) of an IV bolus of oxycodone that blunts the hemodynamic response to tracheal intubation with propofol according to gender and to observe the adverse events of induction-dose oxycodone.
Methods:
Adult patients who required general anesthesia and tracheal intubation were enrolled. Tracheal intubation was performed using unified TD-C-IV video laryngoscopy and an ordinary common endotracheal tube. Dixon's up-and-down method was used to obtain ED50 data for women and men separately. The initial dose of oxycodone was 0.2 mg/kg for women and 0.3 mg/kg for men (step size was 0.01 mg/kg). Next, a dose-response curve from the probit analysis was generated to determine the ED50 and ED95 to blunt the intubation reaction in female and male patients. Adverse events following oxycodone injection were observed for 5 min before propofol injection.
Results:
Sixty-three patients were analyzed, including 29 females and 34 males. According to the probit analysis, the ED50 and ED95 of oxycodone required to blunt the intubation reaction in women were 0.254 mg/kg (95% confidence interval [CI], 0.220–0.328 mg/kg) and 0.357 mg/kg (95% CI, 0.297–2.563 mg/kg), respectively. In men, the ED50 and ED95 were 0.324 mg/kg (95% CI, 0.274–0.381 mg/kg) and 0.454 mg/kg (95% CI, 0.384–2.862 mg/kg), respectively. Men required 28% more oxycodone than women for induction (P < 0.01). The most common adverse events were dizziness (87.3%), vertigo (66.7%), sedation (74.6%), and respiratory depression (66.7%).
Conclusions:
Oxycodone can be used for induction to prevent intubation reactions. Gender affected the ED50 and ED95 of oxycodone for blunting the tracheal intubation reaction.
Keywords: Adverse Events, Hemodynamics, Induction, Intubation, Oxycodone
摘要
背景:
静脉注射羟考酮已在临床上用于预防气管插管反应。本研究的目的是计算在联合应用丙泊酚诱导时,不同 性别静脉注射羟考酮抑制气管插管的血流动力学变化的50%有效剂量(ED50)和95%有效剂量(ED95),并观察 应用羟考酮诱导剂量的不良反应。
方法:
研究对象是成人需要全身麻醉和气管插管的患者。气管插管采用统一的TD-C-IV型可视喉镜和普通的气 管插管。应用Dixon's的上下方分别计算男性和女性的ED50。羟考酮的初始剂量为0.2 mg/kg女性和0.3 mg/kg男性 (相邻剂量组梯度为0.01 mg/kg)。男女组各自出现7个阳性到阴性反应交叉点后结束实验,应用probit分析拟合 剂量-效应曲线获取得抑制女性和男性患者气管插管反应的ED50和ED95及和95%可信区间。羟考酮注射5分钟后 静注丙泊酚和罗库溴铵完成诱导,观察5分钟内羟考酮不良反应。
结果:
共有63名患者纳入分析,其中女性29例,男性34例。根据probit分析,羟考酮抑制女性插管反应的ED50和 ED95分别为0.254 mg/kg(95%可信区间[CI],0.220~0.328 mg/kg)和0.357 mg/kg(95% CI,0.297~2.563 mg/kg)。 男性ED50和ED95分别为0.324 mg/kg(95% CI,0.274~0.381 mg/kg)和0.454 mg/kg(95% CI,0.384~2.862 mg/kg) 。男性比女性的羟考酮诱导的ED50> 28%(P<0.01)。最常见的不良反应为眩晕(87.3%)、视物旋转(66.7% )、镇静(74.6%)和呼吸抑制(66.7%)。
结论:
羟考酮可用于诱导,以预防气管插管反应。性别影响羟考酮抑制插管反应的ED50和ED95。
INTRODUCTION
Endotracheal intubation during general anesthesia can cause intubation reactions that manifest as a hemodynamic response (increased blood pressure and heart rate [HR]) by exciting the sympathetic nervous system. Opioids are administered to patients to prevent the occurrence of these hemodynamic changes during intubation.[1,2,3]
Oxycodone is a strong mu-opioid and kappa-opioid receptor agonist that is normally used to control mild and severe pain.[4,5,6] In anesthesia, oxycodone is used at the end of an operation and for patient-controlled anesthesia to prevent pain.[5] The onset time of oxycodone is 2–3 min, and the maximum time is 5–8 min,[6,7] which are similar to the times observed for fentanyl and sufentanil.[8,9,10] The action of oxycodone lasts approximately 4 h, which is similar to morphine, and it effectively reduces pain sensation for patients.[6,11] Because the short onset time of oxycodone is similar to those of fentanyl and sufentanil, which are commonly administered before intubation, and because the long action duration is similar to that of morphine, we speculate that oxycodone can effectively be used during induction to prevent intubation reactions and to minimize pain from an operation. Lee et al.[12] reported that oxycodone prevented pain due to a nasal bone fracture when administered before induction and did not substantially prolong awakening time, which supports our speculation.
Currently, reports suggest that compared with fentanyl, oxycodone can effectively reduce the tracheal intubation reaction and maintain hemodynamic stability.[12,13] However, the effective dose for tracheal intubation is currently calculated according to the requirements for fentanyl. Only one study[14] has determined the optimal dose of intravenous (IV) oxycodone for attenuating hemodynamic changes after endotracheal intubation with thiopental sodium. Because females reportedly require less opioids than males,[15] we hypothesized that the oxycodone required to blunt the hemodynamic response to tracheal intubation is affected by gender.
In this prospective study, we aimed to determine (1) the median effective dose (ED50) and the 95% effective dose (ED95) of an IV bolus of oxycodone that blunts the hemodynamic response to tracheal intubation with propofol according to gender and (2) the adverse events associated with induction-dose oxycodone.
METHODS
Ethical approval
This study was approved by the Ethics Committee of the First Affiliated Hospital, College of Medicine, Zhejiang University (2016-383, Hangzhou, China) on September 6, 2016, and was registered with the Chinese Clinical Trial Registry (ChiCTR-opc-16009175) on September 8, 2016. Written informed consent was obtained from all patients.
Participants
All patients who required general anesthesia and tracheal intubation were enrolled in this study. We included adult patients (18–64 years) who were classified as Class I or II according to the American Society of Anesthesiologists. Patients were excluded if they (1) had a body mass index >30 kg/m2 or ≤18.4 kg/m2, (2) had a severe cardiovascular or respiratory disease, (3) had a history of difficult intubation, a potentially difficult airway, or received intubation twice during the study, (4) had renal, liver, or hematological disorders, (5) were at a high risk for aspiration or regurgitation, or (6) were taking narcotics for chronic pain or beta blockers for cardiovascular disease.
All patients were informed about the purpose of the study and the anesthesia procedure, including induction and awakening.
Introduction and anesthetic management
All patients were transferred to the operating room without premedication. After the patients were in the supine position on the operating table, they inhaled oxygen at 3 L/min through a face mask and a 16–18 G indwelling catheter was placed within the antecubital or wrist vein. Pulse oximetry (SPO2), electrocardiography, noninvasive blood pressure (NBP), and bispectral index (BIS) were applied to monitor the patients. All patients were instructed to close their mouth and breathe through their nose. A small catheter was inserted into the nasal cavity to measure the end-tidal carbon dioxide partial pressure (Et CO2) and the spontaneous respiratory rate (RR). After a 5-min period of stabilization, NBP and HR were measured twice, and the mean values were used as the baseline (T0). Baseline Et CO2, RR, and BIS were also recorded.
During oxygen inhalation, all patients were quickly injected with an IV bolus of oxycodone in normal saline 5 min before induction with propofol (2 mg/kg) and rocuronium (0.8 mg/kg). During these 5 min, any adverse events that occurred before esthetic induction were recorded, such as dizziness, vertigo, cough, nausea, sedation, and respiratory depression. Systolic blood pressure (SBP), diastolic blood pressure (DBP), HR, RR, Et CO2, and BIS were simultaneously recorded at 1 min (T1), 3 min (T2), and 5 min (T3) after the injection of oxycodone. All patients were asked about pain when propofol and rocuronium were quickly injected and were then observed for pain reactions (hands or arm withdrawal movements). In this study, sedation was defined as the patient experiencing drowsiness or the patient involuntarily closing the eyes. Respiratory depression was defined as a decrease in RR (RR <10 beats/min).
Tracheal intubation was performed approximately 2 min after induction (7 min after the injection of oxycodone) using a unified videolaryngoscopy (TD-C-IV, Zhejiang Yu Yi Medical Equipment Co., Ltd., China) and an ordinary common endotracheal tube. The intubations were performed by two experienced attending anesthesiologists using a highly similar procedure. Patients were excluded from this study if the anesthesiologist could not perform the intubation on the first attempt. Hemodynamic responses to tracheal intubation within 3 min as observed by NBP and HR monitoring were measured at 1-min intervals. An assistant anesthesiologist recorded NBP and HR at the moment of intubation and at 1 min and 3 min after tracheal intubation. In this study, the definition of no intubation reaction (blunted hemodynamic response) included SBP/DBP and HR increases of <20% of the baseline values. Otherwise, the response was defined as an intubation reaction. General anesthesia was maintained by continuous infusion of propofol to keep the BIS within 40–60.
A total of 0.5 mg of atropine was administered via IV when severe bradycardia occurred (HR <50 beats/min); 6 mg ephedrine was administered for events of hypotension (SBP <90 mmHg); and 10 mg Ebrantil was administered via IV for events of hypertension (SBP ≥30% of the baseline value). Concurrent hypertension and tachycardia were treated with esmolol or additional propofol or oxycodone when the anesthesiologist questioned the adequacy of the anesthesia amount.
Median effective dose measurement
The dose of oxycodone was determined by the modified Dixon's up-and-down method. Because gender may affect dose, the study was performed according to the gender. The dose of oxycodone in women was started at 0.2 mg/kg, which was used in a previous report.[12,13] The dose was increased by 0.01 mg/kg for the next patient if the patient exhibited an intubation reaction. Otherwise, the dose of oxycodone was decreased by 0.01 mg/kg for the next patient. The initial dose in men was 0.30 mg/kg (higher than that in women).
The number of patients was based on the Dixon's up-and-down method. This method requires at least six crossover points (no intubation reaction to intubation reaction).[16,17,18] This study was conducted until the collection of seven crossover points each in women and men was achieved. No intubation reaction was defined as SBP/DBP and HR increases <20% of the baseline values within 3 min of intubation.
Statistical analysis
Statistical analyses were performed using SPSS version 22.0 (IBM, Armonk, NY, USA). Continuous variables were checked for normal distribution using the Shapiro-Wilk test. Data are presented as the number or mean ± standard deviation for a normal distribution or as the median (interquartile range) for nonnormal distributions. Parametric data were compared using the t-test, and nonparametric data were analyzed with the Mann-Whitney U-test. Descriptive variables were analyzed by the Chi-squaretest or Fisher's exact test. A probit analysis was performed to calculate the ED50 and ED95 from the Dixon's up-and-down method data, and the results are presented as medians (95% confidence interval [CI]); Pearson's Chi-squared test was used to evaluate goodness-of-fit (P > 0.05 indicate good fit). Differences were considered statistically significant if P < 0.05 (two-tailed).
RESULTS
A total of 29 female and 36 male patients were enrolled in this study until seven crossover points were achieved. Two male patients were excluded from this study because of severe hypertension after the injection of oxycodone. Therefore, 29 females and 34 males were ultimately included in the final analyses.
Demographic data and induction profiles are shown in Table 1. NBP and HR changes remained mainly within the clinical range. BIS decreased after oxycodone injection, but most patients maintained consciousness or sedation, with BIS values higher than 80. The adverse events following oxycodone injection are shown in Table 2. Most patients maintained an SPO2 higher than 92% with mask oxygen inhalation, even during respiratory depression. Six patients exhibited SPO2 decreases to 92% due to sedation and respiratory depression. No patient had hypotension after oxycodone injection before induction. Only two patients exhibited hypotension after propofol induction. Furthermore, no patient exhibited hypotension and bradycardia after intubation. The sequences of no intubation reaction and intubation reaction are shown in Figure 1. The formula of the Dixon's up-and-down method[18,19] showed that the ED50 of oxycodone required to blunt the tracheal intubation reaction in women was 0.252 mg/kg (95% CI, 0.220–0.284 mg/kg), and in men, the ED50 was 0.324 mg/kg (95% CI, 0.289–0.360 mg/kg; P < 0.001). A dose-response curve from the probit analysis of the oxycodone dose and the probability of no intubation reaction are shown in Figure 2. The ED50 and ED95 of oxycodone required to blunt the intubation reaction in women were 0.254 mg/kg (95% CI, 0.220–0.328 mg/kg) and 0.357 mg/kg (95% CI, 0.297–2.563 mg/kg), respectively. In men, the ED50 and ED95 were 0.324 mg/kg (95% CI, 0.274–0.381 mg/kg) and 0.454 mg/kg (95% CI, 0.384–2.862 mg/kg), respectively (Pearson's Chi-squared goodness-of-fit, χ2= 13.615 and P = 0.694). Men required 28% more oxycodone than women for induction (P < 0.01).
Table 1.
Demographic data and induction profiles
| Variables | Total (n = 63) | Women (n = 29) | Men (n = 34) | t | P |
|---|---|---|---|---|---|
| Age (years) | 43.8 ± 11.8 | 41.0 ± 11.3 | 46.1 ± 11.9 | −1.744 | 0.086 |
| Weight (kg) | 61.4 ± 10.9 | 56.0 ± 8.1 | 69.3 ± 9.0 | −6.153 | <0.001 |
| Height (cm) | 164.0 ± 6.9 | 160.0 ± 4.9 | 170.5 ± 4.7 | −8.229 | <0.001 |
| Oxycodone (mg/kg) | 0.29 ± 0.05 | 0.25 ± 0.02 | 0.32 ± 0.02 | −12.960 | <0.001 |
Data are presented as mean ± SD. SD: Standard deviation.
Table 2.
Adverse events after oxycodone injection before induction
| Adverse events | Total (n = 63) | Women (n = 29) | Men (n = 34) | χ2 | P |
|---|---|---|---|---|---|
| Dizziness | 55 (87.3) | 26 (89.7) | 29 (85.3) | 0.269 | 0.604 |
| Vertigo | 42 (66.7) | 24 (82.8) | 18 (52.9) | 6.262 | 0.012 |
| Cough | 5 (7.9) | 3 (10.3) | 2 (5.9) | 0.427 | 0.514 |
| Nausea | 4 (6.3) | 1 (3.4) | 3 (8.8) | 0.761 | 0.383 |
| Sedation | 47 (74.6) | 27 (93.1) | 20 (58.8) | 9.707 | 0.002 |
| Respiratory depression | 42 (66.7) | 17 (58.6) | 25 (73.5) | 1.565 | 0.211 |
| Chest tightness | 2 (3.2) | 0 | 2 (5.9) | 1.762 | 0.184 |
| Chest rigidity | 0 | 0 | 0 | ||
| Hypotension | 0 | 0 | 0 |
Data are presented as n (%); Sedation: Patient feels drowsy or involuntarily closes the eyes; Respiratory depression: Respiratory rate <10 beats/min.
Figure 1.
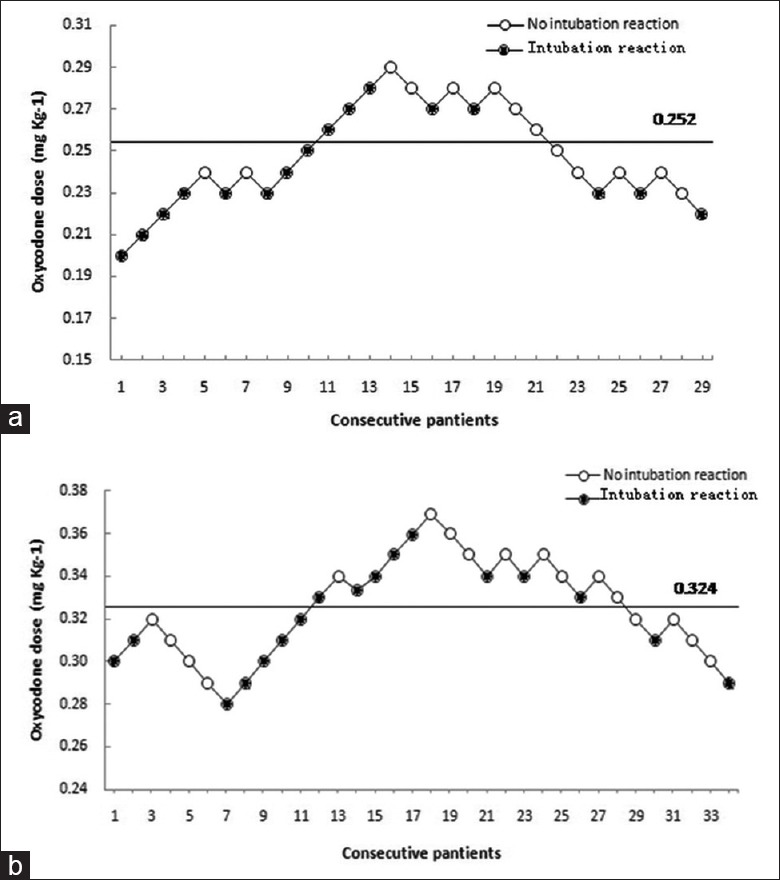
The dose of oxycodone in all consecutive patients for tracheal intubation. The ED50 of oxycodone required to blunt the tracheal intubation reaction in women and men as determined by the up-and-down method is shown in a and b, respectively. The response of each patient is represented with a white or black circle. ED50: Median effective dose.
Figure 2.
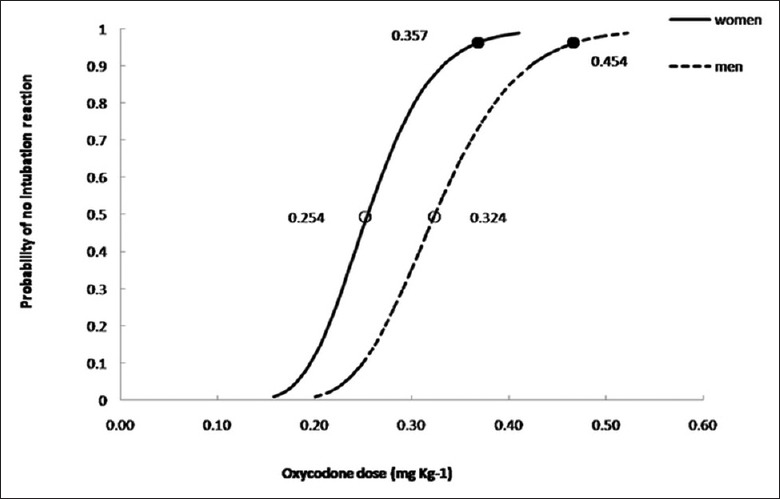
Dose-response curve for oxycodone plotted from the probit analyses of individual doses and no intubation reaction. The white circles represent the 50% probabilities and the black circles represent the 95% probabilities in women and men. The oxycodone doses are marked beside each circle.
Eight patients (8/63, 12.7%) felt pain with propofol and rocuronium injection, but none of these patients withdrew their arms.
DISCUSSION
Oxycodone is an opioid drug that can be used for tracheal intubation. This study aimed to evaluate the ED50 and ED95 of oxycodone for blunting the hemodynamic response to tracheal intubation and the safety of a large-dose injection of oxycodone.
The ED50 and ED95 of oxycodone required to blunt the intubation reaction were 0.254 mg/kg and 0.357 mg/kg, respectively, in women and 0.324 mg/kg and 0.454 mg/kg, respectively, in men. Gender affected the ED50 and ED95 of oxycodone required for blunting the intubation reaction. During the 5-min observation after the quick oxycodone injection, there were no severe adverse events, such as chest rigidity, difficulty breathing, or cyanosis. Blood pressure and HR changed after oxycodone injection, but mainly remained within the clinical range, except for two patients who experienced very severe hypertension and were excluded from the study.
The observation of gender effects on the dose of oxycodone required for blunting the hemodynamic response of tracheal intubation is interesting. Female patients require a lower dose of oxycodone (ED50=0.254 mg/kg) than male patients (ED50=0.324 mg/kg) for tracheal intubation. The finding that men require approximately 28% more oxycodone than women in this study is similar to previous studies that showed that men required 30–40% more morphine[15] and approximately 30% more oxycodone[20] than women for pain relief. This difference may be caused by higher oxycodone concentrations in women[6] or men may be less sensitive than women to opioids (men require higher doses to relieve similar pain).[20] Men and women differ in their pain tolerance and in their blood concentration of oxycodone; the pharmacokinetics and pharmacokinetics were affected by gender. One study reported that females are more sensitive than males to opioid receptor agonists.[16] Furthermore, females may experience respiratory depression and other adverse effects more easily if they are given the same dose as males. In a study of kappa-opioids, the authors also found that kappa-opioid analgesia was greater in females than in males.[21] Multiple mechanisms likely contribute to sex differences in opioid analgesia, including gonadal hormonal effects, pharmacokinetics and pharmacodynamics, genetic influences, balance of analgesic/antianalgesic processes, and psychological factors.[22] In this study, we have only just begun to explore the induction dosages of oxycodone and the effect of gender on the ED50 and ED95 of oxycodone for tracheal intubation.
The dose of oxycodone required for tracheal intubation in this study is higher than previous reports of oxycodone.[12,13,14] However, the standards utilized in this study differed from those in previous reports. In the present study, we defined hemodynamic stability as SBP/DBP and HR increases of <20% of the baseline values. In previous reports,[12,13] the authors observed the mean blood pressure (MBP) and HR and defined unstable hemodynamics as MBP increases of >40% and HR increases of >20%. One report[14] found the ED50 and ED95 of oxycodone for tracheal intubation with thiopental sodium and sevoflurane and defined unstable hemodynamics as SBP or MBP increases of >15% and a HR increase at the study dose. As the previous report indicated, more opioid was required to block the increase in HR than to block the blood pressure increase.[23] Therefore, the restrictive standards for an intubation reaction in this study led to the requirement for more oxycodone.
Oxycodone injection can effectively maintain hemodynamic stability.[6,24] The changes were stable and within a clinical range (<20%). Only two male patients experienced very severe hypertension after oxycodone injection and were excluded from this study. One of these patients was 59 years old, and his SBP/DBP increased from 145/76 mmHg to 240/100 mmHg and his HR increased from 95 to 140 at 3 min after injection. The other patient was 35 years old, and his SBP/DBP increased from 190/100 mmHg to 247/124 mmHg and his HR increased from 94 to 110 at 5 min after injection. The first patient was given 40 mg of esmolol and the second patient was treated with propofol. After the treatments, the patients regained normal hemodynamics and remained stable throughout general anesthesia. These two patients did not present with hypertension histories and did not have any routine drug intake. Thus, we questioned whether these reactions were caused by undiagnosed hypertension, anxiety, or the quick oxycodone injection. Because these reactions affected the hemodynamic analysis, these two patients were excluded. The most commonly reported cardiovascular adverse events associated with oxycodone are hypotension and bradycardia. In this study, hypotension and bradycardia were not evident within 5 min of oxycodone injection, but two patients (3%) experienced hypotension after propofol injection before tracheal intubation, which differs from another study that reported that a small dose of oxycodone with 0.2 mg/kg propofol caused hypotension.[14]
We designed the quick injection of oxycodone to coincide with the time point of adverse events to evaluate any severe adverse events in relation to oxycodone safety. During the 5-min observation before induction with propofol, some adverse events were observed. The four most common adverse events were dizziness (87.3%), vertigo (66.7%), sedation (74.6%), and respiratory depression (66.7%). Four (6.3%) patients reported slight nausea without vomiting. Five (7.9%) patients coughed to varying extents. Two men felt chest wall tightness, but maintained spontaneous breathing and stable vital signs without any treatment. Dizziness was similar to another report on oxycodone injection in Chinese patients[24] and Koreans.[12] Nausea was less frequently observed in this study than in other reports,[24] perhaps because of the short observation time (only 5 min).
Sedation and respiratory depression are common adverse events associated with opioids, and anesthesiologists pay close attention to severe adverse events or death. In this study, sedation (74.6%) was defined as drowsiness or if the anesthesiologist observed that the patient involuntarily closed their eyes. Respiratory depression (66.7%) was defined as a decrease in RR (RR <10 beats/min). Even with the high rate of sedation and RR depression, most patients maintained an SPO2 level higher than 92% with mask oxygen inhalation. Only six patients exhibited SPO2 decreases to 92%, which could be transiently treated by calling the patient's name and asking the patient to breathe deeply to maintain a normal SPO2. Although a very quick injection and a large dose of oxycodone may lead to a higher rate of more serious adverse events, no severe adverse events, such as chest rigidity, difficulty breathing, or cyanosis, occurred in this study. Therefore, a normal dose and slow injection of oxycodone for pain control is safe.
Propofol and rocuronium injection pain is very common in the clinical setting, and anesthesiologists encounter it every day. The injection pain can be treated with local anesthetic, central sedative/analgesic drugs, or rapid injection into a large vein.[25,26,27] Eight (12.7%) patients felt slight pain from the propofol/rocuronium injection, but no patients exhibited arm withdrawal movements; this value is less than those in other reports.[26,27] Thus, we conclude that oxycodone effectively prevented pain from propofol and rocuronium injection.
This study has several limitations. First, the Dixon's up-and-down method design of this study focused on the oxycodone induction dose and hemodynamic responses (no intubation reaction and intubation reaction). We could not compare the hemodynamic response of intubation with fentanyl, which we normally use for induction. Second, this study focused on intubation reactions, and we selected patients who required tracheal intubation without limiting the type of operation. Third, although we observed adverse events from oxycodone injection, the time was short (only 5 min), which is not representative of all adverse events associated with oxycodone. Finally, oxycodone caused slight coughing and prevented pain from propofol and rocuronium injection, but we did not compare it with other opioids.
In conclusion, the ED50 and ED95 of oxycodone required to blunt the tracheal intubation reaction in women were 0.254 mg/kg and 0.357 mg/kg, respectively, and in men, these values were 0.324 mg/kg and 0.454 mg/kg, respectively. Oxycodone is safe for tracheal intubation, and men require a higher dose of oxycodone than women.
Financial support and sponsorship
This work was supported by grants from the Zhejiang Provincial Medical and Health (Nos. 2016KYB104, 2015KYB118 and 2014KYB082), Zhejiang, China.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
All authors would like to thank Duo Lyu, MD (Statistician, Institute of Clinical Trials, the First Affiliated Hospital, College of Medicine, Zhejiang University).
Footnotes
Edited by: Li-Shao Guo
REFERENCES
- 1.Sameenakousar, Mahesh, Srinivasan KV. Comparison of fentanyl and clonidine for attenuation of the haemodynamic response to laryngocopy and endotracheal intubation. J Clin Diagn Res. 2013;7:106–11. doi: 10.7860/JCDR/2012/4988.2682. doi: 10.7860/JCDR/2012/4988.2682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Safavi M, Honarmand A. Attenuation of cardiovascular responses to laryngoscopy and tracheal intubation – Intravenous sufentanil vs.pethidine. Middle East J Anaesthesiol. 2008;19:1349–59. [PubMed] [Google Scholar]
- 3.Casati A, Fanelli G, Albertin A, Deni F, Danelli G, Grifoni F, et al. Small doses of remifentanil or sufentanil for blunting cardiovascular changes induced by tracheal intubation: A double-blind comparison. Eur J Anaesthesiol. 2001;18:108–12. doi: 10.1046/j.1365-2346.2001.0790e.x. doi: 10.1097/00003643-200102000-00008. [DOI] [PubMed] [Google Scholar]
- 4.King SJ, Reid C, Forbes K, Hanks G. A systematic review of oxycodone in the management of cancer pain. Palliat Med. 2011;25:454–70. doi: 10.1177/0269216311401948. doi: 10.1177/0269216311401948. [DOI] [PubMed] [Google Scholar]
- 5.Riley J, Eisenberg E, Müller-Schwefe G, Drewes AM, Arendt-Nielsen L. Oxycodone: A review of its use in the management of pain. Curr Med Res Opin. 2008;24:175–92. doi: 10.1185/030079908x253708. doi: 10.1185/030079908X253708. [DOI] [PubMed] [Google Scholar]
- 6.Xu JG. The pharmacology and clinical application of hydrochloride oxycodone (in Chinese) J Clin Anesthesiology. 2014;30:511–3. [Google Scholar]
- 7.Leow KP, Cramond T, Smith MT. Pharmacokinetics and pharmacodynamics of oxycodone when given intravenously and rectally to adult patients with cancer pain. Anesth Analg. 1995;80:296–302. doi: 10.1097/00000539-199502000-00016. doi: 10.1097/00000539-199502000-00016. [DOI] [PubMed] [Google Scholar]
- 8.Hwang BY, Kwon JY, Kim E, Lee DW, Kim TK, Kim HK, et al. Oxycodone vs. Fentanyl patient-controlled analgesia after laparoscopic cholecystectomy. Int J Med Sci. 2014;11:658–62. doi: 10.7150/ijms.8331. doi: 10.7150/ijms.8331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lenz H, Sandvik L, Qvigstad E, Bjerkelund CE, Raeder J. A comparison of intravenous oxycodone and intravenous morphine in patient-controlled postoperative analgesia after laparoscopic hysterectomy. Anesth Analg. 2009;109:1279–83. doi: 10.1213/ane.0b013e3181b0f0bb. doi: 10.1213/ane.0b013e3181b0f0bb. [DOI] [PubMed] [Google Scholar]
- 10.Mitra S, Carlyle D, Kodumudi G, Kodumudi V, Vadivelu N. New advances in acute postoperative pain management. Curr Pain Headache Rep. 2018;22:35. doi: 10.1007/s11916-018-0690-8. doi: 10.1007/s11916-018-0690-8. [DOI] [PubMed] [Google Scholar]
- 11.Smith MT, Edwards SR, Nielsen CK. Oxycodone's mechanism of action and potency differences after spinal and systemic routes of administration. Anesthesiology. 2007;106:1063–4. doi: 10.1097/01.anes.0000265176.75372.ed. doi: 10.1097/01.anes.0000265176.75372.ed. [DOI] [PubMed] [Google Scholar]
- 12.Lee YS, Baek CW, Kim DR, Kang H, Choi GJ, Park YH, et al. Comparison of hemodynamic response to tracheal intubation and postoperative pain in patients undergoing closed reduction of nasal bone fracture under general anesthesia: A randomized controlled trial comparing fentanyl and oxycodone. BMC Anesthesiol. 2016;16:115. doi: 10.1186/s12871-016-0279-x. doi: 10.1186/s12871-016-0279-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Park KB, Ann J, Lee H. Effects of different dosages of oxycodone and fentanyl on the hemodynamic changes during intubation. Saudi Med J. 2016;37:847–52. doi: 10.15537/smj.2016.8.14822. doi: 10.15537/smj.2016.8.14822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Park YH, Lee SH, Lee OH, Kang H, Shin HY, Baek CW, et al. Optimal dose of intravenous oxycodone for attenuating hemodynamic changes after endotracheal intubation in healthy patients: A randomized controlled trial. Medicine (Baltimore) 2017;96:e6234. doi: 10.1097/MD.0000000000006234. doi: 10.1097/MD.0000000000006234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pleym H, Spigset O, Kharasch ED, Dale O. Gender differences in drug effects: Implications for anesthesiologists. Acta Anaesthesiol Scand. 2003;47:241–59. doi: 10.1034/j.1399-6576.2003.00036.x. doi: 10.1034/j.1399-6576.2003.00036.x. [DOI] [PubMed] [Google Scholar]
- 16.Dixon WJ. Staircase bioassay: The up-and-down method. Neurosci Biobehav Rev. 1991;15:47–50. doi: 10.1016/s0149-7634(05)80090-9. doi: 10.1016/S0149-7634(05)80090-9. [DOI] [PubMed] [Google Scholar]
- 17.Lu W, Ramsay JG, Bailey JM. Reliability of pharmacodynamic analysis by logistic regression: Mixed-effects modeling. Anesthesiology. 2003;99:1255–62. doi: 10.1097/00000542-200312000-00005. doi: 10.1097/00000542-200312000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Sun RY. Quantitative Pharmacology. Beijing: People's Healthy Publisher; 1987. pp. 203–19. [Google Scholar]
- 19.Li Y, Zhu S, Bao F, Xu J, Yan X, Jin X, et al. The effects of age on the median effective concentration of ropivacaine for motor blockade after epidural anesthesia with ropivacaine. Anesth Analg. 2006;102:1847–50. doi: 10.1213/01.ane.0000215999.60513.da. doi: 10.1213/01.ane.0000215999.60513.da. [DOI] [PubMed] [Google Scholar]
- 20.Andreassen TN, Klepstad P, Davies A, Bjordal K, Lundström S, Kaasa S, et al. Influences on the pharmacokinetics of oxycodone: A multicentre cross-sectional study in 439 adult cancer patients. Eur J Clin Pharmacol. 2011;67:493–506. doi: 10.1007/s00228-010-0948-5. doi: 10.1007/s00228-010-0948-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gear RW, Miaskowski C, Gordon NC, Paul SM, Heller PH, Levine JD, et al. Kappa-opioids produce significantly greater analgesia in women than in men. Nat Med. 1996;2:1248–50. doi: 10.1038/nm1196-1248. doi: 10.1038/Nm1196-1248. [DOI] [PubMed] [Google Scholar]
- 22.Fillingim RB, Gear RW. Sex differences in opioid analgesia: Clinical and experimental findings. Eur J Pain. 2004;8:413–25. doi: 10.1016/j.ejpain.2004.01.007. doi: 10.1016/j.ejpain.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 23.Channaiah VB, Chary K, Vlk JL, Wang Y, Chandra SB. Low-dose fentanyl: Hemodynamic response to endotracheal intubation in normotensive patients. Arch Med Sci. 2008;4:293–9. [Google Scholar]
- 24.Hao GT, Zhou HY, Gao HZ, Qu HY, Liang YG, Li YY, et al. Pharmacokinetics of oxycodone hydrochloride and three of its metabolites after intravenous administration in Chinese patients with pain. Pharmacol Rep. 2014;66:153–8. doi: 10.1016/j.pharep.2013.08.012. doi: 10.1016/j.pharep.2013.08.012. [DOI] [PubMed] [Google Scholar]
- 25.Desousa KA. Pain on propofol injection: Causes and remedies. Indian J Pharmacol. 2016;48:617–23. doi: 10.4103/0253-7613.194845. doi: 10.4103/0253-7613.194845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ayoǧlu H, Altunkaya H, Ozer Y, Yapakçi O, Cukdar G, Ozkoçak I, et al. Does dexmedetomidine reduce the injection pain due to propofol and rocuronium? Eur J Anaesthesiol. 2007;24:541–5. doi: 10.1017/S0265021506002250. doi: 10.1017/S0265021506002250. [DOI] [PubMed] [Google Scholar]
- 27.Lu Y, Ye Z, Wong GT, Dong C, Yu J. Prevention of injection pain due to propofol by dezocine: A comparison with lidocaine. Indian J Pharmacol. 2013;45:619–21. doi: 10.4103/0253-7613.121376. doi: 10.4103/0253-7613.121376. [DOI] [PMC free article] [PubMed] [Google Scholar]


