Abstract
Background
HIV/AIDS continues to be a health disparity faced by sexual minority men, and is exacerbated by non-injection drug use.
Objectives
We sought to delineate growth in non-injection drug use and condomless sex in a sample of racially and economically diverse of gay, bisexual, and other young men who have sex with men (YMSM) as they emerged into adulthood between the ages of 18 and 21 and who came of age in the post-HAART era.
Methods
Behavioral data on drug use and condomless sex, collected via a calendar based technique over 7 waves of a cohort study of 600 YMSM, were analyzed using latent growth curve modeling to document patterns of growth in these behaviors, their associations, and the extent to which patterns and associations are moderated by race/ethnicity and socioeconomic status.
Results
Significant growth was noted in the frequencies of condomless oral and anal intercourse, alcohol to intoxication, marijuana use, and inhalant nitrate use. High levels of association were noted between all behaviors across time but associations did not differ by either race/ethnicity or socioeconomic status. The link between drug use and risky sexual behavior continue to be evident in YMSM with significant increases in these behaviors demonstrated as YMSM transition between adolescence and young adulthood.
Conclusions/Importance
Healthcare for a new generation of sexual minority males must address the synergy of these behaviors and also nest HIV prevention and care within a larger context of sexual minority health that acknowledges the advances made in the last three decades.
Keywords: drug use, condomless sex, HIV, sexual minority, YMSM, latent growth curve modeling, longitudinal, cohort study
Alcohol and other drug use is prevalent among young gay, bisexual, and other young men who have sex with men (YMSM) (Halkitis et al., 2011; Newcomb, Ryan, Greene, Garofalo, & Mustanski, 2014; Outlaw et al., 2011; Wong, Schrager, Chou, Weiss, & Kipke, 2013) and is associated with sexual behaviors that place YMSM at risk for sexually transmitted infections (STIs), including HIV (Mustanski, Newcomb, Du Bois, Garcia, & Grov, 2011; Newcomb & Mustanski, 2014). In the United States, sexual minority young men are disproportionately affected by HIV (Centers for Disease Control & Prevention (CDC), 2016), and non-injection drug use has been associated with HIV transmission in this population throughout the history of the disease (Halkitis et al., 2011; Pollock et al., 2012). Moreover, the management of HIV has changed drastically over the last three decades (Beyrer et al., 2012; Lansky et al., 2010), and the meaning of HIV in the lives of young sexual minority men may be different than for those who came of age at the height of the epidemic in the 1980’s and 1990’s in the pre-HAART (Highly Active Antiretroviral Therapy) era (Kingdon et al., 2013; Moeller, Halkitis, Pollock, Siconolfi, & Barton, 2013). Thus, understanding how drug use is associated with sexual risk behaviors over time in a generation of YMSM who came of age post-HAART may provide valuable insight seeking to inform future prevention efforts (Kingdon et al., 2013).
YMSM appear to engage in more instances of substance use and sexual risk behaviors as they age (Perry N Halkitis et al., 2014; Kapadia, Bub, Barton, Stults, & Halkitis, 2015; Newcomb & Mustanski, 2014; Newcomb et al., 2014). Investigating these changes and their associations over time may provide particularly useful information regarding the health-related risks of YMSM during emerging adulthood, a period marked by rapid physical and psychological maturation (Arnett, 2000). Increased impulsivity and psychosocial stressors, including the potential challenges of coming out and negotiating a stigmatized sexual identity, make emerging adulthood an acutely vulnerable developmental stage for YMSM (Halkitis, Kapadia, Bub, et al., 2015). Additionally, increased substance use and sexual risk behaviors may be associated with myriad health-related concerns, including depression (Perdue, Hagan, Thiede, & Valleroy, 2003; Salomon et al., 2009) and intimate partner violence (Stults, Javdani, Greenbaum, Kapadia, & Halkitis, 2015, 2016; Wong, Weiss, Ayala, & Kipke, 2010). We need to examine these dynamic and evolving behaviors over time to understand how they may relate to poor health outcomes in this new generation of YMSM, defined as the generation of Millennials who came of age in the post HAART-era.
In the literature, researchers have noted significant differences in the level of drug use and sexual risk behaviors among YMSM by race/ethnicity and socioeconomic status (SES). White and upper-SES YMSM report greater frequency of substance use and condomless sex behaviors as compared to their non-White, lower-SES counterparts as noted in a meta-analysis of MSM (Millett, Flores, Peterson, & Bakeman, 2007), in samples of MSM across ages (Sullivan et al., 2014) where 74.6% of the Black MSM and 60.8% of the White MSM were below age 30. This is also supported in other studies MSM (64% age 34 and under) (Magnus et al., 2010) and of YMSM (Halkitis & Pérez Figueroa, 2010), where the mean age of the participants was 18. These differences point to heterogeneity within the population and the need to further examine potential differences by race/ethnicity and SES in behavioral patterns as YMSM emerge into adulthood. However, there is limited information on the extent to which change in these behaviors over time vary by both race/ethnicity and SES in a new generation of YMSM as they emerge into adulthood.
The extant literature is limited in several ways. First, most studies utilize cross-sectional designs that cannot observe developmental patterns in drug use, sexual risk behaviors, or their associations (Carey et al., 2009; Kecojevic, Silva, Sell, & Lankenau, 2015; Newcomb & Mustanski, 2014). This is problematic, as these behaviors are dynamic and evolve over time, limiting our ability to examine either temporal associations or the development of these behaviors across time (Carey et al., 2009; Ellen et al., 2015; Mustanski, Garofalo, Herrick, & Donenberg, 2007; Parsons, Grov, & Golub, 2012). Second, studies employing longitudinal designs typically use samples comprised of older adult men who have sex with men (MSM) or youth where sexual minorities are only a small proportion of the overall sample (Perry N Halkitis et al., 2014), thereby diluting any understanding of these phenomena in young men generally, and in those who came of age after the first two decades of AIDS when treatments were available. Third, the few studies that examine changes in drug use and sexual risk behaviors over time do not account for potential differences by race/ethnicity and SES (Colfax et al., 2005; Halkitis, Mukherjee, & Palamar, 2009). YMSM is not a monolithic group, and failure to account for such differences limits our understanding of how important sociodemographic factors may be in explaining changes in these dynamic behaviors. Finally, to our knowledge, no other studies of YMSM examine whether race/ethnicity and SES moderate the longitudinal associations between drug use and sexual risk behaviors. This is an area of ongoing concern, as YMSM continue to be at risk for HIV infection and other health disparities disproportionately experienced by sexual minority men (Institute of Medicine, 2011; Wolitski, Stall, & Valdiserri, 2008).
To address gaps in the extant literature, the present study seeks to model changes in drug use, sexual risk behaviors, and their association over time, while controlling for differences in race/ethnicity and SES. Specifically, during a stage of human development when we would expect increases in both sets of behaviors, we sought to examine the pattern that emerges for YMSM and whether drug use and sexual risk behaviors are related over time.
Methods
Study design
Data for this analysis are derived from the Project 18 (P18) Cohort Study, a prospective study of YMSM residing in the New York City metropolitan area. The purpose of this study is to understand emergence of a syndemic (i.e, the confluence of health issues as directed by psychosocial burdens) (Halkitis, Wolitski, & Millett, 2013) in a generation of racially/ethnically and socioeconomically diverse YMSM who came of age in the 21st century. Study details and methodology for this project have been described previously (Halkitis et al., 2013). Participants were recruited into this study between May, 2009 and June, 2011 using both active and passive recruitment techniques. Eligible participants were between 18–19 years old, biologically male, reporting sex with another man in the past six months, and self-reporting an HIV negative serostatus. Those deemed eligible provided written, informed consent.
Data on recent sexual and drug use behaviors were ascertained via an interviewer-administered, calendar-based approach methodology known as the Timeline Followback (TLFB). These are the data we present in the ensuing analyses (Robinson, Sobell, Sobell, & Leo, 2014; Sobell, Brown, Leo, & Sobell, 1996). These data were collected for the month prior to the assessment. Participants took part in seven study visits (baseline, 6-, 12-, 18-, 24-, 30-, and 36-months post-baseline), and thus those who took part in all seven waves, completed the TLFB at each assessment. Those who relocated from New York City only completed a computer-administered survey while those who completed the assessment in person completed the surveys and the TLFB. Consequently, our data source is based on those in person assessments. Data from all seven waves are included in the present analysis. The New York University Institutional Review Board approved the study protocol, and the study holds a federal certificate of confidentiality.
Measures
Demographic Characteristics
Participants self-reported race/ethnicity and perceived familial socioeconomic status (SES) at the baseline assessment. Perceived familial socioeconomic status was measured via a 5-point Likert scale (lower, lower middle, middle, upper middle, upper), which was categorized as lower, middle (lower middle, middle and upper middle), and upper perceived familial SES. Specifically the participants were asked “What do you perceive to be the economic class of the people who raised you?” Perceived familial SES was used instead of income as this measure has been shown to be a strong indicator of health in adolescents, with those of higher perceived SES demonstrating better health (Goodman, Huang, Schafer-Kalkhoff, & Adler, 2007). Moreover since participants are age 18 when they are asked this questions and likely not earning their own income nor necessarily are aware of the income of their parents, and as has been shown, measures of SES are fraught with complexities in heath disparities research because of “lack of precision and reliability of measures; difficulty with the collection of individual SES data; the dynamic nature of SES over a lifetime; the classification of women, children, retired and unemployed persons; lack of or poor correlation between individual SES measures” (Shavers, 2007), much of which would also manifest in our sample. Thus, we also utilized perceived familial SES as proxy indicator. The measures is based on the work of the MacArthur Research Network on Socioeconomic SES and Health (2009) and has been shown to be highly associated with other indicators of SES and particularly useful in young Black populations (Longmire-Avital & Miller-Duce, 2015). Moreover, as supported by Goodman et al. (2007) perceived SES is complex constructed and is informed by a variety of social factors, including age, race, and objective SES. Such an understanding of SES was more highly aligned with the underlying premises of our study.
Alcohol to Intoxication and Other Drug Use
Participant non-injection drug use behaviors during the 30 days preceding interview were obtained using the TLFB (Sobell et al., 1996). Participants were asked which days they used any of the following substances: alcohol to intoxication, marijuana, inhalant nitrates, powder cocaine, ecstasy, GHB, ketamine, crack cocaine, heroin, rohypnol, methamphetamine, or pharmaceuticals without or in excess of their prescribed use. For the present analysis, and given the distribution of the data, we created sum scores indicating the total number of days that participants stated using alcohol to intoxication, marijuana, inhalant nitrates, and all other drugs to create four summary variables with scores indicating days of use. At baseline we assessed only alcohol use (i.e., not alcohol to intoxication) and thus those data are not reported at baseline.
Condomless Sex Acts
Participants reported each instance of condomless receptive oral intercourse (ROI), receptive anal intercourse (RAI), and insertive anal intercourse (IAI) during the 30 days preceding interview. Data on sexual activity were collected as counts for each of the three sexual behaviors. Total scores indicate instances of each act during the timeframe and accounts for multiple within a day of sexual experience.
Analytic Plan
Means and standard deviations were obtained for all study variables across time. Additionally, correlations among variables within time were obtained. Latent growth curve modeling (LGCM) was used to investigate whether participants’ self-reported drug use and sexual activity increased between baseline and the 36-month follow-up and to determine whether changes in drug use predicted changes in condomless sexual activity. We began by fitting separate models for each drug use variable (i.e., alcohol to intoxication, marijuana use, inhalant use, and other drug use) as well as for each condomless sexual activity variable most associated with the transmission of HIV in gay, bisexual, and other MSM (receptive oral intercourse (ROI), insertive anal intercourse (IAI), and receptive anal intercourse (RAI) (CDC, 2016). Estimates of the final level (i.e., average level at 36-months) and linear rate of change between baseline and 36-months were obtained for each drug use and condomless sexual activity variable. Next, to account for the likelihood that participants used multiple drugs or engaged in multiple condomless sexual activities at one time, we fit two additional models: one in which we simultaneously estimated growth in the four drug use variables and allowed the intercepts and rates of change to correlate with one another and one in which we simultaneously estimated growth in the three unprotected sexual activity variables and allowed the intercepts and rates of change to correlate. By allowing the intercepts and rates of change for each variable to correlate, we were able to account for the comorbidity of drug use (i.e., high use of marijuana and high levels of alcohol to intoxication) or sexual activity, thereby obtaining a more accurate picture of participants’ behaviors.
To explore whether changes in each drug use were associated with changes in all three condomless sexual activity variables, we fit a series of multivariate latent growth models in which we simultaneously estimated growth in one drug variable (e.g., alcohol to intoxication) and all three unprotected sexual activity variables (e.g., condomless RAI, IAI, and ROI) and predicted the intercepts and rates of change in the three unprotected sexual activity variables from the intercept and rate of change in drug use. In other words, we examined whether participants who reported increases in the frequency of alcohol use to intoxication over time also reported increases in one or more unprotected sexual activities. Separate models were fit for each drug use variable, resulting in a total of four models. Again, the intercepts and rates of change in sexual activity were allowed to correlate to account for the possibility that participants engaged in multiple activities. Finally, to examine whether the effects of changes in drug use on changes in sexual activity varied by race/ethnicity or SES, we added to our models interactions between the intercept and rate of change in drug use and a set of dummy variables representing race/ethnicity or a set of dummy variables representing different levels of SES. Statistically significant interactions would suggest that the associations between changes in drug use and changes in sexual activity were not the same for all YMSM.
All models were initially fit without any control variables (i.e., unconditional models) and were subsequently re-fit controlling for participant race/ethnicity and perceived SES. Model fit was assessed using typical fit statistics including chi-square, CFI, and RMSEA. A small and non-significant chi-square value, a CFI close to 1, and a RMSEA value less than .08 all indicate good fit (Hu & Bentler, 1999). Note, however, that chi-square estimates are sensitive to large sample sizes and are thus considered quite conservative (Browne, Cudeck, Bollen, & Long, 1993), which is why other indices are considered. As is often the case in longitudinal studies, just over half (50.5%) of the participants were missing data for at least one of the six assessments (see Table 1 for sample sizes at each assessment). Because growth modeling does not require complete data to estimate an average intercept and rate of change, however, all analyses were based on the baseline sample. Further, there was no missing data for the control variables (i.e., race/ethnicity and perceived income). As previously noted (Halkitis et al., 2014b), no differential attrition was noted on key demographic factors. Further, we undertook analysis of the comparing the drug and sex behaviors at baseline of those who competed the TLFB at the 36-month assessment (72%) versus those did not complete that final assessment. No differences were noted other than for the oral sex variable much as those who were assessed on the TLFB in at the 36-month assessment reported a high rate of condomlesss oral sex at baseline as compared to those whom we did not assess via the TLFB at the final assessment (2.40 vs. 1.61, p = .03).
Table 1.
Participant drug use and condomless sexual behavior across time
| Assessment Period | |||||||
| Baseline (n = 598) | 6 Months (n = 460) | 12 Months (n = 445) | 18 Months (n = 428) | 24 Months (n = 436) | 30 Months (n = 416) | 36 Months (n = 430) | |
| % | |||||||
| Mean (SD) % |
Mean (SD) % |
Mean (SD) % |
Mean (SD) % |
Mean (SD) % |
Mean (SD) % |
Mean (SD) % |
|
| Drug Use | |||||||
| # Days Alcohol to Intoxication |
† | 2.07 (3.28) 50.96% | 2.51 (3.85) 59.55% | 2.55 (3.28) 65.89% | 2.66 (3.67) 65.60% | 2.71 (3.71) 66.11% | 2.73 (3.42) 67.67% |
| # Days Marijuana Use | 4.78 (8.67) 46.23% | 5.17 (8.88) 53.04% | 5.60 (9.41) 51.01% | 6.86 (10.47) 55.61% | 6.90 (10.60) 52.52% | 7.71 (11.06) 57.69% | 8.14 (11.53) 56.28% |
| # Days Inhalant Use | .07 (.64) 2.51% | .07 (.42) 4.13% | .07 (.42) 3.60% | .08 (.43) 5.37% | .15(.76) 6.42% | .15 (.77) 7.21% | .20 (1.03) 7.67% |
| # Days Other Drug Use | .55 (2.55) 12.73% | .64 (2.40) 15.00% | .61 (2.15) 17.75% | .72 (2.57) 21.73% | .77 (3.08) 18.35% | .59 (1.86) 19.47% | .65 (2.11) 19.77% |
| Condomless Sexual Behavior | |||||||
| Condomless ROI | 1.85 (3.45) 54.61% | 2.18 (3.89) 57.31% | 2.31 (3.72) 57.98% | 2.60 (3.76) 63.55% | 2.38 (3.13) 63.39% | 2.90 (4.13) 66.35% | 2.92 (4.62) 62.79% |
| Condomless IAI | .40 (1.99) 11.73% | .55 (2.34) 12.83% | .70 (2.91) 16.40% | .63 (2.27) 16.59% | .54 (2.02) 16.97% | .74 (2.62) 19.47% | .83 (2.60) 23.39% |
| Condomless RAI | .52 (2.26) 14.41% | .64 (2.42) 16.96% | .57 (2.03) 17.75% | .65 (2.06) 17.99% | .65 (1.86) 20.41% | .69 (2.09) 20.19% | .98 (3.19) 22.33% |
Alcohol use not Alcohol use to intoxication was not assessed at baseline
Study participants
A total of 2068 participants screened for the P18 study. Of those, 600 met eligibility criteria and were enrolled in the study, but data for 2 were not complete yielding a baseline sample of N = 598. Follow-up in person assessments were as follows: 6-month (N = 460), 12-month (N = 425), 18-month (N = 448), 24-month (N = 436 ), 30-month (N = 413), and 36 –month (N = 430). As a means of enhancing retention, participants could continue in the study even if an assessment was missed. This was to accommodate participants including those who may have been briefly incarcerated. The cohort was diverse in terms of race ethnicity as previously reported (Halkitis et al, 2015a). Specifically, 14.9% (n = 89) identified as African American, 38.3% (n = 229) identified as Hispanic, and 28.9% (n = 173) as White. In terms of perceived familiar SES 33.5% (n = 200) identified as low SES, while 37.1% (n =222), and 29.5% (n = 176) identified as middle and upper SES respectively. On average participants were 18 years old at baseline (M = 18.23, SD = 0.43, Md = 18). For those completing the assessment at 36-month in person, age was 21 years old (M = 21.27, SD = 0.48, Md = 21). We retained 72% (430 /600) of our baseline sample for in person assessments across seven waves of data collection, which include the administration of the TLFB, although as is noted, complete data are not needed to estimate the parameters of interest.
Results
Drug use and condomless sexual activity
As shown in Table 1, across 7 waves participants reveal persistent substance use and condomless sexual activity. Specifically, self-reported alcohol to intoxication and marijuana increased across time as the YMSM emerged into adulthood. Inhalant use also increased somewhat over this time. Participants reported using other drugs just under one day per month across time, although there was considerable variability in the number of days other drugs were used. Self-reported condomless sexual activity also increased from baseline to 36-month follow-up as is also shown in Table 1. Participants reported increases in condomless ROI across time, from approximately 1.83 episodes per month to just under 3 episodes per month. Similarly, although participants reported overall increases in condomless IAI and RAI between baseline and the 36-month follow-up visit, there was considerable variability in reported episodes both within and across time. For example, condomless IAI increased between baseline and the 12-month follow-up visit, decreased through the 24-month follow-up visit, and then began to increase again. Moreover, the proportion of study participants engaging in the behaviors increased across time as noted in the change in proportions also reported in Table 1.
Correlations among the drug use and unprotected sexual activity variables within each assessment period can be found in Table 2. In general, drug use variables were positively and significantly correlated with one another, suggesting that participants who reported more frequent use of one drug (e.g., alcohol to intoxication) also reported more frequent use of other drugs (e.g., marijuana, inhalants, and other drugs). Similarly, the condomless sexual activity variables were strongly and positively associated with one another, again suggesting that more frequent engagement in one activity was related to more frequent engagement in other unprotected sexual activities. This pattern was evident across time. The pattern of correlations among the drug use variables and sexual activities differed across assessments. In general, however, more frequent use of alcohol and drugs was positively associated with higher levels of condomless sexual activity. For example, at baseline, participants who reported more frequent marijuana and inhalant use, also reported engaging in more condomless ROI and IAI; those who used other drugs more often reported higher levels of unprotected sexual activity.
Table 2.
Correlations of drug use and condomless sexual behavior variables across time
| Baseline | 1 | 2 | 3 | 4 | 5 | 6 |
| 1. Alcohol to Intoxication† | -- | |||||
| 2. Marijuana Use | -- | -- | ||||
| 3. Inhalant Use | -- | .08* | -- | |||
| 4. Other Drug Use | -- | .31*** | .16*** | -- | ||
| 5. Condomless ROI | -- | .17*** | .05 | .21*** | -- | |
| 6. Condomless IAI | -- | .09* | .10* | .08+ | .56*** | -- |
| 7. Condomless RAI | -- | .05 | .02 | .16*** | .48*** | .43*** |
| Month 6 | 1 | 2 | 3 | 4 | 5 | 6 |
| 1. Alcohol to Intoxication | -- | |||||
| 2. Marijuana Use | .21*** | -- | ||||
| 3. Inhalant Use | .13*** | .09* | -- | |||
| 4. Other Drug Use | .29*** | .27*** | .17*** | -- | ||
| 5. Condomless ROI | .05 | .05 | .07 | .01 | -- | |
| 6. Condomless IAI | −.06 | −.01 | −.02 | −.05 | .23*** | -- |
| 7. Condomless RAI | −.03 | .03 | −.02 | .02 | .51*** | .14*** |
| Month 12 | 1 | 2 | 3 | 4 | 5 | 6 |
| 1. Alcohol to Intoxication | -- | |||||
| 2. Marijuana Use | .23*** | -- | ||||
| 3. Inhalant Use | .12* | .13** | -- | |||
| 4. Other Drug Use | .28*** | .22*** | .09+ | -- | ||
| 5. Condomless ROI | .10* | .09* | .04 | .07 | -- | |
| 6. Condomless IAI | −.002 | .09+ | −.02 | −.01 | .60*** | -- |
| 7. Condomless RAI | .01 | .03 | −.02 | .01 | .39*** | .15** |
| Month 18 | 1 | 2 | 3 | 4 | 5 | 6 |
| 1. Alcohol to Intoxication | -- | |||||
| 2. Marijuana Use | .19*** | -- | ||||
| 3. Inhalant Use | .12* | .11* | -- | |||
| 4. Other Drug Use | .18*** | .19*** | .08+ | -- | ||
| 5. Condomless ROI | .13** | .05 | .08 | .11* | -- | |
| 6. Condomless IAI | .01 | .03 | .03 | -.04 | .38*** | -- |
| 7. Condomless RAI | .07 | -.01 | .01 | -.01 | .44*** | .46*** |
| Month 24 | 1 | 2 | 3 | 4 | 5 | 6 |
| 1. Alcohol to Intoxication | -- | |||||
| 2. Marijuana Use | .16*** | -- | ||||
| 3. Inhalant Use | .13** | .07 | -- | |||
| 4. Other Drug Use | .24*** | .08 | .08+ | -- | ||
| 5. Condomless ROI | .13** | .13** | .23*** | .10* | -- | |
| 6. Condomless IAI | .07 | .10* | .14** | .05 | .34*** | -- |
| 7. Condomless RAI | .09+ | .14** | .21*** | .03 | .50*** | .21*** |
| Month 30 | 1 | 2 | 3 | 4 | 5 | 6 |
| 1. Alcohol to Intoxication | -- | |||||
| 2. Marijuana Use | .08 | -- | ||||
| 3. Inhalant Use | .20*** | .14** | -- | |||
| 4. Other Drug Use | .22** | .15** | .11* | -- | ||
| 5. Condomless ROI | .14** | .02 | .11* | .16** | -- | |
| 6. Condomless IAI | .02 | .07 | .03 | .11* | .58*** | -- |
| 7. Condomless RAI | .10* | -.06 | .01 | .13** | .42*** | .30*** |
| Month 36 | 1 | 2 | 3 | 4 | 5 | 6 |
| 1. Alcohol to Intoxication | -- | |||||
| 2. Marijuana Use | .04 | -- | ||||
| 3. Inhalant Use | .03 | .18*** | -- | |||
| 4. Other Drug Use | .13** | .14** | .02 | -- | ||
| 5. Condomless ROI | .11* | .10* | .18*** | .08 | -- | |
| 6. Condomless IAI | -.03 | .08+ | .07 | .05 | .51*** | -- |
| 7. Condomless RAI | .05 | .06 | .15** | .05 | .50*** | .21*** |
Alcohol to intoxication was not assessed at baseline;
p < .001,
p < .01,
p < .05,
p < .10
Latent growth curve analyses
Drug use across time
Results indicated that days of alcohol to intoxication (β = .023, p < .001), marijuana use (β = .091, p < .001), and inhalant use (β = .003, p < .05) all increased over time; there was no significant change in other drug use over time. Next, to account for the possibility that participants engaged in the use of multiple drugs at one time, we modeled simultaneously growth in the four drug use variables and allowed the intercepts and rates of change to correlate. We were unable to obtain results for the model containing changes in the four drug use variables or for the model containing changes in alcohol to intoxication, marijuana use, and inhalant use, likely due to the relatively limited variability in inhalant use across time; although it is possible that multi-collinearity was also an issue in these models. When we excluded inhalant use, a clear model emerged. Results from the model examining the simultaneous change in alcohol to intoxication, marijuana use, and other drug use are presented in Figure 1 (note correlations are not depicted in the figure). All three intercepts were statistically significant, suggesting there was actual (non-zero) use of alcohol to the point of intoxication (B0 = 2.86, p < .001), marijuana (B0 = 8.14, p < .001), and other drugs (B0 = .679, p < .001) at the 36-month follow-up visit. Importantly, there was significant positive growth in days of alcohol to intoxication (B1 = .023, p < .001), suggesting that even after accounting for changes in marijuana use and other drug use, participants increasingly engaged in alcohol consumption to the point of intoxication across time. Similarly, days of marijuana use increased significantly between baseline and the 36-month follow-up visit (B1 = .091, p < .001), controlling for changes in alcohol and other drug use. Not surprisingly given the low levels of days of other drug use at each timepoint, there was no evidence of growth in other drug use over time.
Figure 1.
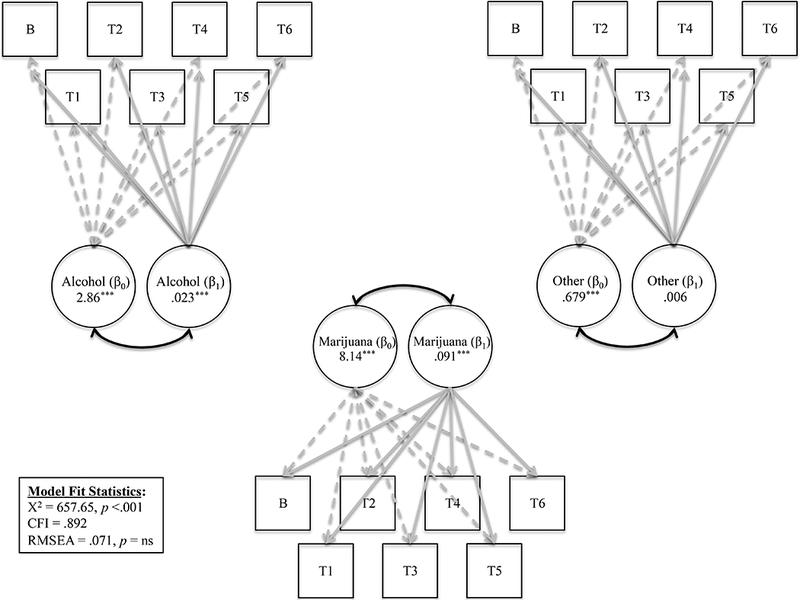
Latent growth curve models depicting drug use over time
Condomless sexual activity across time
Results indicated that instances of condomless ROI (β = .029, p < .001), condomless IAI (β = .011, p < .01), and condomless RAI (β = .009, p < .05) all increased over time. We then modeled simultaneously growth in the three condomless sexual activity variables and results are presented in Figure 2 (correlations are not depicted in the figure). All three intercepts were statistically significant, suggesting that participants regularly engaged in condomless ROI (B0 = 2.97, p < .001), condomless IAI (B0 = .047, p < .001), and condomless RAI (B0 = .049, p < .001) at the 36-month follow-up visit. Controlling for the correlations among sexual activity intercepts and rates of change instances both ROI (B1 = .030, p < .001) and IAI (B1 = .002, p < .01) increased over time, suggesting participants engaged in more condomless anal sexual activity between baseline and the 36-month follow-up visit; there was no significant growth in RAI over time. Note that although we tested whether these growth patterns differed by race/ethnicity and SES, we found no evidence of moderation and thus do not report the results here.
Figure 2.
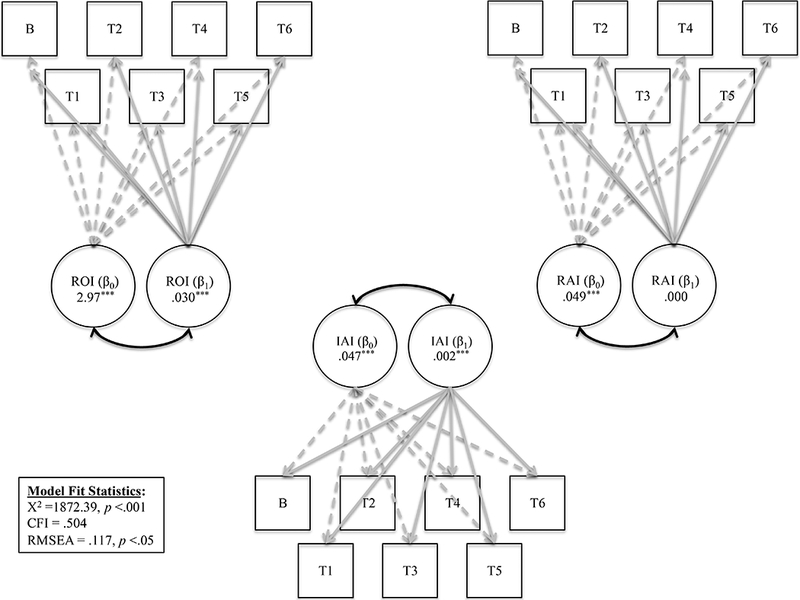
Latent growth curve models depicting condomless sexual behavior over time
Predicting condomless sex from drug use across time
Next, we fit a series of models to examine whether changes in drug use predicted changes in condomless sexual activity. Although a total of four models were fit (i.e., one for each drug use variable), we were only able to obtain results for two of the four models: alcohol to intoxication (Χ2 = 2073.50, p < .001; CFI = .616; RMSEA = .093, p < .001) and marijuana use (Χ2 = 2191.78, p < .001; CFI = .678; RMSEA = .091, p < .001). Alcohol use to intoxication at the 36-month follow-up visit was positively associated with both condomless ROI (B = .197, p < .001) and condomless RAI (B = .054, p < .05) but not with condomless IAI (B = .010, p = ns). Participants who reported more days of alcohol to intoxication also reported more instances of condomless ROI and RAI, even after taking into account their engagement in all other condomless sexual activity (i.e., the correlations among the intercepts and rates of change for ROI, IAI, and RAI). There were no significant associations between the rate of change in alcohol use and the rates of change in any of the sexual activity variables. Days of marijuana use at the 36-month follow-up visit (i.e., intercept) was also positively related to instances of condomless ROI at the 36-month follow-up visit, even after taking into account all other condomless sexual activity, such that participants who reported more marijuana use also reported higher levels of ROI (B = .048, p < .01). No other statistically significant associations were found for either the intercepts or rates of change. Model-fit statistics for both models indicate a relatively poor fit, likely due to several factors, including relatively limited growth in the unprotected sexual activity variables, relatively limited variability in that growth (i.e., most people are changing in a similar way), and a model that could be considered quite conservative given the fact that we controlled for the associations among unprotected sexual activities.
Given the aforementioned limitations, we conducted a set of follow-up analyses in which we examined in separate models the associations between growth in each drug use variable with growth in each condomless sexual activity variable (i.e., we examined in sex variable, ROI, IAI, RAI, separately). Results are presented in Table 3. As expected, model fit was much better for each of the separate sex behavior models. However, as was the case when we attempted to model inhalant use across time, the three models we test for explaining condomless sex also would not converge likely due to the relatively little use of this substance. Days of alcohol to intoxication, days of marijuana use, and days of other drug use at the 36-month follow-up were all positively associated with instances of condomless ROI (B = .197, p < .001; B =.045, p < .01; B = 373, p < .001, respectively). However rate of change in all of the drug use variables was unrelated to growth in condomless ROI. Days of alcohol to intoxication and days of other drug use also were each independently positively related to instances of condomless RAI such that participants who reported higher levels of drug use also reported higher levels of condomless RAI (B = .05, p < .05; B = .142, p < .001, respectively); again rate of change in all of the drug use variables was unrelated to growth in condomless RAI. No significant associations (i.e., neither intercept or slope/rate) were found for any of the drug variables with IAI.
Table 3.
Growth models explaining each condomless sexual behavior from drug use
| Condomless ROI | Condomless IAI | Condomless RAI | ||||
|---|---|---|---|---|---|---|
| Intercept | Rate of Change | Intercept | Rate of Change | Intercept | Rate of Change | |
| Alcohol to Intoxication | ||||||
| Intercept | .197*** | .008 | .056* | |||
| Rate of Change | 1.90 | .139 | -.555 | -.028 | -1.08 | -.087 |
| Model Fit Statistics | χ2 = 196.89*** RMSEA = .050 CFI = .927 |
χ2 = 303.93*** RMSEA = .070 CFI = .859 |
χ2 = 309.45*** RMSEA = .070 CFI = .856 |
|||
| Marijuana Use | ||||||
| Intercept | .045** | .010 | .006 | |||
| Rate of Change | -.957 | -.014 | .694 | -.014 | .356 | -.008 |
| Model Fit Statistics | χ2 = 267.72*** RMSEA = .056 CFI = .936 |
χ2 = 378.59*** RMSEA = .072 CFI = .896 |
χ2 = 349.06*** RMSEA = .070 CFI = .905 |
|||
| Other Drug Use | ||||||
| Intercept | .373*** | .040 | .142*** | |||
| Rate of Change | -2.39 | .053 | 7.99 | .250 | .329 | .207 |
| Model Fit Statistics | χ2 = 452.74*** RMSEA = .081 CFI = .781 |
χ2 = 534.60*** RMSEA = .090 CFI = .724 |
χ2 = 573.93*** RMSEA = .094 CFI = .708 |
|||
Note: Estimates for the model with changes in inhalants could not be obtained;
p <.001,
p <.01,
p < .05
As a final step, we re-fit our models but accounted for potential differences in these associations by perceived familial SES and race/ethnicity. As was the case with our basic growth models, there was no evidence that race/ethnicity and SES moderated the associations between changes in drug use and changes in sexual activity. Thus, we re-fit our models controlling for race/ethnicity and perceived SES and found that the pattern of findings was identical to the pattern from the models without these controls and the coefficients did not change considerably so we have not included the results here.
Discussion
The synergy that exists between non-injection drug use and sexual behavior among gay, bisexual, and other MSM, can be traced throughout the course of the HIV in the United States (Halkitis, Levy, Moreira, & Ferrusi, 2014; Halkitis et al., 2011). What emerges from the scientific literature is an understanding that drug use and sexual risk behavior are best understood as co-occurring phenomena and part of a larger conception of a syndemic across the lifespan (Halkitis et al., 2012; _Halkitis et al., 2013; N. Halkitis, Kapadia, C. Ompad, & Perez-Figueroa, 2015). Additionally, they function in tandem with other health conditions, including mental health burdens (Hanson et al., 2015; O’Cleirigh et al., 2013) and experiences of violence (Stults et al., 2015).
The findings of our investigation attempt to address several shortcomings of the extant literature and to develop new knowledge regarding the interplay between drug use and sexual risk behaviors in emerging adult sexual minority men. Participants in our cohort study were followed across seven waves of data collection between 2009 and 2014, as they emerged into adulthood from ages 18–19 to 21–22. This period of emerging adulthood is often associated with high levels of experimentation both in terms of drug use and sex (Arnett, 2005; Makarios, Cullen, & Piquero, 2015; Quinn & Harden, 2013; Steinberg, 2008; Stone, Becker, Huber, & Catalano, 2012; White et al., 2006), which may set the bases for lifelong behavioral patterns (Chassin, Flora, & King, 2004; Wagner & Anthony, 2002).
The results indicate that across 36-months of data collection there is significant growth in the use of drugs, namely alcohol to intoxication, marijuana, use of inhalant nitrates, although use of the latter remains relatively low throughout the period of assessment. Use of other drugs including those commonly cited in the literature as drivers of HIV, such as methamphetamine, remain relatively stable over time and aligns with previous investigations indicating that the onset of such “party” or “club” drugs often occurs at later ages among gay and bisexual men (Halkitis & Palamar, 2008). As might be expected, we detected associations between use of drugs at each of the timepoints, which support previous studies of poly-drug use (Patterson, Semple, Zians, & Strathdee, 2005; Stall et al., 2003) as well as associations of drug use across time (Halkitis, Palamar, & Mukherjee, 2007). As our findings indicate, there is a significant amount of use of alcohol to intoxication, marijuana, and other drug use at the 36-month assessment, even in models that control for the use of other substances, indicating that a subset of study participants are engaging in these drug use behaviors at ages 20–21. Inhalant nitrate use, which is often cited as a facilitator of HIV transmission in behavioral studies but with samples skewing slightly older (Buchbinder et al., 2005; Macdonald et al., 2008), remains low at the 36-month assessment relative to the other substances we examined in this sample of YMSM. This finding may be due to the very young age of study participants or potentially, a generational effect in relationship to the use of inhalants, a finding which we can continue to examine as the participants in this cohort study continue to age.
As is the case with drug use, condomless sex also increases as the YMSM emerge into adulthood. This was the case for all three behaviors that we examined, namely condomless receptive oral, condomless receptive anal, and condomless insertive anal intercourse. For all emerging adults, entree into adulthood is often associated with a higher frequency of sexual behavior (Arnett, 2000; Claxton & van Dulmen, 2013; Zarrett & Eccles, 2006), a finding that has also been clearly demonstrated in earlier studies of sexual minority men. Our data clearly indicate that YMSM regularly engage in all three behaviors at the 36-month assessment. High levels of association are also detected among the sexual behaviors at each timepoint. In models controlling for the associations between the sexual behaviors, we find independent significant growth of both insertive anal intercourse and receptive oral intercourse over the 36 month assessment period, as the participants become more sexually active.
Finally, through a series of bivariable tests conducted at each assessment and multivariable models examining associations of time, we find convincing evidence of the co-occurrence of drug use with condomless sexual activity. As has previous been noted, numerous studies, often based on cross-sectional data, have determined such associations (Kecojevic, Silva, Sell, & Lankenau, 2015; Newcomb & Mustanski, 2014), and a smaller number of studies (Colfax et al., 2005; Halkitis, Mukherjee, & Palamar, 2009) have examined these patterns across time. Our findings indicate that the link between drug use and sexual risk behavior continues to exist in a new generation of sexual minority men in this the fourth the decade of HIV. However, it is important to note that the most robust finding is with regard to alcohol to intoxication, which we found to be independently associated with both receptive oral and anal intercourse, both in models examining the relationship to these sex behaviors simultaneously and in ones examining sex behaviors independently. This finding with regard to alcohol to intoxication must be considered in light of the age of study participants, who at baseline are underage in terms of drinking, and who remain underage throughout the duration of most of our investigation. Still the relationship between drinking to intoxication and sexual risk is robust, and these findings align with previous investigations of alcohol use among YMSM (Colfax et al., 2004; Salomon et al., 2008). The role of alcohol as risk factor for sexual minority men must be underscored. Too often the focus of risk is directed to psychoactive drugs such as methamphetamine, ketamine, and other club/party drugs under the umbrella of sexualized drug use (Kipke et al., 2007). Yet alcohol must be considered a sexualized drug as it sexually disinhibits YMSM and provides cognitive escape (Woolf & Maisto, 2009), it is much more readily available to the population, and is often at the social venues where young sexual minority men engage with each other (Pollock et al, 2012; Wong, Kipke, & Weiss, 2008).
Findings with regard to marijuana are less constant, and findings with regard to inhalant nitrate use are near absent, as has been previously noted. Data regarding other drug use however merits our attention. While use of other drugs remains relatively low, as our growth curve models support, we do detect a strong association between use and both oral and anal condomless receptive acts. Given the psychoactive effects of many of the drugs included in this category, the impact on sex risk behaviors is not surprising and requires further attention as these YMSM age and likely increase their use of drugs such as methamphetamine.
A critical finding of our investigation is that the association between drug use and condomless sex does not differ by race/ethnicity. This builds upon our earlier reports from this cohort study that show that Black YMSM, who are most affected by HIV in the United States (CDC, 2015) and in our study (Halkitis, Kapadia, & Ompad, 2015), do not engage in more sexual risk behavior than their White peers (Kapadia et al., 2015). Moreover, similar findings are indicated for drug and alcohol use; any differences that do emerge are attenuated in light of socioeconomic status (Perry N Halkitis et al., 2014). Such findings support the notion that behavior in and of itself, is insufficient in explaining HIV prevalence in the Black population, supporting the work of others (Millett, Flores, Peterson, & Bakeman, 2007). Social and structural factors, including poverty and more limited access to quality health, which may lead to more untreated and unmanaged HIV infections within the population and greater psychosocial burdens which may engender risk, provide a clearer explanation of the drivers of these epidemiological patterns.
Limitations
Despite the strengths of our methods, there are limitations that should be considered. The implementation of the TLFB is limited to a one-month recall period, the month prior to assessment, thus failing to capture the totality of behaviors in the six months between assessments. Also with regard to the data, we also note that 28% of those assessed at baselines did not complete an in person assessment at the final assessment and thus have missing TLFB data at this timepoint. Still, those whom we did not assess at this final timepoint did not differ form those who did complete it on any key demographics, drug use, or sex behaviors, other than the frequency of condomless oral sex; although statistically significant the difference limited clinical significance (i.e., less than one act per month). Second, the limited use of psychoactive drugs (e.g., heroin, methamphetamine) and other substances (e.g., use of pharmaceuticals without a prescription) necessitated our amalgamation of these behaviors into an “other drug” use category for the purposes of analyses. Such aggregate scores are limited and provide little room for interpretation other than extrapolating that this set of drugs is not one of the other drugs we model (i.e., alcohol, marijuana, and inhalant nitrates). As use of these drugs increases over time, analyses of individual drugs may be undertaken. Also the limited use of inhalant nitrates created a condition by which models would not converge. This condition coupled with the use of an “other drug” category suggests that we may want to reconsider the handling of these data in future analyses, although this too is dependent on growth in use of the drugs. We note that TLFB data were not collected on those who relocated from the study site to another part of the country. However, our use of latent growth curve modeling was not dependent on following the entire sample for all seven waves of data collections and there is no evidence for differential attrition ( Halkitis et al., 2014). While the cohort study has many design advantages, our sample is not a random one and thus limited in terms of generalizability both within the study region and more generally. Nevertheless, the sample is quite diverse, and in fact we oversample YMSM of color, a segment of the population disproportionately affected by the HIV. Moreover, the failure of a small number of the models to converge is likely due to relatively low levels of drug use or sexual activity and limited variability between individuals in these behaviors, two characteristics of the data that are critical for latent growth modeling. Additionally, the overlap in some of the behaviors (or the engagement in multiple behaviors at once) may have led to higher than average levels of multicollinearity, thus causing the models to fail. Finally, we recognize that we have utilized measure or perceived familial as compared to actual SES. Given the age of the study participants and associated complexities in measuring SES at this developmental stage (Shaver, 2007) and the literature supporting the use of this measure in studies of health (Goodman et al., 2007), we feel that perceived familial captures the construct as we conceptualized it as is a strong indicator of SES in which the participant was raised. Despite these limitations, the study design is strong in so much as data are gathered longitudinally from a sample that is diverse in terms of race/ethnicity and socioeconomic status. Moreover, our use of the TLFB provides a strong tool for gathering reliable behavioral data.
Conclusions
The findings of our analyses, based on an ongoing cohort study of sexual minority, emerging adult YMSM, suggest that this developmental period is one in which both drug use and risky sexual behavior rapidly evolve. In addition, the relationship between these co-occurring behaviors likely is bi-directional and mutually reinforcing. These results support the idea that HIV prevention and care must be nested within the broader context of gay men’s health. To this end, medical practice focused on gay men’s health must understand HIV in this context, with attention to the synergy that exists between drug use and sexual risk and also the numerous other health burdens young sexual minority men face including violence and mental health burdens, and finally within socio-political-economic circumstances of the time.
Acknowledgments
Research reported in this publication was supported by the National Institute on Drug Abuse of the National Institutes of Health under award numbers 1R01DA025537 and 2R01DA025537. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest The authors have no conflict of interest to disclose.
References
- Arnett JJ (2000). Emerging adulthood. A theory of development from the late teens through the twenties. Am Psychol, 55(5), 469–480. [PubMed] [Google Scholar]
- Arnett JJ (2005). The developmental context of substance use in emerging adulthood. Journal of drug issues, 35(2), 235–254. [Google Scholar]
- Beyrer C, Baral SD, van Griensven F, Goodreau SM, Chariyalertsak S, Wirtz AL, & Brookmeyer R (2012). Global epidemiology of HIV infection in men who have sex with men. Lancet, 380(9839), 367–377. doi: 10.1016/S0140-6736(12)60821-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne MW, Cudeck R, Bollen KA, & Long JS (1993). Alternative ways of assessing model fit. Sage focus editions, 154, 136–136. [Google Scholar]
- Buchbinder SP, Vittinghoff E, Heagerty PJ, Celum CL, Seage III GR, Judson FN, Koblin BA (2005). Sexual risk, nitrite inhalant use, and lack of circumcision associated with HIV seroconversion in men who have sex with men in the United States. JAIDS Journal of Acquired Immune Deficiency Syndromes, 39(1), 82–89. [DOI] [PubMed] [Google Scholar]
- Carey JW, Mejia R, Bingham T, Ciesielski C, Gelaude D, Herbst JH, Jenkins RA (2009). Drug use, high-risk sex behaviors, and increased risk for recent HIV infection among men who have sex with men in Chicago and Los Angeles. AIDS and Behavior, 13(6), 1084–1096. [DOI] [PubMed] [Google Scholar]
- CDC. (2015). HIV Surveillance Report, 2014 (Vol. 26): Centers for Disease Control and Prevention. [Google Scholar]
- Chassin L, Flora DB, & King KM (2004). Trajectories of alcohol and drug use and dependence from adolescence to adulthood: the effects of familial alcoholism and personality. Journal of abnormal psychology, 113(4), 483. [DOI] [PubMed] [Google Scholar]
- Claxton SE, & van Dulmen MH (2013). Casual sexual relationships and experiences in emerging adulthood. Emerging Adulthood, 1(2), 138–150. [Google Scholar]
- Colfax G, Coates TJ, Husnik MMJ, Huang Y, Buchbinder S, Koblin B, Team ES (2005). Longitudinal patterns of methamphetamine, popper (amyl nitrite), and cocaine use and high-risk sexual behavior among a cohort of San Francisco men who have sex with men. Journal of Urban Health, 82(1), i62–i70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colfax G, Vittinghoff E, Husnik MJ, McKirnan D, Buchbinder S, Koblin B, Mayer K (2004). Substance use and sexual risk: a participant-and episode-level analysis among a cohort of men who have sex with men. American Journal of Epidemiology, 159(10), 1002–1012. [DOI] [PubMed] [Google Scholar]
- Ellen JM, Greenberg L, Willard N, Stines S, Korelitz J, & Boyer CB (2015). Cross-sectional survey comparing HIV risk behaviours of adolescent and young adult men who have sex with men only and men who have sex with men and women in the US and Puerto Rico. Sexually Transmitted Infections, 91(6), 458–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman E, Huang B, Schafer-Kalkhoff T, & Adler NE (2007). Perceived socioeconomic status: a new type of identity that influences adolescents’ self-rated health. Journal of Adolescent Health, 41(5), 479–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN, Kapadia F, Bub KL, Barton S, Moreira AD, & Stults CB (2015). A Longitudinal Investigation of Syndemic Conditions Among Young Gay, Bisexual, and Other MSM: The P18 Cohort Study. AIDS Behav, 19(6), 970–980. doi: 10.1007/s10461-014-0892-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN, Kapadia F, & Ompad DC (2015). Incidence of HIV Infection in Young Gay, Bisexual, and Other YMSM: The P18 Cohort Study. JAIDS Journal of Acquired Immune Deficiency Syndromes, 69(4), 466–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN, Kupprat SA, Hampton MB, Perez‐Figueroa R, Kingdon M, Eddy JA, & Ompad DC (2012). Evidence for a syndemic in aging HIV‐positive gay, bisexual, and other MSM: implications for a holistic approach to prevention and health care. Annals of Anthropological Practice, 36(2), 365–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN, Levy MD, Moreira AD, & Ferrusi CN (2014). Crystal Methamphetamine Use and HIV Transmission Among Gay and Bisexual Men. Current Addiction Reports, 1(3), 206–213. [Google Scholar]
- Halkitis PN, Mukherjee PP, & Palamar JJ (2009). Longitudinal modeling of methamphetamine use and sexual risk behaviors in gay and bisexual men. AIDS and Behavior, 13(4), 783–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN, & Palamar JJ (2008). Multivariate modeling of club drug use initiation among gay and bisexual men. Substance use & misuse, 43(7), 871–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN, Palamar JJ, & Mukherjee PP (2007). Poly-club-drug use among gay and bisexual men: a longitudinal analysis. Drug Alcohol Depend, 89(2), 153–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN, Pollock JA, Pappas MK, Dayton A, Moeller RW, Siconolfi D, & Solomon T (2011). Substance use in the MSM population of New York City during the era of HIV/AIDS. Subst Use Misuse, 46(2–3), 264–273. doi: 10.3109/10826084.2011.523265 [DOI] [PubMed] [Google Scholar]
- Halkitis PN, Siconolfi DE, Stults CB, Barton S, Bub K, & Kapadia F (2014). Modeling substance use in emerging adult gay, bisexual, and other YMSM across time: The P18 cohort study. Drug Alcohol Depend, 145, 209–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN, Wolitski RJ, & Millett GA (2013). A holistic approach to addressing HIV infection disparities in gay, bisexual, and other men who have sex with men. American Psychologist, 68(4), 261. [DOI] [PubMed] [Google Scholar]
- Hanson KE, Mansergh G, Koblin BA, Flores SA, Hudson SM, Myers L, & Colfax GN (2015). Depressive symptoms by HIV serostatus are differentially associated with unprotected receptive and insertive anal sex among substance-using men who have sex with men in the United States. JAIDS Journal of Acquired Immune Deficiency Syndromes, 68(1), e13–e16. [DOI] [PubMed] [Google Scholar]
- Hu L. t., & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural equation modeling: a multidisciplinary journal, 6(1), 1–55. [Google Scholar]
- Kapadia F, Bub K, Barton S, Stults CB, & Halkitis PN (2015). Longitudinal Trends in Sexual Behaviors Without a Condom Among Sexual Minority Youth: The P18 Cohort Study. AIDS Behav, 19(12), 2152–2161. doi: 10.1007/s10461-015-1175-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kecojevic A, Silva K, Sell RL, & Lankenau SE (2015). Prescription drug misuse and sexual risk behaviors among young men who have sex with men (YMSM) in Philadelphia. AIDS and Behavior, 19(5), 847–856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kingdon MJ, Storholm ED, Halkitis PN, Jones DC, Moeller RW, Siconolfi D, & Solomon TM (2013). Targeting HIV Prevention Messaging to a New Generation of Gay, Bisexual, and Other Young Men Who Have Sex With Men. Journal of health communication, 18(3), 325–342. doi: 10.1080/10810730.2012.727953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lansky A, Brooks JT, DiNenno E, Heffelfinger J, Hall HI, & Mermin J (2010). Epidemiology of HIV in the United States. J Acquir Immune Defic Syndr, 55 Suppl 2, S64–68. doi: 10.1097/QAI.0b013e3181fbbe15 [DOI] [PubMed] [Google Scholar]
- Longmire-Avital B, & Miller-Dyce C (2015). Factors related to perceived status in the campus community for first generation students at an HBCU. College Student Journal, 49(3), 375–386. [Google Scholar]
- MacArrthur Research Network on SES & Health (2009). Social environmet notebook. Retrieved from http://www.macses.ucsf.edu/research/socialenviron/economic.php
- Macdonald N, Elam G, Hickson F, Imrie J, McGarrigle CA, Fenton KA, Power RM (2008). Factors associated with HIV seroconversion in gay men in England at the start of the 21st century. Sexually Transmitted Infections, 84(1), 8–13. [DOI] [PubMed] [Google Scholar]
- Makarios M, Cullen FT, & Piquero AR (2015). Adolescent criminal behavior, population heterogeneity, and cumulative disadvantage untangling the relationship between adolescent delinquency and negative outcomes in emerging adulthood. Crime & Delinquency, 0011128715572094. [Google Scholar]
- Millett GA, Flores SA, Peterson JL, & Bakeman R (2007). Explaining disparities in HIV infection among black and white men who have sex with men: a meta-analysis of HIV risk behaviors. AIDS, 21(15), 2083–2091. doi: 10.1097/QAD.0b013e3282e9a64b [DOI] [PubMed] [Google Scholar]
- Moeller RW, Halkitis PN, Pollock JA, Siconolfi DE, & Barton S (2013). When the Emotions Really Started Kicking In, Which Ended Up Being a Problem: Sex, HIV, and Emotions Among Young Gay and Bisexual Men. Journal of Homosexuality, 60(5), 773–795. doi: 10.1080/00918369.2013.773825 [DOI] [PubMed] [Google Scholar]
- Mustanski B, Garofalo R, Herrick A, & Donenberg G (2007). Psychosocial health problems increase risk for HIV among urban young men who have sex with men: preliminary evidence of a syndemic in need of attention. Ann Behav Med, 34(1), 37–45. doi: 10.1080/08836610701495268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Newcomb ME, Du Bois SN, Garcia SC, & Grov C (2011). HIV in Young Men Who Have Sex with Men: A Review of Epidemiology, Risk and Protective Factors, and Interventions. The Journal of Sex Research, 48(2–3), 218–253. doi: 10.1080/00224499.2011.558645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN, Kapadia F, Ompad DC, & Perez-Figueroa R (2015). Moving toward a holistic conceptual framework for understanding healthy aging among gay men. Journal of Homosexuality, 62(5), 571–587. [DOI] [PubMed] [Google Scholar]
- Newcomb ME, & Mustanski B (2014). Developmental change in the relationship between alcohol and drug use before sex and sexual risk behavior in young men who have sex with men. AIDS Behav, 18(10), 1981–1990. doi: 10.1007/s10461-014-0766-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomb ME, Ryan DT, Greene GJ, Garofalo R, & Mustanski B (2014). Prevalence and patterns of smoking, alcohol use, and illicit drug use in young men who have sex with men. Drug Alcohol Depend, 141, 65–71. doi: 10.1016/j.drugalcdep.2014.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Cleirigh C, Newcomb ME, Mayer KH, Skeer M, Traeger L, & Safren SA (2013). Moderate levels of depression predict sexual transmission risk in HIV-infected MSM: a longitudinal analysis of data from six sites involved in a “prevention for positives” study. AIDS and Behavior, 17(5), 1764–1769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Outlaw AY, Phillips G 2nd, Hightow-Weidman LB, Fields SD, Hidalgo J, Halpern-Felsher B, & Green-Jones M (2011). Age of MSM sexual debut and risk factors: results from a multisite study of racial/ethnic minority YMSM living with HIV. AIDS Patient Care STDS, 25 Suppl 1, S23–29. doi: 10.1089/apc.2011.9879 [DOI] [PubMed] [Google Scholar]
- Parsons JT, Grov C, & Golub SA (2012). Sexual compulsivity, co-occurring psychosocial health problems, and HIV risk among gay and bisexual men: further evidence of a syndemic. American journal of public health, 102(1), 156–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson TL, Semple SJ, Zians JK, & Strathdee SA (2005). Methamphetamine-using HIV-positive men who have sex with men: correlates of polydrug use. Journal of Urban Health, 82, i120–i126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perdue T, Hagan H, Thiede H, & Valleroy L (2003). Depression and HIV risk behavior among Seattle-area injection drug users and young men who have sex with men. AIDS Education and Prevention, 15(1), 81–92. doi: 10.1521/aeap.15.1.81.23842 [DOI] [PubMed] [Google Scholar]
- Pollock JA, Halkitis PN, Moeller RW, Solomon TM, Barton SC, Blachman-Forshay J, Love HT (2012). Alcohol use among young men who have sex with men. Substance use & misuse, 47(1), 12–21. [DOI] [PubMed] [Google Scholar]
- Quinn PD, & Harden KP (2013). Differential changes in impulsivity and sensation seeking and the escalation of substance use from adolescence to early adulthood. Development and Psychopathology, 25(01), 223–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson SM, Sobell LC, Sobell MB, & Leo GI (2014). Reliability of the Timeline Followback for cocaine, cannabis, and cigarette use. Psychology of addictive behaviors, 28(1), 154. [DOI] [PubMed] [Google Scholar]
- Salomon EA, Mimiaga MJ, Husnik MJ, Welles SL, Manseau MW, Montenegro AB, Mayer KH (2008). Depressive Symptoms, Utilization of Mental Health Care, Substance Use and Sexual Risk Among Young Men Who have Sex with Men in EXPLORE: Implications for Age-Specific Interventions. AIDS and Behavior, 13(4), 811–821. doi: 10.1007/s10461-008-9439-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salomon EA, Mimiaga MJ, Husnik MJ, Welles SL, Manseau MW, Montenegro AB, Mayer KH (2009). Depressive symptoms, utilization of mental health care, substance use and sexual risk among young men who have sex with men in EXPLORE: implications for age-specific interventions. AIDS Behav, 13(4), 811–821. doi: 10.1007/s10461-008-9439-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shavers VL (2007). Measurement of socioeconomic status in health disparities research. Journal of the national medical association, 99(9), 1013–1023. [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Brown J, Leo GI, & Sobell MB (1996). The reliability of the Alcohol Timeline Followback when administered by telephone and by computer. Drug Alcohol Depend, 42(1), 49–54. [DOI] [PubMed] [Google Scholar]
- Stall R, Mills TC, Williamson J, Hart T, Greenwood G, Paul J, Catania JA (2003). Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. American journal of public health, 93(6), 939–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L (2008). A social neuroscience perspective on adolescent risk-taking. Developmental review, 28(1), 78–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone AL, Becker LG, Huber AM, & Catalano RF (2012). Review of risk and protective factors of substance use and problem use in emerging adulthood. Addictive behaviors, 37(7), 747–775. [DOI] [PubMed] [Google Scholar]
- Stults CB, Javdani S, Greenbaum CA, Kapadia F, & Halkitis PN (2015). Intimate partner violence and substance use risk among young men who have sex with men: The P18 cohort study. Drug Alcohol Depend, 154, 54–62. doi: 10.1016/j.drugalcdep.2015.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stults CB, Javdani S, Greenbaum CA, Kapadia F, & Halkitis PN (2016). Intimate Partner Violence and Sex Among Young Men Who Have Sex With Men. J Adolesc Health, 58(2), 215–222. doi: 10.1016/j.jadohealth.2015.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner FA, & Anthony JC (2002). From first drug use to drug dependence: developmental periods of risk for dependence upon marijuana, cocaine, and alcohol. [DOI] [PubMed]
- White HR, McMorris BJ, Catalano RF, Fleming CB, Haggerty KP, & Abbott RD (2006). Increases in alcohol and marijuana use during the transition out of high school into emerging adulthood: The effects of leaving home, going to college, and high school protective factors. Journal of studies on alcohol, 67(6), 810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong CF, Schrager SM, Chou CP, Weiss G, & Kipke MD (2013). Changes in developmental contexts as predictors of transitions in HIV-risk behaviors among young men who have sex with men (YMSM). Am J Community Psychol, 51(3–4), 439–450. doi: 10.1007/s10464-012-9562-2 [DOI] [PubMed] [Google Scholar]
- Wong CF, Weiss G, Ayala G, & Kipke MD (2010). Harassment, discrimination, violence, and illicit drug use among young men who have sex with men. AIDS Educ Prev, 22(4), 286–298. doi: 10.1521/aeap.2010.22.4.286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarrett N, & Eccles J (2006). The passage to adulthood: Challenges of late adolescence. New directions for youth development, 2006(111), 13–28. [DOI] [PubMed] [Google Scholar]


