Abstract
Genital tuberculosis (TB) is a rare, comprising <0.5% cases of extrapulmonary TB. Among cases of genitourinary TB, glandular TB is even rarer. Its a diagnosis of exclusion. Most patients present later in the course of disease due to the associated stigma in view of site of involvement and the hesitancy on the patients's part. We saw two such cases of nonhealing genital ulcers in immunocompetent males.
Key words: Genital tuberculosis, glans penis, nonhealing ulcer
INTRODUCTION
Extrapulmonary tuberculosis (EPTB) includes a small percentage of people suffering from tuberculosis (TB) (10%–15% cases) with lymph nodes being the most common site in India.[1] Genitourinary TB is an unusual presentation and has been reported in <0.5% of EPTB.[2] Only 28% patients of genitourinary TB have isolated genital involvement.[3] It is more common in males; epididymis being the most common site. Other parts involved are seminal vesicles, prostate, testis, and vas deferens in descending order.[4] Glandular TB is a very rare form.[5] It is usually a diagnosis of exclusion as it can mimic various pathologies. Here, we have discussed nonhealing genital ulcers in two immunocompetent males.
CASE REPORT
Case 1
A 21-year-old unmarried male presented with raw painless lesions over the glans penis for 2 months. The penile lesion appeared as a small ulcer on the dorsal aspect of the glans penis which progressively increased in size and number with the presence of yellowish discharge. The patient gave a history of similar lesion of smaller size over glans 7 months ago which responded to tablet co-trimoxazole. He gave a history of protected penovaginal intercourse with a commercial sex worker 2 years ago. For present complaints, he had been treated with tablet acyclovir, doxycycline, azithromycin, co-trimoxazole, and 3 doses of injection benzathine penicillin over a period of 4 weeks without any improvement. He did not have a history of pulmonary tuberculosis. On enquiry, the patient gave a history of low-grade fever and decrease in appetite for 2 months.
Cutaneous examination revealed multiple well-defined ulcers on the dorsolateral aspect of glans penis. The lesions measured 0.5–1.5 cm in diameter with yellowish slough on the floor and indurated base [Figure 1]. There was no evidence of significant inguinal lymphadenopathy.
Figure 1.

Case 1: Multiple well-defined ulcers on the dorsolateral aspect of glans penis, measuring 0.5 cm to 1.5 cm in diameter, yellowish slough on the floor and indurated base
During the course of admission, the patient complained of pain in the scrotum for which a testicular sonogram was performed. It revealed a bulky and nodular epididymis on both sides with few calcific specks on the right side. The lesion in right epididymis continued with a focal hypoechoic lesion in the right testis. There was diffuse thickening of the scrotal skin. The finding of bilateral nodular epididymal involvement with right-sided epididymo-orchitis in the given clinical context was highly suggestive of tubercular etiology [Figure 2]. Biopsy from the edge of the ulcer showed the absence of epidermis with dense granulomatous infiltrate comprising lymphohistiocytes, epitheloid cells, and plasma cells in dermis surrounding caseous necrosis [Figure 3].
Figure 2.
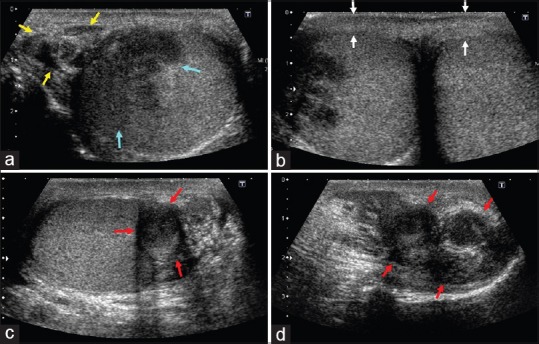
(a) Transverse gray-scale image reveals enlargement and heterogeneous echo texture of tail of the right epididymis (yellow arrows) on right with direct extension to the testicle (blue arrows). (b) Thickening of scrotal skin (white arrows). (c and d) Uninvolved left testicle is with enlarged and nodular left epididymis (red arrows in c and d, longitudinal scan), suggestive of tuberculous epididymo-orchitis
Figure 3.
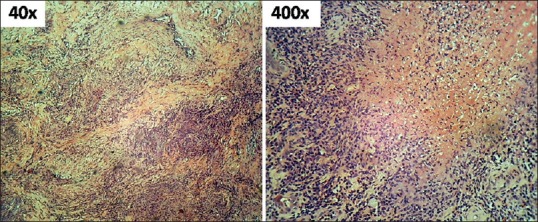
Biopsy from the edge of the ulcer showing the absence of epidermis with dense granulomatous infiltrate of lymphohistiocytes, epitheloid cells, and plasma cells in dermis surrounding caseous necrosis (H and E)
Case 2
A 45-year-old married male presented with multiple ulcers on glans penis for 3 weeks with difficulty in retracting prepuce. He denied the history of high-risk sexual behavior or presence of similar lesions in the spouse. There was no history suggestive of tuberculosis.
He was treated with co-trimoxazole and doxycycline for 2 weeks without significant improvement. Cutaneous examination revealed multiple ulcers on glans penis and inner surface of prepuce, measuring about 0.5–1 cm in size, with white discharge on floor and indurated base [Figure 4] without evidence of regional lymphadenopathy. Biopsy from the edge of the ulcer showed the absence of epidermis with dense granulomatous infiltrate comprising lymphohistiocytes, epitheloid cells, plasma cells, and Langhans giant cell in dermis [Figure 5].
Figure 4.

Case 2: Multiple ulcers on glans penis and inner surface of prepuce, measuring 0.5–1 cm in size, white discharge on floor and indurated base
Figure 5.
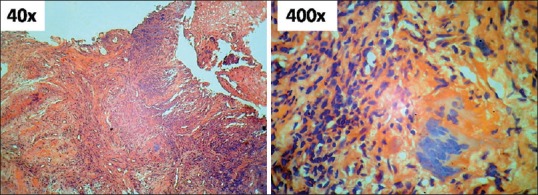
Biopsy from the edge of the ulcer showing the absence of epidermis with dense granulomatous infiltrate comprising lymphohistiocytes, epitheloid cells, and plasma cells in dermis with the evidence of Langhans giant cell
Differential diagnoses of Behcet's disease and genital TB were considered for both patients. Tzanck smear, Gram's stain, and potassium hydroxide mount were negative. Laboratory investigations revealed raised erythrocyte sedimentation rate (ESR) and positive Mantoux test. Tissue for bacterial, fungal, and acid-fast bacilli culture did not reveal any significant growth. Venereal disease research laboratory (VDRL) and ELISA for HIV were nonreactive in both cases.
Both patients were diagnosed to have primary genital TB and were given 4 drug antitubercular therapy (ATT) comprising capsule rifampicin 600 mg OD, tablet isoniazid 300 mg OD, tablet pyrizinamide 1500 mg OD, and tablet ethambutol 800 mg OD with daily cleaning and dressing of the ulcers. After 10 days of treatment, there was a considerable reduction in the slough, and the ulcers showed healing in the first case [Figure 6]. The second patient was lost to follow-up.
Figure 6.

Post treatment improvement in Case 2: Multiple ulcers showing reduction in slough and mild decrease in size of ulcers
DISCUSSION
The term “genitourinary tuberculosis” was first used by Hans Wildbolz in 1937. It is a common delayed manifestation of prior pulmonary tuberculosis.[6] The genitourinary tract involvement in TB is rare. It may be due to reactivation of acid-fast bacilli, hypersensitivity to the bacterial antigens, direct inoculation from contaminated hands, or from an infected partner through sexual intercourse.[7,8,9,10]
The sites of involvement in descending order are epididymis (42%), seminal vesicles (23%), prostrate (21%), testis (15%), and vas deferens (12%).[11] TB of the penis is extremely rare comprising <1% patients of genital TB.
Penile TB may occur as a primary lesion or secondary to pulmonary TB.[12] It may affect the glans, shaft of the penis, or cavernous bodies. In majority of cases, a chronic superficial ulcer or ulceronodular lesion is present on the corona or glans as friction during sexual exposure is common in these parts. Other clinical presentations can be gummatous, phagedenic, or complete penile destruction. Rarely, orificial TB can occur in immunocompromised people[13] which is a severe necrotic form of glandular TB. A relatively mild form of the disease includes papulonecrotic tuberculid. Lupus vulgaris may present as erythematous or keratotic plaques, glandular ulcers, urethritis, or cavernositis[14,15,16,17] which may lead to scarring and disfigurement of the penis.
A raised ESR and lymphocytosis on hematological examination may be seen. Urinalysis and urine culture are usually negative; however, sterile pyuria may be present in case of urinary tract involvement. Mantoux test may be positive. Biopsy of tissue may be confirmatory. ELISA and polymerase chain reaction tests are more specific for the diagnosis. Chest X-ray may show focus of infection in case of pulmonary involvement. To determine the extent of involvement of the genitourinary tract, conventional computed tomography (CT),[18] or CT intravenous pyelography may be done.
The response to antitubercular chemotherapy is excellent and earlier treatment is associated with excellent prognosis.
In Case 1, the penile lesion was probably of primary type and appeared on the glans penis and spread into both epididymides and right testis. Histopathology, positive Mantoux test, and ultrasonography findings helped us make a diagnosis, which was further confirmed by a good response to ATT. We could not determine the response to treatment in Case 2 as he did not follow-up.
CONCLUSION
Even though it is less common, genital TB should be considered in the differential diagnosis of a chronic, nonhealing ulcer over the penis, especially in endemic regions like India where TB is prevalent. Early institution of ATT is of utmost importance. As development of resistance is also a possibility, patients should be followed up till complete resolution of the lesions occur and they should be counseled to complete the treatment regimen.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Das A, Batabyal S, Bhattacharjee S, Sengupta A. A rare case of isolated testicular tuberculosis and review of literature. J Family Med Prim Care. 2016;5:468–70. doi: 10.4103/2249-4863.192334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cho YS, Joo KJ, Kwon CH, Park HJ. Tuberculosis of testis and prostate that mimicked testicular cancer in young male soccer player. J Exerc Rehabil. 2013;9:389–93. doi: 10.12965/jer.130046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shah H, Shah K, Dixit R, Shah KV. Isolated tuberculous epididymo-orchitis. Indian J Tuberc. 2004;51:159–62. [Google Scholar]
- 4.Gurubacharya RL, Gurubacharya SM. A 14-year-old boy with isolated tuberculous orchitis. J Nepal Paediatr Soc. 2009;29:30–2. [Google Scholar]
- 5.Amir-Zargar MA, Yavangi M, Ja'fari M, Mohseni MJ. Primary tuberculosis of glans penis: A case report. Urol J. 2004;1:278–9. [PubMed] [Google Scholar]
- 6.Zajaczkowski T. Genitourinary tuberculosis: Historical and basic science review: Past and present. Cent European J Urol. 2012;65:182–7. doi: 10.5173/ceju.2012.04.art1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lenk S, Schroeder J. Genitourinary tuberculosis. Curr Opin Urol. 2001;11:93–8. doi: 10.1097/00042307-200101000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Narayana AS, Kelly DG, Duff FA. Tuberculosis of the penis. Br J Urol. 1976;48:274. doi: 10.1111/j.1464-410x.1976.tb03018.x. [DOI] [PubMed] [Google Scholar]
- 9.Aires NB, Santi CG, Nico MM. Tuberculid of the glans penis. Acta Derm Venereol. 2006;86:552–3. doi: 10.2340/00015555-0139. [DOI] [PubMed] [Google Scholar]
- 10.Kashima M, Mori K, Kadono T, Nakabayashi Y, Shibayama E, Mizoguchi M. Tuberculide of the penis without ulceration. Br J Dermatol. 1999;140:757–9. [PubMed] [Google Scholar]
- 11.Merchant SA. Tuberculosis of the genitourinary system. Indian J Radiol Imaging. 1993;3:275–86. [Google Scholar]
- 12.Devine JC, Jordan GH, Schlossberg SM. Surgery of the penis and urethra. In: Walsh PC, Retik AB, Stamey TA, Vaughan ED, editors. Campbell's Urology. 6th ed. Philadelphia, PA: W. B. Saunders; 1992. p. 2960. [Google Scholar]
- 13.Nishigori C, Taniguchi S, Hayakawa M, Imamura S. Penis tuberculides: Papulonecrotic tuberculides on the glans penis. Dermatologica. 1986;172:93–7. doi: 10.1159/000249305. [DOI] [PubMed] [Google Scholar]
- 14.Lewis EL. Tuberculosis of the penis: A report of five cases and a complete review of the literature. J Urol. 1946;56:737–45. doi: 10.1016/S0022-5347(17)69866-5. [DOI] [PubMed] [Google Scholar]
- 15.Sekhon GS, Lal MM, Dhall JC. Tuberculosis of penis. J Indian Med Assoc. 1971;56:316–8. [PubMed] [Google Scholar]
- 16.Agarwalla B, Mohanty GP, Sahu LK, Rath RC. Tuberculosis of the penis: Report of 2 cases. J Urol. 1980;124:927. doi: 10.1016/s0022-5347(17)55735-3. [DOI] [PubMed] [Google Scholar]
- 17.Venkataramaiah NR, van Raalte JA, Dutta SN. Tuberculous ulcer of the penis. Postgrad Med J. 1982;58:59–60. doi: 10.1136/pgmj.58.675.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Venyo AK. Tuberculosis of the Penis: A Review of the Literature. Scientifica (Cairo) 2015;2015:601624. doi: 10.1155/2015/601624. [DOI] [PMC free article] [PubMed] [Google Scholar]


