Abstract
In spite of various psychoactive substances (including tobacco, alcohol, and opioids) being closely associated with development of metabolic syndrome (MS), little research exists on the prevalence of MS among persons with addictive disorders. The criteria used to diagnose MS varied across these studies, and part of the variation in the prevalence rate (5.1%–30.6%) could be attributable to this fact. The current study aimed to assess the prevalence of MS in patients with alcohol dependence syndrome (ADS) and opioid dependence syndrome (ODS) using revised National Cholesterol Education Programme Adult Treatment Panel (NCEP ATP-III) criteria and International Diabetes Federation (IDF) criteria. We tried to assess the impact of the choice of the diagnostic criteria on the prevalence rate of MS in the persons with ADS and ODS. This was a cross-sectional observational study. Semi-structured pro forma was used to collect information on the sociodemographic profile and clinical profile. Anthropometric measurements included waist circumference, height, weight, and body mass index (BMI). The systolic and diastolic blood pressure, fasting blood sugar (FBS), serum triglycerides, and serum high-density lipoprotein were measured. Patients were diagnosed as having MS by using revised NCEP ATP-III and IDF criteria. Statistical analysis was done by Chi-square (Fischer's exact test), independent sample Student's t-test, and Cohen's kappa. Among the individuals with ADS, the prevalence of MS was found to be 20.8% and 9.9% according to revised NCEP ATP III criteria and IDF criteria, respectively. Among individuals with ODS, the prevalence of MS was found to be 20.3% and 5.1% according to revised NCEP ATP III criteria IDF criteria, respectively. While there was a good degree of concordance between IDF and modified NCEP-ATP III criteria for MS for ADS (n = 256) (κ = 0.649, P < 0.001), the concordance was only fair for ODS (κ = 0.333, P < 0.001). The findings of our study thereby support the recommendation that revised NCEP ATP-III criteria is better choice than IDF criteria for identification of MS in individuals having addictive disorders, especially opioid dependence.
Keywords: Addictive disorders, alcohol use disorder, metabolic syndrome, opioid use disorder
INTRODUCTION
Metabolic syndrome (MS) is a constellation of several risk factors such as obesity, insulin resistance, dyslipidemia, and hypertension, which predicts higher risk of developing diabetes mellitus type II, coronary heart disease and cardiovascular disease and all-cause mortality.[1,2]
The most commonly used criteria for diagnosing MS include the Revised National Cholesterol Education Programme Adult Treatment Panel (NCEP ATP-III) and International Diabetes Federation (IDF) criteria. Literature suggests that Revised NCEP ATP-III criteria may be better than IDF criteria for diagnosing MS.[3,4]
The main difference between these two criteria is the presence of increased waist circumference as a mandatory requirement of IDF criteria. Wait circumference is a measure of truncal obesity. Interestingly, the clinical observation of persons with opioid dependence suggests that many of them are malnourished and truncal obesity is a rather uncommon observation.
Both MS and psychoactive substance use have been found to be bidirectionally implicated in the development of complications, compliance, and treatment outcomes.[5] In spite of various psychoactive substances (including tobacco, alcohol, and opioids) being closely associated with the development of MS, little research exists on the prevalence of MS among persons with addictive disorders.[6,7,8,9,10,11,12] The criteria used to diagnose MS varied across these studies, and part of the variation in the prevalence rate (5.1%–30.6%) could be attributable to this fact. The current study aimed to assess the prevalence of MS in patients with alcohol dependence syndrome (ADS) and opioid dependence syndrome (ODS) using revised NCEP ATP-III criteria and IDF criteria. We tried to assess the impact of the choice of the diagnostic criteria on the prevalence rate of MS in the persons with ADS and ODS.
MATERIALS AND METHODS
Setting and subjects
The study was a cross-sectional and was carried out at the National Drug Dependence Treatment Center. Consecutive patients of ADS and ODS diagnosed according to Diagnostic and Statistical Manual of Mental Disorders-IV-TR criteria and seeking in patient treatment were screened and recruited as per selection criteria. Individuals having any substance dependence other than nicotine and any psychiatric comorbidity were excluded. Ethical approval was taken from the institute ethics committee.
Semistructured pro forma was used to collect information on the sociodemographic profile, clinical profile including age of onset of substance use, duration of substance use, and dietary history. Anthropometric measurements included waist circumference, height, weight, and body mass index (BMI). The systolic and diastolic blood pressure, fasting blood sugar (FBS), serum triglyceridess, and serum high-density lipoprotein were measured. Patients were diagnosed as having MS by using revised NCEP ATP-III and IDF criteria.
Urine drug screening was carried out using thin layer chromatography to exclude those who used other psychoactive substances.
Statistical analysis
Data analysis was done by statistical package SPSS (version 17.0; SPSS Inc. Chicago, IL, USA). Sociodemographic and clinical data were tabulated, and descriptive analysis including percentages, frequency, measures of central tendencies, and tests for normal distribution was performed. Chi-square (Fischer's exact test) was used to compare the prevalence of MS as diagnosed by the two criteria. For assessing group differences of continuous variables, independent sample Student's t-test was used. We calculated the Cohen's kappa to assess the degree of concordance between the diagnosis of MS based on the two criteria for individuals with ADS and ODS. The two-tailed P < 0.05 was considered statistically significant.
RESULTS
A total of 160 male individuals were recruited, out of which 101 individuals were diagnosed with ADS and 59 with ODS. The mean age of individuals with ADS was 38.86 (standard deviation [SD] = 8.79) years and that of individuals with ODS was 35.20 (SD = 11.06) years. >90% had a history of using heroin and 16.95% were intravenous drug users.
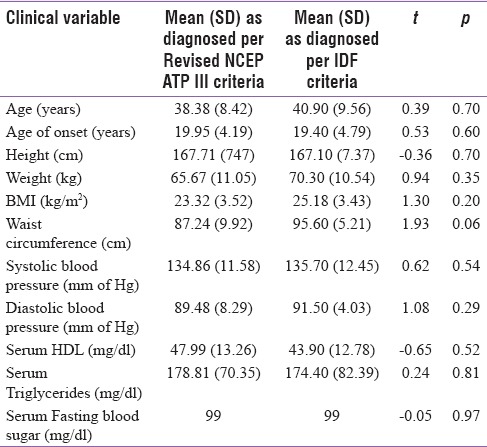
Among the individuals with ADS, the prevalence of MS was found to be 20.8% and 9.9% according to revised NCEP ATP III criteria and IDF criteria, respectively. The difference was statistically significant (χ2 =54.27, df =1, P < 001). No significant difference was found in the anthropometric measures and components of MS between those diagnosed by revised NCEP ATP III criteria and IDF criteria [Table 1].
Table 1.
Comparison of clinical variables of subjects with ADS diagnosed as MS as per revised NCEP ATP III criteria and IDF criteria
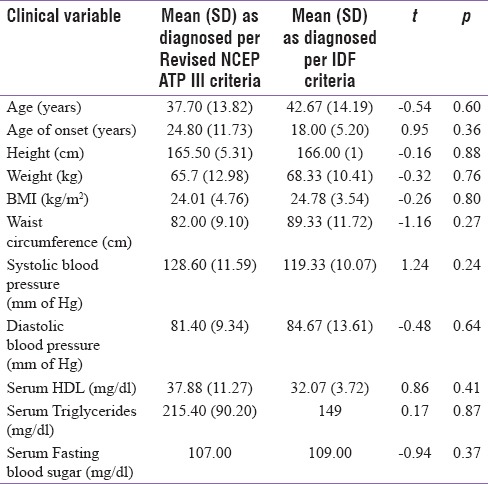
Among individuals with ODS, the prevalence of MS was found to be 20.3% and 5.1% according to revised NCEP ATP III criteria IDF criteria, respectively. The difference was statistically significant (χ2 =14.40, df =1, P = 0.01). No significant difference was found in the anthropometric measures and components of MS between those diagnosed by revised NCEP ATP III criteria and IDF criteria [Table 2].
Table 2.
Comparison of clinical variables of subjects with ODS diagnosed as MS as per revised NCEP ATP III criteria and IDF criteria
While there was a good degree of concordance between IDF and modified NCEP-ATP III criteria for MS for ADS (n = 256) (κ = 0.649, P < 0.001), the concordance was only fair for ODS (κ = 0.333, P < 0.001).
DISCUSSION
In the current study, the prevalence of MS in individuals with ADS and ODS was higher by using revised NCEP ATP III criteria as compared to IDF criteria. The prevalence of MS was comparable among individuals of ADS (20.8%) as well as ODS (20.3%) as per revised NCEP ATP III. However, by IDF criteria, the prevalence of MS was higher in patients of ADS (9.9%) when compared to ODS (5.1%). This observation can be attributed to the fact that the presence of increased waist circumference is a mandatory requirement of IDF criteria of MS. While the IDF has proposed a criteria with ethnic and racial specific cut-offs for waist-circumference, it is likely to miss many potential cases who would be identified as having MS using the NCEP ATP-III criteria.[13]
Alcohol has been found to have complex relationship with weight gain and obesity. Interestingly, heavy drinking has been consistently related to weight gain and obesity in recent prospective studies.[14] Furthermore, obesity was associated with alcohol use disorders but not for other addictive disorders in an epidemiological study.[15] The association between being overweight and psychoactive substance abuse or dependence was found to be inversely related among men.[16] While opioid use has also been auspicated with impaired glycemic control and weight gain, the association is strongest among patients who are receiving opioid agonists as part of treatment. The persons with ODS in our clinical setting are less likely to have truncal obesity. Dietary neglect due to financial constraints, a general neglect of personal care, and presence of co-occurring medical disorders could be some reason for this observation.
There are four previous published studies from India that have assessed MS among individuals with ADS and ODS. All these studies are from the same center. The prevalence of the MS has varied considerably between these studies.
One of the these studies reported the prevalence of MS based on the IDF criteria to be 21.6% and 9.6% among individuals with ADS and ODS, respectively.[12] Another study from the same center reported the prevalence of the MS (as per IDF criteria) to be 24.6% and 29.3% for subjects with ADS and ODS, respectively.[11]
There was only fair concordance for the diagnosis of MS among individuals with ODS based on the two criteria in the current study. However, a previous Indian study reported a high concordance between IDF and modified NCEP-ATP III criteria for MS among the individuals with substance use disorder seeking in-patient treatment. The prevalence rate of MS in the entire study sample was 9.4% by IDF criteria and 10.9% by modified NCEP ATP-III.[9]
Another study from the same center reported the prevalence of MS among individuals with ADS to be 27% and 18% using IDF and NCEP ATP-III criteria, respectively.[10] The concordance for MS between the two classificatory systems was low with Cohen's kappa being 0.522. The authors attributed the higher prevalence of MS by IDF criteria to the lower cutoff of the waist circumference as compared to the NCEP ATP-III criteria. While this rate is comparable to the one observed for the individuals with ADS in the current study, the prevalence of MS was higher using the NCEP ATP-III criteria in the current study.
The study population from the two settings is distinct from each other on certain sociodemographic variables. Majority of the individuals in the current study were currently unemployed and were staying in a rural background. In the other studies from India, the majority of the individuals were employed and lived in urban settings. Furthermore, while the current study excluded the individuals with comorbidities, the other Indian studies included individuals with physical and psychiatric comorbidities. This can explain, at least in part, the difference observed in the prevalence rate of MS across these two settings.
In our study, almost 50% and 75% cases of MS diagnosed by revised NCEP ATP III criteria in individuals of ADS and ODS, respectively, were missed by the IDF criteria. This has important and serious public health implications in terms of management as a sizeable proportion of cases being missed by utilizing IDF criteria which have been supported by existing literature and thereby making a strong case against the waist circumference being a mandatory criterion. Hence, it is recommended to use revised NCEP ATP III criteria for screening for MS, at least among individuals with ODS.
Strengths of the current study include inclusion of individuals with no psychiatric comorbidity, assessment the metabolic parameters when patients were not experiencing withdrawal. Limitations of the study are small sample size, only male sample, nonexclusion of nicotine dependence, and not assessing physical activity. However, no significant correlation was obtained between tobacco use and MS among alcohol and opioid users in the previous studies.[9,11]
CONCLUSIONS
The findings of our study thereby support the recommendation that revised NCEP ATP-III criteria is better choice than IDF criteria for identification of MS in individuals having addictive disorders, especially opioid dependence.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Alberti KG, Zimmet P, Shaw J. Metabolic syndrome – A new world-wide definition. A Consensus statement from the international diabetes federation. Diabet Med. 2006;23:469–80. doi: 10.1111/j.1464-5491.2006.01858.x. [DOI] [PubMed] [Google Scholar]
- 2.Vidigal Fde C, Ribeiro AQ, Babio N, Salas-Salvadó J, Bressan J. Prevalence of metabolic syndrome and pre-metabolic syndrome in health professionals: LATINMETS brazil study. Diabetol Metab Syndr. 2015;7:6. doi: 10.1186/s13098-015-0003-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chackrewarthy S, Gunasekera D, Pathmeswaren A, Wijekoon CN, Ranawaka UK, Kato N, et al. A comparison between revised NCEP ATP III and IDF definitions in diagnosing metabolic syndrome in an urban Sri Lanka population: The Ragama health study. ISRN Endocrinol. 2013;2013:320176. doi: 10.1155/2013/320176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moy FM, Bulgiba A. The modified NCEP ATP III criteria maybe better than the IDF criteria in diagnosing metabolic syndrome among malays in Kuala Lumpur. BMC Public Health. 2010;10:678. doi: 10.1186/1471-2458-10-678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Virmani A, Binienda ZK, Ali SF, Gaetani F. Metabolic syndrome in drug abuse. Ann N Y Acad Sci. 2007;1122:50–68. doi: 10.1196/annals.1403.004. [DOI] [PubMed] [Google Scholar]
- 6.Kahl KG, Greggersen W, Schweiger U, Cordes J, Correll CU, Ristow J, et al. Prevalence of the metabolic syndrome in men and women with alcohol dependence: Results from a cross-sectional study during behavioural treatment in a controlled environment. Addiction. 2010;105:1921–7. doi: 10.1111/j.1360-0443.2010.03059.x. [DOI] [PubMed] [Google Scholar]
- 7.Teixeira PJ, Rocha FL. The prevalence of metabolic syndrome among psychiatric inpatients in Brazil. Rev Bras Psiquiatr. 2007;29:330–6. doi: 10.1590/s1516-44462007000400007. [DOI] [PubMed] [Google Scholar]
- 8.Jarvis CM, Hayman LL, Braun LT, Schwertz DW, Ferrans CE, Piano MR, et al. Cardiovascular risk factors and metabolic syndrome in alcohol- and nicotine-dependent men and women. J Cardiovasc Nurs. 2007;22:429–35. doi: 10.1097/01.JCN.0000297387.21626.88. [DOI] [PubMed] [Google Scholar]
- 9.Nebhinani N, Gupta S, Mattoo S, Basu D. Prevalence of the MSin substance-dependent men. German J Psychiatry. 2013;16:61–7. [Google Scholar]
- 10.Aneja J, Basu D, Mattoo SK, Kohli KK. Metabolic syndrome in alcohol-dependent men: A cross-sectional study. Indian J Psychol Med. 2013;35:190–6. doi: 10.4103/0253-7176.116253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mattoo SK, Chakraborty K, Basu D, Ghosh A, Vijaya Kumar KG, Kulhara P, et al. Prevalence & correlates of metabolic syndrome in alcohol & opioid dependent inpatients. Indian J Med Res. 2011;134:341–8. [PMC free article] [PubMed] [Google Scholar]
- 12.Mattoo SK, Nebhinani N, Aggarwal M, Basu D, Kulhara P. Metabolic syndrome among substance dependent men: A study from North India. Ind Psychiatry J. 2013;22:60–4. doi: 10.4103/0972-6748.123631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: A joint interim statement of the international diabetes federation task force on epidemiology and prevention; National heart, lung, and blood institute; American heart association; world heart federation; International atherosclerosis society; and international association for the study of obesity. Circulation. 2009;120:1640–5. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 14.Traversy G, Chaput JP. Alcohol consumption and obesity: An update. Curr Obes Rep. 2015;4:122–30. doi: 10.1007/s13679-014-0129-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Petry NM, Barry D, Pietrzak RH, Wagner JA. Overweight and obesity are associated with psychiatric disorders: Results from the national epidemiologic survey on alcohol and related conditions. Psychosom Med. 2008;70:288–97. doi: 10.1097/PSY.0b013e3181651651. [DOI] [PubMed] [Google Scholar]
- 16.Desai RA, Manley M, Desai MM, Potenza MN. Gender differences in the association between body mass index and psychopathology. CNS Spectr. 2009;14:372–83. doi: 10.1017/s1092852900023026. [DOI] [PMC free article] [PubMed] [Google Scholar]


