Abstract
Background:
Recent increase in the non-specific use of prokinetics in clinical practice may alter the etiological profile of hyperprolactinemia and galactorrhea. Hence, we have studied the etiological profile of patients presenting with galactorrhea and characteristics of drug-induced galactorrhea.
Materials and Methods:
This retrospective study was conducted at a tertiary health care center from South India. Patients who presented with or referred for galactorrhea and/or hyperprolactinemia to the Department of Endocrinology between January 2017 and December 2017 were included in the study.
Results:
Forty women presented with or referred for galactorrhea to the Department of Endocrinology during the study period. Thirty-two patients had received drugs that are associated with hyperprolactinemia (levosulpiride in 15, domperidone in 13, ranitidine in 2, oral contraceptive pill in 1, and amisulpiride in 1) of whom etiology was proved in 27 patients, whereas in four patients the cause was inconclusive due to lack of follow-up. The patient on amisulpiride was found to have concomitant pituitary microadenoma. Idiopathic galactorrhea (n = 2), idiopathic hyperprolactinemia (n = 2), and prolactinoma (n = 4) accounted for the remaining cases. Six patients with prokinetic-induced galactorrhea had received cabergoline inspite of which hyperprolactinemia and/or galactorrhea persisted and six patients had also undergone pituitary magnetic resonance imaging (MRI) for evaluation of galactorrhea.
Conclusions:
Prokinetic use is the most common cause of galactorrhea in our study and often was investigated with costly tests and treated with D2 agonists unnecessarily. Hence, there is a need to ensure measures to reduce the non-specific use of prokinetics and increase awareness regarding the occurrence of galactorrhea with prokinetics use, to reduce unnecessary investigations and treatment.
Keywords: Domperidone, galactorrhea, hyperprolactinemia, levosulpiride, prokinetics
INTRODUCTION
Galactorrhea is the secretion of milky discharge from breast in men or women who are not breastfeeding for one year. It may result from excessive secretion of prolactin or increased sensitivity of breast tissue to prolactin. Most of the times it is caused by elevation of prolactin and is often associated with menstrual abnormalities.[1] Prolactin is a peptide hormone released from anterior pituitary which in turn is regulated predominantly by inhibitory effect of dopamine and to a small extent by the stimulatory effect of thyrotropin-releasing hormone, oxytocin, vasopressin, vasoactive intestinal peptide and angiotensin 2.[2] Any condition that produces imbalance in these substances can lead to elevation of prolactin and cause galactorrhea and menstrual abnormalities. Varied conditions like stimulation of breast, chest wall diseases, drugs or pathological conditions like pituitary tumors can cause galactorrhea as a symptom.[3] Drugs like antipsychotics, antidepressants, estrogen-containing drugs, prokinetics, antihypertensives, opioids that act by blocking D2 receptors or decrease synthesis of dopamine can reduce the hypothalamic inhibitory tone on pituitary and thereby can increase in prolactin secretion which may cause galactorrhea.[3,4] Usually the prolactin elevation due to drugs is <100 ng/ml except for few antipsychotics which can increase up to 250 ng/ml.[4] According to Petit et al. the rates of hyperprolactinemia according to therapeutic drug classes were 31% associated with neuroleptics, 28% with neuroleptic-like drugs, 26% with antidepressants, 5% with H2-receptor antagonists, and 10% with other drugs.[5] Recent increased use of D2 blockers for the treatment of gastro esophageal reflux disease (GERD) seems to have increased the prevalence of hyperprolactinemia and galactorrhea due to D2 blockers as we have observed in our clinical practice. A recently published case report suggested that levosulpiride-induced hyperprolactinemia could be up to 273 ng/ml.[5,6,7] So, the etiological profile of hyperprolactinemia and galactorrhea might also change and the level of hyperprolactinemia due to drugs needs reconsideration. Hence, we have studied the etiological profile of patients presenting with galactorrhea and characteristics of drug-induced galactorrhea.
MATERIALS AND METHODS
This is a retrospective observational study conducted at Vydehi Institute of Medical Sciences and Research Center, Bengaluru. Patients who were aged >18 years and presented with or referred for galactorrhea and/or hyperprolactinemia to the Department of Endocrinology between January 2017 and December 2017 were included in the study. Hyperprolactinemia was defined as serum prolactin level >25 ng/ml.[3] Galactorrhea was defined as secretion of milky discharge from breast after 1 year of cessation of breastfeeding.[1] It is categorized as expressive if milky discharge is expressed only on application of pressure and spontaneous, if milky discharge occurs without application of pressure. Galactorrhea was considered to be subsided, if no milky discharge on application of pressure. Improvement in galactorrhea is defined as decrease in frequency or quantity of the discharge. Patients who had not reported for persistence of galactorrhea after normalization of serum prolactin and/or improvement of galactorrhea were assumed as galactorrhea subsided. Patients who were pregnant or breastfeeding or had breast fed during the previous year were excluded from the study.
The management protocol followed in the Department of Endocrinology for galactorrhea/hyperprolactinemia included a detailed history regarding drug intake, duration of drug use, headache, visual disturbances, vomiting, menstrual abnormalities, examination for the presence of galactorrhea, visual field defects, and papilledema if required.[1,3] Baseline serum prolactin was tested for those who did not had baseline serum prolactin. If serum prolactin was normal, then it was labeled as idiopathic galactorrhea and patients were assured. Those who had elevated serum prolactin were evaluated further. In patients who had a history of drug intake associated with hyperprolactinemia (D2 blockers, dopamine synthesis inhibitors, opioids, H2 blockers, neuroleptics, antidepressants, and anti-hypertensives), it was confirmed either by verification of the prescription or the drug itself. After confirmation of consumption of the drug that can induce hyperprolactinemia, patients were asked to withhold the drug for a minimum period of 72 hours and serum prolactin and presence of galactorrhea were reassessed. If serum prolactin level decreased by 50% or more from the baseline with or without improvement in galactorrhea, then the patient was considered as drug-induced galactorrhea. These patients were asked to review after 2 weeks and then after 1 month, all galactorrhea or hyperprolactinemia persisted. The time taken for reduction of galactorrhea was noted. In patients who did not had history of drug intake, they were further evaluated with thyroid function tests, liver function tests, and renal function tests. If the above tests were normal, MRI of the pituitary with dynamic contrast scans was performed to look for pituitary hypothalamic lesions that may be associated with hyperprolactinemia such as pituitary tumors, stalk thickening, or hypothalamic lesions. If no cause was identified for hyperprolactinemia, then it was considered as idiopathic hyperprolactinemia. The same protocol had been followed in the department during the study period.
Medical records of the patients were reviewed and detailed history regarding galactorrhea, menstrual abnormalities, headache, visual disturbances, drug intake, baseline and follow-up serum prolactin levels, and improvement in galactorrhea were captured in a pre-designed case record form. Serum prolactin was assayed by chemiluminescence immunoassay using Unicel DxC 600 Synchron®, Beckman Coulter Ireland Inc. The assay sensitivity was 0.25 ng/ml and precision was <10% of CV across the reference range. Normal reference range for premenopausal women was 3.34–26.72 ng/ml. None of the patients were evaluated for macroprolactin (polyethylene glycol precipitation), whereas in two patients with normal serum prolactin, assay was repeated in serial dilutions to rule out the hook effect.
Statistical analysis
Data were analyzed using SPSS software version 21.1(IBM, Armonk, NY). Prevalence of causes of galactorrhea are expressed in absolute numbers or percentages as appropriate. Serum prolactin levels and duration of drug use are expressed as mean and SD and time to galactorrhea subsidence as median range.
RESULTS
Forty patients presented with or referred for galactorrhea to Department of Endocrinology, Vydehi Institute of Medical Sciences and Research Center during the study period. All of them were women. The mean age of presentation was 31.2 ± 6.95 years. Of these, 31 patients presented with galactorrhea (spontaneous or expressive), whereas the remaining nine were identified with galactorrhoea during their evaluation for infertility and/or oligomenorrhea. Baseline serum prolactin levels were available for 38 patients of whom 36 had elevated prolactin. In the records of other two patients, a mention of baseline hyperprolactinemia was there but exact values of serum prolactin were not available.
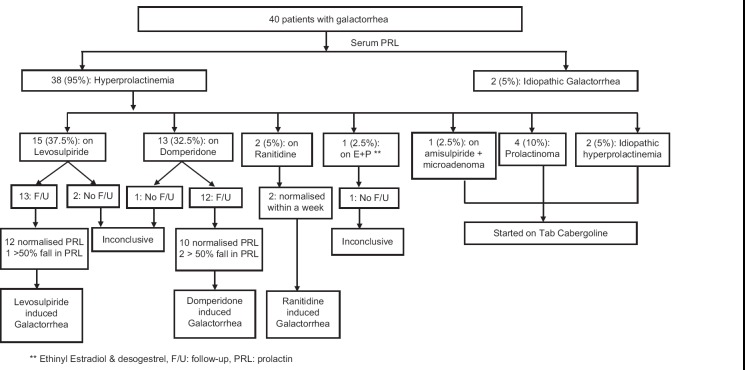
Etiological profile of galactorrhea patients is summarized in Figure 1. Idiopathic galactorrhea and idiopathic hyperprolactinemia accounted for two patients each. Four patients had prolactinoma. Thirty-two patients had received drugs associated with hyperprolactinemia of whom etiology was proved in 27 patients, whereas in four patients the cause was inconclusive due to lack of follow-up. One patient on amisulpiride had a concomitant pituitary microadenoma.
Figure 1.
Summary of etiological profile of galactorrhea
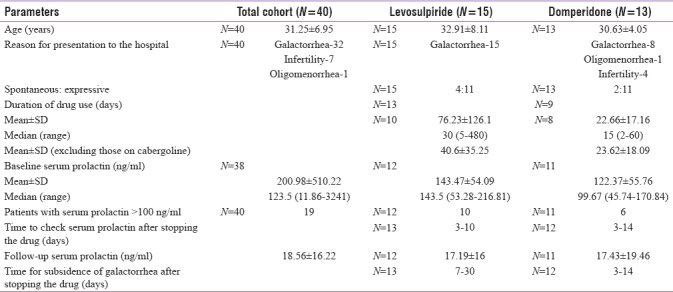
The mean serum prolactin for drug-induced galactorrhea was 133.38 ± 55.99 ng/ml (median: 140 ng/ml, range: 43.23–261.81 ng/ml) and for patients with pituitary adenoma median serum prolactin was 207 ng/ml (range: 140–3241 ng/ml). Characteristics of the total cohort, levosulpiride-associated galactorrhea, and domperidone-associated galactorrhea are summarized in Table 1. All except three patients with prokinetic-induced galactorrhea patients who followed-up had normalized serum prolactin levels within 3–7 days of stopping the drug and those who did not normalize had at least 50% fall in serum prolactin by 72 hours and later two patients normalized by 2 weeks of stopping the implicated drug. One patient with domperidone-induced hyperprolactinemia who had no further fall in serum prolactin even after 2 weeks of stopping the drug was evaluated further with thyroid, liver and renal function tests, and ultrasound pelvis and was diagnosed to have polycystic ovary syndrome.
Table 1.
Characteristics of the study cohort
Non-prokinetic drug-induced galactorrhea
Two patients on ranitidine were diagnosed with hyperprolactinemia while evaluating for infertility and were referred to our department. One patient had serum prolactin of 71 ng/ml and expressive galactorrhea. After stopping ranitidine for 72 hours, serum prolactin was 24.63 ng/ml and galactorrhea subsided after a week. Other patient was on ranitidine for 2 weeks. Baseline serum prolactin was not available for her, but she had hyperprolactinemia (serum prolactin: 42.45 ng/ml) on 5th day after stopping the drug and had expressive galactorrhea. On 8th day of stopping the drug her serum prolactin had reduced to 20.95 ng/ml. Galactorrhea stopped after another seven days. One patient who was on amisulpiride (200 mg/day) for 3 years for psychiatric illness, had amenorrhea and galactorrhea for 2 years. Her serum prolactin was 140 ng/ml. As the drug could not be withheld due to her illness, MRI pituitary was done which revealed a pituitary microadenoma of 2 mm. She was started on cabergoline 1 mg/week and amisulpiride dose was reduced to 150 mg/day. Three months later her serum prolactin had reduced to 76.78 ng/ml but with persisting galactorrhea and amenorrhea.
Menstrual abnormalities
Out of 37 patients, 14 had menstrual abnormalities in the form of oligomenorrhoea (11) and amenorrhea (3). Two of the amenorrhea patients had prolactinoma and one had levosulpiride-induced galactorrhea. The latter patient had amenorrhea prior to the use of levosulpiride. Of the 11 patients with oligomenorrhea, only four had developed menstrual irregularity after initiation of prokinetics. Two of them were using levosulpiride and two were using domperidone. One patient in levosulpiride group and one in domperidone group, who had menstrual irregularity were using drugs for more than a year. Other patient in domperidone group used for 2 months and levosulpiride group used for 20 days but had prior history of prokinetic drug intake on and off. One patient who was using domperidone for more than a year did not develop menstrual irregularity.
Drug-induced galactorrhea and D2 agonist treatment
Six patients with drug-induced galactorrhea (three levosulpiride induced and three domperidone induced) were using cabergoline by the time they presented to our department. One patient on levosulpiride used cabergoline (2 mg/week) for 18 months and then had been switched to oral bromocriptine for 6 months before presenting to us, whereas other two patients on levosulpiride had been treated with cabergoline (0.5 mg/week) for 2–6 weeks. One patient on domperidone used 0.5 mg twice a week for 2 weeks, whereas another patient on domperidone used the same dose for more than a year. The third patient on domperidone had persistent galactorrhea inspite of 0.5 mg twice a week and has had a dose escalation to 2 mg/week. All patients who were treated with D2 agonists with continued use of prokinetics, had persistent hyperprolactinemia and/or galactorrhea. After stopping both prokinetcs and cabergoline, serum prolactin levels were reduced, often below the normal range (0.35–1.07 ng/ml) and galactorrhea subsided within 2 weeks of stopping the implicated drug. One patient on amisulpiride was started on oral cabergoline by us, as the patient had associated pituitary adenoma and amisulpiride could not be withheld due to the disease. Even after 3 months of usage at 1 mg/week of cabergoline, hyperprolactinemia reduced from 140 to 76.78 ng/ml but galactorrhea and amenorrhea persisted. Six patients on prokinetics had undergone MRI pituitary for hyperprolactinemia and galactorrhea prior to the presentation to our department, of whom five had normal imaging findings, whereas one had partial empty sella.
DISCUSSION
The prevalence of drug-induced galactorrhea is on a rise and constituted 80% of galactorrhea cases in the present study. A study conducted approximately two decades ago by Zargar et al.[8] reported drug use in only 5% of 187 hyperprolactinemia cases. Unlike our study, the study by Zargar et al. included all hyperprolactinemia patients irrespective of the presence of galactorrhea. However, this difference in the study design is unlikely to account for the large difference in the prevalence of drug-induced galactorrhea, since 85% of patients in the Zargar et al. study also had galactorrhea. In another recent study from North India, 30.4% of hyperprolactinemia had drug-induced hyperprolactinemia.[9] In this study prokinetics accounted for 61.5% cases of drug-induced hyperprolactinemia whereas antipsychotics accounted 33.3% cases.[9] In our study also prokinetic drugs constituted majority (70%) cases of galactorrhea as compared to neuroleptics and neuroleptic like drugs in Petit et al. study.[6] This change in the etiological pattern of drug-induced galactorrhea may be due to recent increase in the use of prokinetics either due to their rampant prescription by physicians for non-specific symptoms or due to easy availability of prokinetics as over the counter medications. However, in the records of most of the patients it was not mentioned whether the implicated drug was prescribed by a physician or used as an over the counter medication.
A previous study has reported the time to onset of galactorrhea from initiation of drug as 27.2 ± 4.7 days and 23.2 ± 5.8 days for sulpiride and metoclopromide, respectively.[10] In our study the time to onset of galactorrhea from initiation of drug varied from 2 days to 3 months with a mean of 40.6 ± 35.25 and 22.66 ± 17.16 for levosulpiride- and domperidone-induced galactorrhea, respectively. This wide variation in the time to onset of galactorrhea can be due to various reasons such as variation in the perception of galactorrhea by patients, variation in the prokinetic ability to induce galactorrhea in an individual and variation in the sensitivity of the breast tissue of an individual to prolactin. In addition, prior use of hyperprolactinemia causing drugs, as had been vaguely reported in few patients, might have led to priming of breast tissue to prolactin and early onset of galactorrhea from initiation of drug.
Serum prolactin levels ranged from 43.23 ng/ml to 261.81 ng/ml for drug-associated galactorrhea and 140 ng/ml to 3241 ng/ml for prolactinoma. There was a considerable overlap between the serum prolactin levels of drug-induced galactorrhea and that of prolactinoma. The mean serum prolactin in levosulpiride group of our study was 143.47 ± 54.09 ng/ml which was similar to that reported by Kang et al.[11] where mean serum prolactin was 137.7 ± 68.6 ng/ml in females using levosulpiride (25 mg tid) for 2 weeks. A study by Fujino et al.[12] on the effect of intravenous domperidone on healthy volunteers had shown serum prolactin rise above 160 ng/ml in 15 minutes in some cases. Even low-dose amisulpiride can elevate serum prolactin levels to 110.7 ± 49.3 ng/ml in females.[13] So, drug intake can commonly lead to increase in serum prolactin more than 100 ng/ml and often more than 200 ng/ml. Few case reports have also reported that levosulpiride- and domperidone-induced galactorrhea can be associated with serum prolactin of more than 100 ng/ml and sometimes up to 271 ng/ml.[5,7,14,15] Hence, history of drug intake should always be elicited in all patients with galactorrhea or hyperprolactinemia before considering further evaluation even when serum prolactin is more than 100 ng/ml. This would avoid the unnecessary costly investigations like MRI pituitary and unnecessary treatment with D2 agonists as seen in our study. However, a serum prolactin of >300 ng/ml is unlikely to be associated with prokinetic use and can be considered for further evaluation of hyperprolactinemia.
Stopping the implicated drug for 72 hours or more and repeating serum prolactin level helps to confirm the drug-induced galactorrhea. However, it should be kept in mind that serum prolactin may not normalize by 72 hours in few patients and may take a week or more to do so. But all patients with drug-induced galactorrhea had at least 50% fall in serum prolactin by 72 hours of stopping the implicated drug and the same can be used as a criterion to define drug-induced hyperprolactinemia. These patients can be followed up till 2 weeks after stopping the drug for further normalization of serum prolactin.
A previous study has reported a very long time from stopping the implicated drug to subsidence of galactorrhea (50.0 ± 7.3 days in the sulpiride-treated patients and 56.6 ± 12.1 days in the metoclopramide-treated patients) which is much higher than that observed in our study. Although, this time was relatively shorter in our study, galactorrhea took longer time to subside than normalization of serum prolactin level. Hence, if serum prolactin is normalized, then the patient can be assured to wait for galactorrhea to subside spontaneously.
Although D2 agonists can normalize prolactin in few patients with drug-induced hyperprolactinemia, without stopping the implicated drug it may often fail to reduce galactorrhea and/or hyperprolactinemia as observed in our study.[10] It indicates that domperidone and levosulpiride may have stronger antagonistic action at central D2 receptors at the concentrations achieved with the doses used for GERD than agonistic action of cabergoline at the concentrations achieved with the doses used for hyperprolactinemia. Hence, whenever feasible, stopping the galactorrhea-associated drug is the appropriate treatment for drug-induced galactorrhea and not the treatment with D2 agonists. Interestingly, most of the patients who were treated with cabergoline for prokinetic-induced galactorrhea had low or low-normal serum prolactin levels after 3–14 days of stopping both the drugs. It may be due to long lasting D2 agonistic action of cabergoline than D2 antagonistic action of prokinetics. The study is limited by a small sample size and its retrospective nature.
CONCLUSIONS
Prokinetic use was the most common cause of galactorrhea in our study and often was investigated with costly tests and treated with D2 agonists unnecessarily. Hence, there is a need to ensure measures to reduce the non-specific use of prokinetics and increase awareness regarding the occurrence of galactorrhea with prokinetics use, to reduce unnecessary investigations and treatment. Our study also demonstrated that prokinetic-induced galactorrhea may not respond to cabergoline therapy and may take a longer time to subside than that taken for normalization of serum prolactin after stopping the implicated drug.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Huang W, Molitch ME. Evaluation and management of galactorrhea. Am Fam Phys. 2012;85:1073–80. [PubMed] [Google Scholar]
- 2.Melmed S. Mechanisms for pituitary tumorigenesis: The plastic pituitary. J Clin Invest. 2003;112:1603–18. doi: 10.1172/JCI20401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Melmed S, Casanueva FF, Hoffman AR, Kleinberg DL, Montori VM, Schlechte JA, et al. Diagnosis and treatment of hyperprolactinemia: An Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:273–88. doi: 10.1210/jc.2010-1692. [DOI] [PubMed] [Google Scholar]
- 4.Torre DL, Falorni A. Pharmacological causes of hyperprolactinemia. Ther Clin Risk Manag. 2007;3:929–51. [PMC free article] [PubMed] [Google Scholar]
- 5.Kuchay MS, Mithal A. Levosulpiride and Serum Prolactin Levels. Indian J Endocrinol Metab. 2017;21:355–8. doi: 10.4103/ijem.IJEM_555_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Petit A, Piednoir D, Germain ML, Trenque T. Drug-induced hyperprolactinemia: A case-non-case study from the national pharmacovigilance database. Therapie. 2003;58:159–63. doi: 10.2515/therapie:2003023. [DOI] [PubMed] [Google Scholar]
- 7.Rao R, Bhat R, Patil N, Bhushan L, Avinash A, Kunder SK. A rare instance of levosulpiride–induced galactorrhoea. Int J Pharm Pharm Sci. 2016;8:398–9. [Google Scholar]
- 8.Zargar AH, Laway BA, Masoodi SR, Bhat MH, Wani AI, Bashir MI, et al. Clinical and etiological profile of hyperprolactinemia--data from a tertiary care centre. J Assoc Phys India. 2005;53:288–90. [PubMed] [Google Scholar]
- 9.Kulshreshtha B, Pahuja I, Kothari D, Chawla I, Sharma N, Gupta S, et al. Menstrual cycle abnormalities in patients with prolactinoma and drug-induced hyperprolactinemia. Indian J Endocrinol Metab. 2017;21:545–50. doi: 10.4103/ijem.IJEM_515_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aono T, Shioji T, Kinugasa T, Onishi T, Kurachi K. Clinical and endocrinological analyses of patients with galactorrhea and menstrual disorders due to sulpiride or metoclopramide. J Clin Endocrinol Metab. 1978;47:675–80. doi: 10.1210/jcem-47-3-675. [DOI] [PubMed] [Google Scholar]
- 11.Kang CD, Song CW, Lee JW, Hur BW, Jeen MYT, Chun HJ, et al. Effects of Levosulpiride in Patients with Nonspecific Esophageal Motility Disorder. Kor J Neurogastroenterol Motil. 1999;5:111–8. [Google Scholar]
- 12.Fujino T, Kato H, Yamashita S, Aramaki S, Morioka H, Koresawa M, et al. Effects of domperidone on serum prolactin levels in human beings. Endocrinol Jpn. 1980;7:521–5. doi: 10.1507/endocrj1954.27.521. [DOI] [PubMed] [Google Scholar]
- 13.Lee BH, Kang SG, Kim TW, Lee HJ, Yoon HK, Park YM. Hyperprolactinemia induced by low-dosage amisulpride in Korean psychiatric patients. Psychiatry Clin Neurosci. 2012;66:69–73. doi: 10.1111/j.1440-1819.2011.02296.x. [DOI] [PubMed] [Google Scholar]
- 14.Patrascu OM, Chopra D, Dwivedi S. Galactorrhoea: Report of two cases. Mædica. 2015;10:136–9. [PMC free article] [PubMed] [Google Scholar]
- 15.Poovathingal MA, Bhat R, Ramamoorthi Domperidone induced galactorrhea: An unusual presentation of a common drug. Indian J Pharmacol. 2013;45:307–8. doi: 10.4103/0253-7613.111913. [DOI] [PMC free article] [PubMed] [Google Scholar]