Abstract
Background:
The indications for surgery in thyroiditis vary from compressive symptoms to cosmesis. We analyzed the complications in patients who underwent total thyroidectomy (TT) in goiters associated with thyroiditis.
Materials and Methods:
This retrospective study was done in an endocrine surgical center over 4 years. A total of 724 patients, who underwent TT for benign thyroid disorders, were included in the study. Patients were divided into two groups based on histopathology into Group A (nonthyroiditis cases) and Group B (thyroiditis cases); Group B is subdivided into Group B1 (nodular goiter with associated thyroiditis) and Group B2 (Hashimoto's thyroiditis). The preoperative parameters analyzed were serum calcium, serum Vitamin D, serum parathyroid hormone (PTH), and vocal cord status. The intraoperative parameters observed were operating time, parathyroid preservation, and autotransplantation and course of recurrent laryngeal nerve (RLN). Postoperative parameters monitored were serum calcium, serum PTH, serum magnesium, signs and symptoms of hypocalcemia, and vocal cord status. Follow-up was done at 6 months with serum calcium, serum PTH, and video laryngoscopy.
Results:
Both groups were age and sex matched. All preoperative and intraoperative parameters were comparable among groups. Both transient complications (<6 months) were higher in Group B than A. Transient hypocalcemia was higher in Group B (39.70%) than Group A (24.77%) (P = 0.001). Transient hypocalcemia was higher in Group B1 (36.58%) than Group B2 (44.44%) (P = 0.014). Transient RLN palsy was higher in Group B (9.55%) than Group A (7.52%) (P = 0.040). Transient RLN palsy was higher in Group B1 (8.53%) than Group B2 (11.11%) (P = 0.039). Permanent hypoparathyroidism and permanent RLN palsy were comparable between the Groups A and B and between Groups B1 and B2.
Conclusion:
The incidences of transient complications are higher in patients with thyroiditis. Careful analysis of surgical indications will avoid unnecessary surgery in thyroiditis cases.
Keywords: Hypocalcemia, recurrent laryngeal nerve palsy, thyroiditis
INTRODUCTION
Hashimoto's thyroiditis is an autoimmune disorder of thyroid gland, resulting in destruction of thyroid parenchyma leading to reduction in normal thyroid function.[1] The prevalence of thyroiditis is higher in iodine-sufficient areas. The incidence of thyroiditis as well as the degree of lymphocytic infiltration in the thyroid gland increases gradually and in dose-dependent manner.[2] Patients with thyroiditis are generally treated conservatively with medical therapy using levothyroxine, in an attempt to decrease the thyroid volume and to supplement thyroid hormone.[3] However, there are certain circumstances in which patients with thyroiditis require surgical management. The indications for surgery range from suspicion of malignancy goiter that is increasing in size to persistent symptoms not controlled with medical management.[4] Thyroidectomy is not generally recommended to patients because of the inflammatory process associated with thyroiditis. The thyroid gland tends to adhere more to its anatomical surroundings, which may increase the risk of injury to parathyroid glands and recurrent laryngeal nerve (RLN).[4] In this study, we performed analysis on the incidence of both transient and permanent complications in patients undergoing total thyroidectomy in goiters associated with thyroiditis in South Indian population. The coastal areas of south India has a higher prevalence of Thyroiditis.[5]
MATERIALS AND METHODS
This retrospective study was done in the Department of Endocrine Surgery, Madras Medical College, a tertiary care center in coastal South India. A total of 724 patients, who underwent total thyroidectomy for benign thyroid disorders over a period of 4 years from January 2012 to December 2015, were included in the study. Institutional Ethical Committee approval was obtained (22022017 (II) dated 21.02.2017).
Exclusion criteria in this study comprise patients with proven or suspicious of malignancy, reoperative surgery, abnormal renal function, patients already on supplemental calcium, and Vitamin D. The various indications for surgery were given in Table 1.
Table 1.
Indications for surgery
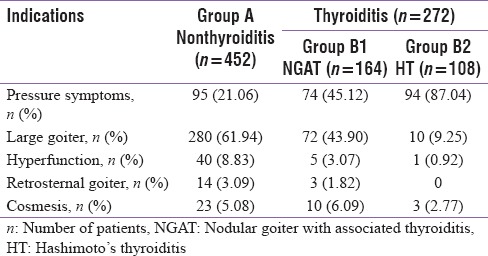
The most common indications for thyroidectomy are large goiters causing compressive symptoms (dysphagia, choking sensation, or voice change), suspicious or proven malignancy, retrosternal extension, toxic multinodular goiter, and cosmesis.
A total of 724 cases comprising 108 males and 616 females were enrolled in the study. All patients were divided into two groups based on histopathology into nonthyroiditis cases and thyroiditis cases (Hashimoto's thyroiditis [HT] and nodular goiter with associated thyroiditis [NGAT]). Out of 724 cases, 452 cases belonged to Group A (nonthyroiditis cases, n = 452/724 [62.4%]) and 272 cases belonged to Group B (thyroiditis cases, n = 272/724 [37.6%]).
The Group B is further subdivided into two groups, Group B1 (NGAT, n = 164/272 [60.29%]) and Group B2 (Hashimoto's thyroiditis [HT], n = 108/272 [39.71%]).
The preoperative biochemical parameters analyzed were serum calcium, serum magnesium, serum intact parathyroid hormone (serum PTH) (Cobas-E 411; Roche Diagnostics, Tokyo), and serum 25-hydroxyvitamin D (25-[OH]D) (Diasorin; Liaison, von Hevesy-Strasse, Dietzenbach). Preoperative video laryngoscopy is done for vocal cord analysis.
The intraoperative parameters included mean operating time, course of RLN, parathyroid preservation, and autotransplantation. Autotransplantation of parathyroid gland was done, only in case of inadvertent parathyroidectomy.
Postoperative parameters analyzed were signs and symptoms of hypocalcemia, serum calcium, serum magnesium, serum intact PTH, and vocal cord analysis.
Symptoms monitored for mild hypocalcemia are perioral numbness, tingling, and paresthesia of the distal extremities. Occasional muscle cramping was considered as moderate hypocalcemia. For severe hypocalcemia, the criteria are severe muscle cramps, tetanic muscle cramps, carpopedal spasm, seizures, life-threatening laryngospasm, and coma were considered. Standard Chvostek's and Trousseau's sign was monitored in the postoperative period.
Patients were followed up with serum calcium, serum PTH, and video laryngoscopy after 6 months of TT.
Complications which were present less than 6 months were termed as transient complications and which continues after 6 months were considered as permanent complications.
Statistical analysis was done using SPSS software (IBM-SPSS statistics 22.0; SPSS Inc., Chicago, IL, USA). Data were expressed as mean ± standard deviation (minimum-maximum). Multivariate analysis was done using logistic regression analysis. Categorical data analysis was done using Chi-square test and student t-test. P < 0.05 was considered statistically significant.
RESULTS
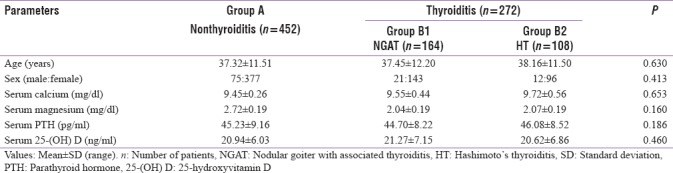
The mean age of the study population among groups was 37.32 ± 11.51 years in Group A, 37.45 ± 12.20 years in Group B1, and 38.16 ± 11.50 years in Group B2. The mean age was comparable among study groups (P = 0.630).
The sex ratio (male:female) among study group was 75:377 in Group A, 21:143 in Group B1, and 12:96 in Group B2. The sex ratio was comparable among study groups (P = 0.413).
The baseline serum calcium (mg/dl) in Group A was 9.45 ± 0.26, Group B1 was 9.55 ± 0.44, and Group B2 was 9.72 ± 0.56. The preoperative serum calcium was comparable among the study groups (P = 0.653).
The baseline serum magnesium (mg/dl) in Group A was 2.72 ± 0.19, Group B1 was 2.04 ± 0.19, and Group B2 was 2.07 ± 0.19. The preoperative serum magnesium was comparable among the study groups (P = 0.160).
The baseline serum intact PTH (pg/ml) in Group A was 45.23 ± 9.16, Group B1 was 44.70 ± 8.22, and Group B2 was 46.08 ± 8.52. The preoperative serum intact PTH was comparable among the study groups (P = 0.186).
The preoperative serum 25-(OH) D (ng/ml) in Group A was 20.94 ± 6.03, Group B1 was 21.27 ± 7.15, and Group B2 was 20.62 ± 6.86. The preoperative serum 25-(OH) D was comparable among the study groups (P = 0.460). The preoperative parameters were documented in Table 2.
Table 2.
Intraoperative parameters
The mean operative time (minutes) in Group A was 101.11 ± 10.84, Group B1 was 102.05 ± 12.86, and Group B2 was 103.02 ± 11.64. The mean operative time was comparable between the three study groups (P = 0.398).
The mean number of parathyroid glands identified and preserved in Group A was 3.49 ± 0.43, Group B1 was 3.69 ± 0.50, and Group B2 was 3.78 ± 0.46. The mean number of parathyroid glands identified and preserved was comparable between the three study groups (P = 0.142).
The number of patients who had parathyroid gland autotransplantation was 106/452 (23.5%) in Group A, 33/164 (20.1%) in Group B1, and 31/108 (28.7%) in Group B2. The rate of parathyroid autotransplantation was comparable among the study groups (P = 0.069). The intraoperative parameters were documented in Table 3.
Table 3.
Intraoperative and postoperative parameters
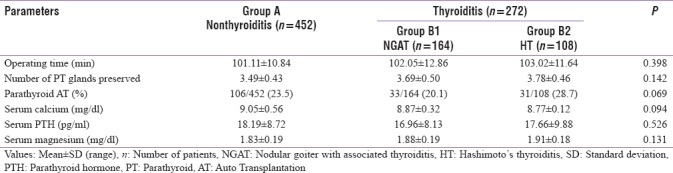
The postoperative serum calcium (mg/dl) in Group A was 9.05 ± 0.56, Group B1 was 8.87 ± 0.32, and Group B2 was 8.77 ± 0.12. The postoperative serum calcium was comparable among the study groups (P = 0.094).
The postoperative serum magnesium (mg/dl) in Group A was 1.83 ± 0.19, Group B1 was 1.88 ± 0.19, and Group B2 was 1.91 ± 0.18. The postoperative serum magnesium was comparable among the study groups (P = 0.131).
The postoperative serum intact PTH (pg/ml) in Group A was 18.19 ± 8.72, Group B1 was 16.96 ± 8.13, and Group B2 was 17.66 ± 9.88. The postoperative serum intact PTH was comparable among the study groups (P = 0.526). The postoperative parameters were documented in Table 3.
The incidence of transient hypoparathyroidism in Group A was 112/452 (24.77%) and Group B was 108/272 (39.70%). The incidence of transient hypoparathyroidism was significantly higher in Group B (thyroiditis) than Group A (nonthyroiditis) (P = 0.001).
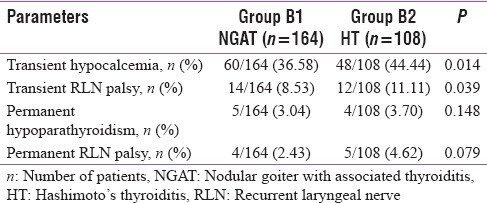
The incidence of transient hypoparathyroidism in Group B1 was 60/164 (36.58%) and Group B2 was 48/108 (44.44%). Subgroup analyses between the thyroiditis cases show that incidence of transient hypoparathyroidism was significantly higher in Group B2 (Hashimoto's thyroiditis) than Group B1 (NGAT) (P = 0.014).
The incidence of transient vocal cord palsy in Group A was 34/452 (7.52%) and Group B was 26/272 (9.55%). The incidence of transient vocal cord palsy was significantly higher in Group B (thyroiditis) than Group A (nonthyroiditis) (P = 0.040).
The incidence of transient vocal cord palsy in Group B1 was 14/164 (8.53%) and Group B2 was 12/108 (11.11%). Subgroup analyses between the thyroiditis cases show that incidence of transient vocal cord palsy was significantly higher in Group B2 (Hashimoto's thyroiditis) than Group B1 (NGAT) (P = 0.039).
On 6-month follow-up, the incidence of permanent hypoparathyroidism in Group A was 10/452 (2.21%) and Group B was 9/272 (3.30%). The incidence of permanent hypoparathyroidism was not statistically significant between Group A (nonthyroiditis) and Group B (thyroiditis) (P = 0.098).
The incidence of permanent hypoparathyroidism in Group B1 was 5/164 (3.04%) and Group B2 was 4/108 (3.70%). Similarly, the incidence of permanent hypoparathyroidism was not statistically significant between Group B1 (NGAT) and Group B2 (Hashimoto's thyroiditis) (P = 0.148).
The incidence of permanent vocal cord palsy in Group A was 8/452 (1.76%) and Group B was 9/272 (3.30%). The incidence of permanent vocal cord palsy was not statistically significant between Group A (nonthyroiditis) and Group B (thyroiditis) (P = 0.288).
The incidence of permanent vocal cord palsy in Group B1 was 4/164 (2.43%) and Group B2 was 5/108 (4.62%). The incidence of permanent vocal cord palsy was not statistically significant between Group B1 (NGAT) and Group B2 (Hashimoto's thyroiditis) (P = 0.079).
Data regarding complications were documented in Table 4, and the subgroup analysis of the thyroiditis cases was given in Table 5.
Table 4.
Postoperative complications
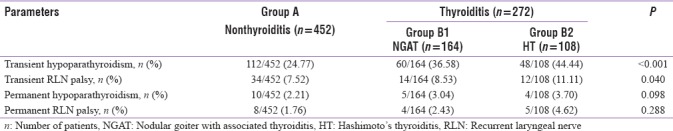
Table 5.
Subgroup analysis of thyroiditis patients
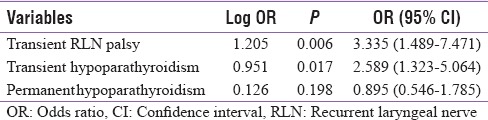
Multivariate analysis shows that the presence of thyroiditis can significantly increase the incidence of transient hypoparathyroidism (odds ratio [OR] = 2.589) and transient vocal cord palsy (OR = 3.335). However, thyroiditis does not impact the occurrence of permanent complications. Multivariate analysis is documented in Table 6.
Table 6.
Multivariate analysis of impact of thyroiditis
DISCUSSION
In 1912, Hashimoto described four patients with a disorder of the thyroid gland showing diffuse lymphocytic infiltration, parenchymal atrophy, fibrosis, and eosinophilic changes in some of the areas, which he described as struma lymphomatosa.[6]
Surgical intervention is not generally advised as treatment for patients with thyroiditis. Most of the thyroiditis cases were kept on periodical follow-up. However, thyroidectomy will be considered in specific cases.
The most common indication for surgery in nonthyroiditis cases was large goiters without any compressive symptoms. Goiters, either having a volume of more than 100 cc or a nodule having a size of 4 cm, were considered as large goiters.
The most common indication for surgery in thyroiditis cases was pressure symptoms. Pain in thyroiditis is generally treated with analgesics. The pressure symptoms considered for surgery are dysphagia (more to solids), foreign body sensation, and choking sensation (dry cough on lying posture). The other causes for pressure symptoms are ruled out before considered for surgical intervention.
The most common complications associated with thyroidectomy are hypoparathyroidism and RLN palsy, which can occur transiently or permanently as a result of trauma or disruption of the blood supply to the parathyroid glands and injury to RLN during dissection.[7,8]
Shih et al.[4] in their retrospective study of 474 thyroiditis cases had 32.1% incidence of transient hypocalcemia. In our study, the incidence of transient hypocalcemia stood at 39.70%.
McManus et al.[9] in their study of 1791 patients had significantly elevated transient hypoparathyroidism in thyroiditis cases compared to other cases (P = 0.002). In our study too, the rate of transient hypoparathyroidism is significantly higher in thyroiditis cases.
Shih et al.[4] reported only 0.4% of transient RLN palsy in thyroiditis cases, and Györy et al.[10] reported a 6.7% incidence of temporary RLN palsy, but in our study, the rate of transient RLN palsy in thyroiditis cases stood at 9.55%.
According to Pradeep et al.,[11] the incidence of temporary hypocalcemia and RLN paralysis was not statistically different between the thyroiditis and nonthyroiditis cases whereas McManus et al.[12] reported higher rate of postoperative complications (12.4%) compared to patients without HT (5.74%). Our study reports are similar to McManus et al. with high temporary hypocalcemia, and transient RLN palsy is higher in thyroiditis cases.
Györy et al.[10] reported a 5.1% permanent RLN palsy in thyroiditis patients. In our study, the incidence of permanent RLN palsy stood at 3.30%.
In our study, the incidence of temporary hypocalcemia and transient RLN palsy is higher in thyroiditis cases, but the incidence of permanent hypoparathyroidism and permanent RLN palsy rates was similar between the groups.
CONCLUSION
The incidence of transient complications is higher in our study than international literature, may be because even mild numbness and tingling are categorized as symptomatic hypoparathyroidism in our study data. Although the incidences of transient complications are higher in thyroiditis patients than nonthyroiditis patients, the permanent complications are comparable between them.
Since the complications are higher in thyroiditis cases, careful analysis of surgical indications will avoid unnecessary surgery in thyroiditis cases.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kasagi K, Kousaka T, Higuchi K, Iida Y, Misaki T, Alam MS, et al. Clinical significance of measurements of antithyroid antibodies in the diagnosis of Hashimoto's thyroiditis: Comparison with histological findings. Thyroid. 1996;6:445–50. doi: 10.1089/thy.1996.6.445. [DOI] [PubMed] [Google Scholar]
- 2.Teng X, Shan Z, Teng W, Fan C, Wang H, Guo R, et al. Experimental study on the effects of chronic iodine excess on thyroid function, structure, and autoimmunity in autoimmune-prone NOD. H-2h4 mice. Clin Exp Med. 2009;9:51–9. doi: 10.1007/s10238-008-0014-0. [DOI] [PubMed] [Google Scholar]
- 3.Thomas CG, Jr, Rutledge RG. Surgical intervention in chronic (Hashimoto's) thyroiditis. Ann Surg. 1981;193:769–76. doi: 10.1097/00000658-198106000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shih ML, Lee JA, Hsieh CB, Yu JC, Liu HD, Kebebew E, et al. Thyroidectomy for Hashimoto's thyroiditis: Complications and associated cancers. Thyroid. 2008;18:729–34. doi: 10.1089/thy.2007.0384. [DOI] [PubMed] [Google Scholar]
- 5.Kapil U, Singh P, Dwivedi SN, Pathak P. Profile of iodine content of salt and urinary iodine excretion levels in selected districts of Tamil Nadu. Indian J Pediatr. 2004;71:785–7. doi: 10.1007/BF02730711. [DOI] [PubMed] [Google Scholar]
- 6.Takami HE, Miyabe R, Kameyama K. Hashimoto's thyroiditis. World J Surg. 2008;32:688–92. doi: 10.1007/s00268-008-9485-0. [DOI] [PubMed] [Google Scholar]
- 7.Reeve T, Thompson NW. Complications of thyroid surgery: How to avoid them, how to manage them, and observations on their possible effect on the whole patient. World J Surg. 2000;24:971–5. doi: 10.1007/s002680010160. [DOI] [PubMed] [Google Scholar]
- 8.Chiang FY, Wang LF, Huang YF, Lee KW, Kuo WR. Recurrent laryngeal nerve palsy after thyroidectomy with routine identification of the recurrent laryngeal nerve. Surgery. 2005;137:342–7. doi: 10.1016/j.surg.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 9.McManus C, Luo J, Sippel R, Chen H. Should patients with symptomatic Hashimoto's thyroiditis pursue surgery? J Surg Res. 2011;170:52–5. doi: 10.1016/j.jss.2011.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Györy F, Lukács G, Juhász F, Mezösi E, Szakáll S, Végh T, et al. Surgically treated Hashimoto's thyroiditis. Acta Chir Hung. 1999;38:243–7. [PubMed] [Google Scholar]
- 11.Pradeep PV, Ragavan M, Ramakrishna BA, Jayasree B, Skandha SH. Surgery in Hashimoto's thyroiditis: Indications, complications, and associated cancers. J Postgrad Med. 2011;57:120–2. doi: 10.4103/0022-3859.81867. [DOI] [PubMed] [Google Scholar]
- 12.McManus C, Luo J, Sippel R, Chen H. Is thyroidectomy in patients with Hashimoto thyroiditis more risky? J Surg Res. 2012;178:529–32. doi: 10.1016/j.jss.2012.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]


