Abstract
This study examined the role of hope and community in achieving and/or maintaining a successful recovery, and their relationships to quality of life for individuals in recovery. The sample included 229 participants in 42 Oxford House sober living homes in 3 locations in the United States. In this cross-sectional investigation, we assessed whether hope and sense of community were predictors of quality of life for individuals living in recovery homes. Findings indicated that both hope and sense of community were predictors supporting contextual as well as individual characteristics as possible influences on recovery trajectories. These findings have implications for both individual and systems-level resource or competency-based interventions, and they suggest one of the important functions of a recovery residence is in the creation of a sense of community.
1 | INTRODUCTION
Traditional approaches to evaluating the effectiveness of substance abuse treatment have focused on measuring the frequency and quantity of drug use, as well as the achievement of abstinence. In recent years, there has been a paradigm shift away from pathological models of addiction and recovery towards a more multidimensional health model encompassing overall functioning and subjective well-being. Reflective of this change is the Substance Abuse and Mental Health Services Administration's (SAMHSA, 2012) working definition of recovery defined as “a process of change through which individuals improve their health and wellness, live a self-directed life, and strive to reach their full potential.” Furthermore, SAMHSA (2012) has delineated four dimensions (Health, Home, Purpose, and Community) that support life in recovery and 10 guiding principles of recovery (Hope, Person-Driven, Many Pathways, Holistic, Peer Support, Relational, Culture, Addresses Trauma, Strengths/Responsibility, and Respect).
Similar to SAMHSA's (2012) conceptualization of recovery is the construct quality of life (QOL). The World Health Organization (WHO) defines QOL as “an individual's perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns” (World Health Organization Quality of Life Group, 1995, p. 1405). Their conceptualization contains four domains of well-being (e.g., physical, mental, social, and environmental). The WHO Quality of Life Assessment (WHOQOL-100) is a cross-culturally sensitive and generic instrument enabling the assessment of variations of QOL, as well as the comparison and generalizability across different populations (Oliveira, Carvalho, & Esteves, 2016). The WHOQOL-Bref is an abbreviated version, which was developed simultaneously in 15 international sites. The WHOQOL-Bref has been tested with different populations including groups with medical conditions (Liou et al., 2005; Michelone & Santos, 2004), psychiatric disorders (Berlim, Pavanello, Caldieraro, & Fleck, 2005; Chand, Mattoo, & Sharan, 2004; Herrman, Hawthorne, & Thomas, 2002; Trompenaars, Masthoff, Van Heck, Hodiamont, & De Vries, 2005), and substance use disorders (Barros da Silva Lima, Fleck, Pechansky, De Boni, & Sukop, 2005).
Quality of life has become an increasingly recognized important outcome of addiction recovery (Muller & Clausen, 2015; Pasareanu, Osapal, Verdehus, Kristensen, & Clausen, 2015) that utilizes domains not captured by traditional severity measures such as the Addiction Severity Index (Donovan, Mattson, Cisler, Longabaugh, & Zweben, 2005). Assessing the QOL of people recovering from addiction contributes to our understanding of the consequences of addiction for everyday life, as well as allow for the evaluation of individual outcome and change over time (Rudolf & Watts, 2002). For instance, there is increasing evidence that QOL has a prognostic value (Foster, Powell, Marshall, & Peters, 2008). Laudet, Becker, and White (2009) found that higher QOL at treatment completion predicts abstinence 1 and 2 years’ posttreatment among individuals recovering from substance use disorders. This relationship was partially mediated by motivation to stay abstinent. Laudet and Stanick (2010) found that satisfaction with QOL at the end of outpatient treatment significantly predicted commitment to abstinence. Moreover, improvement in QOL is regarded as an important outcome of treatment by those in recovery. For instance, Laudet and White (2010) found that in addition to remaining abstinent, participants at different stages of recovery expressed concerns about multiple areas of functioning, including social relationships, emotional well-being, physical health, and their living environment.
It is important to identify the psychological states that are most predictive of QOL for individuals in recovery. SAMHSA (2012) named hope as a one of their guiding principles of recovery, which they identified to be a catalyst of the recovery process. According to SAMHSA (2012), hope is both internalized and fostered by those in one's community, such as peers, family members, service providers, and others supportive of one's recovery. Hope has been researched as a salient influence on an individual's motivation and behavior (Stevens, Buchannan, Ferrari, Jason, & Ram, 2014) and is characterized by three dimensions: (a) the perception of successful agency, (b) the perceived available pathways toward achieving a goal (Snyder et al., 1991), and (c) the opportunities, choices, and obstacles found in the environmental context (Stevens et al., 2014).
Hope is an important component of recovery from substance abuse given that recovery requires both the motivation to overcome repeated challenges and the ability to generate pathways to overcome these challenges. Individuals with strong hope are better prepared to deal with situational threats, able to generate greater number of strategies for attaining goals, and increase the use of appropriate adaptive strategies when faced with the threats (Mathis, Ferrari, Groh,&Jason, 2009). Studies have examined hope among individuals in recovery from substance abuse. Irving, Seidner, Burling, Pagliarini, and Robbins-Sisco (1998) found that higher hope levels was associated with greater time abstinent and higher QOL. Hope acted as a mediator between health promoting behaviors and 12-step affiliation for those with a substance use disorder and in a dual 12-step/mental health self-help treatment program (Magura et al., 2003).
Another important aspect of recovering from addiction is a supportive environment. An individual's feelings about this environment has often been constructed as a sense of community (SOC). Jason, Stevens, and Ram (2015) developed a three-factor Psychological Sense of Community Scale: The “entity” level, which is the macro system that includes the mission (reason for being) and operating rules of the community; “membership” level, which is the people the entity encompasses; and “self” level, which is one's own commitment and investment in the entity and its members. Stevens et al. (2014) found that a person's perceived context accounted for approximately 50% of his/her hopefulness for individuals living in recovery homes. Jason, Stevens, and Light (2016) found that SOC is predictive of hope among individuals living in recovery homes. Moreover, Stevens, Jason, Ferrari, and Hunter (2010) found that abstinence specific self-efficacy and SOC had a significant positive relationship. The results of these studies demonstrate that the importance of one's environmental context and interpersonal relationships in the development of hope.
More research is needed to support SAMHSA's (2012) conceptualization of recovery. Furthermore, few studies exists on the associations between hope, SOC and QOL. In addition, not much is known about the QOL of those living in recovery residences. To address these gaps in the literature, the current study provided empirical validation of SAMHSA's recovery model by examining the relation between hope, SOC and QOL. In this cross-sectional investigation, we examined whether hope and SOC were predictors of QOL for individuals living in recovery homes. We expected that both hope and SOC would be significant predictors of QOL even after controlling for length of stay in a recovery home.
2 | METHOD
2.1 | Participants
Social network information was collected from 229 participants from 42 Oxford Houses, which are democratic, self-running recovery homes, the largest network of such recovery homes in the United States (Jason, Olson, & Foli, 2008). The actual number of potential participants per house was 6.14 and we had 5.45 (88.8% of potential participants) in our study, and there were 1,287 measured relationships. The sample included 55% males and 44.5% females, with a mean age of 38.4 years (standard deviation [SD] = 10.8). Participants were European American (82.1%), African American (9.2%), Hispanic (6.5%), Alaskan Native (6.5%), American Indian (1.3%), and Pacific Islander (.4%). The average length of stay in an Oxford House for participants was 10.3 months (SD = 12.55, range from 7 days to 6.8 years).
2.2 | Procedures
Data were collected from Oxford Houses located in North Carolina, Texas, and Oregon. Field research staff recruited participants via face-to-face meetings. Individuals were informed about the purpose, objectives, and methodology of the study and were advised of the voluntary nature of the study before signing and returning a consent form. Interviews were scheduled and conducted that included self-report measures of QOL, hope, SOC, self-esteem, stress, social support, and other demographic information. Participants were compensated $20 for completing their assessment. Permission to do this study was granted by the DePaul University Institutional Review Board.
2.3 | Measures
2.3.1 | Hope
Snyder's State Hope Scale (Snyder et al., 1996) measures one's current state of hope. The measure contains two subscales Agency (α = .85) and Pathways (α = .71). We included a subscale of hope that measures Environmental Context (Stevens et al., 2014; α = .67). The hope scale was analyzed as a whole measure (α = .88).
2.3.2 | SOC
The Psychological Sense of Community Scale (Jason et al., 2015) measures one's SOC based on three distinct ecological domains: the individual, microsystem, and macrosystem. This version has been modified to measure communal living conditions specific to Oxford Houses. Items include “This Oxford House is important to me” and “For me, this Oxford House is a good fit.” The three subscales, which have been named Entity, Membership, and Self and have Cronbach alphas of .71, .89, and .87, respectively, for this sample. The SOC scale was analyzed as whole measure (α = .88).
2.3.3 | QOL
The World Health Organization Quality of Life Assessment Brief Version (WHOQOL Group, 1998). This is a 26 item (24 items comprising the psychometric scale) measuring QOL across four domains: physical, psychosocial, social relationships, and environment. The subscales vary in their reliability (αs = .66 for the 3-item social relationship subscale, .75 for psychological, .80 for environment, and .82 for physical). The QOL scale was analyzed as a whole measure (α = .89).
3 | RESULTS
A multilevel model was utilized to test QOL for possible random effects due to house membership. The variance components of the null model were Level 1 or σ2 = 21.703 and Level 2 or τ = 5.794 for an intraclass correlation coefficient of .211, χ2(41) = 96.08, p < .001. Overall, a significant relationship was found between an individual's QOL and the house in which they were a resident. Thus, analysis proceeded using a random effects model and individual level predictors were added to investigate demographic differences and the possible relation of Hope to QOL (see Table 1).
TABLE 1.
Final estimation of fixed effects (with robust standard errors)
| Fixed effect | Coefficient | Standard error |
t-ratio | Approx. df |
p-value |
|---|---|---|---|---|---|
| For INTRCPT1, β0 | |||||
| INTRCPT2, γ00 | 48.800 | 1.097707 | 44.454 | 41 | <0.001 |
| For AGE slope, β1 | |||||
| INTRCPT2, γ10 | 0.023 | 0.022966 | 0.983 | 167 | 0.327 |
| For Length slope, β2 | |||||
| INTRCPT2, γ20 | 0.190 | 0.200309 | 0.948 | 167 | 0.344 |
| For HOPE_MEA slope, β3 | |||||
| INTRCPT2, γ30 | 2.858 | 0.315614 | 9.054 | 167 | <0.001 |
| For SEX slope, β4 | |||||
| INTRCPT2, γ40 | −1.937 | 0.665250 | −2.912 | 167 | 0.004 |
| For Afri_Amer slope, β5 | |||||
| INTRCPT2, γ50 | 1.691 | 1.098734 | 1.539 | 167 | 0.126 |
| For Hispanic slope, β6 | |||||
| INTRCPT2, γ60 | 0.425 | 1.032124 | 0.412 | 167 | 0.681 |
| Final estimation of variance components | |||||
| Random effect | Standard deviation |
Variance component |
df | χ2 | p-value |
|---|---|---|---|---|---|
| INTRCPT1, u0 | 1.47979 | 2.18977 | 41 | 74.67287 | 0.001 |
| level-1, r | 3.57438 | 12.77622 |
Note. df = degree of freedom.
Race/ethnicity, age, and length of stay were not significant independent covariates of QOL when combined with Hope. Sex was a significant predictor and being female, on average, projected a lower overall QOL (see Table 1, fixed effects). Prior measurement testing of the QOL instrument found a significant sex difference response to the following item “Are you able to accept your bodily appearance?” where females scored significantly lower than males. However, this systemic difference would not explain the nearly 2-point difference in QOL between males and females in the current results. Since the housing is same sex, these data cannot distinguish between a housing or individual sex difference since no contrast exists (e.g., females in a male houses or males in female houses).
Hope and QOL had a significant relationship with a large effect size (partial r ≈ .57, p < .001), providing evidence that a future orientation or aspirations are associated with a current assessment of life quality. With this random effects model, the house level effect was still significant (see Table 1, variance components).
As conceptualized, SOC is a house-level phenomenon of individuals connected by common purpose and interpersonal relations. As a predictor, it exhibited a significant relationship with QOL and reduced the Level 2 (τ) variance to a level that was not significant (see Table 2).
TABLE 2.
Final estimation of fixed effects (with robust standard errors)
| Fixed effect | Coefficient | Standard error |
t-ratio | Approx. df |
p-value |
|---|---|---|---|---|---|
| For INTRCPT1, β0 | |||||
| INTRCPT2, γ00 | 48.324 | 0.852 | 56.71 | 40 | <0.001 |
| SOC, γ01 | 2.630 | 0.636 | 4.14 | 40 | <0.001 |
| For HOPE slope, β1 | |||||
| INTRCPT2, γ10 | 2.731 | 0.321 | 8.52 | 171 | <0.001 |
| For SEX slope, β2 | |||||
| INTRCPT2, γ20 | −1.454 | 0.510 | −2.85 | 171 | 0.005 |
| Final estimation of variance components | |||||
| Random effect | Standard deviation |
Variance component |
df | χ2 | p-value |
|---|---|---|---|---|---|
| INTRCPT1, u0 | 0.811 | 0.659 | 40 | 51.39 | 0.107 |
| level-1, r | 3.622 | 13.116 |
Note. df = degree of freedom.
3.1 | Discussion
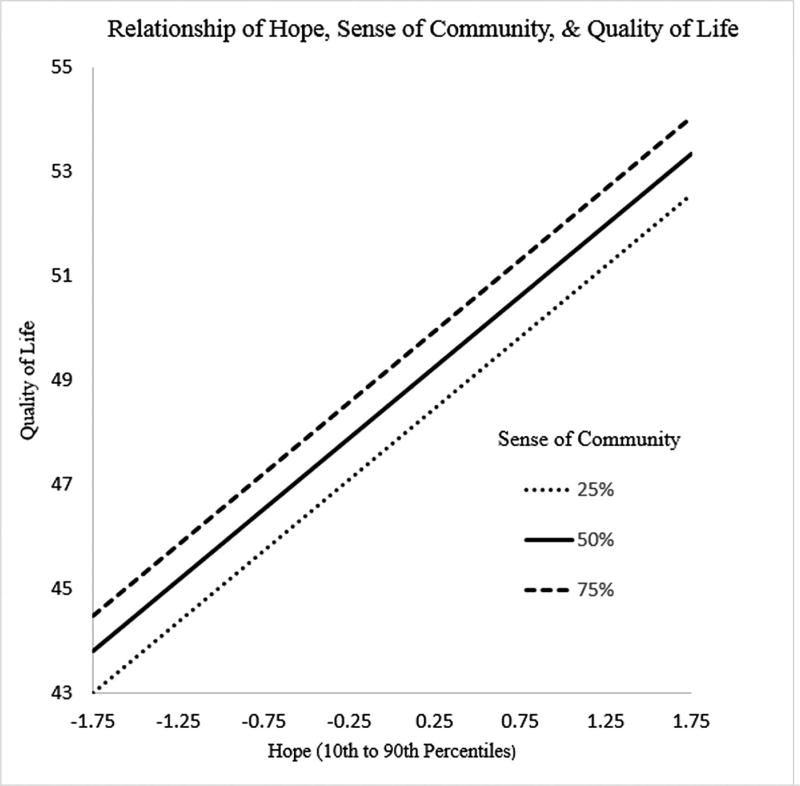
Overall, our findings suggest that an individual's QOL can be reasonably predicted by their individual hopefulness and the SOC within their residence. Both of these characteristics exhibit large effect sizes and substantially reduce the unexplained variance of QOL. For these adults in recovery, both individual- and house-level factors that are largely psychological in nature appear to be associated with QOL outcomes (see Figure 1).
FIGURE 1.
Relationship of hope, SOC, and QOL
Our findings are supportive of SAMHSA's (2012) conception of recovery in which hope and community play significant roles in achieving and/or maintaining a successful recovery, which is accompanied by an increasing QOL. Both hope and SOC were strong predictors supporting contextual as well as individual characteristics as possible influences on recovery trajectories. In addition, these findings have implications for the development of competency-based interventions. For example, motivation-based efforts may be facilitated by addressing the key components of hopefulness. Recovery housing may benefit from community building actions. As an empirical contribution for supporting theory, the house-level effects of SOC accounted for nearly 70% of the variance attributed to house-level clustering. This finding suggests that one of the important possible functions of a recovery residence is in the creation of a SOC.
Some might feel that we could consider both SOC and hope as contextual and individual variables. In other words, we could have modeled the group averages for each of these constructs as level-two fixed effects along with the level one individual differences for each of these variables. However, we believe there is justification for conceptualizing SOC as a group variable and hope as an individual construct. One could measure “one” person's sense of belonging to a group, but this single observation would not capture the group's SOC. Rather than assessing SOC by one person's observation, we believe there needs to be a representative sample of individuals to tap this construct. Furthermore, hope is best thought of an intrapersonal variable in the literature.
This study is limited by its cross-sectional and observational design. In addition, the sample is relatively homogeneous relative to race/ethnicity and certainly, as individuals in recovery. Thus, it lacks claim to causality, relationship direction, and generalization to a broad population; however, the magnitude of the results at both the individual and the house level should encourage future research to better understand the dynamics and possible causal mechanisms that have tied these three concepts—hope, SOC, QOL–tightly together.
These future investigations should include longitudinal designs to examine within-person effects because they interact with opportunities, settings, and others. These designs should also include a control group to better understand the contrast between setting effects. While the current study has a homogeneous setting replicated over 40 times, providing a distribution of SOC scores, there was no counterfactual to measure not being in a house and how that compared on QOL.
Research should also proceed to generalize these relationships to broader populations. For this sample population, although the relationships were strong, this pattern may not replicate across other populations. The degree to which it does or does not would seem to be important in understanding and evaluating QOL for different populations. For example, college students may place greater value on hope and its future orientation, the elderly may appreciate SOC as a remedy to loneliness, and the poor may discount both relative to more concrete contributions to QOL. This speculation illustrates why more population studies might be useful in building a nomothetic case for hope and community as a basis for QOL.
3.2 Conclusion
Because hope is operationalized as subscales of individual agency, pathways, and perceived opportunities/barriers, it may be functioning as a proxy for such constructs as empowerment, self-determination, locus of control, and self-efficacy. Certainly more granular investigations of mechanisms and relations should be pursued; however, hope in these data holistically summarizes a meaningful extent of QOL. In summary, it appears that both hope and SOC are important influences on recovery trajectories. We believe that our study identifies the creation of a SOC as an important functions of a recovery residence, and such findings have implications for both individual and systems-level resource or competency-based interventions.
Acknowledgments
We appreciate the financial support from the National Institute on Alcohol Abuse and Alcoholism (1R01AA022763-01A1).
References
- Barros da Silva Lima AF, Fleck M, Pechansky F, De Boni R, Sukop P. Psychometric properties of the World Health Organization quality of life instrument (WHOQoL-BREF) in alcoholic males: A pilot study. Quality of Life Research. 2005;14:473–478. doi: 10.1007/s11136-004-5327-1. [DOI] [PubMed] [Google Scholar]
- Berlim MT, Pavanello DP, Caldieraro MA, Fleck MP. Reliability and validity of the WHOQOL BREF in a sample of Brazilian outpatients with major depression. Quality of Life Research. 2005;14:561–564. doi: 10.1007/s11136-004-4694-y. [DOI] [PubMed] [Google Scholar]
- Chand PK, Mattoo SK, Sharan P. Quality of life and its correlates in patients with bipolar disorder stabilized on lithium prophylaxis. Psychiatry and Clinical Neurosciences. 2004;58:311–318. doi: 10.1111/j.1440-1819.2004.01237.x. [DOI] [PubMed] [Google Scholar]
- Donovan D, Mattson ME, Cisler RA, Longabaugh R, Zweben A. Quality of life as an outcome measure in alcoholism treatment research. Journal of Studies on Alcohol, Supplement. 2005;107:119–139. doi: 10.15288/jsas.2005.s15.119. [DOI] [PubMed] [Google Scholar]
- Herrman H, Hawthorne G, Thomas R. Quality of life assessment in people living with psychosis. Social Psychiatry and Psychiatric Epidemiology. 2002;37:510–518. doi: 10.1007/s00127-002-0587-y. [DOI] [PubMed] [Google Scholar]
- Irving LM, Seidner AL, Burling TA, Pagliarini R, Robbins-Sisco D. Hope and recovery from substance dependence in homeless veterans. Journal of Social and Clinical Psychology. 1998;17:389–406. [Google Scholar]
- Jason LA, Olson BD, Foli K. Rescued lives: The Oxford House approach to substance abuse. New York: Routledge; 2008. [Google Scholar]
- Jason LA, Stevens E, Light JM. The relationship of sense of community and trust to hope. Journal of Community Psychology. 2016;44:334–341. doi: 10.1002/jcop.21771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jason LA, Stevens E, Ram D. Development of a three-factor psychological sense of community scale. Journal of Community Psychology. 2015;43:973–985. doi: 10.1002/jcop.21726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet AB, Becker JB, White WL. Don't wanna go through that madness no more: Quality of life satisfaction as predictor of sustained remission from illicit drug misuse. Substance Use & Misuse. 2009;44(2):227–252. doi: 10.1080/10826080802714462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet AB, Stanick V. Predictors of motivation for abstinence at the end of outpatient substance abuse treatment. Journal of Substance Abuse Treatment. 2010;38:317–327. doi: 10.1016/j.jsat.2010.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet AB, White W. What are your priorities right now? Identifying service needs across recovery stages to inform service development. Journal of Substance Abuse Treatment. 2010;38:51–59. doi: 10.1016/j.jsat.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liou HH, Chen RC, Chen CC, Chiu MJ, Chang YY, Wang JD. Health related quality of life in adult patients with epilepsy compared with a general reference population in Taiwan. Epilepsy Research. 2005;64:151–159. doi: 10.1016/j.eplepsyres.2005.03.006. [DOI] [PubMed] [Google Scholar]
- Magura S, Knight EL, Vogel HS, Mahmood D, Laudet AB, Rosenblum A. Mediators of effectiveness in dual-focus self-help groups. The American Journal of Drug and Alcohol Abuse. 2003;29:301–322. doi: 10.1081/ADA-120020514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathis GM, Ferrari JR, Groh DR, Jason LA. Hope and substance abuse recovery: The impact of agency and pathways within an abstinent communal-living setting. Journal of Groups in Addiction & Recovery. 2009;4:42–50. doi: 10.1080/15560350802712389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michelone ADPC, Santos VLCG. Quality of life of cancer patients with and without an ostomy. Revista Latino-Americana de Enfermagem. 2004;12:875–883. doi: 10.1590/s0104-11692004000600005. [DOI] [PubMed] [Google Scholar]
- Muller AE, Clausen T. Group exercise to improve quality of life among substance use disorder patients. Scandinavian Journal of Public Health. 2015;43(2):146–152. doi: 10.1177/1403494814561819. [DOI] [PubMed] [Google Scholar]
- Oliveira SE, Carvalho H, Esteves F. Toward an understanding of the quality of life construct: Validity and reliability of the WHOQOL-Bref in a psychiatric sample. Psychiatry Research. 2016;244:37–44. doi: 10.1016/j.psychres.2016.07.007. [DOI] [PubMed] [Google Scholar]
- Pasareanu AR, Opsal A, Vederhus JK, Kristensen Ø, Clausen T. Quality of life improved following in-patient substance use disorder treatment. Health and Quality of Life Outcomes. 2015;13:35. doi: 10.1186/s12955-015-0231-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudolf H, Watts J. Quality of life in substance abuse and dependency. International Review of Psychiatry. 2002;14:190–197. [Google Scholar]
- Snyder CR, Harris C, Anderson JR, Holleran SA, Irving LM, Sigmon ST, Harney P. The will and the ways: Development and validation of an individual-differences measure of hope. Journal of Personality and Social Psychology. 1991;60:570. doi: 10.1037//0022-3514.60.4.570. [DOI] [PubMed] [Google Scholar]
- Stevens EB, Buchannan B, Ferrari JR, Jason LA, Ram D. An investigation of hope and context. Journal of Community Psychology. 2014;42:937–946. doi: 10.1002/jcop.21663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens EB, Jason LA, Ferrari JR, Hunter B. Self-efficacy and sense of community among adults recovering from substance abuse. North American Journal of Psychology. 2010;12:255. [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. SAMHSA's working definition of recovery: 10 guiding principles of recovery. Substance Abuse and Mental Health Services Administration. 2012 (Archived by WebCiteVR Available from: Retrieved from https://www.webcitation.org/6Vm7B2SaF)
- Trompenaars FJ, Masthoff ED, Van Heck GL, Hodiamont PP, De Vries J. Content validity, construct validity, and reliability of the WHOQOL-Bref in a population of Dutch adult psychiatric outpatients. Quality of Life Research. 2005;14:151–160. doi: 10.1007/s11136-004-0787-x. [DOI] [PubMed] [Google Scholar]
- World Health Organization Quality of Life Assessment Group. The World Health Organization Quality of Life Assessment (WHOQOL): Position paper from the World Health Organization. Social Science & Medicine. 1995;41(10):1403–1409. doi: 10.1016/0277-9536(95)00112-k. [DOI] [PubMed] [Google Scholar]