Abstract
Background
Child development is negatively impacted by HIV with children that are infected and affected by HIV performing worse than their peers in cognitive assessments.
Methods
We conducted a descriptive follow-up comparison study (n=989) in South African and Malawi. We tracked child development in 135 HIV-positive children compared to 854 uninfected children aged 4-13 years old attending community-based organisations at baseline and again 12-15 months later.
Results
Children with HIV were more often stunted (58.8% versus 27.4%) and underweight (18.7% versus 7.1%). They also had significantly poorer general physical functioning (M=93.37, versus M=97.00). HIV-positive children scored significantly lower on digit span and the draw-a-person task.
Conclusions
These data clearly show that HIV infection poses a serious risk for child development and that there is a need for scaled up interventions. Community-based services may be ideally placed to accommodate such provision and deliver urgently needed support to these children.
Keywords: HIV/AIDS, cognitive development, physical functioning, quality of life, South Africa, Malawi
Child development is affected by HIV in many ways (Sherr, Cluver, Betancourt, Kellerman, Richter & Desmond, 2014). The increase in access to PMTCT has meant that the lives of a number of children have been saved. However, in spite of these gains, children affected by HIV are at risk of not meeting their developmental potential. There are both indirect and direct effects ofthe virus on the developing child. Firstly, there are numerous indirect effects due to the clustering of HIV infection in families that may affect the quality of parenting, the level of daily stimulation, quality of nutrition, parental mental health, poverty, health care, quality of the home environment and can compromise caregiving (Sherr, Cluver, Betancourt, Kellerman, Richter, & Desmond, 2014). All of these consequences of HIV are known to adversely affect optimal child development in multiple domains. A variety of parental, community and child factors determine the extent of harm and the level of shielding from potential adverse events associated with HIV diagnosis, illness, parental burden, stigma, services, treatment access and death (Stein et al., 2014).
Secondly, there are direct effects of infection. A recent review documented detrimental effects of HIV infection on child development in 36 of 41 studies identified (Sherr, Croome, Parra Castaneda, Bradshaw &Romero, 2014). An earlier systematic review (Sherr, Mueller, & Varrall, 2009) collated all studies on cognitive effects of HIV on children. However, of the fifty-four studies identified, 10 had no control or comparison groups and the data were highly North American biased (63%) with European studies accounting for 13%, 3.7% from South America and 13% from Africa, where the vast majority of HIV-infected children are found. 81% of studies reported a detrimental effect on neurocognitive development, however measured, whilst three reported no differences and four had mixed findings. This review showed that some domains of cognitive functioning seemed to be more affected than others, with gathering evidence on language, executive functioning, global development and behavioural challenges. Even when studies focus specifically on low income countries in Sub-Saharan Africa where the burden of HIV is the highest, a recent review (Banks, Zuurmond, Ferrand, & Kuper, 2015) shows that the majority – 92% – of the 61 studies identified were clinic-based, with criticisms of sampling and non-reporting of response rates. Furthermore, the reviews are often confined to studies of cognitive performance and do not relate or link these to other developmental measures such as physical development, behaviour or mental health such as depression, anxiety or trauma, or positive mental health such as quality of life.
If children are to receive evidence-based interventions to maximise their developmental potential, it is important to monitor children within a community setting and also to understand how community-based organisations (CBOs) are positioned as potential providers of support. This is especially true in low and middle income countries where high-cost interventions or individual based treatments are particularly costly with limited availability.
However, donor efforts to support community-based organisations (CBOs) in providing programmes for children affected by HIV/AIDS have not been matched with concommitant research investment into child development in community settings. A systematic review published in 2009 was not able to identify a single intervention to improve the psychosocial wellbeing of children affected by HIV and AIDS that met their inclusion criteria (King, De Dilva, Stein & Patel, 2009). As a result there was a call for increased investment in evidence-based programming for children affected by HIV and AIDS (Bryant et al., 2012; Engle et al., 2011) and a resultant response from funders recognising the importance of prioritising monitoring and evaluating these types of interventions (UNAIDS, 2010). However, there are a number of challenges inherent in evaluating these types of community programmes, such as the small size of many of these organisations, the lack of local research capacity, the conflict of interest inherent in programme evaluation for funding purposes, high cost and the logistical difficulties of conducting research in vulnerable communities (King, De Silva, Stein, & Patel, 2009). CBO programmes tend to have developed in response to community needs, with blurred lines of provision with other community services and groups. The interventions that are delivered by CBOs are often complex and consist of several components, which can be difficult to disentangle.
This study arose out of this challenge and in partnership with a number of international donors. Previously we reported on baseline differences in HIV-positive and HIV-negative children in terms of parental report developmental disability, quality of life and access to services (Skeen, Tomlinson, Macedo, Miltz, Croome & Sherr, 2014). In this report, we examine differences between these two groups in terms of cognitive outcomes, quality of life and service access over time . This is part of a larger study tracking health and development outcomes in children affected by HIV attending community-based organisations.
Method
This study reports data from the Child Community Care Study, a follow-up comparison study nal study on children affected by HIV/AIDS enrolled at community-based programmes in South Africa and Malawi. Eleven funding partners (World Vision, Comic Relief, Save the Children, Firelight Foundation, Help Age, UNICEF, REPSSI, Bernard van Leer Foundation, STOP AIDS Now, AIDS Alliance and the Diana Memorial Fund) participated in the study. The study has ethical approval from the ethics boards at University College London (reference number 1478/002) and Stellenbosch University (reference number N10/04/112). In both South Africa and Malawi, the funders of the community-based organisations provided permission to do research in the selected programmes and provided letters of support for the project.
Procedure
Children were recruited from community-based organisations in South Africa and Malawi. These countries were selected for their high HIV prevalence. CBOs delivered services directly to children and families affected by HIV, and were varied in scope, with services including provision of material support to families, home-based care, parenting programmes, support groups and linking to other forms of care.
Project funding partners provided access to all funded CBO programmes(N=588,524 in South Africa and 64 in Malawi). The 588 CBOs that were provided were stratified by funder and geographical location and 28 were randomly selected for inclusion (24 across seven South African provinces, and 4 in the Central Region of Malawi). . Children between the ages of 4 and 13 and their primary caregivers were consecutively sampled at each CBO, and both were interviewed. In addition, CBO leadership provided detailed information on CBO services and structure. All data collectors were trained and supervised female data collectors with completed high school level education and experience working with children.
Data input was done using mobile phone technology (Tomlinson et al., 2009). All questionnaires were translated and back-translated into Xhosa and Zulu, Participants were interviewed by data collectors in the language of their choice. Each child interview took approximately 40 minutes and each caregiver interview took approximately one hour. At all stages children were encouraged to have breaks if they were feeling tired. The child and caregiver interviews were often done simultaneously in order to shorten the amount of time that the caregiver and child needed to spend with research team. In most cases, the draw-a-person test was conducted while the data collectors were interviewing children’ primary caregivers. Baseline took place in 2012 and follow-up data were gathered 12-15 months later (2013-2014). Inclusion rate was high (99.3% agreement, 0.7% refusal) at baseline. At follow-up, 86.3% were available for assessment.
Measures
Demographic data
Demographic data included carer report on household variables, employment, food security and family illness. Children also provided information on their housing situation, whether their biological parents were still alive, whether they cared for sick people or younger children, and whether they had enough to eat. HIV status for both child and primary caregivers was gathered utilising caregiver report.
Discipline
Items on harsh discipline practices were taken from the Parent-Child Conflict Tactics Scale (Straus et al., 1998) and the International Society for the Prevention of Child Abuse and Neglect (ISPCAN) screening tools (Runyan et al., 2009). Although the validity of these screening tools have not been assessed in South Africa and Malawi directly, the tools have been shown to have good cross-cultural validity (Dunne et al., 2009).
Growth status of the child
This was measured by the data collectors, who weighed the children and measured their height during the interview. WHO Anthro software (version 3.2.2) was used to calculate three growth assessment indicators: height-for-age, weight-for-age, and height-and-weight-for-age (or BMI-for-age) for each child. Nutritional status was assessed using z-score cut-offs according to the classification of WHO Global Database on Child Growth and Malnutrition. The cut-off point of <−2 Z-scores classifies low height-for-age as stunting, low BMI-for-age as wasting, and low weight-for-age as underweight. Items on food and nutrition in the home were from the Child Status Index (Nyangara, O’Donnell, Murphy, & Nyberg, 2009).
Education
School performance included caregiver report of school enrolment, age-appropriate school grade, attendance and performance drawn from the Child Status Index (CSI) tool (O’Donnell, Nyangara, Murphy, Cannon, & Nyberg, 2008 [2014]). Educational risk was composed of four binary, caregiver-report questions: whether the child was in the incorrect school class for his or her age, whether the child was slow to learn when introduced new chores and things, whether teachers reported that the child struggled at school and whether the child attended less than regularly. For every affirmative answer educational risk went up by one, with a total score of 0-4.
Child mental health
Emotional and behavioural problems
Emotional and behavioural problems were measured by carer report using the short Strengths and Difficulties Questionnaire (SDQ; Goodman, 1997; Goodman, Meltzer, & Bailey, 1998), consisting of nine items divided over several subscales (scored 0=not true, 1=somewhat true, 2=certainly true or vice-versa for reverse-scored items) with higher scores indicating worse behavioural problems. The SDQ has been tested on a similar sample of vulnerable children in South Africa and has shown good validity (Sharp et al., 2014).
Depression
Depression was measured with child report using an adapted version of the Child Depression Inventory (Kovacs, 1992), which has been recently used in South Africa (Cluver, Gardner, & Operario, 2007; Mueller, Alie, Jonas, Brown, & Sherr, 2011), and has been found to have good validity (Timbremont, Braet, & Dreessen, 2004). This scale (α =.63) consists of nine items (scored 0-2, 2 being the worst outcome), with a total score of 0-18 and higher scores indicating worse depression.
Self-esteem
Self-esteem was measured using the traditional Rosenberg Self-Esteem Scale (α =.61), a child-report ten-item scale with extensive validity and reliability data (Rosenberg, 1965; Bagley et al. 1997; Gray-Little et al. 1997; Griffiths et al. 1999). Each item is scored 0-3 (3 being the best outcome) with higher scores indicating better self-esteem (total score of 0-30). This scale is the most widely used measure of self-esteem and has been shown to have excellent reliability and validity in South Africa (Westaway, Jordaan, & Tsai, 2015).
PTSD symptomatology
PTSD symptomatology was assessed with the short version (ten-item) of the child-report Trauma Symptom Checklist for Children (TSCC; Briere, 1996). Although use in South Africa and Malawi has not be reported, the scale has good validity (Lanktree et al., 2008). The items are scored 0=never, 1=sometimes, 2=lots of times, 3=all the time, with a total score of 0-30 and higher scores indicate worse trauma (α =.74).
Quality of life
Quality of life was measured using a short version of the carer-report Paediatric Quality of Life Inventory which has been shown to have good validity (PedsQL 4.0; Varni, Seid, & Kurtin, 2001). The measure consists of 15 items divided over several subscales (physical, educational and psychosocial domains; scored 0=never to 4=almost always), converted into a standardised score from 0-100 for every subscale with higher scores being a sign of better functioning in these subscales. The means of all subscales were taken to determine total quality of life. Physical functioning was assessed using one of the subscale of the PedsQL, with a total score ranging from 0-100.
Child cognitive development
Cognitive development was assessed with two age-appropriate developmental tests: a digit span test for working memory (Wechsler, 2004) and the draw-a-person test (Goodenough,1926–Harris, 1963).
Digit span
Digit span assessments can be comprised of two modalities, digits forward and digits backward. The digit span, when administered by itself, is a good predictor of academic achievement in children (Bowler, Smith, Schwarzer, Perez-Arce, & Kreutzer, 2002). The digit span test was administered by trained data colelctors. Children were verbally presented with a string of numbers and asked to repeat back the numbers in the order presented (either forwards or backwards). A total scaled score for the two recall conditions was computed (range 0-20). The scaled score is an age-based, norm referenced score for each child, based on a large nationally representative norm sample of South African children (Madge, van den Berg, & Robinson, 1985). We computed separate scaled scores for the two modalities of digit span (backwards and forwards). However, the Manual for the South African Individual Scales (Madge, van den Berg, & Robinson, 1985) only provides scaled scores for the combined recall conditions.
Draw-a-person
Draw-a-person test requires children to make three drawings of people – a man, a woman, and themselves. The drawings are scored according to a simple and quantitative system and the number of details portrayed by the children is used to provide a well-used indicator of general nonverbal cognitive ability(Chappell & Steitz, 1993; ter Laak et al., 2005)Drawings were coded and marked by a researcher who was blinded to the child’s identity at the time of assessing the drawings. We used the revised form of the Draw-a-person (DAP) test (Harris, 1963). There are few cognitive screening tools for young children in Sub-Saharan Africa and this test was considered the most appropriate. This revised version of DAP has been previously used in African countries (Lotz, Loxton, Naidoo, 2005; Loxton, Mostert, Moffatt, 2006; Powell, Walker, Rogathe, et al. 2015). An age scaled score was recorded for each drawing, and mean scores were calculated (range 40-130).
Statistical analysis
Analyses were conducted in four stages and data were analysed using SPSS v22.0. First, differences between HIV-positive and non-HIV-positive children on socio-demographic variables and developmental outcomes were analysed for the full sample at baseline (N=989) using t-tests (for categorical variables) and chi-square tests (for continuous variables). Second, associations between child HIV status and developmental outcomes were examinedcross-sectionally at baseline using multivariable logistic (for binary outcomes) and linear (for continuous outcomes) regression analyses. Third, differences between children lost to and retained at follow-up were tested using t-tests and chi-square tests as appropriate. Fourth, we explored differences between HIV-positive and non-HIV-positive children in outcome progression over time using repeated measures ANOVA analyses. The outcomes were: growth status, education, quality of life (measured on four domains), mental health (self-esteem, depressive and trauma symptoms), and cognitive development. Regression and repeated measures analyses were controlled for all covariates found to be significantly associated with being HIV positive, including: country of residence, caregiver gender, caregiver HIV status, HIV in the household, family sickness, food insecurity, and caring for younger children.
Results
Organisation characteristics
Of the total, 11 of the South African CBOs were located in rural areas (46%), two were in semi-urban areas (8%), and 11 were in urban areas (46%). In Malawi, all four CBOs were located in rural areas (100%). We measured the type of services the children received from the CBO based on caregiver report. Most children received food provision (n=537, 54.3%) and play supervision (n=498, 50.4%). Other services included home visits (n=262, 26.5%), early childhood development programmes (n=259, 26.2%), psychosocial interventions (n=252, 25.5%), material supplies such as clothes and blankets (n=246, 24.9%), and school-related support (n=243, 24.6%). Fewer children received emotional support (n=166, 16.8%), cash support grants (n=122, 12.3%), and medical services (n=110, 11.1%)yet those in need received assistance to access these services through referrals (n=91, 9.2%). Caregivers received the following community-based programme services: child support interventions (n=644, 65.1%), material supplies (n=401, 40.5%), parenting interventions (n=297, 30%), home visits (n=262, 26.5%), assistance in accessing grants (n=116, 11.7%), and medical services (n=102, 10.3%).
Sample characteristics
The sample consisted of 989 children (51.4% girls) between the ages of 4-13 (M=8.91, SD=2.84 years). Of the total, 135 children (13.7%) were identified by their carer as HIV-positive. At follow-up, 98.2% of the confirmed HIV-positive children were reported to be on treatment for HIV (92.5% were on antiretroviral medication). For this study, the 135 HIV-positive children were compared to the 854 HIV-negative children. They were compared on demographics and socio-economic variables to identify potential covariates (see Table 1). HIV-positive children were less likely to have a female caregiver (89.6% versus 95.8%), were more likely to have an HIV-positive caregiver (43.7% versus 15.4%), were more likely to live with other HIV-positive people in the household (81.5% versus 26.0%), have other sicknesses in the family (29.6% versus 20.7%) and be from Malawi (29.6% versus 13.5%). They were also more likely to be food insecure (37.8% versus 25.2%), but less likely to care for other young children (36.2% versus 46.8%) compared to the other children.
Table 1.
Simple differences at baseline between HIV-positive children and non-HIV-positive children on demographic and socio-economic variables and cognitive and psychosocial outcomes. Data are M (SD) or N (%). Difference statistics are t (p) for continuous variables or χ2 (p) for proportions.
| Total | HIV-positive children | Non-HIV-positive children | Difference statistic (p-value) | |
|---|---|---|---|---|
| N=989 | N=135 | N=854 | ||
| Demographics | ||||
| Child gendera | 503 (51.4%) | 69 (51.1%) | 434 (51.4%) | 0.004 (.95) |
| Child age | 8.91 (2.84) | 9.08 (2.58) | 8.88 (2.88) | 0.84 (.40) |
| Carer gendera | 939 (94.9%) | 121 (89.6%) | 818 (95.8%) | 9.20 (.002) |
| Carer age | 43.69 (14.94) | 43.93 (14.94) | 43.66 (14.94) | 0.20 (.85) |
| Carer HIV positive | 189 (19.3%) | 59 (43.7%) | 130 (15.4%) | 59.84 (<.001) |
| Country | ||||
| South Africa | 834 (84.3%) | 95 (70.4%) | 739 (86.5%) | 23.04 (<.001) |
| Malawi | 155 (15.7%) | 40 (29.6%) | 115 (13.5%) | |
| Parent died | ||||
| Mother | 150 (17.8%) | 29 (22.8%) | 121 (16.9%) | 8.99 (.061) |
| Father | 154 (18.2%) | 17 (13.4%) | 137 (19.1%) | |
| Both | 149 (17.6%) | 30 (23.6%) | 119 (16.6%) | |
| None | 15 (1.8%) | 48 (37.8%) | 329 (45.8%) | |
| Don’t know | 15 (1.8%) | 3 (2.4%) | 12 (1.7%) | |
| Recent bereavement | 44 (32.6%) | 239 (28.0%) | 1.21 (.27) | |
| HIV in household | 332 (33.6%) | 110 (81.5%) | 222 (26.0%) | 160.94 (<.001) |
| Family sickness | 217 (21.9%) | 40 (29.6%) | 177 (20.7%) | 5.40 (.020) |
| Socio-economic variables | ||||
| Informal housing | 152 (15.5%) | 19 (14.1%) | 133 (15.8%) | 0.25 (.62) |
| Household employment | 526 (53.7%) | 69 (51.1%) | 457 (54.1%) | 0.43 (.51) |
| Number of people in household | 6.42 (2.90) | 6.18 (2.51) | 6.46 (2.96) | 1.00 (.32) |
| Food insecurity | 266 (26.9%) | 51 (37.8%) | 215 (25.2%) | 9.42 (.002) |
| Went to bed hungry last night | 127 (13.0%) | 18 (13.3%) | 109 (12.9%) | 0.018 (.89) |
| Any domestic violence | 462 (47.5%) | 63 (46.7%) | 399 (47.7%) | 0.047 (.83) |
| Any community violence | 413 (42.5%) | 57 (42.2%) | 356 (42.5%) | 0.005 (.95) |
| Any harsh physical discipline | 473 (47.8%) | 63 (46.7%) | 410 (48.0%) | 0.084 (.77) |
| Any harsh psychological discipline | 449 (45.4%) | 60 (44.4%) | 389 (45.6%) | 0.058 (.81) |
| Care for younger kids | 382 (45.2%) | 46 (36.2%) | 336 (46.8%) | 4.87 (.027) |
| Care for sick people | 343 (40.6%) | 52 (40.9%) | 291 (40.5%) | 0.008 (.93) |
| Enrolled in school | 952 (96.3%) | 130 (96.3%) | 822 (96.3%) | 0.001 (.98) |
| Developmental outcomes | ||||
| Developmental disability | 451 (45.6%) | 95 (70.4%) | 356 (41.7%) | 38.67 (<.001) |
| Stunting | 303 (31.7%) | 76 (58.8%) | 227 (27.4%) | 49.94 (<.001) |
| Wasting | 30 (3.1%) | 2 (1.5%) | 28 (3.4%) | 1.31 (.25) |
| Underweight | 45 (8.8%) | 14 (18.7%) | 31 (7.1%) | 10.75 (.001) |
| Physical functioning | 96.50 (10.41) | 93.37 (13.37) | 97.00 (9.78) | 3.03 (.003) |
| Emotional functioning | 89.29 (13.83) | 87.69 (14.00) | 89.55 (13.80) | 1.46 (.15) |
| Social functioning | 89.55 (15.44) | 89.57 (15.99) | 89.55 (15.37) | 0.013 (.99) |
| Educational functioning | 85.14 (22.19) | 79.29 (25.23) | 86.06 (21.55) | 2.90 (.004) |
| Quality of life | 90.96 (9.80) | 88.37 (10.84) | 91.37 (9.57) | 3.03 (.003) |
| Child depression score | 1.08 (1.65) | 0.99 (1.68) | 1.10 (1.65) | 0.67 (.50) |
| Suicidal ideation | 20 (2.0%) | 3 (2.2%) | 71 (2.0%) | 0.028 (.87) |
| Child self-esteem score | 20.99 (2.87) | 20.86 (3.39) | 21.02 (2.77) | 0.50 (.62) |
| Child trauma score | 3.58 (3.23) | 3.63 (3.02) | 3.57 (3.26) | 0.19 (.85) |
| Digit span | 8.77 (3.96) | 7.19 (3.87) | 9.03 (3.92) | 4.90 (<.001) |
| Draw-a-person score | 86.09 (18.56) | 79.18 (21.39) | 87.08 (17.91) | 3.66 (<.001) |
Number of females.
Baseline differences in development
While no differences between the HIV-positive children and the comparison group were found on psychosocial measures (see Table 1), various other differences were found. In terms of growth, HIV-positive children were more often stunted (58.8% versus 27.4%) and underweight (18.7% versus 7.1%; see Table 1). On average, they also had lower general physical functioning (M=93.37, SD=13.37) than non-HIV-positive children (M=97.00, SD=9.78). In the cognitive domain, HIV-positive children scored lower on the digit span test (M=7.19, SD=3.87 vs. M=9.03, SD=3.92) and the draw-a-person task (M=79.18, SD=21.39 vs. M=87.08, SD=17.91).
Unique association of child HIV status with cognitive and physical difficulties
Multivariable logistic regression analyses with child HIV status as predictor, controlled for the covariates country, caregiver gender, caregiver HIV status, household HIV, family sickness, food insecurity, and caring for younger children, were run to show the unique association between child HIV status andgrowth. It was found that HIV-positive children were more than three times as likely to be stunted (OR, 3.25; CI, 2.05-5.15).
Multivariable linear regression analyses controlling for the same covariates were performed to test the unique association of child HIV status with continuous cognitive and physical functioning variables. The differences between HIV-positive and non-HIV-positive children on digit span (B=−0.64, t(767)=1.69, p=.092) and draw-a-person scores (B=−2.23, t(735)=1.19, p=.23) were no longer significant. However, being HIV-positive was associated with significantly worse physical functioning (B=−4.17, t(836)=3.49, p=.001), and worse performance at school (B=−5.23, t(818)=2.17, p=.031). These difficulties were further reflected in a negative association between being HIV-positive and quality of life (B=−2.38, t(836)=2.29, p=.022).
When the HIV-positive children and the comparison group were examined on education variables, there were significant differences (see Fig. 1). A total educational risk score showed that HIV-positive children had higher educational risk (M=1.32, SD=1.23) compared to control children (M=0.69, SD=0.98, p<.001).
Figure 1.
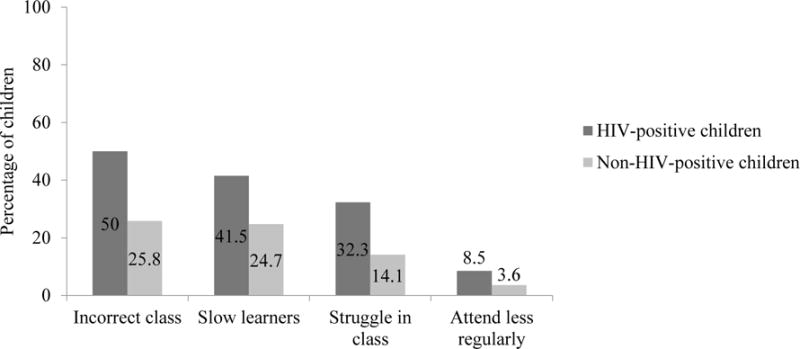
Percentage of children suffering from several educational risks according to their HIV status. All the differences were significant. p<.05.
Follow-up
At follow-up there was an 86.3% response rate with data from 854 children. Children lost to follow-up had younger parents on average (M=39.25, SD=14.64 vs M=44.39, SD=14.87; t(987)=3.74, p<.001), were more likely to live in South Africa (93.3% vs 82.7%; X2(1)=9.59, p=.002), more likely to live in informal housing (27.3% vs 13.7%; X2(1)=16.05, p<.001), more likely to not attend school (7.4% vs 3.2%; X2(1)=5.84, p<.001), and they were more often food secure (80.7% vs 71.9%; X2(1)=4.64, p=.031). All other variables did not differ significantly between those lost to follow-up and those followed up.
Cognitive and psychosocial development over time
At follow-up (see Table 2), HIV-positive children were still more likely to be stunted (X2(1)=29.30, p<.001) and underweight (X2(1)=5.64, p=.018). HIV-positive children also scored lower on the digit span task (t(826)=3.52, p<.001), on the draw-a-person task (t(834)=4.50, p<.001), on educational functioning (t(840)=2.85, p=.005), and on the quality of life scale (t(852)=3.08, p=.002). At follow-up trauma scores also differed significantly between groups, but it was the non-HIV-positive group that scored highest on PTSD (t(866)=2.68, p=.008). No other psychosocial and emotional differences were found between the two groups at follow-up.
Table 2.
Simple differences at follow-up between HIV-positive children and non-HIV-positive children on demographic and socio-economic variables and cognitive and psychosocial outcomes. Data are M (SD) or N (%). Difference statistics are t (p) for continuous variables or χ2 (p) for proportions.
| Total | HIV-positive children | Non-HIV-positive children | Difference statistic (p-value) | |
|---|---|---|---|---|
| N=854 | N=117 | N=737 | ||
| Stunting | 196 (23.6%) | 50 (43.5%) | 146 (20.4%) | 29.30 (<.001) |
| Wasting | 57 (6.8%) | 8 (6.8%) | 49 (6.8%) | <0.001 (.99) |
| Underweight | 33 (9.6%) | 9 (19.1%) | 24 (8.1%) | 5.64 (.018) |
| Physical functioning | 96.84 (9.66) | 97.52 (8.55) | 0.78 (.43) | |
| Emotional functioning | 89.69 (13.49) | 92.06 (11.57) | 1.80 (.074) | |
| Social functioning | 91.52 (14.39) | 94.05 (12.63) | 1.79 (.075) | |
| Educational functioning | 82.69 (22.04) | 88.83 (18.61) | 2.85 (.005) | |
| Quality of life | 91.04 (8.60) | 93.64 (7.80) | 3.08 (.002) | |
| Child depression score | 0.83 (1.91) | 0.80 (1.41) | 0.18 (.86) | |
| Child self-esteem score | 22.62 (4.00) | 22.19 (3.83) | 1.11 (.27) | |
| Child trauma score | 3.24 (3.71) | 4.20 (3.62) | 2.68 (.008) | |
| Digit span | 7.89 (3.65) | 9.14 (3.52) | 3.54 (<.001) | |
| Draw-a-person score | 83.61 (20.08) | 92.47 (16.48) | 4.50 (<.001) |
Cognitive and physical development by HIV status
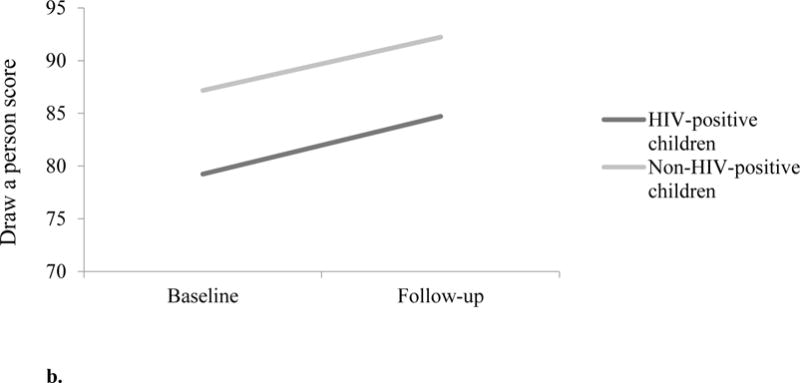
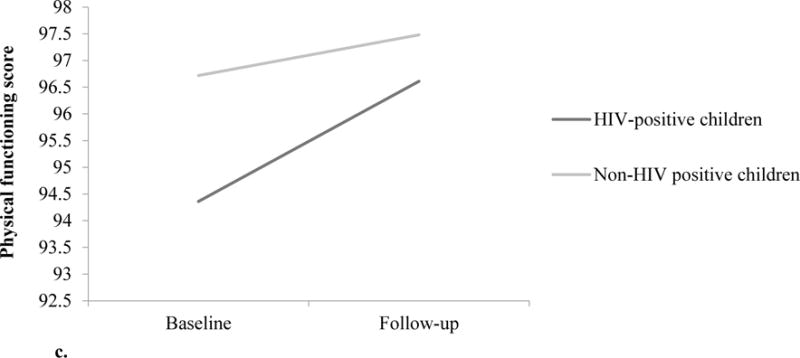
No difference in improvement of digit span was found between HIV-positive children and non-HIV-positive children (F(1, 651)=0.21, p=.73; see Fig. 2), even though the HIV-positive children significantly improved on digit span over time (t(107)=2.24, p=.027) while the non-HIV-positive children did not (t(658)=1.05, p=.30). The change over time of draw-a-person scores of HIV-positive and non-HIV-positive children also did not differ significantly (F(1, 635)=0.14, p=.71; see Fig. 2b), but the scores of the HIV-positive (t(94)=2.38, p=.019) as well as the non-HIV-positive children (t(638)=6.47, p<.001) improved from baseline to follow-up. Educational performance also did not change differently over time for the two groups (F(1, 708)=0.001, p=.98), although performance improved for the non-HIV-positive (t(705)=2.87, p=.004) and not for the HIV-positive children (t(112)=1.56, p=.12). However, change over time in physical functioning scores did differ between the two groups (F(1, 729)=4.03, p=.045; see Fig. 2c), as the HIV-positive children improved (t(116)=2.06, p=.042) while the non-HIV-positive children did not (t(736)=1.09, p=.28; (see Fig. 2). Overall quality of life did not increase more for the HIV-positive children than it did for the comparison group (F(1, 729)=0.22, p=.64), but it increased for the HIV-positive (t(116)=2.14, p=.035) and the non-HIV-positive individually (t(736)=5.24, p<.001).
Figure 2.
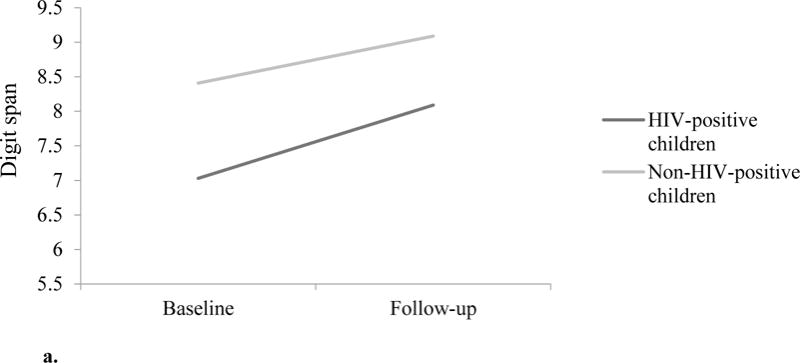
a. Improvement of working memory over time by child HIV status. The two groups did not differ significantly in change over time (F(1, 651)=0.21, p=.73).
b. Improvement of general cognitive development over time by child HIV status. The two groups did not differ significantly in change over time (F(1, 635)=0.14, p=.71).
c. Improvement of physical functioning over time by child HIV status. HIV-positive children improved significantly more over time than did the non-HIV positive children (F(1, 729)=4.03, p=.045).
Discussion
At baseline, the HIV positive children scored significantly lower on developmental measures compared to their non-HIV-positive counterparts. HIV positive children were more likely to perform poorly on cognitive assessments and have lower reported chool achievement. This confirms our previous findings of higher rates of developmental disability in such children (Skeen et al., 2014). They were also significantly more likely to be stunted. Yet other indices of child development, notably behavioural and emotional indices, did not differ between the groups.
At follow up, HIV positive children improved over time at similar rates to HIV negative children. The exceptions to this was physical functioning, where HIV positive children showed significant change compared to HIV negative children who did not improve at all.
This improvement might well be explained by the fact that these children received more medical care referrals from the CBO, and the fact that the overwhelming majority of these HIV-positive children were receiving antiretroviral therapy.
However, they remained significantly worse off than HIV negative children across almost all other domains. It is possible the same benefits are not being felt in other domains of development, possibility due to a lack of access to relevant services, or the complexity of interventions required.
Our study has also highlighted the important role of CBOs in intervening to improving child development outcomes. Firstly, we have shown that it is possible for CBOs to monitor developmental outcomes in low income communities using easy-to-administer inventories implemented by a trained lay health worker.
Secondly, our findings have implications for the type of programming that CBO programmes should be providing in their communities. Good examples of successful community-level programmes exist showing that providing specific services to promote child development to mitigate the impact of developmental difficulties associated with HIV is possible (Potterton et al., 2010, Luyirika, Kikule, Kamba, Buyondo, Batamwita, et al., 2011). Although there are several evidence based interventions to promote development (Sherr, Croome, Bradshaw, Parra Castaneda, 2014), and a large body of evidence of the benefits of special educational input (Merry et al., 2004[2011]), it appears that these children are not receiving the necessary specialised support. The CBOs in our study are serving the most vulnerable children and communities that are rarely reached by other services. Specific targeting, for example, of only HIV+ children in the context of the massive psychosocial adversity facing all families and children, is not a viable strategy. Having said that, our findings make it clear that there are particular difficulties faced by HIV+ve children that require an inclusive approach. The solution is not targeting but rather the CBOs broadening the services they offer into areas such as cognitive stimulation and screening for mental health difficulties.
These organisations need to work together with children’s caregivers, local schools and health services and the community at large to make use of local resources to support children with developmental delay. This has the potential to be of benefit for all children at risk in these communities.
Finally, studies suggest that antiretroviral treatment may help to reduce cognitive delay (Ngoma et al., 2014; Whitehead et al., 2014). HIV testing and treatment falls short for young children (Woldesenbet et al., 2015). As routine screening for HIV is suggested for adult attenders at STD and ante-natal clinics (Roberts et al., 2016), our data suggests it may be useful to consider paediatric testing of children showing developmental delay. As children grow and reach adolescence, cognitive development will be important for them to achieve milestones at school, consider personal decisions and navigate their environment successfully. Our data supplements clinic-based data to show the burden shouldered within the community.
Limitations
Our results need to be considered with some caution as HIV status was measured using carer report, and was not confirmed using biological testing. As such there may be underreporting. HIV treatment was only measured at follow-up, so change over time is not possible to determine. This study, as with others that focus on comparing outcomes between HIV+ and HIV- children, is likely to have included HIV-exposed but uninfected children in the sample. Little is known about the developmental trajectory of HIV-exposed children. There are limited validated tools available for screening for child development outcomes in LMIC. For the purpose of this study, we required screening tools and questionnaires that could be administered by trained data collectors that were not time-consuming or too onerous for participants, who are required to provide responses to a range of tools beyond those described in this paper. Linked to this is the lack of a gold standard robust measure of cognitive development such as the Kaufman Assessment Battery for Children or other measures of IQ. Conducting comprehensive IQ assessment batteries in these contexts is expensive and time-consuming, and where it is not possible to administer them, we need to consider the use of easily administered tablet based measures of executive function.
Conclusions
This study clearly demonstrated high levels of developmental problems among HIV-positive children in the community. Without specific intervention this often persists over time and was present despite high levels of reported antiretroviral treatment. Developmental and cognitive challenges are an important issue to be taken on board within HIV care packages. CBO’s may be well placed to provide support for these children within their broader programming.
References
- Bagley C, Bolitho F, Bertrand L. Norms and construct validity of the Rosenberg Self-Esteem Scale in Canadian high school populations: Implications for counselling. Canadian Journal of Counselling. 1997;31(1):82–92. [Google Scholar]
- Banks LM, Zuurmond M, Ferrand R, Kuper H. The relationship between HIV and prevalence of disabilities in sub-Saharan Africa: systematic review (FA) Tropical Medicine & International Health. 2015;20(4):411–29. doi: 10.1111/tmi.12449. [DOI] [PubMed] [Google Scholar]
- Bowler R, Smith M, Schwarzer R, Perez-Arce P, Kreutzer R. Neuropsychological and Academic Characteristics of Mexican-American Children: A Longitudinal Field Study. Applied Psychology: An International Review. 2002;51(3):458–478. [Google Scholar]
- Briere J. Professional Manual for the Trauma Symptom Checklist for Children (TSCC) Odessa, FL: Psychological Assessment Resources, Inc; 1996. [Google Scholar]
- Bryant M, Beard J, Sabin L, Brooks MI, Scott N, Larson BA, Simon J. PEPFAR’s support for orphans and vulnerable children: some beneficial effects, but too little data, and programs spread thin. Health Affairs. 2012;31(7):1508–1518. doi: 10.1377/hlthaff.2012.0230. [DOI] [PubMed] [Google Scholar]
- Chappell PA, Steitz JA. Young children’s human figure drawings and cognitive development. Perceptual & Motor Skills. 1993;76:611–617. doi: 10.2466/pms.1993.76.2.611. [DOI] [PubMed] [Google Scholar]
- Cluver L, Gardner F, Operario D. Psychological distress among AIDS-orphaned children in urban South Africa. Journal of Child Psychology and Psychiatry. 2007;48:755–63. doi: 10.1111/j.1469-7610.2007.01757.x. [DOI] [PubMed] [Google Scholar]
- Dunne MP, Zolotor AJ, Runyan DK, Andreva-Miller I, Choo WY, Youssef R. ISPCAN Child Abuse Screening Tools Retrospective version (ICAST-R): Delphi study and field testing in seven countries. Child Abuse & Neglect. 2009;33(11):815–825. doi: 10.1016/j.chiabu.2009.09.005. [DOI] [PubMed] [Google Scholar]
- Engle PL, Fernald LC, Alderman H, Behrman J, O’Gara C, Yousafzai A, Iltus S. Strategies for reducing inequalities and improving developmental outcomes for young children in low-income and middle-income countries. The Lancet. 2011;378(9799):1339–1353. doi: 10.1016/S0140-6736(11)60889-1. [DOI] [PubMed] [Google Scholar]
- Goodenough F. Measurement of intelligence by drawings. New York: World Book, Co.; 1926. [Google Scholar]
- Goodman R. The Strengths and Difficulties Questionnaire: A research not. Journal of Child Psychology and Psychiatry. 1997;38:581–6. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Goodman R, Meltzer H, Bailey V. The Strengths and Difficulties Questionnaire: A pilot study on the validity of the self-report version. European child & adolescent psychiatry. 1998;7(3):125–130. doi: 10.1007/s007870050057. [DOI] [PubMed] [Google Scholar]
- Gray-Little B, Williams VSL, Hancock TD. An item-response theory analysis of the Rosenberg Self-Esteem Scale. Personality and Social Psychology Bulletin. 1997;23:443–51. [Google Scholar]
- Griffiths RA, Beumont PJ, Giannakopoulos E, Russell J, Schotte D, Varano P. Measuring self-esteem in dieting disordered patients: The validity of the Rosenberg and Coopersmith contrasted. International Journal of Eating Disorders. 1999;25(2):227–31. doi: 10.1002/(sici)1098-108x(199903)25:2<227::aid-eat13>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- Harris D. Children’s drawings as a measure of intellectual maturity. New York, NY: Harcourt Brace & World, Inc.; 1963. [Google Scholar]
- King E, De Silva M, Stein A, Patel V. Interventions for improving the psychosocial well‐being of children affected by HIV and AIDS. The Cochrane Library. 2009 doi: 10.1002/14651858.CD006733.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M. Children’s Depression Inventory. North Tonawanda, NY: Multi Health Systems, Inc.; 1992. [Google Scholar]
- Lanktree CB, Gilbert AM, Briere J, Taylor N, Chen K, Saltzman WR. Multi-informant assessment of maltreated children: Convergent and discriminant validity of the TSCC and TSCYC. Child Abuse & Neglect. 2008;32:621–625. doi: 10.1016/j.chiabu.2007.10.003. [DOI] [PubMed] [Google Scholar]
- Lotz L, Loxton H, Naidoo AV. Visual-motor integration functioning in a South African middle childhood sample. Journal of child and adolescent mental health. 2005;17(2):63–67. doi: 10.2989/17280580509486602. [DOI] [PubMed] [Google Scholar]
- Loxton H, Mostert J, Moffatt D. Screening of intellectual maturity: Exploring South African preschoolers’ scores on the Goodenough-Harris drawing test and teachers’ assessment. Perceptual and motor skills. 2006;103(2):515–525. doi: 10.2466/pms.103.2.515-525. [DOI] [PubMed] [Google Scholar]
- Luyirika E, Kikule E, Kamba M, Buyondo F, Batamwita R, Featherstone A, Mills EJ. Meeting the challenges of disability and HIV in East Africa. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2011;57(3):e68–e69. doi: 10.1097/QAI.0b013e31821ac9a9. [DOI] [PubMed] [Google Scholar]
- Madge EM, van den Berg AR, Robinson M. Manual for the Junior South African Individual Scales (JSAIS) Pretoria: Human Science Research Council; 1985. [Google Scholar]
- Merry S, McDowell H, Hetrick S, Bir J, Muller N. Psychological and/or educational interventions for the prevention of depression in children and adolescents. Cochrane Database Syst Rev. 2004;1:CD003380. doi: 10.1002/14651858.CD003380.pub2. Review. Update in: Cochrane Database Syst Rev. 2011;(12):CD003380. [DOI] [PubMed] [Google Scholar]
- Mueller J, Alie C, Jonas B, Brown E, Sherr L. A quasi-experimental evlaution of a community-based art therapy intervention exploring the psychosocial health of children affected by HIV in South Africa. Tropical Medicine and International Health. 2011;16:57–66. doi: 10.1111/j.1365-3156.2010.02682.x. [DOI] [PubMed] [Google Scholar]
- Ngoma MS, Hunter JA, Harper JA, Church PT, Mumba, Silverman MS. Cognitive and language outcomes in HIV-uninfected infants exposed to combined antiretroviral therapy in utero and through extended breast-feeding. AIDS. 2014;28(Suppl 3):S323–30. doi: 10.1097/QAD.0000000000000357. [DOI] [PubMed] [Google Scholar]
- Nyangara F, O’Donnell K, Murphy R, Nyberg B. Child Status Index (CSI) – Field users’ guide – Measure evaluation. Washington, USA: United States Agency for International Development; 2009. [Google Scholar]
- O’Donnell K, Nyangara F, Murphy R, Cannon M, Nyberg B. Child Status Index Manual. Chapel Hill, NC: Measure Evaluation; 2008. Revised 2014. [Google Scholar]
- Potterton J, Stewart A, Cooper P, Becker P. The effect of a basic home stimulation programme on the development of young children infected with HIV. Developmental Medicine & Child Neurology. 2010;52(6):547–551. doi: 10.1111/j.1469-8749.2009.03534.x. [DOI] [PubMed] [Google Scholar]
- Powell K, Walker RW, Rogathe J, Gray WK, Hunter E, Newton CR, Burton K. Cognition and behavior in a prevalent cohort of children with epilepsy in rural northern Tanzania: A three-year follow-up study. Epilepsy & Behavior. 2015;51:117–123. doi: 10.1016/j.yebeh.2015.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts T, Cohn J, Bonner K, Hargreaves S. Scale-up of routine viral load testing in resource-poor settings: current and future implementation challenges. Clinical Infectious Diseases. 2016:ciw001. doi: 10.1093/cid/ciw001. pii. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- Runyan DK, Dunne MP, Zolotor AJ, Madrid B, Jain D, Youssef RM. The development and piloting of the ISPCAN Child Abuse Screening Tool-Parent version. (ICAST-P) Child Abuse and Neglect. 2009;33(11):826–32. doi: 10.1016/j.chiabu.2009.09.006. [DOI] [PubMed] [Google Scholar]
- Sharp C, Venta A, Marais L, Skinner D, Lenka M, Serekoane J. First evaluation of a population-based screen to detect emotional-behavior disorders in orphaned children in sub-Saharan Africa. AIDS and Behavior. 2014;1888:1174–1185. doi: 10.1007/s10461-014-0739-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherr L, Cluver LD, Betancourt TS, Kellerman SE, Richter LM, Desmond C. Evidence of impact: Health, psychological and social effects of adult HIV on children. AIDS. 2014;28(3):S251–9. doi: 10.1097/QAD.0000000000000327. [DOI] [PubMed] [Google Scholar]
- Sherr L, Croome N, Bradshaw K, Parra Castaneda K. A systematic review examining whether interventions are effective in reducing cognitive delay in children infected and affected with HIV. AIDS Care. 2014;26(1):S77–7. doi: 10.1080/09540121.2014.906560. [DOI] [PubMed] [Google Scholar]
- Sherr L, Croome N, Parra Castaneda K, Bradshaw K, Romero RH. Developmental challenges in HIV infected children – an updated systematic review. Children and Youth Services Review. 2014;45:74–78. [Google Scholar]
- Sherr L, Mueller J, Varrall R. A systematic review of cognitive development and child human immunodeficiency virus infection. Psychology, Health & Medicine. 2009;14(4):387–404. doi: 10.1080/13548500903012897. [DOI] [PubMed] [Google Scholar]
- Skeen S, Tomlinson M, Macedo A, Miltz A, Croome N, Sherr L. Child development in HIV-positive and HIV-affected children in South Africa and Malawi – What role for community organisations? Children and Youth Services Review. 2014;45:90–97. [Google Scholar]
- Stein A, Desmond C, Garbarino J, van Ijzendoorn MH, Barbarin O, Richter LM. Predicting long-term outcomes for children affected by HIV and AIDS: Pespectives from the scientific study of children’s development. AIDS. 2014;28(S3):S261–8. doi: 10.1097/QAD.0000000000000328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straus M, Hamby S, Finkelhor D, Moore D, Runyan D. Identification of child maltreatment with the Parent-Child Conflict Tactics Scales: Development and psychometric data for national sample of American parents. Child Abuse and Neglect. 1998;22:249–70. doi: 10.1016/s0145-2134(97)00174-9. [DOI] [PubMed] [Google Scholar]
- ter Laak J, de Goede M, Aleva A, van Rijswijk P. The Draw-A-Person Test: an indicator of children’s cognitive and socioemotional adaptation? Journal of Genetic Psychology. 2005;166(1):77–93. doi: 10.3200/GNTP.166.1.77-93. [DOI] [PubMed] [Google Scholar]
- Timbremont B, Braet C, Dreessen L. Assessing depression in youth: Relation between the Children’s Depression Inventory and a structured interview. Journal of Clinical Child and Adolescent Psychology. 2004;33:149–157. doi: 10.1207/S15374424JCCP3301_14. [DOI] [PubMed] [Google Scholar]
- Tomlinson M, Solomon W, Singh Y, Doherty T, Chopra M, Ijumba P, Tsai AC, Jackson D. The use of mobile phones as a data collection tool: A report from a household survey in South Africa. BMC Medical Informatics and Decision Making. 2009;9:51. doi: 10.1186/1472-6947-9-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. Strategic Guidance for Evaluating HIV Prevention Programmes. 2010 Retrieved fom: http://www.unaids.org/sites/default/files/sub_landing/files/12_7_MERG_Guidance_Evaluating%20HIV_PreventionProgrammes.pdf.
- Varni JW, Seid M, Kurtin PS. PedsQL 4.0: Reliability and validity of the Pediatric Quality of Life Inventory Version 4.0 Generic Core Scales in healthy and patient populations. Medical Care. 2001;39:800–812. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- Wechsler D. The Wechsler Intelligence Scale for Children—fourth edition. London, UK: Pearson Assessment; 2004. [Google Scholar]
- Westaway MS, Jordaan ER, Tsai J. Investigating the psychometric properties of the Rosenberg self-esteem scale for South African residents of greater Pretoria. Evaluation & the health professions. 2015;38(2):181–199. doi: 10.1177/0163278713504214. [DOI] [PubMed] [Google Scholar]
- Whitehead N, Potterton J, Coovadia A. The neurodevelopment of HIV-infected infants on HAART compared to HIV-exposed but uninfected infants. AIDS Care. 2014;26(4):497–504. doi: 10.1080/09540121.2013.841828. [DOI] [PubMed] [Google Scholar]
- Woldesenbet S, Jackson D, Lombard C, Dinh TH, Puren A, South African PMTCT Evaluation (SAPMCTE) Team Missed Opportunities along the Prevention of Mother-to-Child Transmission Services Cascade in South Africa: Uptake, Determinants, and Attributable Risk (the SAPMTCTE) PLoS One. 2015;10(7):e0132425. doi: 10.1371/journal.pone.0132425. [DOI] [PMC free article] [PubMed] [Google Scholar]


