Abstract
To investigate factors associated with surgical outcomes of cervical ossification of the posterior longitudinal ligament (OPLL). This retrospective study included patients (662 males and 251 females; mean age 55.8 years) with symptomatic OPLL. All patients had been diagnosed with OPLL based on cervical magnetic resonance imaging and computed tomography scans. Demographic, surgical outcome was measured using visual analog scale (VAS) and Japanese Orthopedic Association (JOA) scale scores. The results of our study indicated radicular pain was more common in segmental and circumscribe OPLL subtypes (P < 0.05). An anterior approach was favored in patients with less than 3 involved vertebral levels (P < 0.05). All surgical methods showed good outcomes (P < 0.05). Continuous and mixed OPLL subtypes showed worse surgical outcome with higher VAS and JOA scores (P < 0.05). Laminoplasty and anterior cervical discectomy and fusion were significantly associated with a higher recovery rate (P < 0.05). Among these patients, there were more complications with the anterior approach (P < 0.05). Male gender, open door laminoplasty ipsilateral, and ipsilateral-to-symptom-side opening were associated with postoperative C5 palsy (P < 0.05). Cervical OPLL may cause myelopathy, surgery is a safe and effective treatment for OPLL. There were no differences in clinical outcome according to surgical type, but complication rates varied depending on sex and surgical approach to symptom.
Keywords: laminoplasty, myelopathy, ossification of posterior longitudinal ligament
1. Introduction
Ossification of the posterior longitudinal ligament (OPLL) is a multifactorial disease resulting from pathologic OPLL that can cause stenotic changes in the spinal canal. It is recognized as one of the most common causes of severe cervical myelopathy and surgery is often necessary. OPLL is a common disease in Asian countries, and its prevalence has been reported to be 1.9% to 4.3% in Japan,[1–7] and 3.4% to 5.7% in Korea.[5,8,9] A variety of surgical approaches have been used to treat cervical OPLL, depending on the degree of compression, sagittal alignment, number of compressed levels, and the patient's general status.[2,10]
In single-level or 2-level disease, anterior cervical discectomy and fusion (ACDF) allows for direct resection of ossified tissues and complete decompression of the spinal cord can be achieved. However, in patients with multilevel (more than 3 involved vertebrae) OPLL, specifically continuous or mixed subtypes, anterior decompression is riskier and more difficult. As a result, poorer clinical results are frequently reported in these patients, and the posterior approach is often considered. However, this technique is still associated with many complications.[6,10–13]
In patients with cervical OPLL, clarifying the relevant factors associated with surgical outcomes will help to guide treatment.[14] However, relatively few large scale OPLL studies have been conducted.[5] The purpose of this study was to investigate relevant factors associated with surgical outcomes in cervical OPLL.
2. Methods
2.1. Patients and operations
This was a single-center retrospective study in Yonsei University Medical Center that evaluated 913 patients who underwent cervical surgery for OPLL (Anterior Cervical Discectomy Fusion, Laminoplasty, Posterior Cervical Fusion) (Figs. 1 and 2) from January 1998 to January 2012. All study methods were approved by the Ethics Committee of Severance Hospital of Yonsei University. Inclusion criteria were defined as follows: cervical OPLL involving level, surgical cases among all patients cases, minimum follow-up of 60 months. OPLL patients were excluded if their symptoms were associated with cervical spondylotic myelopathy from cervical stenosis or cervical deformity from spinal injury, tumor, infection, congenital disorders, or inflammatory arthritis (including ankylosing spondylitis and rheumatoid arthritis). Patients with occipitocervical fusion and cervicothoracic fusion were also excluded. All patients were reviewed and followed up with for a minimum 60 months. Symptom duration was divided into acute (<1 month), subacute (1–3 months), and chronic (>3 months). This study was conducted to retrospectively analyze the demographics, clinical presentation, and radiographic findings in patients with OPLL of the cervical spine. This information could serve as a basis for further studies and potentially guide OPLL treatment in the future. There is no need to obtain informed consent from patients because this is a retrospective study and all data were collected and analyzed anonymously.
Figure 1.
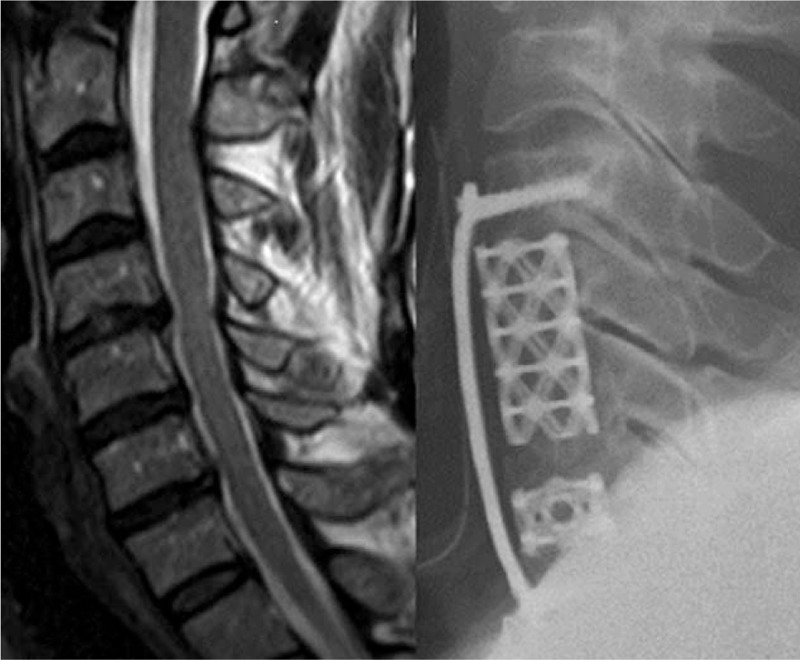
Anterior cervical corpectomy and discectomy fusion.
Figure 2.
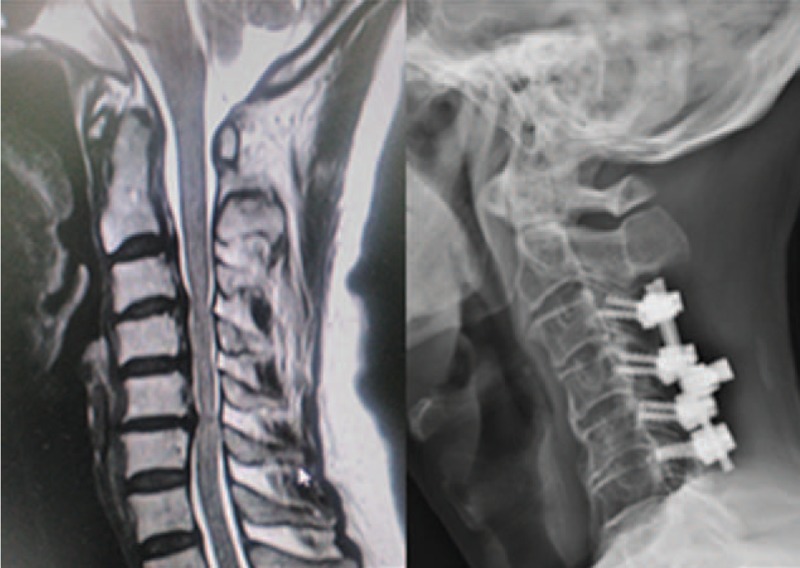
Posterior cervical laminectomy and fusion.
2.2. Radiological and clinical assessment
Computed tomography and magnetic resonance imaging scans of the cervical spine were obtained preoperatively in all cases. Plain X-rays were taken preoperatively and 1, 3, 6, 12, 24, 36, 48, and 60 months postoperatively. C2 to C7 Cobb angle was measured. We subdivided OPLL patients based on the classification system developed by the Japanese Investigation Committee on the Ossification of the Spinal Ligaments that includes localized, segmental, and mixed types. Following laminoplasty, we examined patients’ kyphotic posture by measuring the cervical Cobb angle. By comparing results between pre- and postoperative cervical sagittal alignment, we classified the level of kyphotic changes into 3 subsets by evaluating the changes in C2 to C7 Cobb angle in patients with a laminoplasty: 0°, 0° to 10°, and >10° (lordotic). We also calculated differences in pre- and postoperative clinical outcomes using the visual analog scale (VAS) and Japanese Orthopedic Association (JOA) scores.
2.3. Statistical analysis
Data were presented as the number of subjects or mean ± standard deviation. Comparison of each independent variable between the 2 groups was done by using the independent-sample Student t test for continuous variables and the Chi-squared test, linear-by-linear association, or Fisher exact test for categorical variables. Data analyses were performed using SPSS version 18 for Windows (SPSS, Inc., Chicago, IL).
3. Results
3.1. Patient demographics
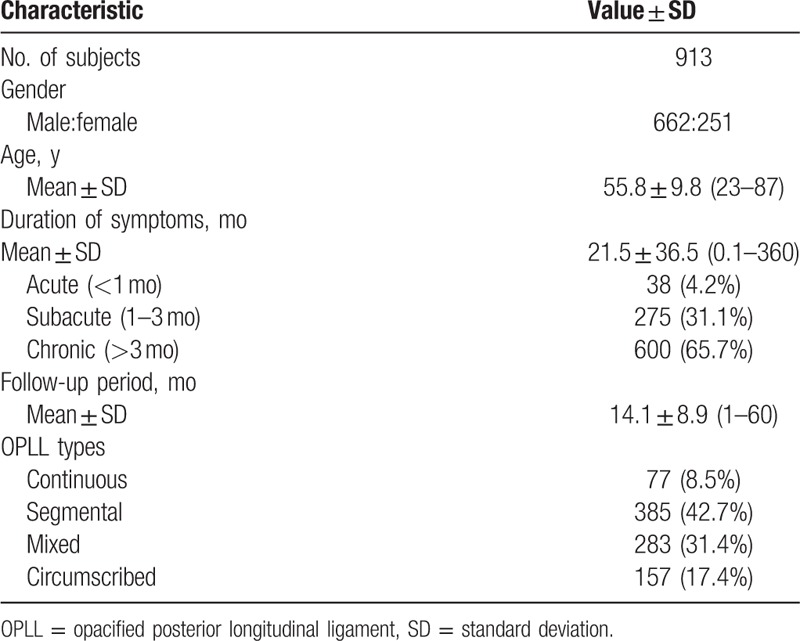
Patient demographic data are summarized in Table 1. The mean preoperative symptom duration was 21.5 months (range 0.1–360 months). The mean follow-up period was 14 months (1–60 months). The majority of patients were male (662 males:251 females) and segmental type OPLL was the most common (42.7%), and also the effects of preoperative variables (age, symptom duration, follow-up period, and OPLL types).
Table 1.
Cervical OPLL patient demographic information.
3.2. Clinical outcome
Clinical outcomes according to surgical approaches are visualized in Figures 3 and 4. The recovery pattern of clinical outcome was similar among the groups. Lower preoperative VAS scores were seen in the laminectomy and combined groups. Until 60 months postoperative, the combined approach group showed lower VAS scores, but the differences were not significant. The posterior approach group showed worse preoperative JOA scores. Laminectomy, posterior fusion and combined surgery showed worse final JOA scores (P < 0.05).
Figure 3.
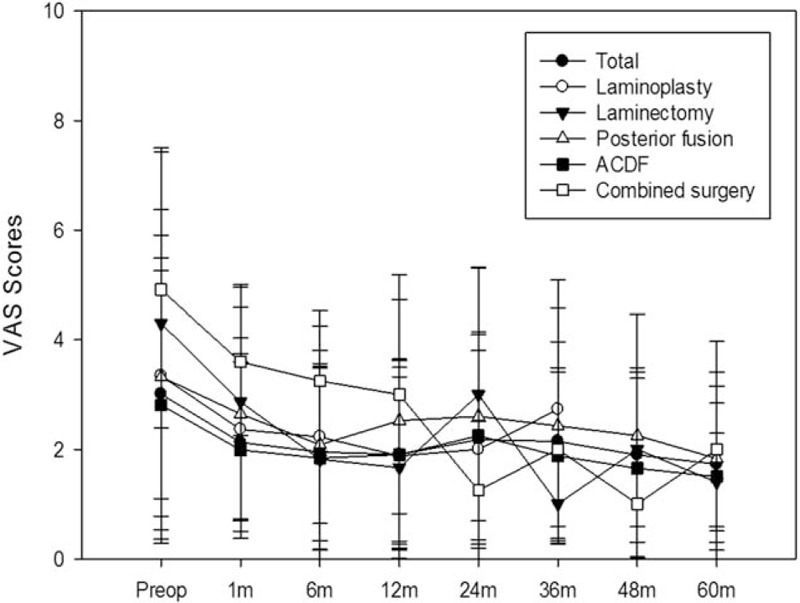
Comparison of baseline and postoperative visual analog scale scores according to surgical technique.
Figure 4.
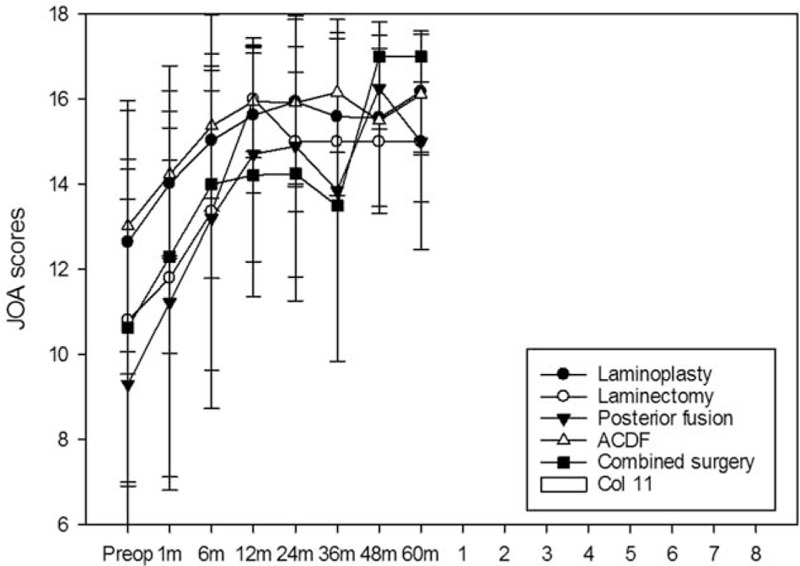
Comparison of baseline and postoperative Japanese Orthopedic Association scores according to surgical technique.
3.3. Surgical procedures
We investigated the choice of surgical approaches in OPLL (Fig. 5). The anterior approach was the most common (55.78%), followed by posterior approach (43%) and combined approach (1.2%). In patients with less than 3 involved spinal levels, the anterior approach was the most common choice and in patients with 3 or more involved spinal levels, the posterior approach was typically used.
Figure 5.
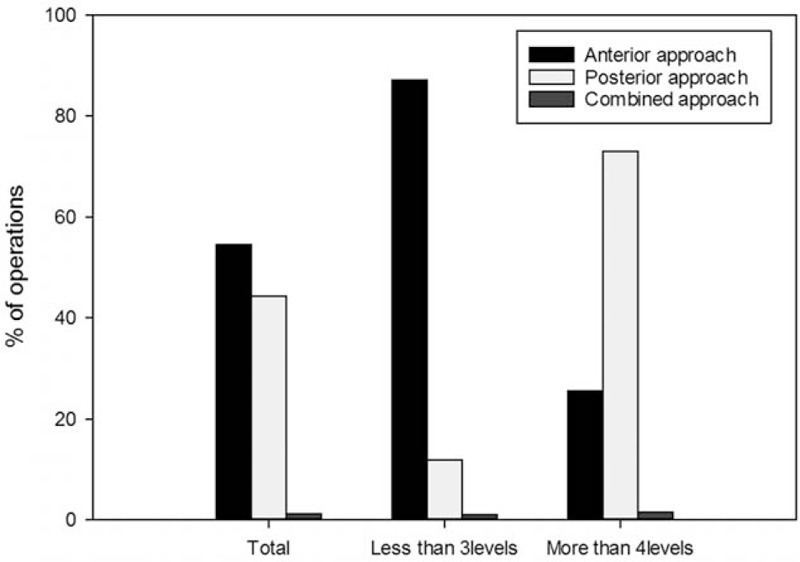
The choice of surgical techniques according to the involved level. Anterior versus posterior.
3.4. Radiologic progression
We investigated the relationship between C2 and C7 Cobb angle in the neutral position and various surgical techniques (Fig. 6). Posterior fusion and laminoplasty have higher progression C2 to C7 Cobb angle but slightly higher in patients who underwent laminoplasty surgery.
Figure 6.
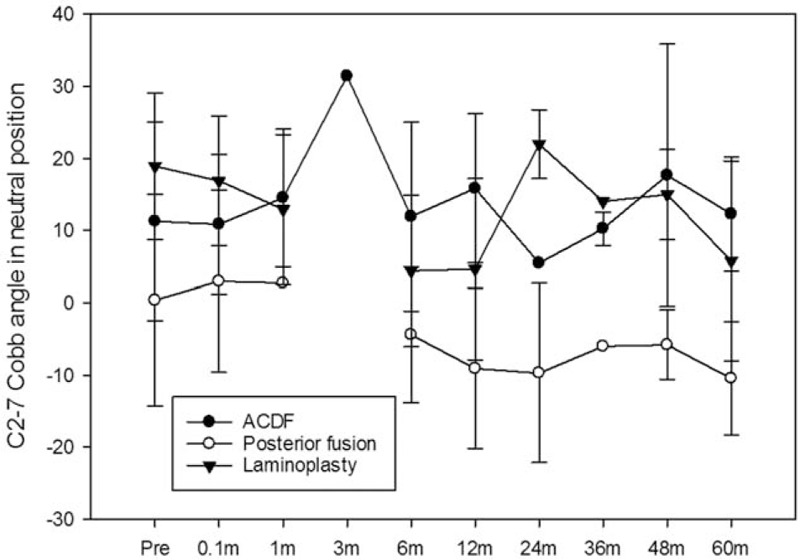
C2 to C7 Cobb angle neutral position according to surgical technique.
3.5. Complications
Postoperative complications were significantly more common in the anterior approach group than the posterior approach. Cerebrospinal fluid (CSF) leakage occurred in 21 patients (2.3%), C5 palsy occurred in 18 patients (2%), and neurological compromise occurred 9 patients (1%).
4. Discussion
Our study evaluated surgical approaches in the treatment of cervical OPLL. The majority of patients in this study were male. This result is consistent with a previous study.[2] In our study, mean patient age was 55.8 years old and this was also consistent with previous OPLL research.[2] Duration of symptoms mostly chronic state. According to OPLL types our study identified mostly segmental.
Surgical management of OPLL, specifically the choice of anterior or posterior approach, is a controversial issue. It is thought best for a neurosurgeon to perform surgery by the most familiar method also by comparation the advantages and disadvantages of each surgical method.[12,15–19] A consensus has not been reached about the most effective surgical management of cervical OPLL. Some researchers have suggested that anterior decompression is associated with better outcome regardless of the canal-occupying ratio and neural function postoperatively, whereas other studies have demonstrated better success with posterior decompression.[20] As relatively few studies have been published regarding the choice of surgical technique for cervical OPLL, our findings are helpful for selecting an appropriate surgical approach and identifying factors that could determine clinical improvement after cervical OPLL surgery.
Improvements in JOA and VAS scores were observed in all posterior neck surgery methods and showed substantial differences between groups (Figs. 3 and 4). Previous studies have demonstrated similar results.[12,15] Although the choice of surgical approach is a critical factor with regard to postoperative complications, the location of spinal cord compression and sagittal alignment of cervical spine need to be considered when choosing operative technique.[14,21]
This study identified that the anterior approach was more commonly performed in patients with cervical OPLL. A variety of complications were associated with the anterior approach, likely due to the soft tissue structure surrounding at the entry site of surgery, more than 3 involved level more frequent complication because technically demanding.[4,10,22–27] ACDF and laminoplasty produces long-lasting improvement, confirmed at 5-year follow-up. Not only have favorable results been achieved higher recovery rate. Our study showed that the ossified cervical curve progression was increased regardless of the laminoplasty method. The cervical C2 to C7 Cobb angle at baseline varied somewhat by group because we usually performed posterior fusion in patients with neutral or correctable kyphosis.[25,28]
Patients in this study had a wide range of follow-up times, ranging from 12 to 60 months. A previous study reported that ossification type was closely related to the outcome of laminoplasty. Our study showed that continuous and mixed subtypes showed worse surgical outcome with higher VAS and JOA scores.[29] Previous researchers discussed the use of titanium miniplates that permitted adequate decompression of the cervical spinal cord and bilateral cervical nerve roots. They showed successful reconstruction of an enlarged rigid spinal canal this similar with our study that showed laminoplasty and ACDF have higher recovery rate among others.[14,30–34] However, there were significant differences among the 3 groups in both C2 to C7 Cobb angle in neutral position during the study period (Fig. 5). Our study, all patients who underwent posterior neck surgery tended to lose greater cervical lordosis (Fig. 6).
The choice of surgical method for cervical OPLL was divided into 2 approaches: anterior or posterior. When planning the approach, the neurosurgeon should consider factors such as the location of spinal cord compression, number of levels involved, the sagittal alignment of the cervical spine, and general health status of the patient.[2,10,35–37]
After posterior surgeries, our study showed a few complications. In patients who underwent anterior surgery, the incidence of CSF leakage and C5 palsy were significantly higher.[38] The significance of demographic factors has been widely studied, but their role in guiding surgical approach has not been demonstrated. In our study, male gender and open door laminoplasty ipsilateral, and ipsilateral-to-symptom-side opening were significantly associated with postoperative C5 palsy.
Our study had several limitations. First, this study was a retrospective clinical analysis at a single institution. Therefore, the possibility of selection bias exists. If patients with worse outcome could be followed, the results of this study would not be critical for selecting the appropriate surgical approach. Second, this study did not include preoperative measurement of dynamic factors, such as cervical range of motion, loss of cervical lordosis, and T1 sagittal slope. It is important to identify the relationships between cervical dynamic factors and surgical outcome in the treatment of OPLL. Our study could support the benefits of an anterior approach in the management of cervical OPLL, but we cannot definitively conclude whether it is superior to other treatment strategies. In conclusion the present study demonstrates that cervical OPLL compression may cause myelopathy, satisfied results can be achieved with surgery. There were no differences in clinical outcome according to surgical type, but complication rates varied depending on sex and surgical approach to symptom.
Author contributions
Conceptualization: Dong Ah Shin, Do Heum Yoon.
Data curation: Farid Yudoyono.
Formal analysis: Farid Yudoyono, Bong Ju Moon.
Investigation: Yoon Ha.
Methodology: Farid Yudoyono, Pyung Go Cho, Sang Hyuk Park, Seong Yi.
Project administration: Dong Ah Shin.
Software: Farid Yudoyono.
Supervision: Dong Ah Shin, Keung Nyun Kim.
Writing – original draft: Farid Yudoyono.
Writing – review & editing: Farid Yudoyono, Dong Ah Shin.
Footnotes
Abbreviations: ACDF = anterior cervical discectomy and fusion, OPLL = ossification of the posterior longitudinal ligament.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Maruo K, Moriyama T, Tachibana T, et al. The impact of dynamic factors on surgical outcomes after double-door laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine. J Neurosurg Spine 2014;21:938–43. [DOI] [PubMed] [Google Scholar]
- [2].Lee CK, Shin DA, Yi S, et al. Correlation between cervical spine sagittal alignment and clinical outcome after cervical laminoplasty for ossification of the posterior longitudinal ligament. J Neurosurg Spine 2016;24:100–7. [DOI] [PubMed] [Google Scholar]
- [3].Jeong SY, Eun JP, Oh YM. Magnetic resonance imaging analysis of deep cervical flexors in patients with ossification of the posterior longitudinal ligament and clinical implication. Am J Phys Med Rehabil 2015;94:967–74. [DOI] [PubMed] [Google Scholar]
- [4].Yang H, Lu XH, Wang X, et al. A new method to determine whether ossified posterior longitudinal ligament can be resected completely and safely: spinal canal “Rule of Nine” on axial computed tomography. Eur Spine J 2015;24:1673–80. [DOI] [PubMed] [Google Scholar]
- [5].Jeon TS, Chang H, Choi BW. Analysis of demographics, clinical, and radiographical findings of ossification of posterior longitudinal ligament of the cervical spine in 146 Korean patients. Spine 2012;37:E1498–503. [DOI] [PubMed] [Google Scholar]
- [6].Xing D, Wang J, Ma JX, et al. Qualitative evidence from a systematic review of prognostic predictors for surgical outcomes following cervical ossification of the posterior longitudinal ligament. J Clin Neurosci 2013;20:625–33. [DOI] [PubMed] [Google Scholar]
- [7].Yoshimura N, Nagata K, Muraki S, et al. Prevalence and progression of radiographic ossification of the posterior longitudinal ligament and associated factors in the Japanese population: a 3-year follow-up of the ROAD study. Osteoporos Int 2014;25:1089–98. [DOI] [PubMed] [Google Scholar]
- [8].Sohn S, Chung CK, Yun TJ, et al. Epidemiological survey of ossification of the posterior longitudinal ligament in an adult Korean population: three dimensional computed tomographic observation of 3,240 cases. Calcif Tissue Int 2014;94:613–20. [DOI] [PubMed] [Google Scholar]
- [9].Kang MS, Lee JW, Zhang HY, et al. Diagnosis of cervical OPLL in lateral radiograph and MRI: is it reliable? Korean J Spine 2012;9:205–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Liu K, Shi J, Jia L, et al. Hemilaminectomy and unilateral lateral mass fixation for cervical ossification of the posterior longitudinal ligament. Clin Orthop Relat Res 2013;471:2219–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Lee SE, Chung CK, Jahng TA, et al. Long-term outcome of laminectomy for cervical ossification of the posterior longitudinal ligament. J Neurosurg Spine 2013;18:465–71. [DOI] [PubMed] [Google Scholar]
- [12].Lee CH, Jang TA, Hyun SJ, et al. Expansive laminoplasty versus laminectomy alone versus laminectomy and fusion for cervical ossification of the posterior longitudinal ligament, is there a difference in the clinical outcome and sagittal alignment? Clin Spine Surg 2016;29:E9–15. [DOI] [PubMed] [Google Scholar]
- [13].Nakashima H, Tetreault L, Nagoshi N, et al. Comparison of outcomes of surgical treatment for ossification of the posterior longitudinal ligament versus other forms of degenerative cervical myelopathy. J Bone Joint Surg Am 2016;98:370–8. [DOI] [PubMed] [Google Scholar]
- [14].Gu Y, Shi J, Cao P, et al. Clinical and imaging predictors of surgical outcome in multilevel cervical ossification of posterior longitudinal ligament: an analysis of 184 patients. PLoS One 2015;10:e0136042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Fujimori T, Iwasaki M, Okuda S, et al. Long-term results of cervical myelopathy due to ossification of the posterior longitudinal ligament with an occupying ratio of 60% or more. Spine 2013;39:58–67. [DOI] [PubMed] [Google Scholar]
- [16].Hirabayashi S, Yamada H, Motosuneya T, et al. Comparison of enlargement of the spinal canal after cervical laminoplasty: open-door type and double-door type. Eur Spine J 2010;19:1690–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Kotani Y, Abumi K, Ito M, et al. Minimum 2-year outcome of cervical laminoplasty with deep extensor muscle-preserving approach: impact on cervical spine function and quality of life. Eur Spine J 2009;18:663–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Fujiyoshi T, Yamazaki M, Okawa A, et al. Static versus dynamic factors for the development of myelopathy in patients with cervical ossification of the posterior longitudinal ligament. J Clin Neurosci 2010;17:320–4. [DOI] [PubMed] [Google Scholar]
- [19].Zhang P, Shen Y, Zhang YZ, et al. Preserving the C7 spinous process in laminectomy combined with lateral mass screw to prevent axial symptom. J Orthop Sci 2011;16:492–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Kim BW, Yoon DH, Shin HC, et al. Surgical outcome and prognostic factors of anterior decompression and fusion for cervical compressive myelopathy due to ossification of the posterior longitudinal ligament. Spine J 2015;15:875–84. [DOI] [PubMed] [Google Scholar]
- [21].Choi JH, Shin JJ, Kim TH, et al. Does intramedullary signal intensity on MRI affect the surgical outcomes of patients with ossification of posterior longitudinal ligament? J Korean Neurosurg Soc 2014;56:121–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Chen Y, Chen D, Wang X, et al. Significance of segmental instability in cervical ossification of the posterior longitudinal ligament and treated by a posterior hybrid technique. Arch Orthop Trauma Surg 2013;133:171–7. [DOI] [PubMed] [Google Scholar]
- [23].Feng F, Ruan W, Liu Z, et al. Anterior versus posterior approach for the treatment of cervical compressive myelopathy due to ossification of the posterior longitudinal ligament: a systematic review and meta-analysis. Int J Surg 2016;27:26–33. [DOI] [PubMed] [Google Scholar]
- [24].Chen Y, Chen D, Wang X, et al. Anterior corpectomy and fusion for severe ossification of posterior longitudinal ligament in the cervical spine. Int Orthop 2009;33:477–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Hida K, Yano S, Iwasaki Y. Considerations in the treatment of cervical ossification of the posterior longitudinal ligament. Clin Neurosurg 2008;55:126–32. [PubMed] [Google Scholar]
- [26].Highsmith JM, Dhall SS, Haid RW, Jr, et al. Treatment of cervical stenotic myelopathy: a cost and outcome comparison of laminoplasty versus laminectomy and lateral mass fusion. J Neurosurg Spine 2011;14:619–25. [DOI] [PubMed] [Google Scholar]
- [27].Liu X, Min S, Zhang H, et al. Anterior corpectomy versus posterior laminoplasty for multilevel cervical myelopathy: a systematic review and meta-analysis. Eur Spine J 2014;23:362–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Yusof MI, Hassan E, Abdullah S. Predicted cervical canal enlargement and effective cord decompression following expansive laminoplasty using cervical magnetic resonance imaging. Surg Radiol Anat 2011;33:109–15. [DOI] [PubMed] [Google Scholar]
- [29].Li H, Jiang LS, Dai LY. A review of prognostic factors for surgical outcome of ossification of the posterior longitudinal ligament of cervical spine. Eur Spine J 2008;17:1277–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Mori E, Ueta T, Maeda T, et al. Effect of preservation of the C-6 spinous process and its paraspinal muscular attachment on the prevention of postoperative axial neck pain in C3–6 laminoplasty. J Neurosurg Spine 2015;22:221–9. [DOI] [PubMed] [Google Scholar]
- [31].Smith ZA, Buchanan CC, Raphael D, et al. Ossification of the posterior longitudinal ligament: pathogenesis, management, and current surgical approaches. A review. Neurosurg Focus 2011;30:E1–0. [DOI] [PubMed] [Google Scholar]
- [32].Park HG, Zhang HY, Lee SH. Box-shape cervical expansive laminoplasty: clinical and radiological outcomes. Korean J Spine 2014;11:152–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Nishida N, Kanchiku T, Kato Y, et al. Biomechanical analysis of cervical myelopathy due to ossification of the posterior longitudinal ligament: effects of posterior decompression and kyphosis following decompression. Exp Ther Med 2014;7:1095–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Masaki U, Yamazaki M, Okawa A, et al. An analysis of factors causing poor surgical outcome in patients with cervical myelopathy due to ossification of the posterior longitudinal ligament anterior decompression with spinal fusion versus laminoplasty. J Spinal Disord Tech 2007;20:7–13. [DOI] [PubMed] [Google Scholar]
- [35].Kwon SY, Shin JJ, Lee JH, et al. Prognostic factors for surgical outcome in spinal cord injury associated with ossification of the posterior longitudinal ligament (OPLL). J Orthop Surg Res 2015;10:2–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Heller JG, Raich AL, Dettori JR, et al. Comparative effectiveness of different types of cervical laminoplasty. Evid Based Spine Care J 2013;4:105–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Seng C, Tow BP, Siddiqui MA, et al. Surgically treated cervical myelopathy: a functional outcome comparison study between multilevel anterior cervical decompression fusion with instrumentation and posterior laminoplasty. Spine J 2013;13:723–31. [DOI] [PubMed] [Google Scholar]
- [38].Imagama S, Matsuyama Y, Yukawa Y, et al. C5 palsy after cervical laminoplasty a multicentre study. J Bone Joint Surg Br 2010;92:393–400. [DOI] [PubMed] [Google Scholar]


