Abstract
Rationale:
Metoprolol and amiodarone are common antiarrhythmic drugs used in clinics throughout the world. The taste and smell alterations induced by antiarrhythmic drugs remain uncommon throughout the world, with less than 10 reported cases.
Patient concerns:
In this case report, we describe a case of a 73-year-old female, diagnosed with arrhythmias, was treated for metoprolol. At the third week of metoprolol treatment, the patient noticed a qualitative change in her ability to smell, also called dysosmia. After the metoprolol was tapered, her ability to smell was recovered. However, her arrhythmia was getting worse and the patient was given amiodarone. After using amiodarone for about 2 weeks, the patient felt hypogeusia, or loss of taste sensation.
Diagnoses:
The patient was diagnosed as dysosmia and taste disturbance induced by the antiarrhythmic drugs.
Interventions:
After noticed the side effects of the antiarrhythmic drugs, we asked the patient to abandon the drugs and have a radiofrequency ablation.
Outcomes:
Her ability of smell and taste were recovered after withdrawing the antiarrhythmic drugs. Also, in the follow-up appointment, she reported no complaints of smell or taste anymore.
Lessons:
These rare sensory disorders induced by anti-arrhythmic drugs were less documented in past literature. Our case report describes a patient with an arrhythmia who suffered reversible dysosmia and hypogeusia after taking metoprolol and amiodarone, respectively. We conclude that smell and taste disorders should be made aware to patients during the anti-arrhythmic treatment, helping to promote the safety of patients and drug compliance.
Keywords: amiodarone, antiarrhythmic drugs, metoprolol, side effects, smell, taste
1. Introduction
Antiarrhythmic drugs, including metoprolol and amiodarone, are widely used in cardiac disease. Metoprolol is a common beta1-selective adrenoceptor blocking drug used mainly used for management of hypertension, coronary heart disease, heart failure, and various arrhythmias.[1] Similar to other beta-adrenergic blockers, the most common side effects of metoprolol include fatigue, weakness, headache, cold peripheries, and gastrointestinal reaction.[1] Metoprolol has the unique ability to enter the central nervous system (CNS) and affect its function.[2] Amiodarone is another effective antiarrhythmic drug used primarily for supraventricular and ventricular arrhythmias. The adverse events of amiodarone are relatively higher than other antiarrhythmic drugs.[3] Long-term use increases the risk for side effects, including hyperthyroidism, elevated aminotransferase, pulmonary toxicity, and gastrointestinal reaction.[4]
Cranial nerve function damage has rarely been reported in the past literature. To our knowledge, it was first introduced by Vital Durand[5] that a recurrent anosmia was induced by metoprolol. Following this report, these rare but serious adverse effects have gained increased attention. The taste and smell alterations induced by antiarrhythmic drugs remain uncommon throughout the world, with less than 10 reported cases. Herein, we first report a case of reversible dysosmia and hypogeusia following the use of antiarrhythmic drugs metoprolol and amiodarone, respectively.
2. Case report
A 73-year-old female was admitted to our clinic with chest distress and palpitations. The physical examination revealed no positive findings. Electrocardiograph (EEG) and dynamic EEG (DCG) showed arrhythmias, including paroxysmal atrial fibrillation, paroxysmal supraventricular tachycardia, atrial premature beats, and ventricular premature beats. A cardiac B-mode ultrasound showed mild aortic valvular regurgitation and left ventricular diastolic dysfunction. Coronary artery CT found stenosis of the left anterior descending artery (50%). Laboratory findings, including blood chemistry and myocardial enzymes, were normal. The patient was prescribed 100 mg aspirin once a day for 2 months by another center. We decided to continue this existing treatment and add metoprolol 47.5 mg/day for her symptoms. Before our treatment, no examination for sense of smell or taste was performed, and the patient did not report any abnormalities in her ability to smell or taste.
After 2 weeks of metoprolol therapy, the patient reported decreased chest distress and palpitations. She reduced her metoprolol dose to 23.75 mg/day without reporting to the clinic her dose alteration. At the third week of metoprolol treatment, the patient noticed a smell disorder, reporting that she could not perceive the same smells as her relatives. And this disorder continued to worsen until complete anosmia. However, she continued this dosage and did not report to the clinic her new symptoms. During this period of time, the patient denied having exposure to chemicals, using other drugs, or experiencing a traumatic nose injury. Approximately 3 months after starting metoprolol, the patient returned to our clinic with the compliant of an olfactory disorder. No abnormalities were found during the endoscopic nasal examination, with normal color. No gland or turbinate hypertrophy was found. No obstruction or excess secretion was noted in the nasal passages, and the olfactory epithelium showed no signs of congestion or inflammation. It was determined that the olfactory dysfunction was an adverse effect of metoprolol. Considering her better initial symptoms and repeated DCG result, the metoprolol was tapered. The patient recovered from the olfactory dysfunction 3 weeks later, as determined by her ability to once again perceive the smell of soap. By the second month after discharging metoprolol, the patient's ability to recognize smells was returning back to baseline (Fig. 1). Also, in the follow-up appointment, she reported no complaints of smell or taste anymore.
Figure 1.
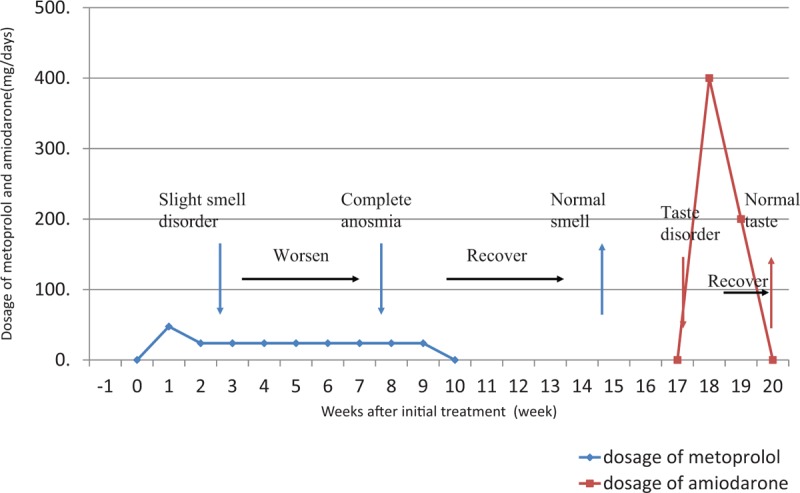
Dosage of metoprolol and amiodarone and time-course of dysosmia and dysgeusia in the antiarrhythmic treatment.
Nevertheless, the patient complained that her palpitations were getting worse following discontinuation of metoprolol. Dynamic electrocardiogram presented premature atrial beats and increasing paroxysmal atrial fibrillation. Therefore, the patient was given amiodarone 400 mg/day for 1 week to treat her arrhythmias, and then was tapered to 200 mg/day. However, after using amiodarone for approximately 2 weeks, the patient was not able to distinguish the tastes of bitter and spicy. Considering the potential side effects of amiodarone, we asked her to abandon the drug and have a radiofrequency ablation. Thus, the patient regained her ability to differentiate tastes 2 weeks following amiodarone discontinuation (Fig. 1).
The authors obtained written consent from the patient to describe her illness and publish this case report. Ethics committee approval is not included, as it is commonly accepted that case reports do not require such approval. In our work, we did not use patient data that would allow identifying her. The patient agreed to the diagnostic tests and treatments used to manage her medical conditions.
3. Discussion
Metoprolol and amiodarone have been wildly reported owing to their protective effects of the cardiovascular system. They can efficiently improve the morbidity and mortality of patients suffering from cardiovascular diseases, including hypertension, coronary heart disease, heart failure, and various arrhythmias.[6] In addition to common side effects of pulmonary or cardiac of beta blockers, metoprolol was more likely to cause CNS side effects through its higher concentrations in the brain.[1] Dysosmia, or smell disorder, is a rare side effect of metoprolol. Meanwhile, adverse events caused by amiodarone including lung toxicity and thyroid dysfunction were mainly related to the dosage and duration.[7] Although dysosmia has been reported as an adverse side effect of amiodarone, hypogeusia or taste disorder of amiodarone was rarely mentioned in the past.[3]
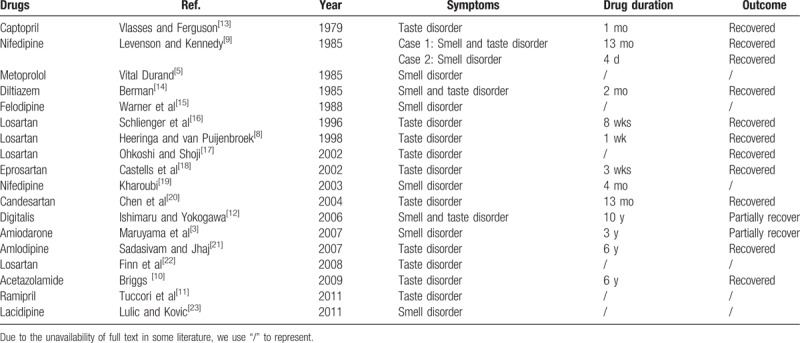
Since first introduced by Vital Durand in 1985,[5] dysosmia and hypogeusia were subsequently reported as side effects of other cardiovascular drugs, including conversion enzyme [angiotensin-converting enzyme (ACE)] inhibitors,[8] calcium antagonist,[9] diuretics, and other antiarrhythmic drugs[10–23] (Table 1). In this case, the patient complained of an olfactory disorder after 3 weeks of using metoprolol, with ongoing use causing further deterioration. After discontinuing metoprolol, the patient regained her ability to smell. In addition, a taste disorder occurred after amiodarone treatment, and was subsequently reversed following discontinuation of the offending agent. Generally, these reversible sensory dysfunctions induced by metoprolol and amiodarone are rare, and the associated clinical research is lacking. Although past literature has summarized the drug-induced taste and smell disorders and the potential mechanisms, the actual frequency, clinical characteristics, and dosage correlation of drugs, especially antiarrhythmic drugs, remains vague.[11] The potential mechanism of cardiovascular drug-induced dysosmia or hypogeusia may involve complex mechanisms. Abnormalities of binding to olfactory receptors, inactivation of post-receptor signal transduction pathway, and dysfunction of the corresponding nerves induced by Na+ or Ca2+ channel inhibition, may be the potential causes of the smell disorder.[24] Other studies suggested that damage to receptor cells could be caused by interference of second messengers or intermediates of Na–K–ATPase, or inhibition of protein synthesis could also function in the pathogenesis of dysosmia.[12] Similarly, the taste disorder was also proposed to have resulted from the same mechanisms that caused dysosmia.[24] However, the receptors for the 5 basic tastes (sweet, sour, bitter, salty, and umami) may be regulated by different systems. The sour and salty tastes receptors are activated by H+ and Na+ channel, respectively, and the bitter, sweet, and umami tastes receptors are regulated by G-protein coupled receptor molecules with second messenger systems.[25] Hence, the exact mechanism and the dosage needed to cause clinical symptoms need to be elucidated in future studies.
Table 1.
The main literature of cardiovascular drugs caused smell and/or taste disorder.
Generally, smell and taste disturbance are not considered life-threatening side effects. They are often ignored by patients, families, and even medical staff. However, such disturbances can severely impair physical or mental health and eventually affect a patient's quality of life. Dysosmia and anosmia decrease the ability to detect natural gas, spoiled food, and smoke. It is noteworthy that a significant number of deaths caused by accidental gas poisonings were due to the inability to smell. Hypogeusia may reduce a patient's appetite and food intake, which leads to weight loss and even depression. Moreover, hypogeusia may lead to decrease compliance with drug regimens. Owing to lack of objective diagnostic standards and effective treatments, smell and taste disturbances caused by drugs might not be observed in a timely manner. This can result in irreversible nerve dysfunction and worse impact on the patient's quality of life.
In conclusion, the incidence of dysosmia or hypogeusia induced by cardiovascular drugs is rare. Here, we report on a patient who suffered from adverse events involving smell and taste following treatment with metoprolol and amiodarone. Considering the detrimental effects of dysosmia and dysgeusia with the long-term use of cardiovascular drugs, clinicians should not only be aware of the common side effects of the drug but also known rare side effects including smell and taste disorders. Besides, earlier detection would prevent irreversible damage to the patient and provide better drug compliance during their antiarrhythmic treatment.
Author contributions
Conceptualization: Cesar Reis.
Data curation: Yuandong Li, Yuanjian Fang.
Investigation: Huan Wang.
Project administration: Huan Wang.
Writing – original draft: Xiaoru Che.
Writing – review & editing: Yuandong Li, Yuanjian Fang.
Footnotes
Abbreviations: CNS = central nervous system, DCG = dynamic electrocardiogram, EEG = electrocardiograph.
The authors report no conflict of interest.
References
- [1].Suzuki M. [Beta-blocking agents]. Nihon Rinsho Jpn J Clin Med 1995;53:978–82. [PubMed] [Google Scholar]
- [2].Bodin NO, Borg KO, Johnansson R, et al. Tissue distribution of metoprolol-(3-h) in the mouse and the rat. Acta Pharmacol Toxicol (Copenh) 1975;36suppl 5:116–24. [DOI] [PubMed] [Google Scholar]
- [3].Maruyama T, Yasuda S, Odashiro K, et al. Anosmia induced by amiodarone. Am J Med 2007;120:e9. [DOI] [PubMed] [Google Scholar]
- [4].Van Cott TE, Yehle KS, DeCrane SK, et al. Amiodarone-induced pulmonary toxicity: case study with syndrome analysis. Heart Lung 2013;42:262–6. [DOI] [PubMed] [Google Scholar]
- [5].Vital Durand M. [Recurrent anosmia under beta-blockers]. Presse Med 1985;14:2064. [PubMed] [Google Scholar]
- [6].Vedin A. Ten years of clinical experience with metoprolol. J Cardiovasc Pharmacol 1987;10suppl 2:S80–5. [PubMed] [Google Scholar]
- [7].Morady F, Sauve MJ, Malone P, et al. Long-term efficacy and toxicity of high-dose amiodarone therapy for ventricular tachycardia or ventricular fibrillation. Am J Cardiol 1983;52:975–9. [DOI] [PubMed] [Google Scholar]
- [8].Heeringa M, van Puijenbroek EP. Reversible dysgeusia attributed to losartan. Ann Intern Med 1998;129:72. [DOI] [PubMed] [Google Scholar]
- [9].Levenson JL, Kennedy K. Dysosmia, dysgeusia, and nifedipine. Ann Intern Med 1985;102:135–6. [DOI] [PubMed] [Google Scholar]
- [10].Briggs ER. Taste disturbances related to medication use. Consult Pharm 2009;24:538–43. [DOI] [PubMed] [Google Scholar]
- [11].Tuccori M, Lapi F, Testi A, et al. Drug-induced taste and smell alterations: a case/non-case evaluation of an Italian database of spontaneous adverse drug reaction reporting. Drug Saf 2011;34:849–59. [DOI] [PubMed] [Google Scholar]
- [12].Ishimaru T, Yokogawa H. Olfactory and gustatory disturbances caused by digitalism: a case report. Auris Nasus Larynx 2006;33:465–9. [DOI] [PubMed] [Google Scholar]
- [13].Vlasses PH, Ferguson RK. Temporary ageusia related to captopril. Lancet 1979;2:526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Berman JL. Dysosmia, dysgeusia, and diltiazem. Ann Intern Med 1985;102:717. [DOI] [PubMed] [Google Scholar]
- [15].Warner MD, Peabody CA, Berger PA. Olfactory deficits and Down's syndrome. Biol Psychiatry 1988;23:836–9. [DOI] [PubMed] [Google Scholar]
- [16].Schlienger RG, Saxer M, Haefeli WE. Reversible ageusia associated with losartan. Lancet 1996;347:471–2. [DOI] [PubMed] [Google Scholar]
- [17].Ohkoshi N, Shoji S. Reversible ageusia induced by losartan: a case report. Eur J Neurol 2002;9:315. [DOI] [PubMed] [Google Scholar]
- [18].Castells X, Rodoreda I, Pedros C, et al. Drug points: dysgeusia and burning mouth syndrome by eprosartan. BMJ 2002;325:1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Kharoubi S. [Drug induced anosmia with nifedipine]. Presse Med 2003;32:1269–72. [PubMed] [Google Scholar]
- [20].Chen C, Chevrot D, Contamin C, et al. [Stomatitis and ageusia induced by candesartan]. Nephrologie 2004;25:97–9. [PubMed] [Google Scholar]
- [21].Sadasivam B, Jhaj R. Dysgeusia with amlodipine: a case report. Br J Clin Pharmacol 2007;63:253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Finn BC, Pellegrini D, Bruetman JE, et al. [Reversible dysgeusia attributed to losartan]. Medicina 2008;68:347–8. [PubMed] [Google Scholar]
- [23].Lulic I, Kovic I. [Can lacidipine cause smell disorders? A case report]. Lijec Vjesn 2011;133:98–100. [PubMed] [Google Scholar]
- [24].Henkin RI. Drug-induced taste and smell disorders. Incidence, mechanisms and management related primarily to treatment of sensory receptor dysfunction. Drug Saf 1994;11:318–77. [DOI] [PubMed] [Google Scholar]
- [25].Gilbertson TA, Margolskee RF, Doty RL. Molecular physiology of gustatory transduction. Handbook of Olfaction and Gustation 2003;703–730. [Google Scholar]


