Abstract
Objective
Sharing personal information about type 1 diabetes (T1D) can help adolescents obtain social support, enhance social learning, and improve self-care. Diabetes technologies, online communities, and health interventions increasingly feature data-sharing components. This study examines factors underlying adolescents’ willingness to share personal T1D information with peers.
Materials and Methods
Participants were 134 adolescents (12–17 years of age; 56% female) who completed an online survey regarding experiences helping others with T1D, perceived social resources, beliefs about the value of sharing information and helping others, and willingness to share T1D information. Hemoglobin A1c values were obtained from medical records.
Results
Adolescents were more willing to share how they accomplished T1D tasks than how often they completed them, and least willing to share glucose control status. In multivariate analyses, sharing/helping beliefs (β = 0.26, P < .01) and glucose control (HbA1c value; β = −0.26, P < .01) were related to greater willingness to share personal health information. Glucose control moderated relationships such that adolescents with worse A1c values had stronger relationships between sharing/helping beliefs and willingness to share (β = 0.18, P < .05) but weaker relationships between helping experience and willingness to share (β = −0.22, P = .07).
Discussion
Many adolescents with T1D are willing to share personal health information, particularly if they have better diabetes health status and a stronger belief in the benefits of sharing.
Conclusion
Social learning and social media components may improve intervention participation, engagement, and outcomes by boosting adolescents’ beliefs about the benefits of sharing information and helping others.
Keywords: adolescent, chronic disease, diabetes mellitus, type 1, data sharing, survey, social learning
INTRODUCTION
Adolescents with type 1 diabetes (T1D) often struggle to adhere to their complicated medical regimen of multiple daily blood glucose checks, carbohydrate intake counts, and accurate dosing and administration of insulin at appropriate times.1,2 Declines in adolescent adherence drives poorer rates of glycemic control during adolescence and early adulthood, as evidenced by higher hemoglobin A1c values.1,3 Inadequate glycemic control is related to serious long-term health consequences such as retinopathy, cardiovascular disease, and kidney disease, as well as short-term risks of hypoglycemia and diabetic ketoacidosis.3,4
Prior research has established social support as an important resource for adolescents with chronic illness,5,6 conceptualized in health literature as a multidimensional construct encompassing informational, emotional, psychosocial, and tangible resource dimensions.5,7 Increasingly, opportunities for social support are available to individuals with chronic illnesses through online and other digital contexts.8
In addition to receiving support from others, sharing one’s personal health information, including strategies, challenges, or data derived from self-care experiences, can be beneficial for building social support. Sharing information in order to help others with the same illness may reap greater benefits for the helper than the individuals receiving help (ie, the helper-therapy principle).9–11 Prior research indicates that helping others benefits helpers through favorable impacts on self-esteem and self-awareness, and a favorable shift in reference toward the illness and engagement in one’s own health.12–15 Self-determination theory points to an intrinsic need for competence and relatedness, both of which can be actualized through sharing and helping others.7,12–14,16 Interventions utilizing peer sharing of information about one’s own care and challenges have evidenced both physical and psychological benefits for adolescents with chronic conditions.17–20
Understanding motivations or reluctance to share personal health information is of growing interest to researchers, clinicians, and technology developers. New and emerging diabetes technologies increasingly allow users to share their data one-on-one or in broader social contexts.21 Online social networking sites (SNS) offer expanded social learning opportunities for individuals with chronic illness through social support, knowledge exchange, and data sharing. Despite potential benefits for social support and sharing and helping opportunities and diabetes self-care, a minority of adolescents with T1D (28%) report using SNS for diabetes.22 While health-focused interventions for youth increasingly incorporate social learning components, including social media features,19,22–24 it is not yet understood what factors are associated with adolescents’ willingness to share personal health information with peers. To overcome their reluctance to share, interventionists need to know which participants are less likely to share.
A large body of health communication research testing the theory of reasoned action has tied expectancy value beliefs (perceptions of favorable or unfavorable things that would result from a given behavior) through attitudes to individuals’ intentions and performance of a behavior.25,26 For example, adults in online professional communities were more likely to share personal knowledge if they believed knowledge sharing would benefit their peers in the community and/or themselves.27,28 Thus, we predicted that adolescents with T1D who have stronger beliefs in the value of sharing information and helping others would report a greater willingness to share personal health information with peers.
Critical to receiving encouragement, advice, and other forms of support is having access to social resources, or people with whom one can talk openly about diabetes-related care and challenges.5,29 Adolescents who do not have individuals with whom they feel they can share openly about diabetes may not be able to imagine comfortably sharing personal information about their diabetes at all. Conversely, having numerous people with whom to share openly could minimize an adolescent’s feelings of stigma related to talking about T1D and encourage information sharing.
In addition, helping another person with a diabetes problem could also encourage sharing personal health information. The experience of helping another with a diabetes problem could help an adolescent develop his or her sense of competence and relatedness among others with T1D,14,30 which in turn should encourage more information sharing in the future. Helping another with T1D could also boost willingness to share information with peers by enhancing the helper’s social self-efficacy and reducing apprehension about disclosing and discussing T1D information.31
There is some evidence to suggest that those with poorer health status feel greater vulnerability to judgment and greater pressure to maintain a positive impression by not sharing less than optimal personal health information.32,33 In 1 study, college students with poorer health status perceived health information as more sensitive and reported lower intention to disclose their own information on a health-oriented website.34 In this study, we hypothesized that adolescents with higher A1c values (worse diabetes health status) would be less willing to share personal health information with others compared to adolescents with lower A1c values (better diabetes health status).
There are several reasons to focus particular attention on individuals with higher A1c values. Given their likely greater reluctance to share personal health information in general, beliefs and experiences related to their willingness to share are of particular interest. Additionally, the fact that higher A1c values indicate worse health status means that these adolescents stand to benefit most from increased social support and data sharing. Thus, it is especially crucial to understand what beliefs and experiences might be related to willingness to share among adolescents with higher A1c values in order to gain insight into intervention techniques that could encourage their sharing in particular.
As such, we expected that A1c could moderate relationships with perceived social resources, helping experience, and sharing/helping beliefs such that these factors were more strongly related to willingness to share among adolescents with worse A1c values. Given their expected reluctance to share in general, adolescents with worse diabetes health status might only be willing to share information with others if they perceive strong value to themselves or others in doing so. Positive experiences helping other persons with diabetes could have particularly profound effects on adolescents who are struggling themselves as well, leading to a particularly high association between helping experience and willingness to share among these youth. Having greater perceived social resources might also be especially tied to an increased willingness to share personal health information among adolescents with worse health status, who are otherwise likely to feel particularly stigmatized.
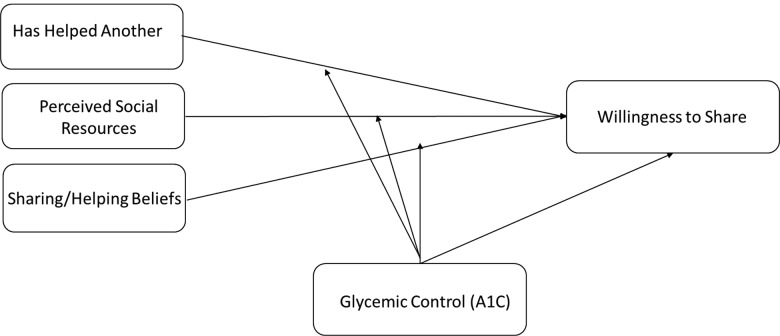
To our knowledge, this study provides the first examination of underlying beliefs and experiences that could help to explain willingness to share personal health information among adolescents with T1D. Analyses examine whether prior helping experience, beliefs about the value of sharing personal health information to help oneself and others, perceived social resources, and health status are linked to adolescents’ willingness to share health information with peers with T1D (see model in Figure 1 ). We take a novel approach to using the HbA1c test. Instead of using that variable as an outcome, as in most research, we conceptualize it as a predictor of willingness to share and as a moderator of helping experience, sharing/helping beliefs, and perceived social resources. Results will inform the design of interventions and technologies that promote social learning and data sharing, including those targeting improved self-care in youth with chronic illnesses such as T1D, and particularly those with worse diabetes health status.
Figure 1.
Proposed model of relationships.
METHODS
Sample and procedures
Recruitment took place within a large regional pediatric diabetes clinic in an academic medical center. Adolescents were eligible for the study if they had been diagnosed with T1D for at least 6 months, were between 13 and 17 years of age, had no cognitive or sensory impairments that would prevent completing a questionnaire, and had Internet access. Parents of all potentially eligible adolescents seen in the diabetes clinic were identified through medical records and initially contacted with a letter home inviting participation and providing a link to the online survey (n = 485). Of those, 166 (34.2%) completed the survey. Once a parent had completed online consent, the questionnaire URL was sent to the child in an e-mail or text message. Interested adolescents were then able to assent and complete the online questionnaire. (Parents completed a survey containing questions about their own use and perceptions of technology, in addition to questions regarding their children’s demographic and clinical characteristics. Some of those data have been reported elsewhere.22) The online survey system was closed once the study met recruitment goals. There were 134 dyads with complete data. Study data were collected using Research Electronic Data Capture.35 All study procedures and materials were approved by the Vanderbilt University Institutional Review Board prior to data collection.
Measures
Demographic and clinical characteristics. Parents reported their number of years of education, as well as the adolescents’ age, gender, and race/ethnicity, and clinical data such as diagnosis date and insulin pump use. Median household income was inferred using patient household zip code and data from the US Census American Community Survey.36
Glycemic control. Adolescents’ most recent A1c values (ie, collected at their last clinic appointment) were obtained from medical records. No A1c tests completed > 6 months prior to the study were included.
Helping experience. Participants responded yes or no to the following question: “Have you ever helped another person solve a diabetes problem or deal with a diabetes experience?”
Perceived social resources. Adolescents were asked: “How many people do you feel you can talk with openly about your diabetes?” Response options were ordinal and ranged from 0 (0 people) to 5 (>10 people).
Sharing and helping beliefs. Based on literature review and content expertise, 5 researcher-developed survey items were created to assess adolescents’ beliefs about the value of helping and sharing information related to T1D. These items were: (1) I know things that could help other people with diabetes; (2) If I had the chance, I would share my experiences with diabetes in order to help someone; (3) I believe people with diabetes can help each other with everyday challenges; (4) I believe a lot of teens with type 1 diabetes share the same challenges; and (5) I feel that I could learn from other teens that have type 1 diabetes. Each item had a response scale from 1 (strongly disagree) to 5 (strongly agree). Cronbach’s alpha for the scale was .86 in this sample.
Willingness to share T1D information. Adolescents indicated the types of information that they “would be willing to share with other teens” (binary response: not willing to share [0] or willing to share [1]). Four items pertained to how adolescents carry out self-care (eg, “how I carry supplies”), 4 pertained to information about how often T1D self-care behaviors were carried out (eg, “how often I count carbs”), and 2 asked about sharing specific objective health data related to glycemic control (blood glucose values, A1c values). The items to which adolescents responded affirmatively (ie, willing to share) were summed to create an index representing the extent of T1D information they were willing to share with other adolescents (KR-20 = 0.89). Scores could range from 0 to 10.
Statistical analyses
All analyses were conducted using SPSS v23 (IBM, Armonk, NY, USA). After examining univariate characteristics, correlations tested bivariate relationships between variables of interest. Figure 1 shows the hypothesized model. All demographic and clinical variables with an observed relationship with the dependent variable (willingness to share) were included as covariates in subsequent analyses. In a hierarchical linear regression, sharing/helping beliefs, helping experience, perceived social resources, and A1c values were entered as independent variables predicting scores on the willingness to share index. Next, 3 centered multiplicative terms representing the potential moderating relationships of interest (A1c with sharing/helping beliefs, helping experience, and perceived resources) were entered in the second step. The analysis was also run using bootstrap resampling procedures (1000 resamples with replacement) to derive coefficients with corresponding bias-corrected confidence intervals. Bootstrapping is a nonparametric procedure that allows estimation of test statistic distribution and can result in standard errors and confidence intervals that are more stable than conventional methods in small samples.37,38 Coefficient significance levels (P values) from the original nonbootstrapped analyses and unstandardized coefficient confidence intervals from the bootstrapped analyses are reported.
RESULTS
Sample characteristics
Means for demographic and clinical variables are in Table 1. The majority of participants were white (84.3%), which reflects the disproportionate burden of T1D among this racial group.3 The average age of respondents was 14.5 years, and 56.3% of respondents were female. Participants had been living with T1D for 5.5 years on average (SD = 3.6). This sample was very similar demographically and clinically to other samples of adolescents with T1D obtained within behavioral studies conducted at regional pediatric diabetes clinics.3,39–41
Table 1.
Descriptive statistics for demographic and clinical variables and study measures
| Respondent characteristics | Mean (SD) or % |
|---|---|
| Demographic/Clinical Variables | |
| Parent education (%) | |
| Less than high school | 2.2 |
| High school | 30.6 |
| 2-year college | 14.9 |
| 4-year college | 30.6 |
| Master’s | 18.7 |
| Doctoral or JD/MD | 3.0 |
| Household income (in thousands of dollars) | 60.6 (27.8) |
| Married (%) | 79.9 |
| Adolescent age | 14.52 (1.69) |
| Adolescent gender (% male) | 43.7 |
| Adolescent race (%) | |
| White | 84.3 |
| African American | 10.4 |
| Asian/Pac islander | 1.5 |
| Adolescent is Hispanic (%) | 5.2 |
| Duration of diabetes (in years) | 5.47 (3.59) |
| Use insulin pump (% yes) | 57.5 |
| Willingness to share index | 6.41 (3.63) |
| Has helped another (% yes) | 53.0 |
| Perceived social resourcesa | 3.66 (1.48) |
| Sharing/helping beliefsb | 3.92(0.78) |
| A1c | 8.63 (1.78) |
N = 134. a6 ordinal categories from 0 (0 people) to 5 (>10). b5-point scale from 1 (strongly disagree) to 5 (strongly agree).
Descriptive and bivariate statistics
Table 1 contains results of univariate analyses. On average, adolescents were willing to share 6.4 (SD = 3.63) forms of personal health information with peers, out of 10 queried. As shown in Table 2, they were generally willing to share more information about how they complete T1D tasks than how often they complete tasks or their T1D control status. The bivariate correlations presented in Table 3 indicate small or moderate bivariate relationships among the variables of interest, and few bivariate associations with demographic and additional clinical factors. One clinical variable (in addition to A1c) was significantly related to willingness to share: adolescents who used an insulin pump reported slightly higher willingness to share personal health information (rpb = 0.17, P < .05). This variable was included in subsequent models as a covariate.
Table 2.
Distributions of individual willingness to share index items
| Type of information | Percent willing to share (n) |
|---|---|
| How | |
| How I carry supplies | 74.6 (100) |
| How I count carbs | 73.9 (99) |
| How I dose insulin | 69.4 (93) |
| How I put exercise, carbs, and meter information together | 54.4 (73) |
| How often | |
| How often I carry fast sugar | 58.2 (78) |
| How often I count carbs | 53.7 (72) |
| How often I check my blood glucose (BG) | 64.2 (86) |
| How often I use my BG to guide my insulin dose | 50.7 (68) |
| Control | |
| My BG values | 52.2 (70) |
| My A1c values | 41.8 (56) |
| Total index, mean (SD) | 5.9 (3.4) |
N = 134.
Table 3.
Zero-order correlations
| Study variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Willingness to share index | – | – | – | – | – | – | – | – | –– | – |
| 2. Sharing and helping beliefs | .32*** | – | – | – | – | – | – | – | – | – |
| 3. Has helped anothera | .16 | .42*** | – | – | – | – | – | – | – | – |
| 4. Perceived social resources | .19* | .25** | .29** | – | – | – | – | – | – | – |
| 5. A1c | −.31*** | −.22** | −.06 | −.13 | – | – | – | – | – | – |
| 6. Age | −.10 | −.08 | .10 | .03 | .17 | – | – | – | – | – |
| 7. Duration of diabetes | −.07 | .12 | .18* | −.05 | .19* | .42*** | – | – | – | – |
| 8. Pump usera | .17* | .14 | .31*** | .26** | −.05 | −.10 | .14 | – | – | – |
| 9. Household income | .02 | −.03 | −.03 | .06 | −.20* | .05 | .01 | .14 | – | – |
| 10. White/not Hispanica | .12 | .14 | .07 | .21* | −.25** | −.21* | .05 | .19* | .20* | – |
| 11. Femalea | .01 | .14 | .05 | .06 | −.12 | .05 | −.07 | .002 | .06 | −.003 |
N = 134. aValues represent point-biserial correlations (all other values are Spearman correlations). ***P < .001; **P < .01; *P < .05.
Predictors of willingness to share personal health information
The first step of the hierarchical regression analysis contained the 4 independent variables (sharing/helping beliefs, helping experience, perceived social resources, and A1c), as well as pump use as a covariate. Collinearity diagnostics indicated sufficiently low multicollinearity in the model (lowest tolerance value = .77; highest VIF value = 1.30).42 Standardized and unstandardized coefficients are presented in Table 4. The first step of the model was significant (F [5,133] = 5.99, P < .001) and indicated that sharing/helping beliefs and lower A1c were significantly related to greater willingness to share.
Table 4.
Predictors of adolescents’ willingness to share diabetes information
| Study variables | Step 1 |
Step 2 |
||||
|---|---|---|---|---|---|---|
| B (CI B)a | Beta | P valueb | B (CI B)a | Beta | P valueb | |
| Pump user | 0.58 (−.78, 9.50) | 0.09 | .32 | 0.67 (−.46, 1.73) | 0.10 | .24 |
| Perceived social resources | 0.19 (−.20, .59) | 0.08 | .34 | 0.21 (−.20, .62) | 0.09 | .28 |
| Has helped another | −0.01 (−1.30, 1.31) | −0.001 | .99 | −0.06 (−1.39,1.16) | −0.01 | .93 |
| Sharing/helping beliefs | 1.14 (.18, 2.14) | 0.26** | .003 | 1.07 (.26, 1.99) | 0.24** | .004 |
| A1c (medical record) | −0.46 (−.75, −.16) | −0.26** | .002 | −0.18 (−.51, .24) | −0.10 | .39 |
| A1c × social resources | −0.19 (−.37, .03) | −0.15
|
.06 | |||
| A1c × helped | −0.53 (−1.10, −.07) | −0.22* | .07 | |||
| A1c × sharing/helping beliefs | 0.57 (0.09, 1.09) | 0.18* | .02 | |||
| Adj. R2 | 0.16 | 0.21 | ||||
N = 134. ***P < .001, **P < .01, *P < .05,  P < .10. aValues represent coefficient confidence intervals obtained from bootstrapping 1000 subsamples with replacement. bValues represent coefficient significance estimates (P values) from nonbootstrapped model.
P < .10. aValues represent coefficient confidence intervals obtained from bootstrapping 1000 subsamples with replacement. bValues represent coefficient significance estimates (P values) from nonbootstrapped model.
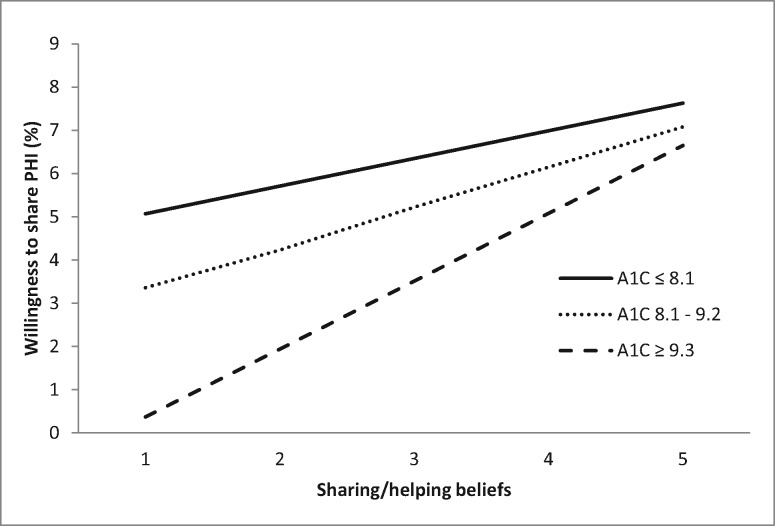
Moderation. The second model step introduced the 3 multiplicative interaction terms between A1c and (1) sharing/helping beliefs, (2) helping experience, and (3) perceived social resources. Results indicated that A1c moderated the relationships between willingness to share and sharing/helping beliefs (B = .57, CI [0.09, 1.09]) (nonbootstrapped P = .02) and helping experience (B = −.53, CI [−1.10, −0.07]) (nonbootstrapped P = .07). Results suggest a marginally significant interaction for perceived social resources (B = −.19, CI [−0.37, 0.03]) (nonbootstrapped P = .06). In order to clarify the relationships, tertiary cutpoints for A1c values were created based on the A1c distribution in this sample (low A1c:≤8.1 [n = 45]; moderate A1c: 8.2–9.2 [n = 45]; high A1c: ≥9.3 [n = 44]). (These points were also consistent with ranges found in national surveys of adolescents with T1D.43,44) As shown in Figure 2 , sharing/helping beliefs among adolescents with high A1c values were particularly related to willingness to share information about T1D compared to those with moderate or low A1C values.
Figure 2.
Adolescent A1c value moderates relationship between sharing/helping beliefs and willingness to share T1D information.
Conversely, having helped another was most related to willingness to share personal health information among adolescents with low and moderate A1c values. Among participants with the lowest A1c values (≤8.1), those who had helped another with T1D were willing to share 7.84 pieces of health information on average, compared to an average of 6.11 among those who had no experience helping another (P < .001). Adolescents with moderate A1c values (8.2–9.2) who had helped were willing to share 6.53 pieces of information on average, while those who had not helped another were willing to share 5.56 pieces (P < .001). Participants with the highest A1cs (≥9.3) did not differ in the amount of health information they would share based on whether they had helped another (M = 4.64) or not (M = 4.58, P = .91).
DISCUSSION
In this study, adolescents’ diabetes health status and beliefs about the value of sharing and helping were related to their willingness to share personal health information with peers. In general, adolescents in this study reported fairly high willingness to share personal health information with others who have T1D (ie, about 6 types of information out of a possible 10). Participants were particularly receptive to sharing information about how they complete diabetes tasks (eg, how they count carbs), and least willing to share potentially sensitive health status information such as blood glucose or A1c value. Prior literature indicates relatively low use of social media technologies to share information and gain social support among adolescents with chronic illness.22,24 The present findings highlight a mismatch between adolescents’ low reported use of SNS for diabetes and the extent of personal health information that many would be willing to share with peers. These findings suggest that the low rates of social media use do not reflect an inherent unwillingness to share some kinds of personal health information among adolescents with chronic illness, such as T1D; rather, adolescents may not be encountering technologies or sharing contexts that fit their needs.
As predicted, adolescents with poorer glycemic control (higher A1c values) were less willing to share information with others with T1D than their peers with lower A1c values. Similarly, Weitzman and colleagues33 found that patients with lower A1c values used less restrictive share settings and shared their A1c values more frequently than their peers in a diabetes-specific online community. It may be that adolescents with higher A1c values (worse diabetes health status) feel they have less useful information for helping others, or that they anticipate stigmatization based on their data. Those who consider posting health-related information online face a tension between pursuing health-related goals, such as obtaining advice or emotional support, and maintaining a favorable impression as someone who is healthy and competent.32 It seems the balance may shift in favor of the latter among adolescents who are struggling with glycemic control.
On the other hand, adolescents who believed more strongly that sharing information and helping others was valuable were more willing to share personal health information in the current study. As predicted, this relationship was especially strong among adolescents with poorer health status. One possibility is that perceiving value in sharing personal health information, for oneself or for others, may counter the reluctance to share information that many adolescents with poorer glycemic control feel. Prior findings indicate that sharing personal health information can benefit individuals with chronic illness, and that social networking offers unique opportunities to provide and receive support.7,12,19 These data suggest that it may be especially important to boost positive perceptions of the value of sharing and helping behaviors among adolescents struggling with glycemic control in order to encourage them to share information with peers. Similarly, getting adolescents to share information may boost their sense of the value of such behavior.
While A1c also moderated relationships between willingness to share and helping experience, the nature of the interaction was unexpected. The experience of helping another person deal with a diabetes-related problem was associated with greater willingness to share, particularly among adolescents with better health status (lower A1c values). It is not clear why the experience of helping another with a diabetes problem is not related to greater willingness to share information among those with higher A1c values. It may be that the quality or nature of the experience of helping others is relatively more important for those with poorer health status, or that different forms of helping are differentially related to willingness to engage in future sharing behavior. On the other hand, helping another person may feel particularly rewarding to an adolescent with better health status, leading to greater feelings of competence or relatedness. Moreover, adolescents in better glycemic control may in fact be more competent with their diabetes care, and thus their advice may be more successful. Additional research is needed to identify particularly effective forms of helping behaviors and peer interactions among adolescents with chronic illness.
Counter to expectations, having more perceived social resources was not significantly related to willingness to share among adolescents in this study. While an adolescent who is struggling might have access to multiple individuals they trust, he or she may not have interacted with or viewed those individuals as social resources.45 Similarly, adolescents’ willingness to share may influence how they evaluate sources of support in their lives. The actual experience of sharing information may be critical for developing positive sharing and helping beliefs and building confidence in one’s own value in helping others. Particular social referents with whom an adolescent can speak about diabetes issues (eg, peers with or without diabetes) may also play differential roles or have varying influence.45 These relationships should be explored in future research.
Additional clinical characteristics and demographic factors largely did not distinguish between adolescents who were more or less willing to share personal health information. Use of an insulin pump had a small positive correlation with greater willingness to share in bivariate relationships, although this relationship did not persist in multivariate analyses. It is possible that wearing an insulin pump may be more readily visible to others compared to administering insulin injections, thereby creating a greater possibility for discussion of diabetes with peers. Recent developments in diabetes technologies have led to insulin pump devices that enable data sharing.21 Of interest is whether a substantial portion of adolescents who use pumps have had more experiences sharing their personal health data through these technologies compared to peers who use insulin injections.
LIMITATIONS
Study findings should be interpreted with several limitations in mind. Because data were cross-sectional, it is not possible to confirm the temporal order of relationships or causality. In fact, we anticipate that many of these relationships are reciprocal in nature (eg, sharing and helping beliefs and information sharing and other helping experiences may be mutually reinforcing). Moreover, it is possible that unmeasured cognitions or behaviors could account for relationships uncovered here. Little prior research has been conducted in this area, and standardized measures were not available for variables of interest. In addition, the measures were not specific to online or offline contexts and did not include additional constructs that could feasibly impact adolescents’ willingness to share (eg, personality dimensions or sharing-related trust).34
CONCLUSIONS
These findings can inform youth-focused health interventions with social learning and social media components; boosting adolescents’ beliefs about the value of sharing information to help oneself and others may be a necessary first step. Targeting those efforts toward adolescents who have poor health status may be especially fruitful. Interventions that target youth with chronic illnesses like T1D and employ online or offline social learning components may be more successful if preemptive efforts are made to enhance adolescents’ beliefs that sharing information is valuable to helping others and oneself. Additionally, offering opportunities to help others could be fruitful in encouraging sharing among adolescents with better health status. Future research should examine whether vicarious learning experiences, such as viewing stories in which other adolescents model T1D sharing and helping behaviors, could initiate interest and self-efficacy associated with sharing and helping others and boost sharing/helping beliefs.46
Funding
This research was funded by grants from the National Institutes of Health (grant number DP3 DK097706) and Vanderbilt University’s Clinical and Translational Science Award (grant number UL1TR000445).
Contributors
SV: conceptualization, statistical analyses, results preparation, drafting and editing of manuscript. JL: conceptualization, measurement critique and review, analyses conceptualization and review, results interpretation, drafting and editing of manuscript. KH: funding, conceptualization, measurement selection and development, results interpretation, drafting and editing of manuscript. SM: funding, conceptualization, measurement selection and development, online survey design supervision, implementation and data acquisition oversight, results interpretation, drafting and editing of manuscript. All authors approved of the final manuscript and agree to be accountable for the integrity and accuracy of the work submitted.
Competing Interests
The authors have no competing interests to declare.
ACKNOWLEDGMENTS
We would like to thank Dr Mary S. Dietrich for her statistical consultation on this project.
References
- 1. Hood KK, Peterson CM, Rohan JM, et al. . Association between adherence and glycemic control in pediatric type 1 diabetes: a meta-analysis. Pediatrics. 2009;124:e1171–79. [DOI] [PubMed] [Google Scholar]
- 2. Wood JR, Miller KM, Maahs DM, et al. . Most youth with type 1 diabetes in the T1D Exchange Clinic Registry do not meet American Diabetes Association or International Society for Pediatric and Adolescent Diabetes clinical guidelines. Diabetes Care. 2013;36:2035–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Miller KM, Foster NC, Beck RW, et al. . Current state of type 1 diabetes treatment in the US: updated data from the T1D Exchange clinic registry. Diabetes Care. 2015;38:971–78. [DOI] [PubMed] [Google Scholar]
- 4. Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;1993:977–86. [DOI] [PubMed] [Google Scholar]
- 5. La Greca AM, Auslander WF, Greco P, et al. . I get by with a little help from my family and friends: Adolescents’ support for diabetes care. J Pediatr Psychol. 1995;20:449–76. [DOI] [PubMed] [Google Scholar]
- 6. La Greca AM, Bearman KJ, Moore H. Peer relations of youth with pediatric conditions and health risks: promoting social support and healthy lifestyles. J Dev Behav Pediatr. 2002;23:271–80. [DOI] [PubMed] [Google Scholar]
- 7. Hether HJ, Murphy ST, Valente TW. It’s better to give than to receive: The role of social support, trust, and participation on health-related social networking sites. J Health Commun. 2014;19:1424–39. [DOI] [PubMed] [Google Scholar]
- 8. Zhang S, Bantum EO, Owen J, et al. . Online cancer communities as informatics intervention for social support: conceptualization, characterization, and impact. J Am Med Inform Assoc. 2017;242:451–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Riessman F. The “helper” therapy principle. Soc Work. 1965;102:27–32. [Google Scholar]
- 10. Wicks P, Massagli M, Frost J, et al. . Sharing health data for better outcomes on PatientsLikeMe. J Med Internet Res. 2010;12:e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Heisler M. Different models to mobilize peer support to improve diabetes self-management and clinical outcomes: evidence, logistics, evaluation considerations and needs for future research. Fam Pract. 2009;27(suppl 1):cmp003. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 12. Rini C, Austin J, Wu LM, et al. . Harnessing benefits of helping others: a randomized controlled trial testing expressive helping to address survivorship problems after hematopoietic stem cell transplant. Health Psychol. 2014;33:1541. [DOI] [PubMed] [Google Scholar]
- 13. Proudfoot JG, Jayawant A, Whitton AE, et al. . Mechanisms underpinning effective peer support: a qualitative analysis of interactions between expert peers and patients newly-diagnosed with bipolar disorder. BMC Psychiatry. 2012;12:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Schwartz CE, Sendor RM. Helping others helps oneself: response shift effects in peer support. Soc Sci Med. 1999;48:1563–75. [DOI] [PubMed] [Google Scholar]
- 15. Solomon P. Peer support/peer provided services underlying processes, benefits, and critical ingredients. Psychiatr Rehabil J. 2004;27:392. [DOI] [PubMed] [Google Scholar]
- 16. Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55:68. [DOI] [PubMed] [Google Scholar]
- 17. Barak A, Dolev-Cohen M. Does activity level in online support groups for distressed adolescents determine emotional relief? Couns Psychother Res. 2006;6:186–90. [Google Scholar]
- 18. Barnfather A, Stewart M, Magill-Evans J, et al. . Computer-mediated support for adolescents with cerebral palsy or spina bifida. Comput Inform Nurs. 2011;29:24–33. [DOI] [PubMed] [Google Scholar]
- 19. Nicholas DB, Fellner KD, Frank M, et al. . Evaluation of an online education and support intervention for adolescents with diabetes. Soc Work Health Care. 2012;51:815–27. [DOI] [PubMed] [Google Scholar]
- 20. Treadgold CL, Kuperberg A. Been there, done that, wrote the blog: the choices and challenges of supporting adolescents and young adults with cancer. J Clin Oncol. 2010;28:4842–49. [DOI] [PubMed] [Google Scholar]
- 21. Wahowiak L. The Psychology of Data Sharing. Diabetes Forecast 2016. http://www.diabetesforecast.org/2016/jul-aug/data-sharing-ii.html?referrer=https://www.google.com/. Accessed September 16, 2016. [Google Scholar]
- 22. Vaala SE, Hood KK, Laffel L, et al. . Use of commonly available technologies for diabetes information and self-management among adolescents with type 1 diabetes and their parents: a web-based survey study. Interact J Med Res. 2015;4:e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ho Y-X, O’Connor BH, Mulvaney SA. Features of online health communities for adolescents with type 1 diabetes. West J Nurs Res. 2014;36:1183–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Van Der Velden M, El Emam K. “Not all my friends need to know”: a qualitative study of teenage patients, privacy, and social media. J Am Med Inform Assoc. 2013;20:16–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Albarracin D, Johnson BT, Fishbein M, et al. . Theories of reasoned action and planned behavior as models of condom use: a meta-analysis. Psychol Bull. 2001;127:142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Fishbein M. A reasoned action approach to health promotion. Med Decis Making. 2008;28:834–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wang S, Noe RA. Knowledge sharing: A review and directions for future research. Hum Resour Manag Rev. 2010;20:115–31. [Google Scholar]
- 28. Wasko MM, Faraj S. “It is what one does”: why people participate and help others in electronic communities of practice. J Strateg Inf Syst. 2000;9:155–73. [Google Scholar]
- 29. Kyngäs H. Support network of adolescents with chronic disease: adolescents’ perspective. Nurs Health Sci. 2004;6:287–93. [DOI] [PubMed] [Google Scholar]
- 30. Weinstein N, Ryan RM. When helping helps: autonomous motivation for prosocial behavior and its influence on well-being for the helper and recipient. J Pers Soc Psychol. 2010;98:222. [DOI] [PubMed] [Google Scholar]
- 31. Alessandri G, Caprara GV, Eisenberg N, et al. . Reciprocal relations among self-efficacy beliefs and prosociality across time. J Pers. 2009;77:1229–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Newman MW, Lauterbach D, Munson SA, et al. . It’s not that I don’t have problems, I’m just not putting them on facebook: challenges and opportunities in using online social networks for health. In: Proceedings of the ACM 2011 Conference on Computer Supported Cooperative Work. ACM; 2011. [Google Scholar]
- 33. Weitzman ER, Adida B, Kelemen S, et al. . Sharing data for public health research by members of an international online diabetes social network. PloS One. 2011;6:e19256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bansal G, Gefen D. The impact of personal dispositions on information sensitivity, privacy concern and trust in disclosing health information online. Decis Support Syst. 2010;49:138–50. [Google Scholar]
- 35. Harris PA, Taylor R, Thielke R, et al. . Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. US Census Bureau. American Community Survey 2013. Washington, DC:US Department of Commerce; 2014. https://www.census.gov/programs-surveys/acs/. Accessed January 13, 2014.
- 37. Gonçalves S, White H. Bootstrap standard error estimates for linear regression. J Am Stat Assoc. 2005;100:970–79. [Google Scholar]
- 38. Walters SJ, Campbell MJ. The use of bootstrap methods for analysing health-related quality of life outcomes (particularly the SF-36). Health Qual Life Outcomes. 2004;2:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Valenzuela JM, Seid M, Waitzfelder B, et al. . Prevalence of and disparities in barriers to care experienced by youth with type 1 diabetes. J Pediatr. 2014;164:1369–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Wong JC, Dolan LM, Yang TT, et al. . Insulin pump use and glycemic control in adolescents with type 1 diabetes: predictors of change in method of insulin delivery across two years. Pediatr Diabetes. 2015;16:592–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wysocki T, Lochrie A, Antal H, et al. . Youth and parent knowledge and communication about major complications of type 1 diabetes. Diabetes Care. 2011;34:1701–05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. O’Brien RM. A caution regarding rules of thumb for variance inflation factors. Qual Quant. 2007;41:673–90. [Google Scholar]
- 43. Carlsen S, Skrivarhaug T, Thue G, et al. . Glycemic control and complications in patients with type 1 diabetes–a registry-based longitudinal study of adolescents and young adults. Pediatr Diabetes. 2016;183:188–95. [DOI] [PubMed] [Google Scholar]
- 44. Clements MA, Foster NC, Maahs DM, et al. . Hemoglobin A1c (HbA1c) changes over time among adolescent and young adult participants in the T1D exchange clinic registry. Pediatr Diabetes. 2015;175:327–36. [DOI] [PubMed] [Google Scholar]
- 45. Rini C, Symes Y, Campo RA, et al. . I keep my problems to myself: negative social network orientation, social resources, and health-related quality of life in cancer survivors. Ann Behav Med. 2016;50:385–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Bandura A. Social cognitive theory of mass communication. Media Psychol. 2001;3:265–99. [Google Scholar]