Abstract
Background
The proportion of racial/ethnic minorities receiving ventricular assist devices (VAD) has previously been less than expected. It is unclear if trends have changed since the broadening of access to insurance in 2014 and the rapid adoption of VAD technology.
Methods and Results
Using the Interagency Registry of Mechanically Assisted Circulatory Support, we analyzed time trends by race/ethnicity for 10,795 patients (Caucasian 67.4%, African-American 24.8%, Hispanic 6.3%, Asian 1.5%) who had a VAD implanted between 2012–2015. Linear models were fit to the annual census-adjusted rate of VAD implantation for each racial/ethnic group, stratified by sex and age group. From 2012–2015, African-Americans had an increase in the census-adjusted annual rate of VAD implantation per 100,000 [0.26(95% Confidence Interval 0.17–0.34)], while other ethnic groups exhibited no significant changes [Caucasian: 0.06(−0.03–0.14); Hispanic: 0.04(−0.05–0.12); Asian: 0.04(−0.04–0.13)]. Stratified by sex, rates increased in both African-American men and women (p<0.05), but the change in rate was highest among African-American men [men 0.37 (0.28–0.46); women 0.16 (0.07–0.25), interaction with sex p=0.004]. Stratified by age group, rates increased in African-Americans aged 40–69 and Asians aged 50–59 years (p<0.05). The observed differential change in VAD implantation rate by age group was significant among African-Americans (interaction with age p<0.01) and Asians (interaction with age p=0.02).
Conclusions
From 2012–2015, VAD implantation rates increased among African-Americans, but not other racial/ethnic groups. The greatest increase in rate was observed among middle-aged African-American men, suggesting a decline in racial disparities. Further investigation is warranted to reduce disparities among women and older racial/ethnic minorities.
Keywords: disparities, heart failure, age, women’s health
Heart failure disproportionately affects racial/ethnic minorities, particularly African-Americans.1 Among patients with advanced heart failure, ventricular assist devices (VAD) extend life expectancy and improve quality of life.2 However, historically racial/ethnic minorities received less than 1/3 of VADs in the U.S.3 despite representing 40% of all heart failure hospitalizations and having similar rates of survival compared to Caucasians post VAD.4,5 The distribution declines further among African-American women, who have the highest prevalence of heart failure compared to all other racial/ethnic groups and sexes.1
African-Americans and Hispanics are at higher risk for developing heart failure at young ages.1 African-Americans have two to three-fold higher rates of heart failure compared to Caucasians before the age of 75.1 Historically, half of all VADs are implanted in patients aged 60 to 79 years. It is unclear if racial/ethnic disparities are present across age groups.3
The factors that contribute to disparate racial/ethnic distribution are complex but may be accounted for by the higher proportion of underinsured racial/ethnic minorities.6 Insurance is a prerequisite for VAD implantation.7 The broadening of public insurance has been associated with reduced racial disparities in heart transplant listings6 and may expand to VADs. In addition, there has been a rapid rise in VAD implantations nationwide8 and increased public awareness of this technology.9 It is unclear if racial/ethnic disparities have changed. Using the Interagency Registry of Mechanically Assisted Circulatory Support (INTERMACS) registry and U.S. Census, we sought to evaluate racial/ethnic per capita trends in receipt of VADs by sex and age. We hypothesized that temporal changes in the census-adjusted rate of receipt of VADs would be higher for racial/ethnic minorities than Caucasians, independent of sex and age.
METHODS
Data Source
The INTERMACS registry collects quarterly data on patients receiving mechanically assisted devices for heart failure.10 Prior to 2014, the Centers for Medicare and Medicaid Services (CMS) required all implanting centers to participate in INTERMACS.11 Since that time, the number of centers participating in INTERMACS has increased.10 Participating centers are incentivized through receipt of individualized outcomes and quality of care data. Each center obtains informed consent from individual patients and institutional review board approval. In order to maintain good standing within INTERMACS, centers must provide complete data at regular intervals, including demographics and comorbidities.10 Race/ethnicity are reported by individual centers. Insurance data is not recorded but required for implantation. Researchers are blinded to center name and location. The National Heart, Lung, and Blood Institute provide oversight to data collection. This study was approved by the INTERMACS Data Access, Analysis, and Publications Committee. The data, analytic methods, and study materials are available to other researchers for the purposes of reproducing the results or replicating the procedure upon approval of application to the INTERMACS Data Access, Analysis, and Publications Committee.
Study Cohort
Inclusion criteria comprised adults aged 18 years or older who received a VAD at a participating INTERMACS registry center from 2012 to 2015. Patients with a listed race of African-American, Asian, or Caucasian or ethnicity of Hispanic were included. Patients were characterized as Non-Hispanic Caucasian (Caucasian), Non-Hispanic African-American (African-American), Hispanic, and Non-Hispanic Asian (Asian). Other races were excluded due to low representation (n=517). The final cohort included 10,795 patients.
Outcomes of Interest
The primary outcome was the annual census-adjusted rate of VAD implantation. The number of patients living with advanced heart failure in the U.S. is unknown and could not be used in the rate denominator. Given variation in racial/ethnic U.S. population by time, the annual projected U.S. Census Bureau Estimates for 2012 to 2015 were used in the rate denominator according to race/ethnicity, sex, and age group. This method has been established for demonstrating racial/ethnic differences in rate of receipt of advanced therapies elsewhere.6
Statistical Analysis
Patient characteristics were compared by race/ethnicity using chi-squared tests for categorical variables and Kuskal-Wallace tests for continuous variables. Linear models were fit to the annual census-adjusted rate of VAD implantation in order to assess racial/ethnic trends by time. Monthly implantation dates were not available. From 2012 to 2015, the rate of change in VAD implantation was performed within each racial/ethnic group and stratified by sex and age group. Analyses were performed using SAS, version 9.4 (SAS Institute, Inc., Cary, North Carolina) and R statistical software (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
Patient Characteristics
From 2012 to 2015, 10,795 patients (Caucasian 67.4%, African-American 24.8%, Hispanic 6.3%, Asian 1.5%) received a VAD implantation (Table 1). Among each racial/ethnic group, women received less than a third of VADs. Over half of all patients were aged 50–69 years. Across all racial/ethnic groups, over 90% of patients received a Left VAD. Destination VAD was a more common strategy in Caucasians (45.2%) and African-Americans (44.1%) than Hispanics (37.9%) and Asians (30.5%). More Caucasians were implanted at lower INTERMACS profiles 4–7 than racial/ethnic minorities (Profile 4–7: Caucasians 18.9%, African-Americans 10.8%, Hispanics 12.9%, Asian 8.5%). Caucasians had more pulmonary disease or active smoking, more African-Americans had obesity or history of prior drug use, more Hispanics had severe diabetes, fewer African-Americans had prior cardiac surgery, and fewer Hispanics had a history of smoking.
Table 1.
Patient Characteristics from 2012–2015
| Caucasian N=7,272 |
African-American N=2,676 |
Hispanic N=683 |
Asian N=164 |
|||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| N | (%) | N | (%) | N | (%) | N | (%) | |
| Sex* | ||||||||
| Women | 1299 | (17.9) | 831 | (31.1) | 151 | (22.1) | 29 | (17.7) |
| Age* | ||||||||
| 20–39 | 617 | (8.5) | 498 | (18.6) | 122 | (17.9) | 31 | (18.9) |
| 40–49 | 784 | (10.8) | 584 | (21.8) | 102 | (14.9) | 23 | (14.0) |
| 50–59 | 1930 | (26.5) | 822 | (30.7) | 179 | (26.2) | 49 | (29.9) |
| 60–69 | 2665 | (36.6) | 624 | (23.3) | 214 | (31.3) | 43 | (26.2) |
| 70+ | 1276 | (17.5) | 148 | (5.5) | 66 | (9.7) | 18 | (11.0) |
| Primary Diagnosis*† | ||||||||
| CAD | 434 | (6.0) | 52 | (1.9) | 40 | (5.9) | 14 | (8.5) |
| Dilated | 6466 | (88.9) | 2506 | (93.6) | 609 | (89.2) | 142 | (86.6) |
| Hypertrophic | 69 | (0.9) | 11 | (0.4) | 7 | (1.0) | 3 | (1.8) |
| Restrictive | 91 | (1.3) | 49 | (1.8) | 8 | (1.2) | 0 | (0.0) |
| Valvular | 86 | (1.2) | 13 | (0.5) | 6 | (0.9) | 3 | (1.8) |
| Congenital | 50 | (0.7) | 9 | (0.3) | 6 | (0.9) | 0 | (0.0) |
| Other | 76 | (1.0) | 36 | (1.3) | 7 | (1.0) | 2 | (1.2) |
| Device Strategy* | ||||||||
| BTT | 3885 | (53.4) | 1468 | (54.9) | 412 | (60.3) | 113 | (68.9) |
| Destination | 3287 | (45.2) | 1179 | (44.1) | 259 | (37.9) | 50 | (30.5) |
| Other | 100 | (1.4) | 29 | (1.1) | 12 | (1.8) | 1 | (0.6) |
| Device Type*† | ||||||||
| LVAD | 6815 | (93.7) | 2513 | (93.9) | 621 | (90.9) | 148 | (90.2) |
| RVAD | 15 | (0.2) | 1 | (0.0) | 0 | (0.0) | 1 | (0.6) |
| Both | 283 | (3.9) | 111 | (4.1) | 36 | (5.3) | 11 | (6.7) |
| TAH | 159 | (2.2) | 51 | (1.9) | 26 | (3.8) | 4 | (2.4) |
| INTERMACS Profile* | ||||||||
| 1 | 1252 | (17.2) | 387 | (14.5) | 145 | (21.2) | 38 | (23.2) |
| 2 | 2408 | (33.1) | 1011 | (37.8) | 249 | (36.5) | 63 | (38.4) |
| 3 | 2179 | (30.0) | 968 | (36.2) | 197 | (28.8) | 46 | (28.0) |
| 4–7 | 1371 | (18.9) | 290 | (10.8) | 88 | (12.9) | 14 | (8.5) |
| Unknown | 62 | (0.9) | 20 | (0.7) | 4 | (0.6) | 3 | (1.8) |
| VAD Center Volume* | ||||||||
| 1–10 | 481 | (6.6) | 173 | (6.5) | 40 | (5.9) | 8 | (4.9) |
| 11–30 | 2154 | (29.6) | 834 | (31.1) | 246 | (36.0) | 78 | (47.6) |
| 31–50 | 2712 | (37.3) | 1014 | (37.9) | 246 | (36.0) | 44 | (26.8) |
| > 50 | 1895 | (26.1) | 638 | (23.8) | 148 | (21.7) | 34 | (20.7) |
| Unknown | 30 | (0.4) | 17 | (0.6) | 3 | (0.4) | 0 | (0.0) |
| Prior cardiac surgery* | 2888 | (39.7) | 525 | (19.6) | 229 | (33.5) | 61 | (37.2) |
| Prior congenital cardiac surgery*‡ | 47 | (0.6) | 6 | (0.2) | 5 | (0.7) | 0 | (0.0) |
| Cancer‡ | 50 | (0.7) | 22 | (0.8) | 1 | (0.1) | 1 | (0.6) |
| Pulmonary Disease* | 702 | (9.7) | 208 | (7.8) | 31 | (4.5) | 9 | (5.5) |
| Severe Diabetes* | 644 | (8.9) | 178 | (6.7) | 79 | (11.6) | 15 | (9.1) |
| Intravenous Inotropes* | 5713 | (78.6) | 2312 | (86.4) | 555 | (81.3) | 135 | (82.3) |
| BMI ≥ 30* | 933 | (12.8) | 501 | (18.7) | 95 | (13.9) | 10 | (6.1) |
| KCCQ12, Median (IQR)* | 30.7 | (18.1, 45.8) | 32.3 | (19.3, 52.1) | 27.1 | (13.5, 43.7) | 36.1 | (17.2, 56.3) |
| History of smoking* | 2059 | (28.3) | 663 | (24.8) | 131 | (19.2) | 37 | (22.6) |
| Current smoking* | 361 | (5.0) | 100 | (3.7) | 12 | (1.8) | 2 | (1.2) |
| Prior drug use* | 351 | (4.8) | 290 | (10.8) | 40 | (5.9) | 2 | (1.2) |
| Education level* | ||||||||
| Grade School | 127 | (1.8) | 40 | (1.5) | 105 | (15.4) | 2 | (1.2) |
| High School | 2270 | (31.2) | 974 | (36.4) | 189 | (27.7) | 25 | (15.2) |
| College | 2321 | (31.9) | 794 | (29.7) | 154 | (22.5) | 65 | (39.7) |
| Post College | 429 | (5.9) | 92 | (3.4) | 14 | (2.0) | 17 | (10.4) |
| Unknown | 2125 | (29.3) | 776 | (29.0) | 221 | (32.4) | 55 | (33.5) |
| Working for Income* | 1286 | (17.7) | 299 | (11.2) | 90 | (13.2) | 38 | (23.2) |
BMI indicates body mass index; BTT, bridge to transplant; CAD, indicates coronary artery disease; KCCQ12, Kansas City Cardiomyopathy Questionnaire 12; LVAD, left ventricular assist device; VAD center volume, number per center per year; RVAD, right ventricular assist device; TAH, total artificial heart
Indicates significance at p<0.05;
p-values may be invalid due to small cell counts, exact values cannot be calculated;
exact test due to small counts in some cells.
Outcomes
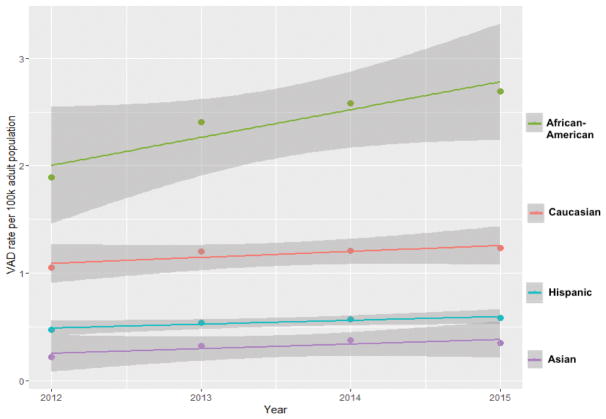
In 2012, the estimated annual census-adjusted rate of VAD implantation per 100,000 was 1.09 (95% Confidence Interval 0.93–1.25) in Caucasians, 2.01 (1.84–2.17) in African-Americans, 0.49 (0.33–0.65) in Hispanics, and 0.26 (0.10–0.42) in Asians (Table 2, Figure 1a). From 2012–2015, the rate increased significantly per 100,000 by 0.26 (0.17–0.34) in African-Americans. No significant changes were observed in other racial/ethnic groups [rate change: Hispanics 0.04 (−0.05–0.12), Asians 0.04 (−0.04–0.13), Caucasians 0.06 (−0.03–0.14)].
Table 2.
Estimated Baseline Rates and Estimated Change in Annual Census-Adjusted Rate of VAD Implantation Per 100,000
| Caucasian | African-American | Hispanic | Asian | |||||
|---|---|---|---|---|---|---|---|---|
| 2012 Rate n=1621 |
Change in Rate per Year 2012–2015 |
2012 Rate n=514 |
Change in Rate per Year 2012–2015 |
2012 Rate n=143 |
Change in Rate per Year 2012–2015 |
2012 Rate n=27 |
Change in Rate per Year 2012–2015 |
|
| All Groups | 1.09 (0.93–1.25) | 0.06 (−0.03–0.14) | 2.01 (1.84–2.17) | 0.26* (0.17–0.34) | 0.49 (0.33–0.65) | 0.04 (−0.05–0.12) | 0.26 (0.10–0.42) | 0.04 (−0.04–0.13) |
| Sex | † | |||||||
| Women | 0.38 (0.20–0.55) | 0.02 (−0.07–0.11) | 1.15 (0.98–1.33) | 0.16* (0.07–0.25) | 0.21 (0.04–0.39) | 0.02 (−0.07–0.11) | 0.08 (−0.09–0.26) | 0.02 (−0.08–0.11) |
| Men | 1.85 (1.67–2.02) | 0.09 (0.00–0.18) | 2.99 (2.82–3.17) | 0.37* (0.28–0.46) | 0.76 (0.59–0.94) | 0.05 (−0.04–0.14) | 0.46 (0.28–0.63) | 0.07 (−0.02–0.17) |
| Age group (years) | † | † | ||||||
| 20–39 | 0.27 (−0.12–0.66) | 0.03 (−0.18–0.24) | 0.88 (0.49–1.28) | 0.12 (−0.09–0.33) | 0.19 (−0.2–0.58) | 0.00 (−0.21–0.21) | 0.15 (−0.25–0.54) | 0.00 (−0.21–0.21) |
| 40–49 | 0.64 (0.25–1.03) | 0.08 (−0.13–0.28) | 2.08 (1.69–2.47) | 0.48* (0.27–0.69) | 0.33 (−0.06–0.72) | 0.04 (−0.17–0.25) | 0.16 (−0.23–0.55) | 0.04 (−0.16–0.25) |
| 50–59 | 1.35 (0.96–1.74) | 0.15 (−0.06–0.36) | 3.28 (2.89–3.67) | 0.46* (0.25–0.66) | 0.89 (0.5–1.28) | 0.05 (−0.16–0.26) | 0.22 (−0.17–0.61) | 0.24* (0.03–0.45) |
| 60–69 | 2.63 (2.24–3.02) | 0.02 (−0.19–0.23) | 4.28 (3.88–4.67) | 0.23* (0.02–0.44) | 1.88 (1.49–2.27) | 0.09 (−0.12–0.3) | 0.66 (0.27–1.05) | 0.04 (−0.17–0.25) |
| 70+ | 1.39 (1.00–1.78) | −0.04 (−0.25–0.17) | 1.43 (1.04–1.82) | 0.02 (−0.19–0.23) | 0.74 (0.35–1.13) | 0.04 (−0.17–0.25) | 0.59 (0.20–0.98) | −0.13 (−0.34–0.08) |
Denotes significant p<0.05;
significant subgroup interactions of sex*time for African-Americans p=0.004, age group*time for African-Americans p<0.01, and age group*time Asians p=0.02; and 95% Confidence Intervals are in parenthesis
Figure 1. VAD Implantation Rates Per Capita (A), VAD Implantation Rates Per Capita by Sex (B), and VAD Implantation Rates Per Capita by Age Group (C).
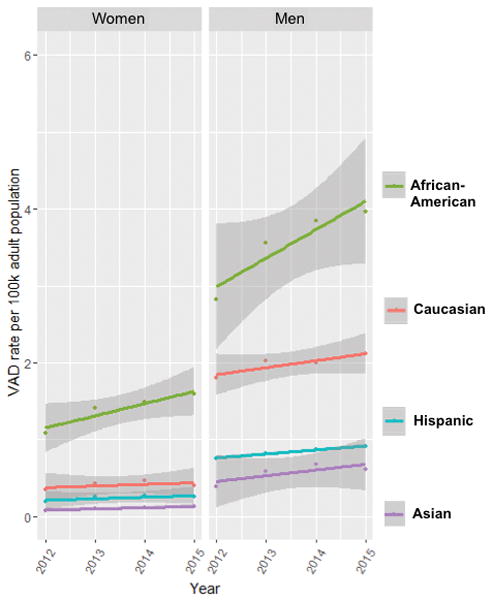
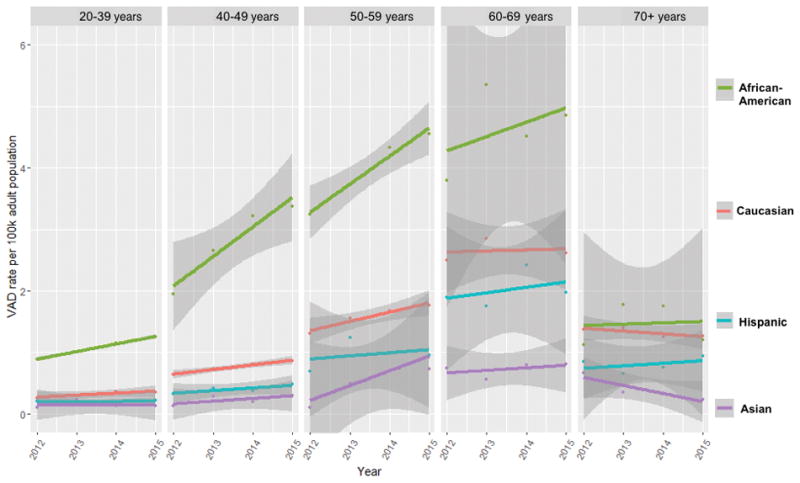
Dots represent annual rates within each race/ethnic group; k indicates 1,000 people. The 95% Confidence Interval band is shaded in gray.
Men had significantly higher baseline rates of VAD implantation than women within each racial/ethnic group [Caucasian men 1.85 (1.67–2.02), Caucasian women 0.38 (0.20–0.55), interaction p<0.001; African-American men 2.99 (2.82–3.17), African-American women 1.15 (0.98–1.33), interaction p<0.001; Hispanic men 0.76 (0.59–0.94), Hispanic women 0.21 (0.04–0.39), interaction p<0.001; Asian men 0.46 (0.28–0.63), Asian women 0.08 (−0.09–0.26), interaction p=0.005, Table 2, Figure 1b]. Both African-American men and women exhibited significant changes in rate of implantation from 2012–2015, but the rate of increase was higher in African-American men than women [African-American men 0.37 (0.28–0.46); African-American women 0.16 (0.07–0.25), interaction sex*time among African-Americans p=0.004]. Other racial/ethnic groups had no significant changes in the rate of VAD implantation by sex.
Stratified by age group, the baseline rate of VAD implantation trended towards higher rates with each successive decade until age 70, after which rates declined in each racial/ethnic group (Table 2, Figure 1c). African-Americans aged 40–69 years and Asians aged 50–59 years exhibited changes in the rate of VAD implantation from 2012–2015 [African-Americans: 40–49 years 0.48 (0.27–0.69), 50–59 years 0.46 (0.25–0.66), 60–69 years 0.23 (0.02–0.44); Asians 50–59 years 0.24 (0.03–0.45)]. The rate of VAD implantation differed by age group among African-Americans and Asians, and this difference persisted over time (interaction age groups*time among African-Americans p<0.01 and among Asians p=0.02).
DISCUSSION
In our study of the national INTERMACS database, VAD implantation rates increased significantly among African-Americans but not among other racial/ethnic groups from 2012–2015. When stratified by sex, a rate increase was observed in both African-American men and women, with the greatest increase observed in African-American men. When stratified by age group, rates increased among middle-aged African-Americans and Asians. The increased trend in VAD implantation rates among African-Americans is an important observation, since African-Americans consistently have the highest rates of heart failure and highest mortality secondary to heart failure.1
Insurance is required for VAD implantation.7 African-Americans have a high proportion of underinsurance,12 and the broadening of access to insurance during the period of study may have contributed to our findings. Similar patterns have been observed in heart transplants, which also require insurance, over the same time period.6 From 2012 to 2015, an increase in heart transplant listings in African-Americans was associated with the Affordable Care Act Medicaid Expansion.6 However, the INTERMACS dataset does not provide insurance type, month of implantation, or implantation center location granularity. Therefore, it is difficult to infer that the changes in rate are all or in part due to insurance.
Additional considerations for racial differences in VAD implantation include an increase in the number of destination VAD centers during the study period. The bridge to transplant strategy occurs primarily at heart transplant centers, which have been stagnant in number.13 Since 2012, over 20 additional destination therapy VAD centers have received CMS approval.14 Most VAD centers are located in metropolitan settings with larger proportions of African-American residents.14 In this study, destination VAD was the strategy for a greater proportion of African-American and Caucasian patients than Hispanic and Asian patients. An additional contributor to the observed changes in VAD implant rates may be increased public awareness of VAD technology following the publicity resulting from VAD implantation in a public figure.9 However, no data on racial/ethnic preferences for advanced therapies currently exist. Increased awareness would not be expected to differ by race or ethnicity, but awareness may contribute to the overall upwards trend of total VAD implantations across the U.S.
Women received fewer VADs than men, similar to heart transplant where women receive less than a quarter of heart transplants.6,15 It is posited that this is related to the lower incidence of systolic heart failure in women1 and higher prevalence of heart failure with preserved ejection fraction,1,7 which is not an indication for VAD implantation. However, this rationale for disparities breaks down when considering the interaction of race/ethnicity. Heart failure with reduced ejection fraction is the most common etiology of heart failure admissions for African-American women,16 who have the highest rate of HF among women, followed by Caucasian, Hispanic, and Asian women.1 In addition, before the age of 75, rates of heart failure are higher in African-American women than either Caucasian men or women.1 In our study, the rate of VAD implantation increased significantly among African-American women, with rates higher than Caucasian women but lower than Caucasian men. Many factors likely contribute to these findings by age and sex. Further study is needed to understand the healthcare provider and patient decision-making process for VAD implantation.
By age, VAD implantation rates mimicked rates of heart failure, increasing with successive decades of life.1 Within racial/ethnic groups, rates increased among African-Americans aged 40–69 and Asians aged 50–59. This follows an expected pattern for African-Americans since they develop heart failure at younger ages.1 The pattern is less clear for Asians who have the lowest prevalence of heart failure.1 The underreporting of Asian race, heterogeneity of the Asian population, and variability of cardiovascular risk factors among the different Asian ethnicities likely contribute and require further study.17
A new trend developed among the age group of 70+. Beyond the seventh decade of life, implant rates declined across all racial/ethnic groups, particularly among African-Americans. This may reflect a hesitancy to provide advanced therapies to those 70+ years of age. As observed in heart transplants, patients in their seventh decade are often declined VAD therapy due to increased comorbidities, frailty, and lower life expectancy due to age alone.18 As the general population continues to age, the advanced heart failure guidelines for older patients may require additional consideration.7,18 Investigation of the racial differences in VAD implantation in patient older than 70 years, is warranted.
The understanding of racial disparities in VAD implantation is incomplete. We found that per capita VAD implantation rates were the highest among African-Americans, followed by Caucasians, Hispanics, and Asians. Although the per capita rate in African-Americans was double the rate of Caucasians, this rate was lower than expected based on differences in HF incidence by race. In 2012, a per capita rate of 2.01 in African-Americans translates to 514 VAD and a per capita rate of 1.09 in Caucasians translates to 1621 VAD. Annual heart failure rates are two to three times higher in African-Americans than Caucasians before age 75,1 and the majority of VADs are implanted in this population.3 Adjusted for age, the 2012 heart failure discharge rate per capita of 100,000 has been reported as 875 in African-American men, 376 in Caucasian men, 663 in African-American women, and 270 in Caucasian women.19 Thus, this suggests there is a racial disparity. Yet, several factors reduce the ability to clarify disparities. Specifically, it is unknown nationally who has advanced heart failure, who is not getting an appropriate referral for VAD evaluation, and who is not being approved for VAD. It is known that African-Americans with heart failure are less likely to receive care by cardiologists than Caucasians and that racial biases inhibit general referral of African-Americans to cardiologists.20,21 Comprehensive identification of the at risk U.S. advanced heart failure population and identification of racial/ethnic and gender variation in the referral and evaluation for advanced therapies is needed to achieve health equity. Specifically, future work should investigate 1) whether clinical decision-making for allocation of advanced therapies differ by race/ethnicity and gender and 2) whether patient preferences for advanced therapies differ by race/ethnicity and gender.
Study Limitations
This study has several limitations. First, the denominator of the rate included the U.S. census population, which prohibited adjustment for patient characteristics. However, results were stratified and adjusted for by age and sex, which may be the most pertinent characteristics. The best denominator, all patients with advanced heart failure, is not currently available and collection of this data should be an objective of future national registries. Second, insurance status was unknown. We do know that carrying insurance is a guideline requirement for VAD implantation.7 Therefore, it is likely that all patients had some form of health insurance, but we do not know about otherwise eligible patients who had insufficient insurance to receive a VAD in this time period. Third, this dataset lacks information on patients referred for VAD evaluation and declined for implantation. The clinical decision-making processes leading to referral and approval of VAD may contribute to racial/ethnic and gender disparities, and these processes require investigation. Last, INTERMACS was not a required registry for VAD implantation after 2014.10 Although all VAD implants in the U.S. may have not been captured, the continued increase in center participation with INTERMACS suggests that the number of missing patients is likely trivial in the dataset used for this analysis.
CONCLUSIONS
From 2012–2015, VAD implantation rates increased significantly among African-Americans, particularly among middle-aged African-American men. Other races/ethnicities and subgroups by sex and age had no changes in the rate of VAD implantation during this time period with the exception of middle-aged Asians. This suggests that racial disparities may be declining among African-Americans, but further investigation is needed to reduce racial/ethnic disparities observed by sex and age.
What Is New?
From 2012–2015, the annual census-adjusted rate of ventricular assist devices (VAD) implantation increased in African-Americans but not among other racial/ethnic groups.
The change in rate was higher among African-American men than women. No differences by sex were seen among other racial/ethnic groups.
Changes in rate varied according to age group. The change in rate of VAD implant was higher among middle-aged African-Americans and Asians relative to older and younger age groups. No differences by age group were seen among other racial/ethnic groups.
What Are The Clinical Implications?
This study demonstrates that per capita, disparities in receipt of VAD appear to be decreasing among African-Americans who have the highest rates of heart failure. However, racial/ethnic differences in referral rates and approval rates for VAD are unknown. Further investigation should address racial/ethnic and gender variability in the clinical decision-making process for VAD.
Acknowledgments
Sources of Funding: Dr. Breathett received support from the American Heart Association (AHA) Heart Failure Strategically Focused Research Network (#16SFRN29640000), NIH L60 MD010857, University of Colorado, Department of Medicine, Health Services Research Development Grant Award, and the University of Arizona Health Sciences, Strategic Priorities Faculty Initiative Grant. Dr. Allen discloses grant funding from NIH (K23 HL105896), the Patient Centered Outcomes Research Institute (CDR-1310-06998), and the AHA (#16SFRN29640000). Dr. Daugherty received grant funding from the NIH (R01 HL133343) and the AHA (#2515963). Dr. Sweitzer received grant funding from the NIH (U01 HL131014).
Footnotes
Disclosures: Dr. Allen has served as consultant for J&J, Novartis, St. Jude, and ZS Pharma. Otherwise there are no disclosures.
References
- 1.Benjamin EJ, Virani SS, Callaway CW, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, Ferranti SD, de Ferguson JF, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Lutsey PL, Matchar DB, Matsushita K, Mussolino ME, Nasir K, O’Flaherty M, Palaniappan LP, Pandey DK, Reeves MJ, Ritchey MD, Rodriguez CJ, Roth GA, Rosamond WD, Sampson UKA, Satou GM, Shah SH, Spartano NL, Tirschwell DL, Tsao CW, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P. Heart Disease and Stroke Statistics—2018 Update: A Report From the American Heart Association. Circulation. 2018 doi: 10.1161/CIR.0000000000000558. CIR.0000000000000558. [DOI] [PubMed] [Google Scholar]
- 2.Breathett K, Allen LA, Ambardekar AV. Patient-centered care for left ventricular assist device therapy: current challenges and future directions. Curr Opin Cardiol. 2016;31:313–20. doi: 10.1097/HCO.0000000000000279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Interagency Registry for Mechanically Assisted Circulatory Support: The Data and Clinical Coordinating Center. University of Alabama; Birmingham: 2015. [Accessed April 16, 2016]. INTERMACS Quarterly Statistical Report 2015 Q1 Implant and event dates: June 23, 2006 to March 31, 2015. https://www.uab.edu/medicine/intermacs/images/Federal_Quarterly_Report/Federal_Partners_Report_2015_Q1.pdf. [Google Scholar]
- 4.Lampropulos JF, Kim N, Wang Y, Desai MM, Barreto-Filho JAS, Dodson JA, Dries DL, Mangi AA, Krumholz HM. Trends in left ventricular assist device use and outcomes among Medicare beneficiaries, 2004–2011. Open Heart. 2014;1:e000109. doi: 10.1136/openhrt-2014-000109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Munir MB, Sharbaugh MS, Thoma FW, Nisar MU, Kamran AS, Althouse AD, Saba S. Trends in hospitalization for congestive heart failure, 1996–2009. Clin Cardiol. 2017;40:109–119. doi: 10.1002/clc.22638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Breathett K, Allen LA, Helmkamp L, Colborn K, Daugherty SL, Khazanie P, Lindrooth R, Peterson PN. The Affordable Care Act Medicaid Expansion Correlated With Increased Heart Transplant Listings in African-Americans But Not Hispanics or Caucasians. JACC Heart Fail. 2017;5:136–147. doi: 10.1016/j.jchf.2016.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Feldman D, Pamboukian SV, Teuteberg JJ, Birks E, Lietz K, Moore SA, Morgan JA, Arabia F, Bauman ME, Buchholz HW, Deng M, Dickstein ML, El-Banayosy A, Elliot T, Goldstein DJ, Grady KL, Jones K, Hryniewicz K, John R, Kaan A, Kusne S, Loebe M, Massicotte MP, Moazami N, Mohacsi P, Mooney M, Nelson T, Pagani F, Perry W, Potapov EV, Eduardo Rame J, Russell SD, Sorensen EN, Sun B, Strueber M, Mangi AA, Petty MG, Rogers J. The 2013 International Society for Heart and Lung Transplantation Guidelines for mechanical circulatory support: Executive summary. J Heart Lung Transplant. 2013;32:157–187. doi: 10.1016/j.healun.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 8.Kirklin JK, Naftel DC, Pagani FD, Kormos RL, Stevenson LW, Blume ED, Myers SL, Miller MA, Baldwin JT, Young JB. Seventh INTERMACS annual report: 15,000 patients and counting. J Heart Lung Transplant. 2015;34:1495–1504. doi: 10.1016/j.healun.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 9.Pandey A, Abdullah K, Drazner MH. Impact of Vice President Cheney on public interest in left ventricular assist devices and heart transplantation. Am J Cardiol. 2014;113:1529–1531. doi: 10.1016/j.amjcard.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 10.UAB - School of Medicine. [Accessed January 4, 2018];Interagency Registry for Mechanically Assisted Circulatory Support - Home. https://www.uab.edu/medicine/intermacs/
- 11. [Accessed January 4, 2018];Decision Memo for Ventricular Assist Devices for Bridge-to-Transplant and Destination Therapy (CAG-00432R) https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=268.
- 12.McMorrow S, Long SK, Kenney GM, Anderson N. Uninsurance Disparities Have Narrowed For Black And Hispanic Adults Under The Affordable Care Act. Health Aff Proj Hope. 2015;34:1774–1778. doi: 10.1377/hlthaff.2015.0757. [DOI] [PubMed] [Google Scholar]
- 13. [Accessed October 4, 2016];SRTR -- Scientific Registry of Transplant Recipients. http://www.srtr.org/csr/archives/default.aspx.
- 14.Medicare C for, Baltimore MS 7500 SB, Usa M. [Accessed January 8, 2018];VAD Destination Therapy Facilities. 2016 https://www.cms.gov/Medicare/Medicare-General-Information/MedicareApprovedFacilitie/VAD-Destination-Therapy-Facilities.html.
- 15.Colvin-Adams M, Smith JM, Heubner BM, Skeans MA, Edwards LB, Waller CD, Callahan ER, Snyder JJ, Israni AK, Kasiske BL. OPTN/SRTR 2013 Annual Data Report: Heart. Am J Transplant. 2015;15:1–28. doi: 10.1111/ajt.13199. [DOI] [PubMed] [Google Scholar]
- 16.Chang PP, Chambless LE, Shahar E, Bertoni AG, Russell SD, Ni H, He M, Mosley TH, Wagenknecht LE, Samdarshi TE, Wruck LM, Rosamond WD. Incidence and survival of hospitalized acute decompensated heart failure in four US communities (from the Atherosclerosis Risk in Communities Study) Am J Cardiol. 2014;113:504–510. doi: 10.1016/j.amjcard.2013.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Palaniappan LP, Araneta MRG, Assimes TL, Barrett-Connor EL, Carnethon MR, Criqui MH, Fung GL, Narayan KMV, Patel H, Taylor-Piliae RE, Wilson PWF, Wong ND Prevention on behalf of the AHAC on E and, Disease C on PV, Nutrition C on, Activity P, Metabolism A, Cardiology C on C, Nursing and C on C. Call to Action: Cardiovascular Disease in Asian Americans: A Science Advisory From the American Heart Association. Circulation. 2010;122:1242–1252. doi: 10.1161/CIR.0b013e3181f22af4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mehra MR, Canter CE, Hannan MM, Semigran MJ, Uber PA, Baran DA, Danziger-Isakov L, Kirklin JK, Kirk R, Kushwaha SS, Lund LH, Potena L, Ross HJ, Taylor DO, Verschuuren EAM, Zuckermann A International Society for Heart Lung Transplantation (ISHLT) Infectious Diseases, Pediatric and Heart Failure and Transplantation Councils. The 2016 International Society for Heart Lung Transplantation listing criteria for heart transplantation: A 10-year update. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2016;35:1–23. doi: 10.1016/j.healun.2015.10.023. [DOI] [PubMed] [Google Scholar]
- 19.Ziaeian B, Kominski GF, Ong MK, Mays VM, Brook RH, Fonarow GC. National Differences in Trends for Heart Failure Hospitalizations by Sex and Race/Ethnicity. Circ Cardiovasc Qual Outcomes. 2017;10:e003552. doi: 10.1161/CIRCOUTCOMES.116.003552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Breathett K, Jones J, Lum HD, Koonkongsatian D, Jones CD, Sanghvi U, Hoffecker L, McEwen M, Daugherty SL, Blair IV, Calhoun E, de Groot E, Sweitzer NK, Peterson PN. Factors Related to Physician Clinical Decision-Making for African-American and Hispanic Patients: a Qualitative Meta-Synthesis. J Racial Ethn Health Disparities. 2018 Mar 5; doi: 10.1007/s40615-018-0468-z. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Breathett K, Liu WG, Allen LA, Daugherty SL, Blair IV, Jones J, Grunwald GK, Moss M, Kiser TH, Burnham E, Vandivier RW, Clark BJ, Lewis EF, Mazimba S, Battaglia C, Ho PM, Peterson PN. African Americans Are Less Likely to Receive Care by a Cardiologist During an Intensive Care Unit Admission for Heart Failure. JACC Heart Fail. 2018;6:413–420. doi: 10.1016/j.jchf.2018.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]