Abstract
Background
Suboptimal diets are a major contributor to cardiometabolic disease (CMD) mortality, and substantial disparities exist for both dietary quality and mortality risk across income groups in the United States. Research is needed to quantify how food pricing policies to subsidize healthy foods and tax unhealthy foods could affect US CMD mortality, overall and by Supplemental Nutrition Assistance Program (SNAP) eligibility and participation.
Methods
Comparative risk analysis based on national data on diet (NHANES, 2003–2012) and mortality (mortality-linked NHIS) and meta-analyses of policy-diet and diet-disease relationships.
Results
A national 10% price reduction on fruits, vegetables, nuts, and whole grains was estimated to prevent 19,600 CMD deaths/year, including 2.6% (95% UI: 2.4%, 2.8%) of all CMD deaths among SNAP participants, 2.7% (2.4%, 3.0%) among SNAP-eligible non-participants, and 2.6% (2.4%, 2.8%) among SNAP-ineligible non-participants. Adding a national 10% tax on sugar-sweetened beverages (SSBs) and processed meats would prevent a total of 33,700 CMD deaths/year, including 5.9% (5.4%, 7.4%) of all CMD deaths among SNAP participants, 4.8% (4.4%, 5.2%) among SNAP-eligible non-participants, and 4.1% (3.8%, 4.5%) among SNAP-ineligible non-participants. Adding a SNAP-targeted 30% subsidy for the same healthy foods would offer the largest reductions in both CMD mortality and disparities.
Conclusion
National subsidies for healthy foods and taxes on SSBs and processed meats would each reduce CMD mortality; taxes would also reduce CMD mortality more steeply for SNAP participants than for non-participants.
INTRODUCTION
Coronary heart disease (CHD), stroke, and type 2 diabetes contribute to more than 800,000 deaths each year in the United States (US),1 representing the first, third, and seventh leading causes of death, respectively.2 Direct and indirect economic costs of these diseases are staggering, approaching 1 trillion dollars annually.1 Suboptimal diets are a major contributor to these cardiometabolic diseases (CMD),2–3 and substantial disparities exist with regard to both dietary quality and mortality risk across income groups in the US.1 These burdens highlight the need for innovative systems investments to improve diet, reduce costs, and reduce disparities among Americans.
Food pricing policies support and promote healthier dietary choices.4–8 Such policies might also reduce dietary and health disparities, given the higher price-sensitivity of lower income groups.9 Eight US cities/localities have now passed taxes on sugar-sweetened beverages (SSBs), including 4 in the 2016 elections.10 In addition, several pilot programs now subsidize purchases of fruits and vegetables for low-income Americans, including a new $100M program for the Supplemental Nutrition Assistance Program (SNAP, formerly Food Stamps).11–14 Yet, the potential impacts on health and disparities of similar national efforts in the United States are not well-established.
To address these issues, we combined nationally representative data with evidence from interventional and longitudinal studies on the effects of food pricing interventions to model the potential effects of price decreases for specific healthy foods (fruits, vegetables, nuts, whole grains) and price increases for specific unhealthy foods (SSBs, processed meats) on changes in dietary habits and mortality from CHD, stroke, and diabetes in the United States. We evaluated the possible impact of both national pricing changes and additional targeted incentives within SNAP, the largest US nutrition assistance program, which provides financial benefits for food retail purchases to ~42.2 million individuals (about 1 in 8 Americans).15–16 While SNAP has been successful at improving food insecurity,17 the dietary quality of SNAP participants remains low;18 SNAP participants have higher mortality rates than Americans not on SNAP, even compared to income-eligible non-participants; and much of this excess death is due to CMD.19
Evaluating the potential impact of national and SNAP-targeted food pricing strategies may help to inform important US policy discussions, including new nutrition-oriented provisions proposed in the SNAP reauthorization as part of the next U.S. Farm Bill, as well as taxes on soda and other foods being proposed and implemented in many localities. Such findings may also help to inform the potential impact of recently implemented or announced national food pricing frameworks in other countries.20–21 This research was performed as part of the Food-PRICE (Policy Review and Intervention Cost-Effectiveness) Project.
METHODS
Study design
We used a comparative risk assessment (CRA) model22 to estimate the effects of changes in food retail prices on dietary habits and cardiometabolic mortality in the United States among SNAP participants, SNAP-eligible non-participants, and SNAP-ineligible individuals. The CRA model combined nationally representative inputs on baseline demographics, diet, and mortality; effects of population pricing interventions on dietary behaviors from interventional studies and natural experiments; and associations of dietary changes with disease outcomes from meta-analyses of prospective cohort studies; each according to age, sex, and other underlying population demographics (each listed in Table S1 and described further below).
Current food consumption
Baseline national dietary habits of adults according to SNAP status were acquired from the National Health and Nutrition Examination Survey (NHANES),23–24 averaging 5 cycles (2003–2012; N=20,102 adults with dietary data) to maximize precision in subgroups. Data from the most recent cycle (2013–2014) were not included because at the time of analysis, USDA had not yet released datasets to account for mixed dishes. SNAP participants were identified by whether someone in their household received benefits at some point in the previous 12 months; and SNAP eligibility by the primary USDA criterion of a household income-to-poverty ratio<=1.3. As previously described,23 we included all participants completing at least one 24-hour recall administered by a trained interviewer; the great majority of participants also completed a second 24-hour recall by telephone on a non-consecutive day. Data from available 24-hour recalls were averaged for each participant for each dietary target, and resulting intakes were then investigated by strata of interest including age (25–34y, 35–44y, 45–54y, 55–64y, 65–74y, and 75y+), sex, and SNAP eligibility and participation status. We focused on four food groups for subsidies (fruits, vegetables, nuts, whole grains) and two food/beverage groups for taxes (SSBs, processed meats), based on existing experience and interest in altering their food prices and/or evidence for their effects on cardiometabolic outcomes.22, 25 Fruits and vegetables included any form: fresh, frozen, canned, or dried. Dietary factors were modeled based on their mean and SD in each stratum using gamma (rather than normal) distributions, allowing for and incorporating skewed distributions.
Current population and mortality data
Baseline mortality rates from CHD, stroke, and diabetes were derived from 2000–2009 National Health Interview Survey (NHIS) data, by age, sex, and SNAP eligibility and participation status.26–27 To estimate the absolute number of deaths within each age-sex-SNAP group, we used 2014 data from the Current Population Survey (N=88,595),28 a sufficiently large sample to enable precise estimates by SNAP eligibility and participation group. The population size of each stratum was obtained from the 2014 American Community Survey. Further details on data development related to population and mortality estimates are provided in the Supplemental Methods.
Effects of price changes on food consumption
We modeled national pricing interventions as well as targeted interventions implemented through the SNAP Electronic Benefit Transfer (EBT) card. The effects of price changes on dietary consumption were derived from a recent meta-analysis of longitudinal and interventional studies of food pricing changes.8 For national pricing interventions, we incorporated evidence for modestly larger price-responsiveness among lower income groups,29 with an 18% greater price response among SNAP participants and SNAP-eligible non-participants, compared with SNAP-ineligible (higher-income) individuals. For example, based on these data sources, each 1% reduction in national food price was estimated to increase fruit consumption by 1.31% among SNAP-ineligible individuals, compared with 1.54% among SNAP participants and SNAP-eligible non-participants.
For SNAP-targeted interventions operating through the EBT card, we used results from the SNAP Healthy Incentives Pilot (HIP), a randomized trial of food subsidies for purchasing fruits and vegetables.12–13 Because most SNAP participants also purchase foods with their own funds outside the EBT system,13 we modeled a smaller net effect of this intervention on total dietary consumption. For these SNAP-specific interventions, a 1% reduction in price would lead to an average 0.87% increase in consumption among SNAP participants. The details of our price response assumptions are provided in Table S2, and the distribution of population by age/sex and SNAP category are provided in Table S3.
Effect of dietary changes on disease outcomes
Methods for identifying, synthesizing, and validating evidence to estimate effect sizes (relative risks) for associations between dietary factors and cardiometabolic endpoints have been described in detail.22, 30 Briefly, etiologic effects were obtained from meta-analyses of prospective studies for both direct diet-disease relationships (e.g. fruit intake and CHD) and, for SSBs, additional effects mediated by changes in body mass index (see Table S4). We incorporated declining proportional effects of dietary factors on disease endpoints with age, as previously described.25 Several validity analyses assessed the potential influence of confounding as well as bias from health effects of overall dietary patterns, including compared to findings from randomized controlled trials.22, 30 These validity analyses demonstrated that estimated effect sizes for individual dietary components were very similar to what would be expected based on these other independent lines of evidence, including from trials.
Pricing interventions
We evaluated two levels of price changes (10%, 30%) based on recent existing and proposed interventions of food subsidies and taxes.7, 12–13, 31 We modeled the impact of subsidies alone (on fruits, vegetables, nuts, whole grains), or these subsidies plus additional taxes (on SSBs and processed meat); and at nationwide levels alone, or at nationwide levels plus additional SNAP-specific incentives. The resulting 6 interventions are shown in Table 1.
Table 1.
Six food and beverage subsidy and tax policy interventions.*
| National | SNAP participants only | ||
|---|---|---|---|
|
|
|
||
| Intervention (Subsidy / Tax / SNAP subsidy) |
Subsidy Fruit, veg., nuts, whole grains |
Tax SSBs, processed meats |
Additional SNAP subsidy via EBT Fruit, veg., nuts, whole grains‡ |
| 1a. (10/0/0) | 10% | - | - |
| 1b. (10/10/0) | 10% | 10% | - |
| 2a. (30/0/0) | 30% | - | - |
| 2b. (30/30/0) | 30% | 30% | - |
| 3a. (10/0/30) | 10% | - | 30% |
| 3b. (10/10/30) | 10% | 10% | 30% |
The modeled price change reflects the final retail price, without assumptions about the specific mechanism for the price changes. For example, lower prices (subsidies) could be achieved by subsidies for agricultural production, storage, or transport; R&D or tax incentives for food manufacturers, retailers, and restaurants; or direct subsidies to wholesalers, retailers, or consumers. Higher prices (taxes) could be achieved by changes in agricultural policies; tariffs; or excise taxes at manufacturer, wholesaler, or retailer levels.
The SNAP-targeted subsidy operates through Electronic Benefit Transfer (EBT) cards and is in addition to the national subsidy or tax.
Our modeling evaluated the final retail price changes, without assumptions about the mechanisms of pricing changes. For example, lower prices (subsidies) for fruits, vegetables, nuts, and whole grains could be potentially achieved by direct subsidies to wholesalers, retailers, or consumers; subsidies for agricultural production, storage, or transport; or research and development or tax incentives for food manufacturers, retailers, and restaurants. Similarly, higher prices (taxes) on SSBs and processed meats could be achieved by changes in agricultural policies; tariffs; fees; or (most commonly) excise taxes on food manufacturers, distributors, wholesalers, or retailers.32 For the SNAP-targeted subsidy, we assumed this would operate through the Electronic Benefit Transfer (EBT) system and apply to fruit, vegetables, nuts, and whole grains.
Statistical analysis
The CRA model separately assessed stratum-specific mortality outcomes for CHD, stroke subtypes, and diabetes, which were summed to quantify total stroke and total CMD (CHD, stroke, and diabetes) mortality. Estimated changes in absolute mortality (deaths/year) and proportional mortality (percent of CMD deaths) were calculated for each age-sex-SNAP stratum (see Supplemental Methods for additional detail). For the main statistical analyses, we summed across the age-sex strata to report estimated changes for all adults in proportional mortality (percent of CMD deaths) and mortality per 100,000 adults in the population, by SNAP participation and eligibility status. The main results reported estimated changes in mortality outcomes for the actual US populations of SNAP participants, SNAP-eligible non-participants, and SNAP-ineligible (higher-income) individuals, in response to the six interventions. Given the much lower mean age of SNAP participants compared with both SNAP-eligible non-participants and ineligible individuals (Table S3), we also adjusted for age-sex distributions by reporting (a) the estimated changes in mortality for each detailed age-sex-SNAP stratum and (b) the age- and sex-adjusted summary results for all adults.
Sources of uncertainty were incorporated into all results by means of multi-way probabilistic sensitivity analyses, jointly accounting for statistical uncertainty in baseline dietary consumption, main effects of food pricing changes on dietary intakes, and associations of dietary changes with mortality. Monte Carlo simulations (1,000) provided a final central estimate derived from the median (50th percentile) result, and 95% uncertainty intervals (UIs) from the 2.5th and 97.5th percentile results. Analyses were performed using R version 3.2.4 (Vienna, Austria).
RESULTS
Current US dietary intakes and responses to food pricing interventions
At baseline, consumption of fruits, vegetables, nuts, and whole grains were each below dietary recommendations in all groups, with the shortfall larger among SNAP-eligible non-participants and especially SNAP participants, compared to SNAP-ineligible Americans (Table 2). For example, compared with the recommended consumption of about 120–160 g/d (1.5–2.0 cups/d), fruit consumption was 76 g/d among SNAP participants, 98 g/d among SNAP-eligible non-participants, and 114 g/d among SNAP-ineligible adults. Similarly, intakes of sugar-sweetened beverages (SSBs) and processed meat were higher than optimal for all groups, with disparities by SNAP participation and eligibility status. For example, mean intake of SSBs was 518 g/d (2.2 8-fl.-oz servings/d) among SNAP participants, 413 g/d (1.7 servings/d) among SNAP-eligible non-participants, and 293 g/d (1.2 servings/d) among ineligible individuals.
Table 2.
Baseline intakes and changes in intake for food groups targeted by pricing changes in the United States.
| Baseline intake among U.S. adults (age 25+ y), mean (95% UI)* | ||||
|
|
||||
| SNAP participants | SNAP non-participants | |||
|
|
|
|||
| Eligible | Ineligible | |||
|
| ||||
| U.S. adult population in 2014 (1000s) | 21465 | 20677 | 171559 | |
| Subsidized foods | ||||
| fruit (g/d) | 76 (69,82) | 98 (91,104) | 114 (109,119) | |
| vegetables (g/d) | 140 (134,146) | 171 (161,180) | 186 (181,190) | |
| nuts (g/d) | 5.6 (4.8,6.4) | 6.4 (5.4,7.3) | 10.9 (10.3,11.5) | |
| whole grains (g/d) | 13.5 (12.1,14.9) | 15.8 (14.4,17.3) | 19.5 (18.7,20.2) | |
| Taxed foods | ||||
| SSB (g/d) | 518 (477,556) | 413 (384,442) | 293 (277,309) | |
| processed meat (g/d) | 33 (30,36) | 28 (27,30) | 31 (30,33) | |
| Change in intake for 10% subsidy (+) or tax (−), mean (95% UI)† | ||||
|
|
||||
| SNAP participants | SNAP non-participants | |||
|
|
|
|||
| Eligible | Ineligible | |||
|
|
|
|||
| Subsidized foods | ||||
| fruit (g/d) | 11.7 (10.6,12.6) | 15.1 (14,16) | 14.9 (14.3,15.6) | |
| vegetables (g/d) | 21.6 (20.6,22.5) | 26.3 (24.8,27.7) | 24.4 (23.7,24.9) | |
| nuts (g/d) | 0.86 (0.74,0.99) | 0.99 (0.83,1.12) | 1.43 (1.35,1.51) | |
| whole grains (g/d) | 2.08 (1.86,2.29) | 2.43 (2.22,2.66) | 2.55 (2.45,2.65) | |
| Taxed foods | ||||
| SSB (g/d) | −38 (−35,−41) | −30 (−28,−32) | −18 (−17,−19) | |
| processed meat (g/d) | −3.1 (−2.9,−3.4) | −2.7 (−2.5,−2.9) | −2.5 (−2.4,−2.6) | |
From NHANES, 2003–2012, accounting for complex survey sampling and weights to be nationally representative.
Based on longitudinal and interventional studies of food subsidies or taxes and including 18% greater price-responsiveness among low-income adults (SNAP-eligible non-participants or participants). Elasticity assumptions for changes in intake are detailed in Table S2. Changes in intake for larger taxes and subsidies are detailed in Table S5.
Average changes in intake in response to a 10% nationwide subsidy or tax varied according to SNAP eligibility and participation (Table 2). The uncertainty interval (UI) reflects sampling variation in the NHANES source data. Absolute changes (g/d) were dependent on both price elasticity (modestly higher among lower-income individuals) and baseline consumption levels (generally lower for healthier foods and higher for unhealthy foods among lower-income individuals). For example, a 10% reduction in the price of fruit generated an increase of 11.7 g/d among SNAP participants, 15.1 g/d among SNAP-eligible nonparticipants, and 14.9 g/d among SNAP-ineligible Americans. By contrast, based on both higher price responsiveness and higher baseline intake, a 10% price increase for SSBs and processed meats led to greater absolute reductions among lowest-income individuals. For example, a 10% price increase in SSBs generated a reduction of 38 g/d (0.16 servings/d) for SNAP participants, 30 g/d (0.12 servings/d) for SNAP-eligible non-participants, and 18 g/d (0.07 servings/d) for SNAP-ineligible individuals.
In response to 30% nationwide price changes (interventions 2a and 2b), changes in intake were correspondingly larger (Table S5). With the 30% SNAP-targeted price subsidy plus 10% national price subsidy (intervention 3a), changes in intake for the SNAP group were approximately the same as for the 30% national price subsidy (intervention 2a) (Table S5), because the additional impact of combining national and SNAP-targeted interventions was offset by the lower estimated price-responsiveness for the subsidy operating through the SNAP EBT card (Table S2).
Estimated effects of food pricing interventions on cardiometabolic mortality
The national 10% subsidy (intervention 1a) was estimated to prevent 2.2% of all CHD deaths, 5.5% of all stroke deaths, and 0.9% of all diabetes deaths, with negligible effects on disparities by SNAP participation and eligibility status (Figure 1, Table 3). The UI reflects multiple sources of uncertainty, including sampling variation in the NHANES source for the food intake data and uncertainty in the price elasticity estimates and the relative risk estimates. Overall, this intervention was estimated to reduce US CMD deaths by approximately 2.6% (Table S6). This mortality reduction amounted to 19,600 deaths/y nationally (Table 4, Table S7, Table S8). Corresponding estimates with adjustment for the age/sex distribution within SNAP participation and eligibility groups are provided in Tables S9 and S10.
Figure 1.
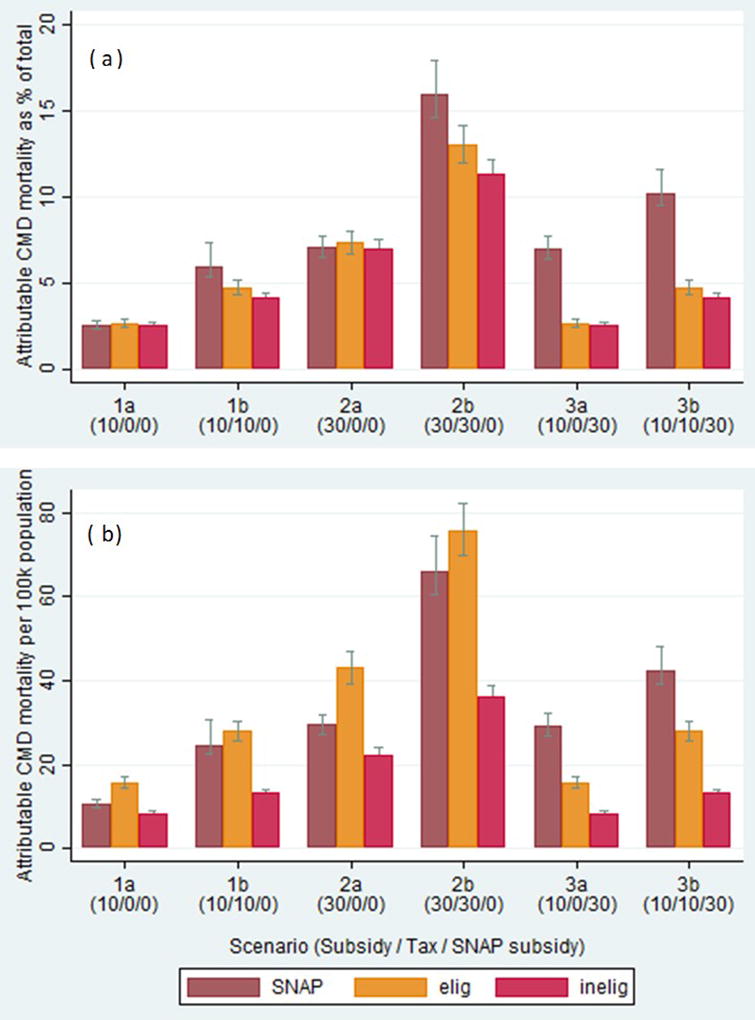
Estimated annual cardiometabolic disease (CMD) deaths averted as a percentage of total CMD deaths (panel A) or per 100,000 adults, adjusted for age and sex (panel B) attributable to six food price subsidy and tax interventions in the United States (see Table 1 for definitions of each intervention).
Table 3.
Annual CMD deaths averted (as % of deaths for each disease) attributable to six food price subsidy and tax interventions in the United States.*
| SNAP participants | SNAP non-participants | ||
|---|---|---|---|
|
|
|
||
| Eligible | Ineligible | ||
|
|
|
||
| U.S. adult population in 2014 (1000s) | 21465 | 20677 | 171559 |
| CHD: Baseline deaths/y per 100k adults | 248 | 354 | 193 |
| Prevented deaths as % of total CHD deaths (95% UI) | |||
| (Subsidy/Tax/SNAP subsidy) | |||
| 1a. (10/0/0) | 2.2 (1.9,2.5) | 2.2 (2,2.5) | 2.1 (1.9,2.4) |
| 1b. (10/10/0) | 4.3 (3.7,5.3) | 3.5 (3.1,4) | 2.9 (2.6,3.3) |
| 2a. (30/0/0) | 6.1 (5.4,6.9) | 6.1 (5.4,6.9) | 5.8 (5.2,6.5) |
| 2b. (30/30/0) | 11.5 (10.2,13.7) | 9.6 (8.5,10.8) | 8 (7.1,8.9) |
| 3a. (10/0/30) | 6 (5.3,6.9) | 2.2 (2,2.5) | 2.1 (1.9,2.4) |
| 3b. (10/10/30) | 8 (7.1,9.3) | 3.5 (3.1,4) | 2.9 (2.6,3.3) |
| Stroke: Baseline deaths/y per 100k adults | 81 | 139 | 73 |
| Prevented deaths as % of total stroke deaths (95% UI) | |||
| 1a. (10/0/0) | 5.5 (4.8,6.2) | 5 (4.2,5.8) | 4.9 (4.3,5.6) |
| 1b. (10/10/0) | 5.6 (4.9,6.3) | 5.1 (4.3,5.9) | 5 (4.3,5.6) |
| 2a. (30/0/0) | 14.9 (13.1,16.6) | 13.6 (11.5,15.5) | 13.2 (11.5,14.9) |
| 2b. (30/30/0) | 15.2 (13.4,17) | 13.8 (11.7,15.7) | 13.4 (11.6,15) |
| 3a. (10/0/30) | 14.7 (12.9,16.7) | 5 (4.2,5.8) | 4.9 (4.3,5.6) |
| 3b. (10/10/30) | 14.8 (13,16.8) | 5.1 (4.3,5.9) | 5 (4.3,5.6) |
| Diabetes: Baseline deaths/y per 100k adults | 85 | 91 | 53 |
| Prevented deaths as % of total diabetes deaths (95% UI) | |||
| 1a. (10/0/0) | 0.9 (0.7,1) | 0.9 (0.7,1) | 0.9 (0.7,1) |
| 1b. (10/10/0) | 6 (5.1,8) | 4.4 (3.8,5.3) | 3.4 (3,3.9) |
| 2a. (30/0/0) | 2.5 (2.1,3) | 2.5 (2.1,2.9) | 2.4 (2.1,2.8) |
| 2b. (30/30/0) | 16.2 (13.9,20.1) | 12.2 (10.6,14.1) | 9.6 (8.6,10.9) |
| 3a. (10/0/30) | 2.5 (2,3) | 0.9 (0.7,1) | 0.9 (0.7,1) |
| 3b. (10/10/30) | 7.6 (6.5,9.6) | 4.4 (3.8,5.3) | 3.4 (3,3.9) |
Six policy interventions as described in Table 1: (1a) national 10% subsidy, (1b) national 10% subsidy and 10% tax, (2a) national 30% subsidy, (2b) national 30% subsidy and 30% tax, (3a) national 10% subsidy plus 30% subsidy for SNAP purchases, (3b) national 10% subsidy and 10% tax plus 30% subsidy for SNAP purchases. Figure 1 (A) and Table S6 report combined results for total CMD (CHD, stroke, diabetes).
Table 4.
Annual deaths averted by disease (per 100k population) attributable to six food price subsidy and tax interventions in the United States.
| SNAP participants | SNAP non-participants | ||
|---|---|---|---|
|
|
|
||
| Eligible | Ineligible | ||
|
|
|
||
| U.S. adult population in 2014 (1000s) | 21465 | 20677 | 171559 |
| CHD: Baseline deaths/y per 100k adults | 248 | 354 | 193 |
| Prevented deaths/y per 100k adults (95% UI) | |||
| 1a. (10/0/0) | 5.5 (4.8,6.2) | 7.9 (6.9,9) | 4.1 (3.7,4.6) |
| 1b. (10/10/0) | 10.6 (9.2,13.1) | 12.5 (11,14.2) | 5.6 (5,6.3) |
| 2a. (30/0/0) | 15.1 (13.3,17.1) | 21.8 (19.1,24.6) | 11.2 (10,12.5) |
| 2b. (30/30/0) | 28.6 (25.2,33.9) | 34.1 (30.2,38.4) | 15.4 (13.7,17.1) |
| 3a. (10/0/30) | 15 (13.1,17.1) | 7.9 (6.9,9) | 4.1 (3.7,4.6) |
| 3b. (10/10/30) | 19.9 (17.7,23.2) | 12.5 (11,14.2) | 5.6 (5,6.3) |
| Stroke: Baseline stroke deaths/y per 100k adults | 81 | 139 | 73 |
| Prevented deaths/y per 100k adults (95% UI) | |||
| 1a. (10/0/0) | 4.4 (3.9,5) | 7 (5.9,8) | 3.6 (3.1,4.1) |
| 1b. (10/10/0) | 4.6 (4,5.1) | 7.1 (6,8.1) | 3.6 (3.1,4.1) |
| 2a. (30/0/0) | 12 (10.6,13.5) | 18.8 (15.9,21.6) | 9.7 (8.4,10.9) |
| 2b. (30/30/0) | 12.3 (10.9,13.8) | 19.1 (16.3,21.8) | 9.8 (8.5,11) |
| 3a. (10/0/30) | 11.9 (10.4,13.5) | 7 (5.9,8) | 3.6 (3.1,4.1) |
| 3b. (10/10/30) | 12 (10.5,13.6) | 7.1 (6,8.1) | 3.6 (3.1,4.1) |
| Diabetes: Baseline diabetes deaths/y per 100k adults | 85 | 91 | 53 |
| Prevented deaths/y per 100k adults (95% UI) | |||
| 1a. (10/0/0) | 0.7 (0.6,0.9) | 0.8 (0.7,0.9) | 0.5 (0.4,0.5) |
| 1b. (10/10/0) | 5.2 (4.3,6.8) | 4 (3.5,4.8) | 1.8 (1.6,2.1) |
| 2a. (30/0/0) | 2.1 (1.8,2.5) | 2.3 (1.9,2.7) | 1.3 (1.1,1.5) |
| 2b. (30/30/0) | 13.8 (11.9,17.1) | 11.1 (9.7,12.8) | 5.1 (4.6,5.8) |
| 3a. (10/0/30) | 2.1 (1.7,2.6) | 0.8 (0.7,0.9) | 0.5 (0.4,0.5) |
| 3b. (10/10/30) | 6.5 (5.6,8.2) | 4 (3.5,4.8) | 1.8 (1.6,2.1) |
Six policy interventions as described in Table 1: (1a) national 10% subsidy, (1b) national 10% subsidy and 10% tax, (2a) national 30% subsidy, (2b) national 30% subsidy and 30% tax, (3a) national 10% subsidy plus 30% subsidy for SNAP purchases, (3b) national 10% subsidy and 10% tax plus 30% subsidy for SNAP purchases. Figure 1 (B) and Table S6 report combined results for all three causes.
Adding a national 10% tax (intervention 1b) increased the numbers of both CHD and diabetes deaths prevented. Overall, this intervention was estimated to prevent 5.9% of all CMD deaths among SNAP participants, 4.8% among SNAP-eligible non-participants, and 4.1% among SNAP-ineligible non-participants (Figure 1, Table S6, Table S8). This combined intervention reduced US CMD by 33,700 deaths/y (Table S8), and also reduced disparities, with largest benefits among SNAP participants. The combined national 30% subsidy and 30% tax (intervention 2b) had larger absolute benefits and similarly reduced disparities, preventing 11.5% of CHD deaths, 15.2% of stroke deaths, and 16.2% of diabetes deaths among SNAP participants (Table 3).
The combination of 10% national subsidy, 10% national tax, and 30% SNAP-targeted subsidy (intervention 3b) was estimated to reduce US CMD deaths by 10.2% for SNAP participants, 4.8% for SNAP-eligible non-participants, and 4.1% for SNAP-ineligible non-participants (Figure 1, Table S6), representing 37,500 deaths/y prevented nationally (Table S8). This intervention had the largest benefits on disparities, with 2 to 3 fold larger percentage reductions in proportional CMD mortality among SNAP participants, compared with SNAP-ineligible adults (Table 3).
DISCUSSION
We modeled, based on nationally representative datasets, the potential effects of specific food pricing interventions on national cardiometabolic mortality as well as disparities according to SNAP participation status. Our findings provide several new inferences. First, the potential effects of modest food taxes and subsidies on CMD mortality were large. A 10% national subsidy on 4 healthy food categories was estimated to reduce about 19,600 CMD deaths/y, or approximately 2.6% of all CMD deaths; while a 30% national subsidy generated a 7% reduction in CMD mortality. Adding a tax on SSBs and processed meats led to an approximate doubling of these national benefits. Second, national subsidies alone similarly benefited all groups, with negligible effects on disparities by SNAP participation and eligibility. In contrast, the addition of taxes was progressive for health, with the greatest benefits among SNAP participants due to both higher price-responsiveness and higher baseline intakes of these unhealthy foods. The addition of a targeted SNAP incentive led to the greatest reductions in disparities, with approximately 2 to 3 fold larger proportional reductions in CMD among SNAP participants compared with SNAP-ineligible adults.
Results of population interventions in Massachusetts,12–13 Minnesota,14 and Mexico6–7 support healthier dietary choices as a result of subsidies on healthier foods and taxes on less healthy foods. A recent analysis by our group used the US IMPACT model to compare the mortality effects of fruit and vegetable media health promotion campaigns vs. price policies on CVD mortality, finding that pricing policies had larger effects and were also more equitable for benefits by race.31 While assessment of cost and cost-effectiveness were beyond the scope of the present investigation, a recent cost-effectiveness analysis by Basu and colleagues estimated that, for SNAP participants, raising the price of SSBs would offer a substantial benefit for health and a net cost savings from lower healthcare utilization, while a produce subsidy would have more modest impacts.33 The six distinct policy interventions provide new evidence on an array of options with complementary tradeoffs between political feasibility, national mortality impact, and effects on disparities.
Our investigation has several strengths. Nationally representative datasets on dietary habits, CMD risk factors, and death rates provide generalizability to the US adult population. Our modeling accounted for differences for each population group in baseline dietary intake, baseline CMD mortality, and price-responsiveness, as well as differential proportional effects of dietary changes on CMD by age, each of which are relevant to the magnitude of estimated benefit. We accounted for smaller potential effects of SNAP-targeted pricing changes, as individuals receiving SNAP may also purchase foods with their own money outside the program. Our approach considered and jointly incorporated multiple sources of uncertainty, including in baseline food intake, price responsiveness, and associations of dietary changes with mortality.
Potential limitations and opportunities for future research should be considered. In these interventions, we modeled own-price responses of foods and not complements or substitutes. Yet, this is consistent with the evidence base used for etiologic effects of these food intake changes, which were derived from long-term longitudinal studies that implicitly account for the average long-term complements and substitutes when estimating health effects. For example, the estimated effect of SSB changes on BMI is much smaller than would be estimated based on the reduced calorie content from SSBs,22 reflecting the partial substitution of other caloric drinks or foods. Future research can evaluate how such average effects could be strengthened by complementary policy focus on specific complements or substitutes. The NHIS data on SNAP participation is for a single point in time. USDA data show that, for SNAP participants in any given month, half are in spells of 8 years or more.34 We used the best available evidence to estimate effects of dietary changes on CMD mortality, but did not forecast the dynamic time path of mortality change. We included both sampling variation (for NHANES intake data and mortality estimates) and non-sampling variation (in the UI for price elasticities and relative risks) in the reported UI estimates, but recognize potential additional uncertainty beyond what we could quantify. While every effort was made to maximize validity, minimize bias, and incorporate heterogeneity and uncertainty, our modeling findings cannot prove that these pricing strategies would reduce CMD. As with any intervention, our findings should be considered the average population effect; for any individual person, health effects could vary depending on other characteristics. We limited our investigation to 6 dietary factors with strongest evidence, not including many other dietary factors which may influence cardiometabolic health.
These results provide timely and important estimates of national impact on CMD mortality and disparities. They provide motivation for further pilot testing of price interventions in both the SNAP population and the general population. SSB taxes are being rapidly adopted by a growing number of municipalities, including Berkeley, Philadelphia, San Francisco, Boulder, and Seattle, among others.10 The SNAP Healthy Incentive Pilot (HIP)12–13 in Massachusetts has been followed by an independent pilot study that includes an SSB limitation,14 and also by additional fruit and vegetable incentives in local retail channels through USDA’s Food Insecurity Nutrition Incentives (FINI) pilots in selected locations. The Farm Bill, omnibus legislation that reauthorizes SNAP as well as crop insurance and farm subsidy programs, is expected to be revised in 2018. Our results suggest a need to consider how a suite of agricultural and food pricing policies, together with potential pricing disincentives rather than outright restrictions, can be best invested to help reduce prices of fruits, vegetables, nuts, and whole grains and increase prices of SSBs and processed meats in both SNAP and nationally.
Supplementary Material
SUMMARY BOX.
What is already known on this subject?
Coronary heart disease, stroke, and type 2 diabetes are major contributors to US mortality. They strike especially hard for low-income populations, including participants in the Supplemental Nutrition Assistance Program (SNAP). For prevention, there already has been great interest in using tax policy for sugar-sweetened beverages (SSBs). There also have been pilot demonstrations for using subsidy policy for fruits and vegetables for the SNAP population.
What does this study add?
Moving beyond just SSB taxes and SNAP subsidies, this study systematically analyzes the potential mortality reduction from a more comprehensive set of policy interventions for taxes (SSBs and processed meat) and price subsidies (fruits, vegetables, nuts, and whole grains) in three relevant populations (SNAP participants, SNAP-eligible non-participants, and SNAP-ineligible non-participants). It finds that combining general price policies for the full population with SNAP-targeted subsidies has the greatest simultaneous effect on reducing cardiometabolic disease mortality and disparities in mortality.
Acknowledgments
DM, MOF, JPS, and ZC conceived of this research project; ZC, FC, CDR, and PW conducted the quantitative analysis; CDR, ZC, JL Penalvo, and FC prepared the data for analysis; and PW, ZC, CDR, JL Penalvo, JL Pomeranz, FC, JPS, MOF, RM, and DM interpreted the results and wrote the manuscript.
FUNDING
This research was supported by the NIH, NHLBI (R01 HL130735, PI Micha; R01 HL115189, PI Mozaffarian).
Footnotes
COMPETING INTERESTS
Mozaffarian reports personal fees from Haas Avocado Board, Pollock Communications, Life Sciences Research Organization, Boston Heart Diagnostics, GOED, DSM, Unilever North American, and UpToDate. Micha reports research funding from Unilever and personal fees from the World Bank and Bunge, all outside the submitted work. Peñalvo now is employed by Merck KGaA. For all other authors: none declared.
LICENCE FOR PUBLICATION
The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive licence (or non exclusive for government employees) on a worldwide basis to the BMJ Publishing Group Ltd to permit this article (if accepted) to be published in JECH and any other BMJPGL products and sublicences such use and exploit all subsidiary rights, as set out in our licence (http://group.bmj.com/products/journals/instructions-for-authors/licence-forms).
Contributor Information
Parke Wilde, Friedman School of Nutrition Science and Policy, Tufts University, Boston, MA 02111, USA; parke.wilde@tufts.edu; 617-636-3495
Zach Conrad, Friedman School of Nutrition Science and Policy, Tufts University, Boston, MA 02111, USA
Colin D. Rehm, Office of Community and Population Health, Montefiore Medical Center, Bronx, NY 10467, USA
Jennifer L. Pomeranz, College of Global Public Health. New York University, New York, NY 10003, USA.
Jose L. Penalvo, Friedman School of Nutrition Science and Policy, Tufts University, Boston, MA 02111, USA
Frederick Cudhea, Friedman School of Nutrition Science and Policy, Tufts University, Boston, MA 02111, USA
Jonathan Pearson-Stuttard, School of Public Health, Imperial College London, UK; Department of Public Health and Policy, Liverpool University, Liverpool, UK.
Martin O’Flaherty, Department of Public Health and Policy, Liverpool University, Liverpool, UK
Renata Micha, Friedman School of Nutrition Science and Policy, Tufts University, Boston, MA 02111, USA
Dariush Mozaffarian, Friedman School of Nutrition Science and Policy, Tufts University, Boston, MA 02111, USA.
References
- 1.Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, de Ferranti SD, Floyd J, Fornage M, Gillespie C, Isasi CR, et al. Heart disease and stroke statistics—2017 update: A report from the American Heart Association. Circulation. 2017;135(10):e146–e603. doi: 10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.U. S. Burden of Disease Collaborators. The state of U.S. health, 1990–2010: Burden of diseases, injuries, and risk factors. JAMA. 2013;310:591–606. doi: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Global Burden of Disease Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1659–1724. doi: 10.1016/S0140-6736(16)31679-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. [Accessed April 23, 2017];Using price policies to promote healthier diets. 2015 http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/publications/2015/using-price-policies-to-promote-healthier-diets-2015.
- 5.Wada R, Han E, Powell LM. Associations between soda prices and intake: Evidence from 24-h dietary recall data. Food Policy. 2015;55:54–60. [Google Scholar]
- 6.Colchero MA, Popkin BM, Rivera JA, et al. Beverage purchases from stores in Mexico under the excise tax on sugar sweetened beverages: observational study. BMJ. 2016 Jan 6;352:h6704. doi: 10.1136/bmj.h6704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Colchero MA, Rivera-Dommarco J, Popkin BM, Ng SW. In Mexico, evidence of sustained consumer response two years after implementing a sugar-sweetened beverage tax. Health Affairs. 2017;36:3564–3571. doi: 10.1377/hlthaff.2016.1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Afshin A, Peñalvo JL, Del Gobbo L, Silva J, Michaelson M, O'Flaherty M, Capewell S, Spiegelman D, Danaei G, Mozaffarian D. The prospective impact of food pricing on improving dietary consumption: A systematic review and meta-analysis. PloS One. 2017;12(3):e0172277. doi: 10.1371/journal.pone.0172277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Powell LM, Chriqui JF, Khan T, Wada R, Chaloupka FJ. Assessing the potential effectiveness of food and beverage taxes and subsidies for improving public health: a systematic review of prices, demand and body weight outcomes. Obesity Reviews. 2013;14(2):110–128. doi: 10.1111/obr.12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Soda taxes spread after votes in four U.S. cities. [Accessed April 23, 2017];Reuters. 2016 Nov 9; http://www.reuters.com/article/us-usa-election-soda-tax-idUSKBN1341FL.
- 11.Dimitri C, Oberholtzer L. Potential National Economic Benefits of the Food Insecurity and Nutrition Incentives Program of the US Agricultural Act of 2014. Journal of Agriculture, Food Systems, and Community Development. 2016;5(4):49–61. [Google Scholar]
- 12.Olsho LE, Klerman JA, Wilde P, Bartlett S. Financial incentives increase fruit and vegetable intake among Supplemental Nutrition Assistance Program participants: A randomized controlled trial of the USDA Healthy Incentives Pilot. AJCN. 2016;104(2):423–435. doi: 10.3945/ajcn.115.129320. [DOI] [PubMed] [Google Scholar]
- 13.Wilde P, Klerman J, Olsho L, Bartlett S. Explaining contrasting measures of the food spending impact in USDA’s Healthy Incentives Pilot. Applied Economic Perspectives & Policy. 2015 Nov 30; doi: 10.1093/aepp/ppv028. online. [DOI] [Google Scholar]
- 14.Harnack L, Oakes JM, Elbel B, Beatty T, Rydell S, French S. Effects of subsidies and prohibitions on nutrition in a food benefit program: a randomized clinical trial. JAMA Internal Medicine. 2016;176(11):1610–1618. doi: 10.1001/jamainternmed.2016.5633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pomeranz JL, Chriqui JF. The Supplemental Nutrition Assistance Program: Analysis of program administration and food law definitions. Am J Prev Med. 2015;49:428–36. doi: 10.1016/j.amepre.2015.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.US Department of Agriculture, Food and Nutrition Service. [Accessed December 12, 2017];Supplemental Nutrition Assistance Program (SNAP) National Level Annual Summary. 2017 http://www.fns.usda.gov/pd/supplemental-nutrition-assistance-program-snap.
- 17.Mabli J, Ohls J. Supplemental Nutrition Assistance Program Participation is associated with an increase in household food security in a national evaluation. Journal of Nutrition. 2015;145:344–51. doi: 10.3945/jn.114.198697. [DOI] [PubMed] [Google Scholar]
- 18.Andreyeva T, Tripp AS, Schwartz MB. Dietary quality of Americans by Supplemental Nutrition Assistance Program participation status: A systematic review. Am J Prev Med. 2015;49:594–604. doi: 10.1016/j.amepre.2015.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Conrad Z, Rehm CD, Wilde P, Mozaffarian D. Cardiometabolic mortality by Supplemental Nutrition Assistance Program (SNAP) participation and eligibility in the United States. Am J Public Health. 2017;107(3):466–474. doi: 10.2105/AJPH.2016.303608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hawkes C, Jewell J, Allen K. A food policy package for healthy diets and the prevention of obesity and diet-related non-communicable diseases: the NOURISHING framework. Obesity Reviews. 2013;14(S2):159–168. doi: 10.1111/obr.12098. [DOI] [PubMed] [Google Scholar]
- 21.Sturm R, An R, Segal D, Patel D. A cash-back rebate program for healthy food purchases in South Africa: results from scanner data. Am J Prev Med. 2013;44(6):567–572. doi: 10.1016/j.amepre.2013.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Micha R, Peñalvo JL, Cudhea F, Imamura F, Rehm CD, Mozaffarian D. Association between dietary factors and mortality from heart disease, stroke, and type 2 diabetes in the United States. JAMA. 2017;317(9):912–924. doi: 10.1001/jama.2017.0947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rehm CD, Peñalvo JL, Afshin A, Mozaffarian D. Dietary Intake Among US Adults, 1999–2012. JAMA. 2016;315(23):2542–2553. doi: 10.1001/jama.2016.7491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.US Department of Health and Human Services, Centers for Disease Control and Prevention (CDC) [Accessed April 23, 2017];About the National Health and Nutrition Examination Survey. 2015 www.cdc.gov/nchs/nhanes.htm.
- 25.Singh GM, Micha R, Khatibzadeh S, Lim S, Ezzati M, Mozaffarian D. Estimated global, regional, and national disease burdens related to sugar-sweetened beverage consumption in 2010. Circulation. 2015 Jun 29; doi: 10.1161/CIRCULATIONAHA.114.010636. CIRCULATIONAHA-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.US Department of Health and Human Services, Centers for Disease Control and Prevention. [Accessed April 23, 2017];2000–2009. National Health Interview Survey. 2015 http://www.cdc.gov/nchs/nhis.htm.
- 27.US Department of Health and Human Services, Centers for Disease Control and Prevention. [Accessed April 23, 2017];2000–2009. US Death Certificates. 2015 http://wonder.cdc.gov/ucd-icd10.html.
- 28.US Census Bureau and US Bureau of Labor Statistics. [Accessed April 23, 2017];Current Population Survey: Poverty. 2015 http://www.census.gov/cps/data/
- 29.Green R, Cornelsen L, Dangour AD, Turner R, Shankar B, Mazzocchi M, Smith RD. The effect of rising food prices on food consumption: systematic review with meta-regression. BMJ. 2013;346:f3703. doi: 10.1136/bmj.f3703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Micha R, Shulkin ML, Peñalvo JL, Khatibzadeh S, Singh GM, Rao M, Fahimi S, Powles J, Mozaffarian D. Etiologic effects and optimal intakes of foods and nutrients for risk of cardiovascular diseases and diabetes: systematic reviews and meta-analyses from the Nutrition and Chronic Diseases Expert Group (NutriCoDE) PLoS One. 2017;12(4):e0175149. doi: 10.1371/journal.pone.0175149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pearson-Stuttard J, Bandosz P, Rehm CD, Whitsel L, et al. Reducing US cardiovascular disease burden and disparities through national and targeted dietary policies; a modelling study. PLoS Medicine. 2017;14(6):e1002311. doi: 10.1371/journal.pmed.1002311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pomeranz JL. Implications of the Supplemental Nutrition Assistance Program tax exemption on sugar-sweetened beverage taxes. American Journal of Public Health. 2015;105(11):2191–3. doi: 10.2105/AJPH.2015.302850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Basu S, Seligman HK, Gardner C, Bhattacharya J. Ending SNAP subsidies for sugar-sweetened beverages could reduce obesity and type 2 diabetes. Health Affairs. 2014 Jun 1;33(6):1032–9. doi: 10.1377/hlthaff.2013.1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Leftin J, Wemmerus N, Mabli J, Godfrey T, Tordella S. Prepared by Decision Demographics for the U.S. Department of Agriculture. Food and Nutrition Service; Alexandria, VA: 2014. Dynamics of SNAP Participation from 2008 to 2012. http://www.fns.usda.gov/research-and-analysis. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


