Abstract
Background
Mycoplasma genitalium is an important cause of bacterial sexually transmitted diseases. Diagnosis and susceptibility testing of Mycoplasma genitalium are limited by the fastidious nature of the organism. Therefore, the prevalence of infection and azithromycin resistance are poorly studied.
Methods
We conducted an exploratory study on remnant clinical specimens. We collected remnant DNA from consecutive urine samples and clinical swabs (cervical/vaginal, rectal, and pharyngeal) previously tested for Neisseria gonorrhoeae and Chlamydia trachomatis using the Cobas™ 4800 CT/NG assay (Roche Molecular Systems, Pleasanton, CA) between March–April 2017 from across the University of California, Los Angeles Health System. We then retrospectively tested all specimens with the ResistancePlus™ MG (550) kit, a molecular assay for the detection of Mycoplasma genitalium and genetic mutations associated with azithromycin resistance.
Results
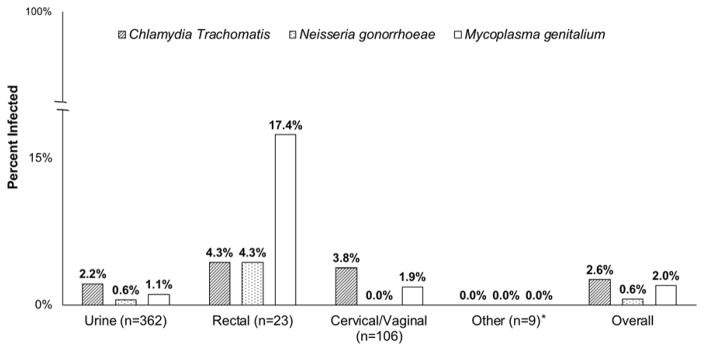
Among 500 specimens, the prevalence of Mycoplasma genitalium was 1.1% (95% CI 0.04%–3.0%) in urine samples (n=362), 17.4% (95% CI 5.7%–39.6%) in rectal swabs (n=23), and 1.9% (95% CI 0.3%–7.3%) in cervical/vaginal swabs (n=106). The prevalence of Neisseria gonorrhoeae was 0.6% in urine samples and 4.3% in rectal swabs, while the prevalence of Chlamydia trachomatis was 2.2% in urine samples, 4.3% in rectal swabs and 3.8% in cervical/vaginal swabs. Of the 10 Mycoplasma genitalium positive specimens, 8 (80.0%) had a mutation associated with azithromycin resistance.
Conclusion
The prevalence of Mycoplasma genitalium infection in our population varied by anatomic site of infection. Most Mycoplasma genitalium infections had at least one mutation associated with azithromycin resistance.
Introduction
Mycoplasma genitalium infections are increasingly recognized as an important cause of bacterial sexually transmitted diseases in the United States, however estimates of the infectious burden differ [1–10]. Prevalence estimates range from 1.0% among a screening population of adolescent men and women [1, 2] to as high as 16.3% and 17.2% among symptomatic and asymptomatic women and men, respectively [3]. All three of those studies included participants from across the United States. The prevalence of Mycoplasma genitalium has been reported to be as high as 22.4% among adolescent women from Cincinnati [4]. Several studies have found a higher prevalence of Mycoplasma genitalium infection than Trichomonas vaginalis, Neisseria gonorrhoeae, or Chlamydia trachomatis [5, 8, 10].
Mycoplasma genitalium infections have also been consistently associated with urethritis in men [11, 12] as well as cervicitis, pelvic inflammatory disease, and pre-term birth in women [12, 13]. Given those sequela of untreated or inadequately diagnosed infection, the emergence of antimicrobial resistance in Mycoplasma genitalium has caused concern [11]. From one study in the United States, the prevalence of macrolide resistance in men and women is estimated to be 50% and 42%, respectively [3]. A rapid assay for the simultaneous detection of Mycoplasma genitalium and mutations associated with azithromycin resistance has been developed [14, 15]. That assay is a single well rapid multiplex test detecting the pathogen Mycoplasma genitalium as well as the 5 most common mutations in the 23S rRNA gene (A2058G, A2059G, A2058T, A2058C, and A2059C, Escherichia coli numbering) associated antimicrobial resistance to azithromycin. The assay is compatible with multiple extraction platforms and real-time polymerase chain reaction machines. In a clinical study, that assay has been shown to have 98.5% sensitivity and 100.0% specificity for detection of Mycoplasma genitalium [15] as well as a 99.1% sensitivity and 98.5% specificity for detection of mutations associated with azithromycin resistance [14].
Evidence is lacking regarding the benefits of screening for Mycoplasma genitalium infection. In addition, there are currently no Food and Drug Administration approved assays for Mycoplasma genitalium. Furthermore, there are no current screening recommendations in the United States. However, the Centers for Disease Control and Prevention sexually transmitted diseases treatment guidelines added Mycoplasma genitalium infection as an emerging issue in 2015, and specify that Mycoplasma genitalium infection should be suspected in cases where urethritis is persistent or recurrent [11]. In order to further understand the prevalence of Mycoplasma genitalium infection, we aimed to characterize the infection prevalence as well as prevalence of mutations associated with azithromycin resistance at the University of California Los Angeles using a rapid genotypic assay.
Methods
For our exploratory study, we collected all remnant DNA from consecutive clinical specimens including urine samples, and urethral, vaginal, cervical, pharyngeal and rectal swab specimens submitted to the University of California Los Angeles Health System Clinical Microbiology Laboratory. Those specimens were submitted between March and April 2017 for standard of care Neisseria gonorrhoeae and Chlamydia trachomatis nucleic acid amplification testing. The University of California Los Angeles Health System is comprised of two hospitals, two emergency departments, and over 150 primary care clinics serving approximately 500,000 patient-visits each year.
The University of California Los Angeles Health System uses the Cobas™ 4800 CT/NG assay (Roche Molecular Systems, Pleasanton, CA, USA), which is used to extract and amplify Neisseria gonorrhoeae and Chlamydia trachomatis DNA from a clinical swab specimen. As part of routine clinical practice, internal Chlamydia trachomatis and Neisseria gonorrhoeae DNA controls were added to each individual sample well prior to the automated sample preparation, were amplified, and were detected simultaneously to monitor the entire process to ensure adequate DNA amplification. An individual sample in which the control was not within the specified range established was considered invalid. Additionally, the limit of Chlamydia trachomatis and Neisseria gonorrhoeae detection in different anatomical specimens ranges from 10–200 Elementary Bodies/mL and 0.2–3.0 Colony Forming Units/mL, respectively, per the Cobas™ 4800 CT/NG assay product insert. Although it is unknown if that translates to an equivalent level of detection for Mycoplasma genitalium, it was assumed that if there was sufficient bacterial DNA extracted (as evaluated by the internal control validation) the presence of Mycoplasma genitalium DNA would likely be detected by the sensitive assay described below. Remnant DNA specimens from the Cobas™ 4800 CT/NG assay were de-identified and stored at −20ºC for up to 22 days prior to subsequent testing.
DNA specimens were shipped to Australia in the same media in which they were extracted, and directly subjected to Mycoplasma genitalium testing as well as testing for mutations associated with azithromycin resistance using the ResistancePlus™ MG (550) kit (SpeeDx Pty. Ltd., Sydney, Australia) on the Applied Biosystems 7500 platform (Thermo Fisher Scientific, Waltham, MA, USA). A positive Mycoplasma genitalium control template was used to ensure DNA amplification was performing as expected. All Mycoplasma genitalium positive specimens were subjected to genotype sequencing using previously published primers [16]. Sanger sequencing was performed at Ramaciotti Centre for Genomics (University of New South Wales, Sydney, Australia). Of note, the ResistancePlus™ MG (550) kit has not been approved by the Food and Drug Administration in the United States, thus this research is a non-clinical investigational use of this assay.
We also gathered data on anatomic site of specimen collection, Neisseria gonorrhoeae and Chlamydia trachomatis nucleic acid amplification test results, and collection date. Specimens with incomplete data were not used in the analysis.
We then determined the prevalence of Mycoplasma genitalium infection as well as the frequency of mutations associated with azithromycin resistance. We also report the prevalence of infection and azithromycin resistance mutations by anatomic site from which the specimen was collected, as well as the 95% confidence intervals (CIs) for those proportions including a continuity correction. All analysis was performed using STATA software version 14.2 (College Station, TX, USA). The University of California Institutional Review Board determined that the testing of de-identified remnant clinical specimens and the review of de-identified data did not constitute human subjects’ research.
Results
We analyzed 500 specimens. The Figure shows the prevalence of infection by anatomic site. Overall 10 (2.0%; 95% CI 1.1% – 3.8%) samples tested positive for Mycoplasma genitalium. One (0.2%) of 500 specimens tested positive for both Neisseria gonorrhoeae and Chlamydia trachomatis. No Neisseria gonorrhoeae or Chlamydia trachomatis positive specimen tested positive for Mycoplasma genitalium DNA.
Figure.
Prevalence of Mycoplasma genitalium, Neisseria gonorrhoeae, and Chlamydia trachomatis infections among remnant DNA specimens collected from men and women undergoing testing for Neisseria gonorrhoeae and Chlamydia trachomatis.
By anatomic site, the prevalence of azithromcyin resistance among Mycoplasma genitalium positive specimens was 75% (rectal), 75% (urine), and 100% (cervix/vaginal).
* Includes 4 genital swabs from an unspecified anatomic site, 4 pharyngeal swabs, and 1 conjunctival swab
Of the 10 specimens that tested positive for Mycoplasma genitalium, 8 (80.0%; 95% CI 44.2% – 96.5%) had at least one mutation associated with azithromycin resistance by the ResistancePlus™ MG (550) kit. Of those, 3 (37.5%) were from urine samples, 3 (37.5%) were from rectal specimens, and 2 (25.0%) were from vaginal/cervical samples.
On genotype sequencing, all 8 specimens testing positive for a mutation by the ResistancePlus™ MG (550) kit were confirmed to have a mutation associated with azithromycin resistance (Table). The 2 remaining specimens that tested positive for Mycoplasma genitalium with no resistance mutation were unable to be sequenced.
Table.
The anatomic site of Mycoplasma genitalium infection and 23S rRNA gene mutation associated with azithromycin resistance.
| Specimen Number | Anatomic Site of Mycoplasma genitalium Infection | Specific 23S rRNA Mutation |
|---|---|---|
| 1 | Urine | A2059G |
| 2 | Rectal Swab | A2059G |
| 3 | Vaginal Swab | A2059G |
| 4 | Rectal Swab | A2059G |
| 5 | Cervical/Vaginal Swab | A2058G |
| 6 | Urine | A2058G |
| 7 | Urine | A2059G |
| 8 | Rectal Swab | A2058G |
Discussion
We report the prevalence of Mycoplasma genitalium infection among remnant DNA samples collected from persons being tested for Neisseria gonorrhoeae and Chlamydia trachomatis at the University of California Los Angeles Health System. We also report the prevalence of azithromycin resistance among those infections. The overall prevalence of infection is similar to past reports of Mycoplasma genitalium infection from the general population reported in the United States [1, 2]. However, the prevalence of Mycoplasma genitalium among populations at higher risk for sexually transmitted infections has been reported to be as high as 20.5% from a multicenter study in the United States [17]. Our prevalence estimates were lower for urethral [5] and cervical/vaginal [4, 8] infections than prior estimates. We also found a higher prevalence of rectal Mycoplasma genitalium infection than the 5% prevalence reported among men who have sex with men presenting to a sexually transmitted diseases clinic in San Francisco [18]. From that same study, the prevalence of rectal Trichomonas vaginalis was 1%, Neisseria gonorrhoeae was 11%, and Chlamydia trachomatis was 10%. A recent report found a higher prevalence of rectal Chlamydia trachomatis (21%) and Neisseria gonorrhoeae (40%) infections than rectal Mycoplasma genitalium infections (17%) among men who have sex with men [19]. The wide range of prevalence estimates in the literature likely reflects differing risk groups as well as different detection methods (e.g. polymerase chain reaction vs. transcription-mediated amplification) [2, 3, 5, 7, 17, 20].
The prevalence of resistance mutations among our population was concerning because azithromycin is the first line recommended treatment, and antibiotic selection is already limited [21]. Mycoplasma genitalium is not easily treated with tetracyclines [21]. Moxifloxacin has been shown to be effective against azithromycin-resistant strains of Mycoplasma genitalium [22], however concern for fluoroquinolone resistance and moxifloxacin treatment failure is increasing; one study reported cure in only 88% of macrolide-resistant Mycoplasma genitalium infections after treatment with moxifloxacin [23].
A previous study among the general population in the United States reported a 51% and 42% prevalence of azithromycin resistant Mycoplasma genitalium infections among women and men, respectively [3]. Notably, that study also reported a considerably higher prevalence of Mycoplasma genitalium infection overall than was found in other surveillance studies among the general population. Therefore, that population may be at a higher risk for sexually transmitted infections.
Worldwide, similar estimates of macrolide-resistant Mycoplasma genitalium infections have been reported. A Danish nationwide survey found a 38% prevalence of macrolide resistance among Mycoplasma genitalium infections in the general population, and a 43% prevalence of resistance among infections diagnosed at sexually transmitted diseases clinics [24]. A prior report from Australia using the same assay used in the present study demonstrated an 81% prevalence of azithromycin resistant Mycoplasma genitalium infections among men presenting to a sexual health center, with all rectal swabs testing positive for azithromycin resistance; the prevalence of azithromycin resistance mutations among women from the same population was 30% [15]. In Greenland, the prevalence of macrolide-resistant Mycoplasma genitalium infections may be as high as 100% in the general population [25].
The prevalence of Mycoplasma genitalium infection in our sample was comparable to the prevalence of Neisseria gonorrhoeae and Chlamydia trachomatis infections. Other studies have reported similar findings [1, 2], while some studies have even reported a higher prevalence of Mycoplasma genitalium compared to Trichomonas vaginalis, Neisseria gonorrhoeae, or Chlamydia trachomatis. One study reported a higher prevalence of Mycoplasma genitalium (17%) among men [3], another reported a higher prevalence of Mycoplasma genitalium among women with cervicitis (29%) [5], and another reported a higher prevalence of Mycoplasma genitalium (8%) compared to Neisseria gonorrhoeae or Chlamydia trachomatis among participants with symptoms of a sexually transmitted infection [8].
A high prevalence of infection is necessary but not a sufficient condition to support screening recommendations; other conditions must apply, such as demonstration that screening favorably improves prognosis. Further evidence is needed to support any recommendation for increased screening. Such research should aim to characterize the population at highest risk of infection, provide evidence of the benefits of screening, and document the risks of screening [26].
Beyond screening, however, testing of symptomatic patients for Mycoplasma genitalium infection has been hindered for many years because it is difficult to culture the bacteria. The introduction of molecular assays for the detection of infection and resistance mutations may facilitate earlier and more appropriate treatment. Molecular assays for the diagnosis of Mycoplasma genitalium have been developed [10, 14, 27]. Given the reported health consequence of untreated infection [12, 13], we advocate for including Mycoplasma genitalium testing in individuals with urethritis, as well as testing for azithromycin resistance among those that test positive for Mycoplasma genitalium.
The use of genotypic assays for guiding antimicrobial selection may reduce the selective pressure for antimicrobial resistance by improving antimicrobial stewardship [28]. Improved diagnostics for Mycoplasma genitalium infection and for determining antimicrobial susceptibility will be important for optimal clinical management. Several rapid molecular assays for the prediction of antimicrobial susceptibility have been developed for other organisms, and are used clinically to guide therapy for Mycobacterium tuberculosis [29], Staphylococcus aureus [30], carbapenem-resistant Enterobacteriaceae [31], and Neisseria gonorrhoeae [32]. All have been shown to be highly sensitive and specific.
Strengths and Limitations
One strength of our study was the use of consecutive remnant specimens, which reduces participation bias. Our study does have limitations, however. Primarily we did not perform confirmatory culture on the specimens that tested positive for Mycoplasma genitalium infection. Similarly, it was assumed that successful bacterial DNA extraction for Chlamydia trachomatis and Neisseria gonorrhoeae (as determined by the internal control) would result in sufficient Mycoplasma genitalium DNA extraction, however that assumption has not been validated and it is possible our results underestimate the prevalence of Mycoplasma genitalium infection. Additionally, the internal amplification controls for the Cobas™ 4800 do not control for adequate specimen collection. Furthermore, we were unable risk stratify our population as we performed analysis of only de-identified data and clinical or behavioral information was not available to us.
Conclusion
We report the prevalence of Mycoplasma genitalium infection and mutations associated with azithromycin resistance from consecutive remnant clinical samples collected from men and women at the University of California, Los Angeles being tested for Neisseria gonorrhoeae and Chlamydia trachomatis infection. The prevalence of Mycoplasma genitalium infection in our population varied by anatomic site of infection. The prevalence of mutations associated with azithromycin resistance in the specimens that tested positive for Mycoplasma genitalium was higher than expected. Those findings warrant further investigation into the prevalence of Mycoplasma genitalium infection and local azithromycin resistance rates.
Summary.
Using a molecular assay, we evaluated the prevalence of Mycoplasma genitalium infection and azithromycin-resistant infections among consecutive remnant specimens tested for Neisseria gonorrhoeae and Chlamydia trachomatis.
Acknowledgments
This research was supported by SpeeDx as well as the National Institutes of Health (NIH) grants: R21AI117256, and R21AI109005 and the South American Program in HIV Prevention Research NIH/NIMH R25MH087222.
Footnotes
Disclosure of Interest Statement:
Elisa Mokany and Rachel Wee are employees of SpeeDx and SpeeDx manufactures and sell the ResistancePlus™ MG (550) kit provided for this study, which is not available for sale in the USA. The other authors have no conflicts of interest.
References
- 1.Buffardi AL, Thomas KK, Holmes KK, et al. Moving upstream: ecosocial and psychosocial correlates of sexually transmitted infections among young adults in the United States. Am J Public Health. 2008;98(6):1128–36. doi: 10.2105/AJPH.2007.120451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Manhart LE, Holmes KK, Hughes JP, et al. Mycoplasma genitalium among young adults in the United States: an emerging sexually transmitted infection. Am J Public Health. 2007;97(6):1118–25. doi: 10.2105/AJPH.2005.074062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Getman D, Jiang A, O’Donnell M, et al. Mycoplasma genitalium Prevalence, Coinfection, and Macrolide Antibiotic Resistance Frequency in a Multicenter Clinical Study Cohort in the United States. J Clin Microbiol. 2016;54(9):2278–83. doi: 10.1128/JCM.01053-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huppert JS, Mortensen JE, Reed JL, et al. Mycoplasma genitalium detected by transcription-mediated amplification is associated with Chlamydia trachomatis in adolescent women. Sex Transm Dis. 2008;35(3):250–4. doi: 10.1097/OLQ.0b013e31815abac6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gaydos C, Maldeis NE, Hardick A, et al. Mycoplasma genitalium compared to chlamydia, gonorrhoea and trichomonas as an aetiological agent of urethritis in men attending STD clinics. Sex Transm Infect. 2009;85(6):438–40. doi: 10.1136/sti.2008.035477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dehon PM, Hagensee ME, Sutton KJ, et al. Histological Evidence of Chronic Mycoplasma genitalium-Induced Cervicitis in HIV-Infected Women: A Retrospective Cohort Study. J Infect Dis. 2016;213(11):1828–35. doi: 10.1093/infdis/jiw025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wroblewski JK, Manhart LE, Dickey KA, et al. Comparison of transcription-mediated amplification and PCR assay results for various genital specimen types for detection of Mycoplasma genitalium. J Clin Microbiol. 2006;44(9):3306–12. doi: 10.1128/JCM.00553-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hancock EB, Manhart LE, Nelson SJ, et al. Comprehensive assessment of sociodemographic and behavioral risk factors for Mycoplasma genitalium infection in women. Sex Transm Dis. 2010;37(12):777–83. doi: 10.1097/OLQ.0b013e3181e8087e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thurman AR, Musatovova O, Perdue S, et al. Mycoplasma genitalium symptoms, concordance and treatment in high-risk sexual dyads. Int J STD AIDS. 2010;21(3):177–83. doi: 10.1258/ijsa.2009.008485. [DOI] [PubMed] [Google Scholar]
- 10.Munson E, Bykowski H, Munson KL, et al. Clinical Laboratory Assessment of Mycoplasma genitalium Transcription-Mediated Amplification Using Primary Female Urogenital Specimens. J Clin Microbiol. 2016;54(2):432–8. doi: 10.1128/JCM.02463-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Workowski KA, Bolan GA Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015;64(RR-03):1–137. [PMC free article] [PubMed] [Google Scholar]
- 12.Anagrius C, Lore B, Jensen JS. Mycoplasma genitalium: prevalence, clinical significance, and transmission. Sex Transm Infect. 2005;81(6):458–62. doi: 10.1136/sti.2004.012062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lis R, Rowhani-Rahbar A, Manhart LE. Mycoplasma genitalium infection and female reproductive tract disease: a meta-analysis. Clin Infect Dis. 2015;61(3):418–26. doi: 10.1093/cid/civ312. [DOI] [PubMed] [Google Scholar]
- 14.Tabrizi SN, Tan LY, Walker S, et al. Multiplex Assay for Simultaneous Detection of Mycoplasma genitalium and Macrolide Resistance Using PlexZyme and PlexPrime Technology. PLoS One. 2016;11(6):e0156740. doi: 10.1371/journal.pone.0156740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tabrizi SN, Su J, Bradshaw CS, et al. Prospective Evaluation of ResistancePlus MG, a New Multiplex Quantitative PCR Assay for Detection of Mycoplasma genitalium and Macrolide Resistance. J Clin Microbiol. 2017;55(6):1915–1919. doi: 10.1128/JCM.02312-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jensen JS, Bradshaw CS, Tabrizi SN, et al. Azithromycin treatment failure in Mycoplasma genitalium-positive patients with nongonococcal urethritis is associated with induced macrolide resistance. Clin Infect Dis. 2008;47(12):1546–53. doi: 10.1086/593188. [DOI] [PubMed] [Google Scholar]
- 17.Seña AC, Lee JY, Schwebke J, Philip SS, Wiesenfeld HC, Rompalo AM, Cook RL, Hobbs MM. A silent epidemic: the prevalence, incidence and persistence of Mycoplasma genitalium among young, asymptomatic high-risk women in the United States. Clin Infect Dis. 2018 doi: 10.1093/cid/ciy025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Francis SC, Kent CK, Klausner JD, et al. Prevalence of rectal Trichomonas vaginalis and Mycoplasma genitalium in male patients at the San Francisco STD clinic, 2005–2006. Sex Transm Dis. 2008;35(9):797–800. doi: 10.1097/OLQ.0b013e318177ec39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ong JJ, Aung E, Read TRH, et al. Clinical characteristics of anorectal Mycoplasma genitalium infection and microbial cure in men who have sex with men. Sex Transm Dis. 2018 doi: 10.1097/OLQ.0000000000000793. Published ahead of print. [DOI] [PubMed] [Google Scholar]
- 20.Wetmore CM, Manhart LE, Lowens MS, et al. Demographic, behavioral, and clinical characteristics of men with nongonococcal urethritis differ by etiology: a case-comparison study. Sex Transm Dis. 2011;38(3):180–6. doi: 10.1097/OLQ.0b013e3182040de9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Couldwell DL, Lewis DA. Mycoplasma genitalium infection: current treatment options, therapeutic failure, and resistance-associated mutations. Infect Drug Resist. 2015;8:147–61. doi: 10.2147/IDR.S48813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bradshaw CS, Chen MY, Fairley CK. Persistence of Mycoplasma genitalium following azithromycin therapy. PLoS One. 2008;3(11):e3618. doi: 10.1371/journal.pone.0003618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bissessor M, Tabrizi SN, Twin J, et al. Macrolide resistance and azithromycin failure in a Mycoplasma genitalium-infected cohort and response of azithromycin failures to alternative antibiotic regimens. Clin Infect Dis. 2015;60(8):1228–36. doi: 10.1093/cid/ciu1162. [DOI] [PubMed] [Google Scholar]
- 24.Salado-Rasmussen K, Jensen JS. Mycoplasma genitalium testing pattern and macrolide resistance: a Danish nationwide retrospective survey. Clin Infect Dis. 2014;59(1):24–30. doi: 10.1093/cid/ciu217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gesink DC, Mulvad G, Montgomery-Andersen R, et al. Mycoplasma genitalium presence, resistance and epidemiology in Greenland. Int J Circumpolar Health. 2012;71:1–8. doi: 10.3402/ijch.v71i0.18203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Strong K, Wald N, Miller A, et al. Current concepts in screening for noncommunicable disease: World Health Organization Consultation Group Report on methodology of noncommunicable disease screening. J Med Screen. 2005;12(1):12–9. doi: 10.1258/0969141053279086. [DOI] [PubMed] [Google Scholar]
- 27.Tabrizi SN, Costa AM, Su J, et al. Evaluation of the Hologic Panther Transcription-Mediated Amplification Assay for Detection of Mycoplasma genitalium. J Clin Microbiol. 2016;54(8):2201–3. doi: 10.1128/JCM.01038-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee CR, I, Cho H, Jeong BC, et al. Strategies to minimize antibiotic resistance. Int J Environ Res Public Health. 2013;10(9):4274–305. doi: 10.3390/ijerph10094274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Boehme CC, Nabeta P, Hillemann D, et al. Rapid molecular detection of tuberculosis and rifampin resistance. N Engl J Med. 2010;363(11):1005–15. doi: 10.1056/NEJMoa0907847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim JU, Cha CH, An HK, et al. Multiplex real-time PCR assay for detection of methicillin-resistant Staphylococcus aureus (MRSA) strains suitable in regions of high MRSA endemicity. J Clin Microbiol. 2013;51(3):1008–13. doi: 10.1128/JCM.02495-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Miller S, Humphries RM. Clinical laboratory detection of carbapenem-resistant and carbapenemase-producing Enterobacteriaceae. Expert Rev Anti Infect Ther. 2016;14(8):705–17. doi: 10.1080/14787210.2016.1206815. [DOI] [PubMed] [Google Scholar]
- 32.Allan-Blitz LT, Humphries RM, Hemarajata P, et al. Implementation of a Rapid Genotypic Assay to Promote Targeted Ciprofloxacin Therapy of Neisseria gonorrhoeae in a Large Health System. Clin Infect Dis. 2017;64(9):1268–1270. doi: 10.1093/cid/ciw864. [DOI] [PMC free article] [PubMed] [Google Scholar]