Abstract
Among 307 patients enrolled in an HIV pre-exposure prophylaxis (PrEP) program in the Public Health – Seattle & King County STD Clinic, 52 patients (17%) did not fill their PrEP prescription and 40% of those who started PrEP discontinued it at least once within 12 months.
Keywords: Human Immunodeficiency Virus, Pre-Exposure Prophylaxis, Patient Engagement, Sexually Transmitted Diseases
INTRODUCTION
Sexually transmitted disease (STD) clinics are key venues for linking patients to HIV pre-exposure prophylaxis (PrEP)1 and diminishing disparities in access to PrEP. Many patients seen in STD clinics are at risk for HIV infection, and these clinics provide care to patients who are disproportionately Black, young, and uninsured.2,3 The effectiveness of PrEP depends on patient adherence to the medication, and some reports indicate that patient retention in PrEP care may be suboptimal.4,5 Since PrEP provision in many STD clinics is relatively new, the focus of reports on STD Clinic PrEP programs to date has been on patient interest in and initiation of PrEP.6,7 Less is known about ongoing engagement in PrEP care. The objective of our study was to evaluate patient disengagement from the PrEP program at the Public Health – Seattle & King County (PHSKC) STD Clinic.
METHODS
The PHSKC PrEP program is integrated with STD clinic operations and provides PrEP to men who have sex with men (MSM) and transgender individuals who have sex with men (TGSM) at high risk for HIV according to King County and Washington State PrEP implementation guidelines.8 This includes patients who have had rectal gonorrhea or syphilis, used methamphetamine or amyl nitrates, or provided sex for money or drugs in the last 12 months and patients in sexual relationships with HIV-infected persons who are not virally suppressed. In 2017, with the goal of improving equity in access to PrEP, the program expanded to provide PrEP to all interested Black and Latino MSM or TGSM. STD clinicians and disease intervention specialists (DIS) refer patients who are interested in PrEP but do not meet the criteria above to other providers in the community. PrEP is widely available in King County, and uptake is relatively high.9
All clinicians in the PHSKC STD Clinic can prescribe PrEP, and the goal is to provide a same-day prescription. Two DIS coordinate the program, assist patients with enrollment in payment assistance programs, schedule follow-up appointments at the time of each visit, and attempt to contact and reschedule all patients who miss appointments. After enrollment, patients follow-up in clinic at 1 month then every 3 months with DIS. Clinicians see patients every 6 months or as needed. Patients who enroll in a text message support program receive automated appointment reminders, monthly two-way check-in messages, and the opportunity to initiate two-way text communication with the coordinators. Enrollment in the text message program is associated with retention in the PrEP program.10
We conducted a retrospective cohort analysis of MSM who completed at least one PrEP encounter during October 2014 – December 2016. The PrEP coordinators record patient information in an electronic database, including the medication start date (verified pharmacy pick-up date), dates of completed appointments, and the status of PrEP use at each visit (continuing, stopped, restarted). When a patient reports discontinuing PrEP, either during or between visits, the DIS record the patient-reported discontinuation date and reason for discontinuation. DIS ask about discontinuation reasons with an open-ended question and code the reason in the database according to defined categories or, for reasons not included in the list, in a free text field. Patients who do not complete a scheduled follow-up visit and do not respond to 3 calls or text messages are classified as lost to follow-up.
For this analysis, we defined patient disengagement as either failure to start PrEP after enrolling, discontinuation of PrEP after initiation, or loss to follow-up. We excluded patients known to have moved away or transferred care since we could not determine the status of PrEP continuation. We determined the percentage of patients who disengaged and assessed the timing of discontinuation with a Kaplan-Meier analysis. We examined differences by race/ethnicity and age in the prevalence of and reasons for disengagement (chi-square tests) and the timing of discontinuation (log-rank test). To assess the extent to which patients in the PrEP program represent those at risk for HIV, we compared PrEP patients to MSM newly diagnosed with HIV in King County 2011–201511 using a chi-square test for race/ethnicity and t-test for age.
RESULTS
During the 27 month analysis period, 334 MSM enrolled in the PrEP program. The race/ethnicity of PrEP patients differed from the population of newly diagnosed MSM in King County in 2011–2015 (N=925), with a higher proportion of Hispanic patients in the PrEP program (24% vs. 15%; p<0.001), but lower proportions of non-Hispanic Black persons (8% vs. 12%, p=0.048) and non-Hispanic White persons (52% vs. 62%; p<0.001). PrEP patients were younger than the newly HIV-diagnosed (mean age 29; standard deviation (SD) 9 years vs. 36 (SD, 11) years; p value<0.001).
Twenty-seven men moved or transferred care (Figure 1). Among the 307 men in the analysis population, the median observation time was 12 months [interquartile range (IQR): 6–18 months]. A total of 133 men (N=43%) disengaged from the PrEP program: 52 (17% of the overall population) never started PrEP and 81 (32% of those who started PrEP; 26% of the overall population) discontinued after starting. The timing of PrEP discontinuation was relatively steady throughout the observation period (Figure 2), with 40% discontinuing at least once by 12 months. Neither discontinuation, non-initiation, nor the timing of discontinuation was associated with race/ethnicity or age (data not shown).
Figure 1.
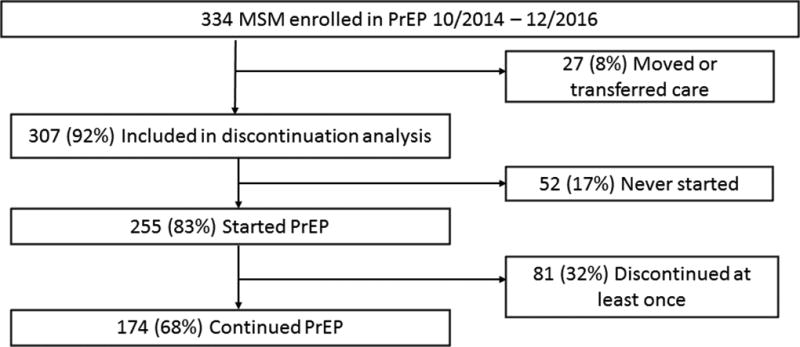
Flow Chart of Patients in the STD Clinic PrEP Program
Figure 2.
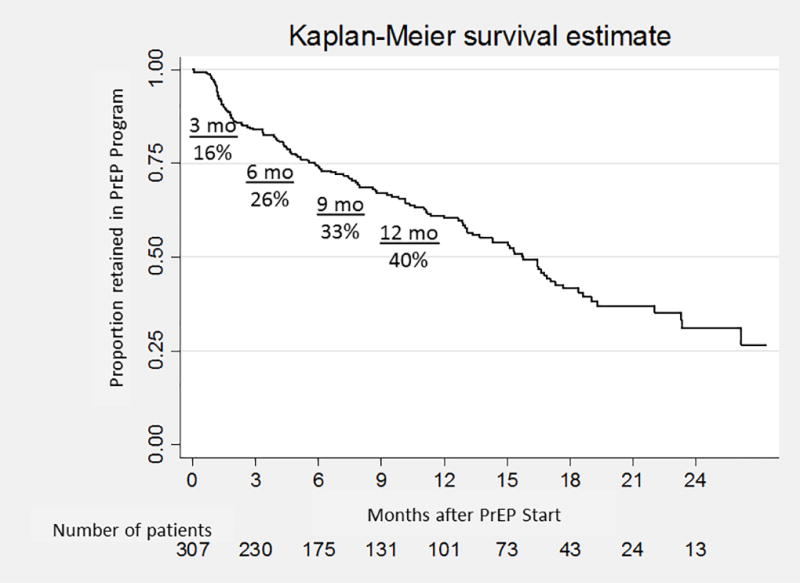
Timing of Patient Disengagement from the STD Clinic PrEP Program (N=307)
We were unable to determine patients’ reasons for discontinuing because most who did so were lost to follow-up (N=41), recorded as discontinuing for unknown reasons (N=5) or were missing information (N=7). Of the 28 patients with complete data, 13 (46%) discontinued because they were in a monogamous relationship with an HIV-seronegative partner, 4 (14%) stated they were otherwise no longer at risk for HIV, and 11 (39%) discontinued due to side effects. Reasons for discontinuation did not vary by race/ethnicity or age (data not shown).
DISCUSSION
We found that among 307 MSM in the PrEP program, 17% never filled their prescription, and 40% of those who started PrEP discontinued it at least once within 12 months. Our finding of 17% non-initiation was similar to Chan and colleagues’ report of 19% non-initiation among persons prescribed PrEP in 3 U.S. cities.5 Our finding of 40% discontinuation in 12 months was similar to recent reports from San Francisco community-based sexual health clinics (38% discontinuation in 13 months),4 and publicly-funded safety net clinics (33% discontinuation at a mean of approximately 8 months),12 but somewhat higher than that reported from a pharmacy-based program in Seattle (25% in 1 year),13 an online survey of MSM in Washington State (20% in 1 year),14 and an integrated health system in California (23% in 9 months).15 Higher discontinuation rates among STD clinic patients might reflect a higher risk patient population or, at least in our clinic, promotion of PrEP to persons who did not come to clinic specifically seeking PrEP and are ambivalent about it.
The generalizability of our study is limited because it included only one clinic recruiting high-risk patients. We could not determine the reasons for disengagement for most patients due to loss to follow-up, and we did not independently assess ongoing risk among patients who reported they were no longer at risk for HIV. The prevalence of treatment-limiting side effects in our analysis is difficult to interpret in the context of missing data on those lost to follow-up.
Our study suggests that patient retention in STD clinic PrEP programs is suboptimal, but without more information about why patients stop taking PrEP, this is uncertain. Discontinuation is appropriate for patients who are no longer at risk for HIV, but patients may not accurately perceive their risk. Available data suggest that at least some portion of discontinuation is not attributable to decreased risk. Patients with STDs4 and drug or alcohol use15 are less likely to stay on PrEP, and both younger age7 and Black race12 are associated with drop-off of the PrEP care continuum. A better understanding of the relative contributions of health systems and patient factors to PrEP discontinuation is needed to inform the development of interventions to support patient PrEP engagement.
SUMMARY.
This study describes patient failure to start HIV pre-exposure prophylaxis (PrEP), medication discontinuation, and loss to follow-up among patients enrolled in a sexually transmitted disease Clinic-based PrEP program.
Acknowledgments
Sources of Funding: This work was supported by the University of Washington Center for AIDS Research (CFAR), an NIH funded program under award number P30AI027757 which is supported by the following NIH Institutes and Centers (NIAID, NCI, NIMH, NIDA, NICHD, NHLBI, NIA, NIGMS, NIDDK). JCD has conducted research unrelated to this work supported by grants to the UW from the following companies: Hologic, Genentech, Curatek, ELITech and Quidel. JCD received a speaker’s honorarium and travel support from Gilead for meetings on retention in HIV care.
The authors acknowledge the crucial contributions of Cheryl Malinski, Glorya Afful, Mike Barry, Dawn Spellman, Negusse Ocbamichael, and Susannah Herrmann to the PHSKC PrEP program, the contributions of John Diemer to the PrEP data management system, and the WelTel team led by Dr. Richard Lester for collaboration on the two-way text message system used in the PrEP program.
Footnotes
Conflicts of Interest: All other authors report no conflicts of interest.
Note: These findings were presented in part at the World STI Congress & HIV Congress 2017, Rio de Janiero, Brazil, July 9–12, 2017.
References
- 1.Hoover KW, Ham DC, Peters PJ, Smith DK, Bernstein KT. Human immunodeficiency virus prevention with preexposure prophylaxis in sexually transmitted disease clinics. Sex Transm Dis. 2016;43(5):277–282. doi: 10.1097/OLQ.0000000000000441. [DOI] [PubMed] [Google Scholar]
- 2.Pathela P, Klingler EJ, Guerry SL, et al. Sexually transmitted infection clinics as safety net providers: exploring the role of categorical sexually transmitted infection clinics in an era of health care reform. Sex Transm Dis. 2015;42(5):286–293. doi: 10.1097/OLQ.0000000000000255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hoover KW, Parsell BW, Leichliter JS, et al. Continuing need for sexually transmitted disease clinics after the affordable care act. Am J Public Health. 2015;105(Suppl 5):S690–695. doi: 10.2105/AJPH.2015.302839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hojilla JC, Vlahov D, Crouch PC, Dawson-Rose C, Freeborn K, Carrico A. HIV pre-exposure prophylaxis (PrEP) uptake and retention among men who have sex with men in a community-based sexual health clinic. AIDS Behav. 2017 doi: 10.1007/s10461-017-2009-x. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chan PA, Mena L, Patel R, et al. Retention in care outcomes for HIV pre-exposure prophylaxis implementation programmes among men who have sex with men in three US cities. J Int AIDS Soc. 2016;19(1):20903. doi: 10.7448/IAS.19.1.20903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chan PA, Glynn TR, Oldenburg CE, et al. Implementation of preexposure prophylaxis for human immunodeficiency virus prevention among men who have sex with men at a New England sexually transmitted diseases clinic. Sex Transm Dis. 2016;43(11):717–723. doi: 10.1097/OLQ.0000000000000514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhatia R, Modali L, Lowther M, et al. Outcomes of preexposure prophylaxis referrals from public STI clinics and implications for the preexposure prophylaxis continuum. Sex Transm Dis. 2018;45(1):50–55. doi: 10.1097/OLQ.0000000000000690. [DOI] [PubMed] [Google Scholar]
- 8.Golden MR, Lindquist S, Dombrowski JC. Public Health-Seattle & King County and Washington State Department of Health preexposure prophylaxis implementation guidelines, 2015. Sex Transm Dis. 2016;43(4):264–265. doi: 10.1097/OLQ.0000000000000427. [DOI] [PubMed] [Google Scholar]
- 9.Hood JE, Buskin SE, Dombrowski JC, et al. Dramatic increase in preexposure prophylaxis use among MSM in Washington state. AIDS. 2016;30(3):515–519. doi: 10.1097/QAD.0000000000000937. [DOI] [PubMed] [Google Scholar]
- 10.Khosropour CM, Lester RT, Golden MR, Dombrowski JC. Text messaging is associated with improved retention in a clinic-based PrEP program; Presented at: The Conference on Retroviruses and Opportunistic Infections [abstract 964]; 2017; Seattle, Washington. [Google Scholar]
- 11.HIV/AIDS Epidemiology Unit, Public Health - Seattle & King County and the Infectious Disease Assessment Unit, Washington State Department of Health. HIV/AIDS Epidemiology Report. 2016 [Google Scholar]
- 12.Scott H, Nordell M, Hirozawa A, et al. Racial/ethnic disparities in persistence among PrEP users in San Francisco; Presented at: The Conference on Retroviruses and Opportunistic Infections [abstract 974]; 2017; Seattle, Washington. [Google Scholar]
- 13.Tung E, Thomas A, Eichner A, Shalit P. Feasibility of a pharmacist-run HIV PrEP clinic in a community pharmacy setting; Presented at: The Conference on Retroviruses and Opportunistic Infections [abstract 961]; 2017; Seattle, Washington. [Google Scholar]
- 14.Rao DW, Carr J, Naismith K, et al. Monitoring PrEP use among Washington State MSM: results of an internet survey; Presented at: The Conference on Retroviruses and Opportunistic Infections [poster 243]; 2018; Boston, Massachusetts. [Google Scholar]
- 15.Marcus JL, Hurley LB, Hare CB, et al. Preexposure prophylaxis for HIV prevention in a large integrated health care system: adherence, renal safety, and discontinuation. J Acquir Immune Defic Syndr. 2016;73(5):540–546. doi: 10.1097/QAI.0000000000001129. [DOI] [PMC free article] [PubMed] [Google Scholar]


