Abstract
Background
Living with a left ventricular assist device (LVAD) has significant psychosocial sequelae that impact health related quality of life (HRQOL).
Objective
The purpose of this study was to 1) describe psychosocial indicators of stress including perceived stress, depression, fatigue and coping 2) examine relationships among stress indicators by level of perceived stress 3) examine relationships among indicators of stress and clinical outcomes and 4) test the moderation of social support on the relationship between stress and clinical outcomes.
Methods
Participants were recruited from two outpatient clinics in a cross-sectional study design. Standardized measures were self-administered via survey. Descriptive statistics, correlation and multiple linear regression analysis were done.
Results
The sample (N=62) was mostly male (78%), black (47%), married (66%), with mean age 56.5± 13 years. The overall sample had a moderate stress profile: moderate perceived stress (mean 11.7 ± 7), few depressive symptoms (mean 3.2 ± 3.9) and moderate fatigue (mean 14.3 ± 9.1). Increased perceived stress was associated with fatigue, depressive symptoms and maladaptive coping (p< 0.001). Regression analysis demonstrated perceived stress and fatigue were significant correlates of overall HRQOL (adj. R2=0.41, p < 0.0001). Social support moderated the relationship between perceived stress and HRQOL, controlling for fatigue (R2 = 0.49, p < 0.001).
Conclusions
Individuals living with LVAD with high perceived stress have worse depressive symptoms, fatigue and coping. The influence of high social support to improve the relationship between stress and HRQOL underscores the importance of a comprehensive plan to address psychosocial factors.
Living with advanced heart failure (HF) and a left ventricular assist device (LVAD) is complex, stressful and commonly burdensome.1 The number of individuals living with a LVAD is increasing, underscoring the importance of examining psychological as well as physiological and clinical outcomes such as health-related quality of life (HRQOL), exercise capacity and healthcare utilization.2 Emotional and psychological sequelae occur due to challenges of LVAD self-care (e.g., adapting to dependence on a power source and manipulation of the device), impaired sleep, pain, limitations on activities of daily living and management of complex medication regimens.3
Stress has been defined as the experience of appraising events as threatening, due to exceeding personal resources.4 Psychological stress response may be characterized by perceived stress, depressive symptoms and fatigue due to common causal pathways.5,6 Although little is known about the psychological stress experienced by LVAD patients, perceived stress and depression have been associated with poor health outcomes among cardiac patients.7,8 In a study by Arnold et al comparing cardiac patients by level of perceived stress, those with higher perceived stress had worse 2-year mortality compared to those with low perceived stress even after controlling for clinical factors such as depression.7 Perceived stress and the relationship between stress and outcomes has not been studied among patients living with an LVAD.
Coping, the cognitive and behavioral efforts to respond to stressful events and chronic stress can take adaptive and maladaptive forms.4 Maladaptive coping strategies, such as denial and avoidance, are associated with worse outcomes in HF patients.9 One important adaptive coping strategy evaluated by transplant committees is social support. Typically, LVAD patients must have caregivers, identified prior to implantation; however, the caregiver-patient relationship, demonstrated in qualitative studies, can be strained by changes in levels of independence, roles and relationships. 3,10,11 Higher levels of social support have been associated with better outcomes including HRQOL and HF self-care in HF studies, but have not been studied among LVAD patients.12,13
To our knowledge, no studies to date have taken a comprehensive view of psychological indicators of stress, nor related these indicators to social support and outcomes. Therefore, the purpose of this study was to describe and examine the relationships between indicators of psychological stress, coping, social support and clinical outcomes including HRQOL, exercise capacity, and healthcare utilization. Our aims were to 1) Describe indicators of psychological stress among LVAD patients 2) Compare indicators of stress, social support and outcomes by level of perceived stress 3) Examine the relationships between indicators of psychological stress response and outcomes and 4) Test the role of social support as a moderator of the relationships between psychological stress response and outcomes.
METHODS
Study Design
A cross-sectional study design was used to describe indicators of psychological stress, coping, social support and outcomes among patients living with an LVAD. The conceptual framework for this study is an adaptation of the Lazarus and Folkman Stress Model (see figure 1).4 Poor outcomes result from the inability to respond to the demands of stress. In this conceptual framework, individual characteristics of LVAD patients (i.e., implant strategy, emergent implantation, time since implant, stressful life events) influence indicators of psychological stress response (i.e., perceived stress, depressive symptoms, fatigue and coping). In particular, we wanted to examine the relationships between perceived stress and other indicators of psychological stress response. Psychological stress response is related to LVAD patient outcomes (i.e., HRQOL, exercise capacity and healthcare utilization). Based on the literature and clinical experience of the investigators, we hypothesized that social support would moderate the relationship between indicators of psychological stress and outcomes.12–14
Figure 1.
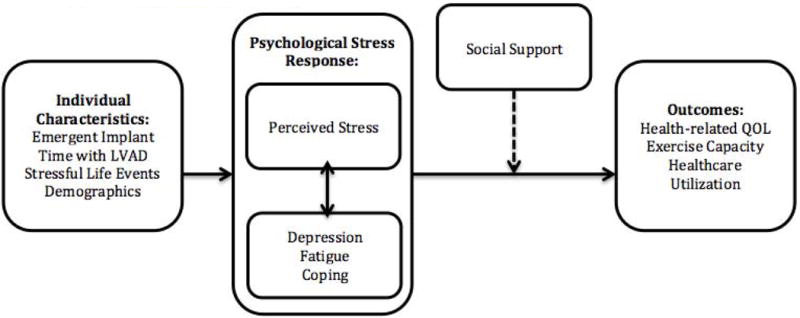
Conceptual Framework
Setting & Sampling
Patients living with an LVAD and served by the LVAD clinic at two large tertiary care centers in the mid-Atlantic region of the United States were included in the study. Convenience sampling was used to recruit patients living with an LVAD from both centers. Institutional Review Board approval was obtained and informed consent was obtained in person during clinic visits. We recruited outpatients with an LVAD at >2 months post-implant. The timing of recruitment was based on an understanding that early surgical recovery is very stressful with functional and HRQOL improvements that change rapidly.15 Eligibility criteria included: patients with continuous flow LVAD treated in outpatient clinic, over 21 years of age, had a Montreal Cognitive Assessment (MoCA) score ≥17 (no severe cognitive impairment)16 and could speak and understand English. Patients were excluded if being treated in inpatient rehabilitation or acutely hospitalized with the assumption that stress during inpatient stays would be different than outpatient stress.
Sample Size
A power analysis was conducted to determine the sample size needed based on co-variates in the model and estimated effect sizes. Because of the limited literature demonstrating relationships between our key variables in this population, we used a small effect size (f2=0.2) in our calculations .17–19 Based on the power analysis for linear regression, an estimated effect size of f2=0.2, α=0.05, and power of 80%, we planned to recruit 80 patients.
Study Procedures and Measurement
Patients were recruited on scheduled clinic visit days. Surveys were administered on paper and collected at the end of the visit if completed, but often were completed at a subsequent clinic visit. Demographic characteristics and instruments assessing study variables were self-administered. Widely validated instruments were selected based on their use with HF populations and relevance to the conceptual model for the variables of interest (Table 1).
Table 1.
Instrument Description
| Variable Instrument | # Items Sub-scales | Scoring: Score range, Significance of high score, Diagnostic cutoffs |
|---|---|---|
|
Stressful Life Events Holmes and Rahe Stressful Life Events Scale33,34 |
43 Total Weighted Score |
0 - 450 Higher total weighted score indicates higher stress. Scores >150 are associated with higher health risk. |
|
Perceived Stress Perceived Stress Scale24 |
10 Total Score |
0 – 40 Higher score indicates worse stress No diagnostic cutoff |
|
Depressive symptoms Perceived Health Questionnaire35 |
9 Total Score |
0 - 25 Higher score indicates worse depressive symptoms 5 = mild, 10 = moderate depressive symptoms |
|
Fatigue Multidimensional Assessment of Fatigue36 |
16 Global Fatigue Index |
1 – 50 A higher score indicates worse fatigue and impact on activities of daily living. |
|
Coping Brief COPE37 |
28 Adaptive Coping: (task-focused, seeks social support, religion & acceptance) Maladaptive Coping: (behavioral disengagement, substance abuse & self-blame) |
Adaptive Coping: 0 - 64 Maladaptive coping: 0 - 48 Higher Score indicates more frequent use of more strategies. No diagnostic cutoffs |
|
Social Support ENRICHD30 |
10 Emotional, Instrumental, Informational and Appraisal |
0 – 25 Higher score indicates more social support No diagnostic cutoffs |
|
Health-related Quality of Life Kansas City Cardiomyopathy Questionnaire38 |
12 Physical Limitation, Symptoms, Quality of Life, Social Limitation Overall |
0 – 100 Higher score indicates better quality of life 50-75 good QOL, > 75 excellent QOL |
In addition to survey data, the Six Minute Walk (6MWT) was administered according to the American Thoracic Society Protocol. This test has a reported reliability of 0.8620–22 and is used in “standard of care” in many LVAD centers. Healthcare utilization was operationalized as number of outpatient visits, number of days hospitalized and number of outpatient procedures. Relevant data were captured from the electronic medical record for the 6 months prior to the date of survey completion or since the date of LVAD implant. Due to the complicated nature of these patients, only 78% were able to complete the survey; a STROBE diagram is presented in figure 2 to demonstrate completion rates.23
Figure 2.
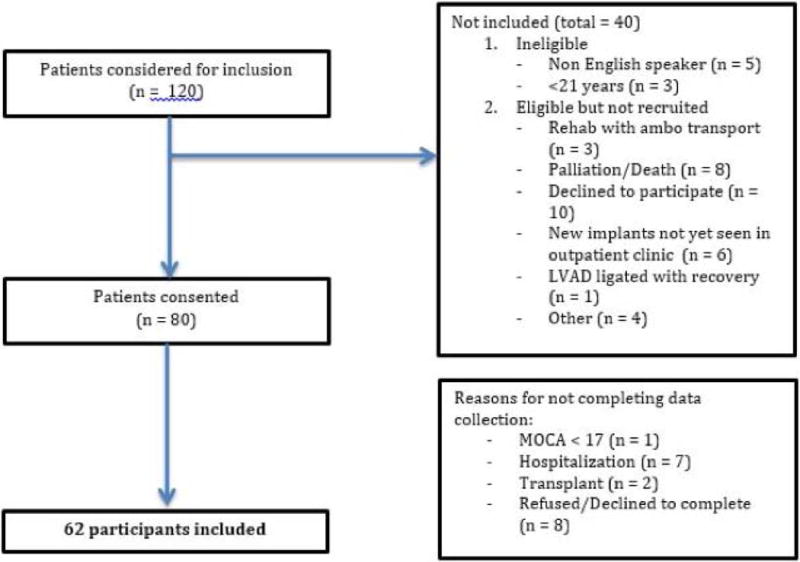
STROBE diagram of participant selection and inclusion
Data analysis
Data were checked for quality and consistency. All statistical analyses were completed with Stata version 14 (StataCorp, College Station, Texas). Descriptive statistics and graphical displays were used to summarize overall data (aim 1) and by perceived stress level (aim 2). We examined the distribution of perceived stress and ranked low (0-11), moderate and high (12-40), using approximately the upper two quartiles to designate moderate and high stress.7 T-tests were used to compare high and low stress groups. We also examined differences between clinic settings. A correlation matrix was created to examine relationships between continuous variables. Categorical variables were examined for their bivariate association using chi-square tests. A multiple linear regression model was then fit using only variables with p<0.20 from the bivariate correlation analysis (aim 3). This analysis was followed by tests for multi-collinearity between model variables using variance inflation factor. The assumptions of this parametric analysis were met. The final model includes only variables with p<0.05.
The moderation of social support was tested using two additional models (aim 4). To test these relationships we dichotomized social support at the median of 20. Interaction terms were created for 1) social support and perceived stress, then 2) social support and fatigue. Building on the multiple linear regression models, social support and interaction terms were tested.
RESULTS
Descriptive findings
The 62 patients who completed the survey were predominantly male (78%), black (47%), and married (66%) with mean age 56.7± 13.0 years. (See Table 2) Patients were nearly evenly distributed by implant strategy (destination therapy 49%, bridge to transplant 51%) and mean length of LVAD support was 25.3 ± 24.5 months. (See Table 3) Forty-nine percent were Intermacs Profiles 1 and 2, implanted emergently. On the Holmes & Rahe stressful life event inventory patients reported frequent stressful life events with average life event score 111.9 ± 91.8 (Table 3); 17 participants (27%) had a summed weighted score greater than 150, the hi-risk threshold.
Table 2.
Sample Characteristics by Level of Perceived Stress
| Perceived Stress | ||||
|---|---|---|---|---|
|
| ||||
| N=62 n (%) |
Low (n = 31) n (%) |
Moderate to High (n = 31) n (%) |
T-test or chi2 p-value | |
| Gender | ||||
| Male | 48 (77) | 24 (50) | 24 (50) | 1.00 |
| Female | 14 (23) | 7 (50) | 7 (50) | |
|
| ||||
| Age | ||||
| Mean ± SD | 56.7 ± 13.0 | 58.2 ± 12.6 | 55.3 ± 13.2 | 0.38 |
| Median | 58.8 | 60.6 | 56.5 | |
|
| ||||
| Race | ||||
| Black | 29(47) | 16 (55) | 13 (45) | |
| White | 25 (40) | 12 (48) | 13 (52) | 0.65 |
| Other | 8 (13) | 3 (38) | 5 (62) | |
|
| ||||
| Marital Status | ||||
| Married or Living with Partner | 40 (66) | 19 (48) | 21 (52) | 0.72 |
| Other | 21 (34) | 11 (52) | 10 (48) | |
|
| ||||
| Annual Household Income | ||||
| < $30,000 | 16 (25) | 9 (56) | 7 (44) | 0.53 |
| $30, 000-60,000 | 9 (15) | 3 (33) | 6 (67) | |
| >$60,000 | 37 (60) | 19 (51) | 18 (49) | |
|
| ||||
| Highest Level of Education | ||||
| <= high school | 14 (23) | 8 (57) | 6 (43) | 0.52 |
| technical school or some college | 18 (30) | 7 (39) | 11 (61) | |
| graduated college or beyond | 28 (47) | 15 (54) | 13 (46) | |
|
| ||||
| Co-morbidities | ||||
| Diabetes | 20 (32) | 9 (45) | 11 (55) | 0.59 |
| Chronic Renal Disease | 19 (31) | 11 (58) | 8 (42) | 0.41 |
| Depression | 6 (10) | 0 (0) | 6 (100) | 0.01 |
| Right heart failure | 5 (8) | 3 (60) | 2 (40) | 0.64 |
Table 3.
LVAD and Individual Characteristics by Level of Perceived Stress
| Perceived Stress | ||||
|---|---|---|---|---|
|
| ||||
| Overall N = 62 n (%) |
Low (n = 31) n (%) |
Moderate to High (n = 31) n (%) |
T-test or chi2 p-value | |
| Device | ||||
| Heartware | 23 (37) | 12 (52) | 11 (48) | 0.97 |
| Heartmate II | 37 (60) | 18 (49) | 19 (51) | |
| Heartmate III | 2 (3) | 1 (50) | 1 (50) | |
|
| ||||
| Implant Strategy | ||||
| Bridge to Transplant | 31 (49) | 15 (48) | 16 (52) | 0.80 |
| Destination Therapy | 32 (51) | 16 (52) | 15 (48) | |
|
| ||||
| Emergent Implant | ||||
| Intermacs Profile 1 or 2 | 30 (49) | 14 (47) | 16 (53) | 0.61 |
| Intermacs Profile > 2 | 32 (51) | 17 (57) | 15 (43) | |
|
| ||||
| Stressful Life events | ||||
| Mean ± SD | 111.9 ± 91.8 | 90.9 ± 79.8 | 133 ± 99.3 | 0.07 |
| Median | 97.5 | 82 | 128 | |
|
| ||||
| Months since initial implant | ||||
| Mean ± SD | 25.3 ± 24.5 | 25.3 ± 4.4 | 25.2 ± 4.5 | 0.98 |
| Median | 18.5 | |||
|
| ||||
| Complications | ||||
| Gastrointestinal bleed | 16 (27) | 6 (38) | 10 (62) | 0.25 |
| Stroke | 13 (21) | 7 (54) | 6 (46) | 0.76 |
| Driveline Infection | 10 (16) | 5 (50) | 5 (50) | 1.00 |
| Right Heart Failure | 4 (7) | 2 (50) | 2 (50) | 1.00 |
| Pump replaced | 4 (7) | 2 (50) | 2 (50) | 1.00 |
| Sepsis | 4 (7) | 1 (25) | 3 (75) | 0.30 |
| Tracheostomy | 3 (5) | 1 (33) | 2 (67) | 0.55 |
Notes: Higher total Stressful Life Events score indicates higher stress.
Mean perceived stress for the sample was 11.7 ± 7 (Table 4). The overall sample had a moderate stress profile: moderate perceived stress (mean 11.7 ± 7), few depressive symptoms (mean 3.2 ± 3.9) and moderate fatigue (mean 14.3 ± 9.1). Both adaptive and mal-adaptive coping strategies were commonly used by all participants. Patients reported very high social support (mean 19.9 ± 5.4).
Table 4.
Indicators of Psychosocial Stress, Social Support and Outcomes by Level of Perceived Stress
| Perceived Stress | ||||
|---|---|---|---|---|
|
| ||||
| Overall N = 62 Mean ± SD |
Low (n = 31) Mean ± SD |
Moderate to High (n = 31) Mean ± SD |
T-test p-value | |
| Indicators of Psychosocial Stress and Social Support | ||||
|
| ||||
| Perceived Stress | 11.7 ± 7.0 | 5.9 ± 2.1 | 17.6 ± 4.4 | - |
|
| ||||
| Depressive symptoms | 3.2 ± 3.9 | 1.2 ± 1.6 | 5.2 ± 4.5 | <0.01 |
|
| ||||
| Fatigue | 14.3 ± 9.1 | 8.4 ± 8 | 18.8 ± 7.4 | <0.01 |
|
| ||||
| Coping | ||||
| Adaptive Strategies | 37.4 ± 11.9 | 35.2 ±13.4 | 39.6 ± 10.0 | 0.14 |
| Mal-adaptive Strategies | 15.5 ± 4.4 | 13.6 ± 3.8 | 17.4 ± 4.1 | <0.01 |
|
| ||||
| Social Support | 19.9 ± 5.4 | 21.9 ± 4.8 | 18 ± 5.3 | <0.01 |
|
| ||||
| Outcomes | ||||
|
| ||||
| Quality of Life | ||||
| Physical limitation | 66.4 ± 16.0 | 70.4 ± 14.8 | 62.5 ± 16.3 | 0.05 |
| Symptom frequency | 88 ± 14.7 | 91.8 ± 11.8 | 84.4 ± 16.5 | 0.05 |
| QOL | 73.7 ± 23.8 | 83.5 ± 19.1 | 63.9 ± 24.3 | <0.01 |
| Social Limitation | 64.4 ± 20.3 | 74.6 ± 11.8 | 54.5 ± 22.0 | <0.01 |
| Overall | 73 ± 14.6 | 80.1 ± 9.5 | 66.3 ± 15.2 | <0.01 |
|
| ||||
| Six Minute Walk Test Distance (meters) | 287 ± 193 | 270 ± 187 | 306 ± 200 | 0.46 |
|
| ||||
| Healthcare Utilization* | ||||
| Days of Outpatient Visits | 6.5 ± 4.6 | 5.4 ± 3.5 | 7.5 ± 5.2 | 0.08 |
| Days Hospitalized | 9.9 ± 14.2 | 10.9 ± 16.4 | 9 ± 12.0 | 0.60 |
| Total healthcare days | 16.8 ± 15.7 | 15.8 ± 17.5 | 17.8 ± 14.0 | 0.62 |
| #days hospitalized/#days with LVAD | 0.08 ± 0.13 | 0.09 ± 0.16 | 0.07 ± 0.11 | 0.59 |
Higher Scores indicate worse perceived stress, depression, fatigue and utilization of coping strategies. Higher scores indicate better social support, HRQOL and exercise capacity.
Healthcare utilization was calculated for the 6 months prior to study date or in the time since LVAD implant.
Overall HRQOL was rated good (mean 73 ± 14.6). Regarding HRQOL domains, LVAD patients reported little interference of heart failure symptom frequency (88 ± 14.7) but social limitation was more severely limiting (64.4 ± 20.3). Mean 6MWT distance was 287 ± 193 meters overall, demonstrating low level of exercise capacity. Participants spent an average of 6.5 ± 4.6 days or 8% of days in the 6 months prior to the study in the hospital or attending outpatient visits. There were no significant differences by clinic setting for any variables studied.
Higher Perceived Stress is related to Depressive Symptoms, Fatigue and HRQOL
When comparing psychological stress response by perceived stress level using t-tests, the higher stress group had more depressive symptoms (p< 0.01), more fatigue (p< 0.001), used more maladaptive coping (p< 0.003) and had less social support (p < 0.003). In addition, overall HRQOL was worse in the higher stress group (P< 0.01); social limitation and QOL domains were worse in the higher stress group (p<0.01), while the physical limitation and symptom frequency domains trended toward significance (p=0.05). There were no demographic differences between groups, but the higher stress group included 6/31 participants with a history of depression compared to none in the lower stress group (p = 0.01). There were also no differences between groups by implant strategy, emergent implantation, time since implant, stressful life events, 6MWT distance or healthcare utilization.
Multi-variate Modeling
In multivariate regression analysis, perceived stress and fatigue were independent predictors of worse HRQOL. Using the model for HRQOL we tested social support as a moderator of the relationships between psychological stress response and HRQOL. High social support moderated the relationship between perceived stress and HRQOL when controlling for fatigue (R2 = 0.49, p< 0.001). (See Table 5 & Figure 3) Variance inflation factors were less than 2 on the final models, indicating low likelihood of collinearity. Regression analysis showed no significant multivariate models for exercise capacity or healthcare utilization.
Table 5.
Social Support Moderation Model, R2 = 0.49, df = 59, p< 0.001
| Beta Coefficient | Standard Error | P-value | |
|---|---|---|---|
| Perceived Stress | −0.99 | 0.33 | <0.01 |
| Fatigue | −0.62 | 0.19 | <0.01 |
| Social Support (Dichotomized at median = 21.5) | −4.54 | 5.5 | 0.41 |
| Perceived Stress * Social Support | 0.86 | 0.42 | 0.04 |
Figure 3.
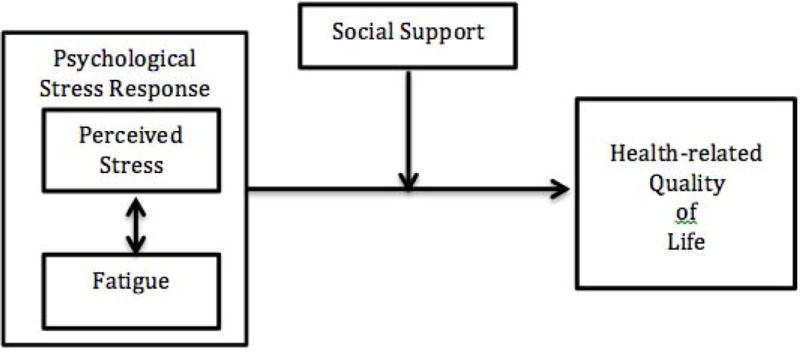
Final Multi-variate Quality of Life Model (R2 = 0.49, p< 0.01)
DISCUSSION
We found that most LVAD patients had a moderate level of perceived stress, mild depressive symptoms and moderate fatigue. Those with higher perceived stress had worse depressive symptoms, fatigue and more frequently used mal-adaptive coping compared with those with lower stress. In multivariate analysis, high perceived stress and fatigue was associated with lower HRQOL and this relationship was moderated by social support.
The perceived stress mean score was similar to the age-adjusted normal value of 12, which has been reported for the general population and similar to those reported in other cardiac populations.24 Higher perceived stress has been related to higher mortality in myocardial infarction patients.7 Further investigation is warranted to examine the role of perceived stress in LVAD patients, the mechanisms for these effects and the possible impact on adverse events and survival. These findings suggest that enhanced clinical assessment of psychosocial factors is important for understanding LVAD outcomes. This is a challenge as LVAD patient visits are frequently full, including physical exams and equipment checks. However, early referral for psychological counseling and even palliative care symptom management may reduce the burden felt by patients and providers.
We did not see a relationship between coping strategies and HRQOL, however we did find that more frequent use of adaptive and mal-adaptive coping strategies was associated with a worse perceived stress. This is consistent with the Lazarus and Folkman description of the economics of stress - as stress increases, the demand for coping increases.25 Thus, those with higher levels of perceived stress also reported more frequent use of both mal-adaptive and adaptive coping strategies because more coping is required when more stress is experienced. The brief COPE does not evaluate effectiveness of coping strategies, only frequency of use. Understanding how individuals living with an LVAD cope with stress is important for understanding issues of adherence and self-management and for determining ways to support patients and families throughout LVAD therapy.
Overall, this sample of community dwelling LVAD patients appears similar in HRQOL and exercise capacity compared to previous research. KCCQ-12 average scores 12 months after implant range between 66 and 75.15,26,27 HRQOL in this study was within this range, which is nearly double reported KCCQ values prior to LVAD implant and exceeds the minimal clinically important difference for the KCCQ.26,28,29 Exercise capacity was also within range of findings from Intermacs.2,26 Hospital length of stay has been reported in the literature, but we did not identify any other studies that considered outpatient visits in LVAD healthcare utilization. The frequency of outpatient visits may vary by region and LVAD program as a function of the distance from the patient’s home to clinic, use of outreach strategies and stability of the patient, which we did not capture in this study.
Social support was reported at a comparable level to previously reported cardiac populations who were partnered.30 This was expected, as LVAD patients are required to have caregivers available for initial implant care, to support clinic attendance and to manage LVAD care. Multi-variate modeling and moderation analysis revealed that, when comparing those with the same level of perceived stress, those with high social support had a higher HRQOL than those with low social support after controlling for fatigue. This moderation analysis provides evidence for the importance placed on social support when considering advanced HF patients for VAD implantation. However, it was not possible to determine in this study if the caregiver, healthcare team or other sources are responsible for the perceived level of social support. Support is provided by LVAD programs through 24/7 access to providers. Yet, patients and caregivers have reported variable levels of satisfaction with the support provided by LVAD programs, suggesting a need to explore additional ways to increase the type(s) and level of support provided.31 Specifically, it is not clear how programs are assessing patient stress or helping patients manage stress. Resources vary between institutions, although some offer support groups and other activities for LVAD patients and caregivers. Support strategies that are tailored to the individual patients’ needs may be most effective.
Strengths and Limitations
To our knowledge, this is the first study to examine indicators of psychological stress, coping and social support in a moderate size continuous flow LVAD patient sample, providing important intervention targets for future work. In addition, we evaluated important psychosocial factors and their impact on outcomes in a diverse, multi-center population. Finally, we have introduced evidence that supports LVAD program policies related to social support. To expand these findings, the next step will be to conduct a longitudinal study to examine how psychosocial factors change over time and to establish approaches to tailoring future interventions.
This study has several limitations. As a cross-sectional study, no causal relationships can be drawn from this analysis. Further we had several challenges in completion rates. Long patient clinic visits and frequent complications often resulted in patients who consented being unable to complete the survey. This may have resulted in a self-selection bias and in the under-estimation of variables related to stress and over-estimation of HRQOL compared to the total LVAD population. This concern is consistent with other survey data collected from the LVAD population.32 Also, our statistical approach may not have captured all possible confounders. In addition, the patients in our sample had an average of almost 2 years of LVAD support, which also may have resulted in lower reported stress and higher HRQOL than the overall LVAD population. Another limitation is that we used a HF-specific measure for HRQOL. This measure is not specific to having a VAD, however as of yet there are no VAD-specific measures of HRQOL. Finally, our conceptual framework incorporated coping as a component of psychological stress response, due to the nature of the Brief COPE which measures frequency of coping strategy use. Others have described coping as a mediator of stress and outcomes and another instrument which incorporates a measure of coping effectiveness may provide a more clear understanding of coping as a mediator of stress in this population.
Conclusions
Increased perceived stress was related to worse depressive symptoms, fatigue, mal-adaptive coping and worse HRQOL. Further, the influence of high levels of social support on HRQOL despite fatigue confirms the need to continually assess the social support available to LVAD patients. Thorough, ongoing assessment by healthcare providers and social workers may uncover stressful conditions requiring increased monitoring and possible intervention. Future studies to test the effects of interventions designed to enhance stress management via adaptive coping may improve HRQOL and other LVAD outcomes.
Acknowledgments
Grant Support:
Interdisciplinary Training in Cardiovascular Research T32 NR 012704 (2012-2014)
Predoctoral Training in Research Program (NIH 5TL1TR001078-02 (2014-2015)
1F31NR015179-01A1 National Institute of Nursing Research, NIH (2015-2017)
Heart Failure Society of America Nursing Research Grant (2014-2016)
Footnotes
Disclosures:
Dr. Russell serves on the Data Safety and Monitoring Board for Thoratec/St. Jude.
Author Contributions:
Study design: MA, CB, KG, PD, SR, HH, SD, CDH
Study Implementation: MA, SR, SD, CDH
Manuscript Development: MA, CB, PD, SR, HH, KG, SD, CDH
Final Approval: MA, CB, PD, SR, HH, KG, SD, CDH
References
- 1.Abshire M, Prichard R, Cajita M, DiGiacomo M, Dennison Himmelfarb C. Adaptation and coping in patients living with an LVAD: A metasynthesis. Hear Lung J Acute Crit Care. 2016;45(5):397–405. doi: 10.1016/j.hrtlng.2016.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kirklin JKJK, Naftel DCDCDCDC, Pagani FDFD, Kormos RLRLRLRL, Stevenson LWLWLW, Blume ED, et al. Seventh INTERMACS annual report: 15,000 patients and counting. J Hear Lung Transplant. 2015;34(12):1495–1504. doi: 10.1016/j.healun.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 3.Casida JM, Marcuccilli L, Peters RM, Wright S. Lifestyle adjustments of adults with long-term implantable left ventricular assist devices: a phenomenologic inquiry. Heart Lung. 2011;40(6):511–520. doi: 10.1016/j.hrtlng.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 4.Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York, NY: Springer Publishing; 1984. [Google Scholar]
- 5.Heim C, Ehlert U, Hellhammer DH. The potential role of hypocortisolism in the pathophysiology of stress-related bodily disorders. Psychoneuroendocrinology. 2000;25(1):1–35. doi: 10.1016/s0306-4530(99)00035-9. http://www.ncbi.nlm.nih.gov/pubmed/10633533. [DOI] [PubMed] [Google Scholar]
- 6.Ehlert U, Gaab J, Heinrichs M. Psychoneuroendocrinological contributions to the etiology of depression, posttraumatic stress disorder, and stress-related bodily disorders: the role of the hypothalamus–pituitary–adrenal axis. Biol Psychol. 2001;57(1–3):141–152. doi: 10.1016/S0301-0511(01)00092-8. [DOI] [PubMed] [Google Scholar]
- 7.Arnold SV, Smolderen KG, Buchanan DM, Li Y, Spertus JA. Perceived stress in myocardial infarction: long-term mortality and health status outcomes. J Am Coll Cardiol. 2012;60(18):1756–1763. doi: 10.1016/j.jacc.2012.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scherer M, Himmel W, Stanske B, Scherer F, Koschack J, Kochen MM, et al. Psychological distress in primary care patients with heart failure: a longitudinal study. Br J Gen Pract. 2007;57(543):801–807. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2151812&tool=pmcentrez&rendertype=abstract. Accessed July 16, 2014. [PMC free article] [PubMed] [Google Scholar]
- 9.Allman E, Berry D, Nasir L. Depression and coping in heart failure patients: a review of the literature. J Cardiovasc Nurs. 2009;24(2):106–117. doi: 10.1097/JCN.0b013e318197a985. [DOI] [PubMed] [Google Scholar]
- 10.Overgaard D, Grufstedt Kjeldgaard H, Egerod I. Life in transition: a qualitative study of the illness experience and vocational adjustment of patients with left ventricular assist device. J Cardiovasc Nurs. 2012;27(5):394–402. doi: 10.1097/JCN.0b013e318227f119. [DOI] [PubMed] [Google Scholar]
- 11.Magid M, Jones J, Allen La, McIlvennan CK, Magid K, Thompson JS, et al. The Perceptions of Important Elements of Caregiving for a Left Ventricular Assist Device Patient. J Cardiovasc Nurs. 2015;0(0):1. doi: 10.1097/JCN.0000000000000242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dickson VV, McCarthy MM, Howe A, Schipper J, Katz SM. Sociocultural influences on heart failure self-care among an ethnic minority black population. J Cardiovasc Nurs. 2013;28(2):111–118. doi: 10.1097/JCN.0b013e31823db328. [DOI] [PubMed] [Google Scholar]
- 13.Staniute M, Brozaitiene J, Bunevicius R. Effects of social support and stressful life events on health-related quality of life in coronary artery disease patients. J Cardiovasc Nurs. 28(1):83–89. doi: 10.1097/JCN.0b013e318233e69d. [DOI] [PubMed] [Google Scholar]
- 14.Cobb S. PRESIDENTIAL ADDRESS—Social Support as a Moderator of Life Stress. Psychosom Med. 1976;38(5):300–314. doi: 10.1097/00006842-197609000-00003. https://campus.fsu.edu/bbcswebdav/institution/academic/social_sciences/sociology/ReadingLists/Mental_Health_Readings/Cobb-PsychosomaticMed-1976.pdf. Accessed November 21, 2017. [DOI] [PubMed] [Google Scholar]
- 15.Grady KL, Meyer PM, Dressler D, Mattea A, Chillcott S, Loo A, et al. Longitudinal change in quality of life and impact on survival after left ventricular assist device implantation. Ann Thorac Surg. 2004;77(4):1321–1327. doi: 10.1016/j.athoracsur.2003.09.089. [DOI] [PubMed] [Google Scholar]
- 16.Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–699. doi: 10.1111/j.1532-5415.2005.53221.x. [DOI] [PubMed] [Google Scholar]
- 17.Ginty AT, Conklin SM. High perceived stress in relation to life events is associated with blunted cardiac reactivity. Biol Psychol. 2011;86(3):383–385. doi: 10.1016/j.biopsycho.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 18.Doering LV, Dracup K, Caldwell MA, Moser DK, Erickson VS, Fonarow G, et al. Is coping style linked to emotional states in heart failure patients? J Card Fail. 2004;10(4):344–349. doi: 10.1016/j.cardfail.2003.10.001. http://www.ncbi.nlm.nih.gov/pubmed/15309703. Accessed July 24, 2014. [DOI] [PubMed] [Google Scholar]
- 19.Tabachnick BG, Fidell LS. Using Multivariate Statistics. Pearson Education; 2013. [Google Scholar]
- 20.Fleg JL, Piña IL, Balady GJ, Chaitman BR, Fletcher B, Lavie C, et al. Assessment of functional capacity in clinical and research applications: An advisory from the Committee on Exercise, Rehabilitation, and Prevention, Council on Clinical Cardiology, American Heart Association. Circulation. 2000;102(13):1591–1597. doi: 10.1161/01.cir.102.13.1591. http://www.ncbi.nlm.nih.gov/pubmed/11004153. Accessed July 16, 2014. [DOI] [PubMed] [Google Scholar]
- 21.Guyatt GH, Sullivan MJ, Thompson PJ, Fallen EL, Pugsley SO, Taylor DW, et al. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985;132(8):919–923. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1345899&tool=pmcentrez&rendertype=abstract. Accessed July 16, 2014. [PMC free article] [PubMed] [Google Scholar]
- 22.Guyatt GH, Thompson PJ, Berman LB, Sullivan MJ, Townsend M, Jones NL, et al. How should we measure function in patients with chronic heart and lung disease? J Chronic Dis. 1985;38(6):517–524. doi: 10.1016/0021-9681(85)90035-9. http://www.ncbi.nlm.nih.gov/pubmed/4008592. Accessed July 16, 2014. [DOI] [PubMed] [Google Scholar]
- 23.Vandenbroucke JPJ, von Elm E, Altman DDG, Gøtzsche PPC, Mulrow CDC, Pocock SSJ, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and Elaboration. PLoS Med. 2007;4(10):e297. doi: 10.1371/journal.pmed.0040297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cohen S, Kamarck T, Mermelstein R. Stress A Global Measure of Perceived. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 25.Lazarus Richard S U California, Berkeley, USFolkman S. Transactional theory and research on emotions and coping. Eur J Pers. 1987;1(3, Special Issue):141–169. [Google Scholar]
- 26.Allen JG, Weiss ES, Schaffer JM, Patel ND, Ullrich SL, Russell SD, et al. Quality of life and functional status in patients surviving 12 months after left ventricular assist device implantation. J Heart Lung Transplant. 2010;29(3):278–285. doi: 10.1016/j.healun.2009.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grady KL, Naftel DC, Myers SL, Dew MA, Weidner G, Spertus JA, et al. Change in Health-related Quality of Life from Before to After Destination Therapy Mechanical Circulatory Support is Similar for Older and Younger Patients: Analyses from INTERMACS. J Hear Lung Transplant. 2015;34(Suppl 2):213–221. doi: 10.1097/MPG.0b013e3181a15ae8.Screening. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maciver J, Ross HJ. Quality of life and left ventricular assist device support. Circulation. 2012;126(7):866–874. doi: 10.1161/CIRCULATIONAHA.111.040279. [DOI] [PubMed] [Google Scholar]
- 29.Abshire M, Dennison Himmelfarb CRCR, Russell SDSD. Functional status in left ventricular assist device-supported patients: a literature review. J Card Fail. 2014;20(12):973–983. doi: 10.1016/j.cardfail.2014.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vaglio J, Conard M, Poston WS, O’Keefe J, Haddock CK, House J, et al. Testing the performance of the ENRICHD Social Support Instrument in cardiac patients. Health Qual Life Outcomes. 2004;2:24. doi: 10.1186/1477-7525-2-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Blumenthal-Barby JS, Kostick KM, Delgado ED, Volk RJ, Kaplan HM, Wilhelms LA, et al. Assessment of patients’ and caregivers’ informational and decisional needs for left ventricular assist device placement: Implications for informed consent and shared decision-making. J Heart Lung Transplant. 2015;34(9):1182–1189. doi: 10.1016/j.healun.2015.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Grady KL, Wissman Sherri, Naftel DC, Myers S, Gelijins A, Moskowitz A, et al. Age and gender differences and factors related to change in health-related quality of life from before to 6 months after left ventricular assist device implantation: Findings from Interagency Registry for Mechanically Assisted Circulatory Support. J Hear Lung Transplant. 2016;35(6):777–788. doi: 10.1016/j.healun.2016.01.1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Holmes TH, Rahe RH. The social readjustment rating scale. J Psychosom Res. 1967;11(2):213–218. doi: 10.1016/0022-3999(67)90010-4. [DOI] [PubMed] [Google Scholar]
- 34.Rahe RH, Arthur RJ. Life change and illness studies: past history and future directions. J Human Stress. 1978;4(1):3–15. doi: 10.1080/0097840X.1978.9934972. [DOI] [PubMed] [Google Scholar]
- 35.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1495268&tool=pmcentrez&rendertype=abstract. Accessed July 10, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Belza BL, Henke CJ, Yelin EH, Epstein WV, Gilliss CL. Correlates of fatigue in older adults with rheumatoid arthritis. Nurs Res. 42(2):93–99. http://www.ncbi.nlm.nih.gov/pubmed/8455994. Accessed May 19, 2015. [PubMed] [Google Scholar]
- 37.Carter C. You want to measure coping but your protocol’s too long: consider the brief COPE. Int J Behav Med. 1997;4(1):92–100. doi: 10.1207/s15327558ijbm0401_6. http://www-ncbi-nlm-nih-gov.ezproxy.welch.jhmi.edu/pubmed?holding=jhumlib_fft_ndi&otool=jhumlib&term=You+Want+to+Measure+Coping+But+Your++Protocol’s+Too+Long:+Consider+the++Brief+COPE. Accessed July 2, 2014. [DOI] [PubMed] [Google Scholar]
- 38.Spertus JA, Jones PG, Kim J, Globe D. Validity, reliability, and responsiveness of the Kansas City Cardiomyopathy Questionnaire in anemic heart failure patients. Qual Life Res. 2008;17(2):291–298. doi: 10.1007/s11136-007-9302-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


