Abstract
Objective
To identify organizational factors contributing to workplace violence in hospitals.
Methods
A questionnaire survey was conducted in 2013 among employees in a Midwestern hospital system (n=446 respondents). Questions concerned employees’ experiences of violence at work in the previous year and perceptions of the organizational safety climate. Logistic regressions examined staff interaction and safety climate factors associated with verbal and physical violence, respectively.
Results
Interpersonal conflict was a risk factor for verbal violence (OR 1.49, 95% CI 1.04-2.12, p<.05) and low work efficiency was a risk factor for physical violence (OR .98, 0.97-0.99). A poor violence prevention climate was a risk factor for verbal (OR 0.48, 0.36-0.65, p<.001) and physical (OR 0.60, 0.45-0.82, p<.05) violence.
Conclusions
Interventions should aim at improving coworker relationships, work efficiency, and management promotion of the hospital violence prevention climate.
Keywords: workplace violence, health care workers, hospitals, workplace safety climate
BACKGROUND
Workplace violence in the healthcare sector is a serious occupational and public health concern. Hospital workers comprise almost 40% of all employees in the healthcare industry in the United States1 and have long been recognized as being at increased risk for non-fatal injuries due to workplace violence.2-4 While violence is an occupational hazard in all types of hospitals (i.e., private, state, and local government), it is the predominant cause of work-related injury among employees of state-run and government hospitals, which often include psychiatric and substance abuse treatment facilities.1 Patients are the primary perpetrators of violence towards hospital workers, with patient assault the main cause of violence-related injury requiring time away from work.5 However, U.S. official statistics capture only work-related injuries that result in a minimum of one day away from work.6 Consequently, much less is known regarding the prevalence of non-physical violence, such as verbal aggression, threatening behavior, or violent acts that do not result in serious physical injury or lost time. Research suggests that such workplace violence is significantly underreported, especially when no physical injury is incurred.7 Yet a growing body of research has identified non-physical aggression, including bullying, from both patients and co-workers as a serious cause of psychological ill-health that is associated with decreased work satisfaction8 and productivity9-10 and increased job turnover.11 Underreporting leaves hospitals with an incomplete picture of the full gamut of violent events, greatly hindering the development of prevention efforts. This dilemma raises questions as to what hospitals and occupational health professionals can do to reduce hospital workers’ risk of harm from violence, both physical and non-physical.
Risk factors for workplace violence in hospitals
Research to date has identified perpetrator,12-15 worker,13 situational14 and environmental13,16 factors associated with violence towards healthcare workers. Knowledge of these factors provides some guidance into how violence-related injury can potentially be reduced, such as through improving workplace lighting, shortening work shifts, and providing workers with cell phones or personal alarms.16 To our knowledge, none of these interventions has been rigorously tested in scientific studies. Moreover, these factors, while important, do not shed light on the healthcare organization’s broader culture of safety or its role in protecting workers from potential violence-related harm. A better understanding of organizational attitudes towards, and practices related to, violence prevention would enhance efforts to design interventions to reduce worker exposure to, and injury from, violence at work.
Establishing an organizational climate of safety
In health care, a culture of safety describes an organization’s overall commitment to safety,17 encompassing efforts to protect both patients and workers from harm.18 Such efforts include open communication about adverse events; a nonpunitive response to error; a focus on learning from mistakes and developing strategies to prevent recurrence; teamwork; and management support for safety.19 In the organizational health literature, the concepts of “safety culture” and “safety climate” have been debated for decades.20 In general, safety culture is defined as the fundamental values, norms, and expectations that an organization places on safety, while safety climate describes employees’ perceptions and beliefs about the organization’s focus on, and support for, safety.20 Safety climate has traditionally been investigated in studies of occupational accidents and injuries.21-22 In hospitals, a recent study examined the role of management commitment to safety and teamwork in worker injuries, reporting that management commitment was positively associated with teamwork but not directly associated with documented injuries. However, teamwork was directly associated with, and mediated the effect of, management commitment on worker injury.23
Safety climate has recently been studied specifically for its potential role in the reduction of workplace violence.24-25 In a Taiwanese study of physicians from four hospitals, lower safety climate ratings, along with higher job demands, were associated with workplace violence.24 Although that study distinguished between violent threats and sexual harassment, violent threats were defined as any verbal or physical violence, and thus did not distinguish between the two when examining safety climate determinants. A study from a single Israeli hospital found that enhancing the safety climate via a three-day educational program helped to decrease the number of aggressive incidents towards staff on closed psychiatric wards.25 However, the latter study did not examine any other organizational factors that could potentially influence violence towards psychiatric staff; moreover, violence was restricted to physical assaults only. To the best of our knowledge, no previous studies have examined safety climate determinants of verbal and physical violence, respectively.
Work stress and co-worker interaction
Additional factors that have been associated with violence towards health care workers are work stress and poor co-worker relationships.26-27 One of the few large-scale, longitudinal studies examining occupational factors associated with violence in healthcare was conducted in eight European countries in the Nurses’ Early Exit (NEXT) Study.26 While that study examined predictors of organizational commitment, and not violence, it did report that greater time pressure and poor interpersonal relationships were significantly associated with a higher frequency of violence by patients and harassment by supervisors.26 Work stress and low social support were both associated with non-physical violence towards nurses in Italy.27 Job demands, like work stress, is a measure that reflects time pressure and predicted violent threats towards physicians in Taiwan.24
Current Study
Building further on this research, the current study aimed to identify malleable factors in the healthcare work environment that could contribute to self-reported experience with violence among hospital workers. Identification of such factors would provide concrete support for hospital administrators and occupational health professionals in protecting workers from violence. We hypothesized that work stress, the nature of co-worker interaction, and the work safety climate would all influence hospital workers’ exposure to workplace violence and aggression, i.e., both physical and non-physical violence. A conceptual model for the study is illustrated in Figure 1.
Figure 1.
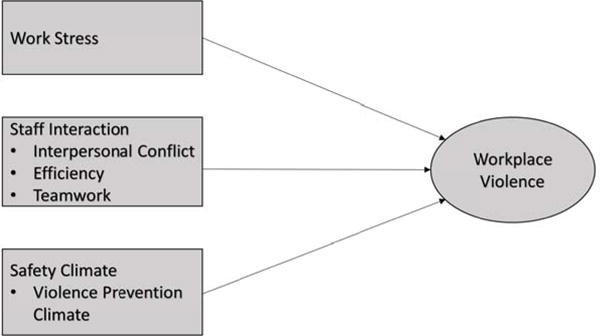
Conceptual model of organizational determinants of workplace violence against hospital workers. Workplace violence encompasses both verbal and physical violence.
The aim of this study was to examine the effect of work stress, staff interaction and organizational safety climate on self-reported workplace violence towards hospital workers. In order to better understand possible differences due to the type of violence, the aim was to identify organizational determinants of verbal and physical violence, respectively.
MATERIALS AND METHODS
Setting and Participants
The study was conducted within a multi-site hospital system in the Midwest United States with approximately 15,000 employees. The current study was limited to employees on 41 hospital units (N=2,010) across the hospital system that were identified as being at increased risk of violence based on rates of documented incidents from a 30-month period (January 2010-June 2012).28 In the spring of 2013, employees assigned to the 41 units were asked by the researchers to participate in a questionnaire survey regarding their exposure to workplace violence. Questionnaires were mailed home to employees along with a postage-paid return envelope and a cover letter. The letter described the purpose of the study and informed employees that participation was voluntary and questionnaire responses were confidential. Employees gave their consent to participate in the study by completing and returning the questionnaire. Each employee responding to the questionnaire received a $10 gift card by mail. The cover letter explained that each questionnaire was coded with an identification number that enabled the research team to identify respondents from a master list. Once the questionnaires had been returned and the gift cards had been mailed out, the list linking identification numbers with respondent names and addresses was destroyed. Approximately 2 weeks after the first mailing, reminders and questionnaires were re-sent to non-respondents.
Ethical approval for this study was granted by the Institutional Review Board at Wayne State University and the Research Review Council of the hospital system.
Questionnaire
The questionnaire was developed for the study and measured employees’ experiences with violence and aggression at work during the past year. Socio-demographic/background items included age, gender, and job category. Violence was defined as acts or threats of physical or verbal aggression at work. Employees were asked whether they had been a target of violence or aggression at work during the past year. Response alternatives were “No, never,” “Yes, once or twice,” and “Yes, several times.”29 Additional questions concerned the perpetrator (patient, patient relative/visitor, hospital staff, manager/supervisor, or other) and the type of violence/aggression that the employee experienced. Response alternatives included verbal aggression (shouting, swearing), threat, physical violence (hitting, punching, kicking, spitting, biting, etc.), use of an object or weapon, or other.
Organizational measures
Based on our conceptual model, the current study focused on measures of work stress, staff interaction, and organizational safety climate as factors potentially influencing exposure to workplace violence.
Work Stress
The work stress scale originates from the Quality Work Competence (QWC) survey that is used to evaluate the work environment.30 It consists of four items related to employee perceptions of the time available to plan, carry out, and reflect about their work. A sample item is, “Do you have enough time to carry out your work tasks?” Items are rated on a four-point response scale ranging from 1 (often) to 4 (never). Thus, higher scores represent higher levels of stress. Stress scores were calculated by totaling the scores on the four component items and converting that sum to a percentage of the maximum possible score.31 Cronbach’s alpha for Work Stress in this study was .82.
Staff Interaction
Three scales assessed communication and interaction among coworkers. The Interpersonal Conflict at Work scale (ICAWS)32 is a four-item measure that assesses how well one gets along with coworkers. Each of the items measures some form of incivility.33 A sample item is, “How often do coworkers ignore or exclude you at work?” The ICAWS is rated on a five-point scale from 1 (never) to 5 (always), with higher total sum scores indicating more frequent conflicts with others. Cronbach’s alpha for the scale was .86. Work Efficiency,34-35 another QWC scale, is a four-item measure of employees’ perceptions of how well work processes function at their workplace. A sample item is, “At my workplace, resources are optimally utilized.” Efficiency is rated on a four-point response scale from 1 (strongly disagree) to 4 (strongly agree), with higher scores indicating better perceived efficiency (Cronbach’s alpha .85). Scores for work efficiency were calculated by totaling the four component item scores and converting that sum to a percentage of the maximum possible score.31 Teamwork19,23 is comprised of four items measuring the degree to which unit staff work together to accomplish work tasks (Cronbach’s alpha .91). A sample item is, “People support one another in this unit.”
Organizational Safety Climate
The current study utilized a safety climate measure specifically concerned with workplace violence prevention. The Violence Prevention Climate scale was developed to assess an organization’s efforts to protect its employees from exposure to violence, both physical and non-physical.36-37 In the current study, we used the four-item “Practices” subscale from the 12-item version of the full scale.38 This subscale focuses on perceptions that management takes action to promote worker safety against workplace violence. Cronbach’s alpha was .90. A sample item includes, “Management in this hospital quickly responds to episodes of violence.” Component items in the scale were expressed as statements, with each rated on a five-point scale that measured the respondent’s agreement from 1 (Strongly disagree) to 5 (Strongly agree). Higher total sum scores indicated more positive ratings of the violence prevention climate.
Data Analysis
Two dependent variables representing verbal and physical violence, respectively, were created based on the type of violence that employees reported having experienced. Responses of verbal aggression and threat were combined as the verbal violence variable; responses of physical violence or use of an object or weapon were combined as the physical violence variable. Reponses in the “other” category, which included descriptions of bullying, sexually verbal abuse, and physical assault, were categorized accordingly as verbal or physical. Analyses revealed that 61.3% of employees (n=268) had experienced verbal violence and 29.5% (n=129) experienced physical violence. These categories were not mutually exclusive, as employees were asked about violence in the past year and could have experienced multiple events that varied in nature.
Bivariate analysis was used to examine correlations between the predictor variables (work stress, staff interaction and safety climate variables). Previous analyses of this population indicated that aggregation at the unit level was not justified and relationships between variables were more appropriately studied at the individual level.23 For the current study, hierarchical cluster analysis using scree plots and dendrograms39 confirmed that meaningful clusters could also not be created at the hospital level (data not shown). For this reason, we were not able to account for clustering of workers. A four-step logistic regression analysis was conducted with verbal workplace violence and physical workplace violence in the last year, respectively, as the dependent variables. The violence variable was recoded into a binary variable (yes/no response) according to whether the participants experienced violence at work during the past year or not. The demographic variables age, gender and job category were entered in the first step. Work stress was entered in the second step, staff interaction variables (interpersonal conflict, efficiency, teamwork) were entered in the third step, and the safety climate variable (violence prevention climate) was entered in the final step. Statistical analyses were conducted using IBM SPSS statistics, version 23 (IBM Corp, Armonk, NY).
RESULTS
A total of 2,010 questionnaires were mailed out to employees on the 41 units; of those, 89 were returned as undeliverable. Of the 1921 staff who received a questionnaire, 446 staff responded, for an overall response rate of 23%. Questionnaire respondents did not differ from the total population of hospital system workers in terms of age or gender; however, respondents were significantly older and included significantly fewer patient care associates than non-respondents.7 Characteristics of questionnaire respondents are summarized in Table 1. The majority of the respondents were in the 40-49 age group (25.6%) and female (81.8%); registered nurses comprised the largest job category (58.1%).
Table 1.
Characteristics of Questionnaire Respondents (n=446)
| n | % | |
|---|---|---|
| Age | ||
| <29 | 104 | 23.4 |
| 30–39 | 73 | 16.4 |
| 40–49 | 114 | 25.6 |
| 50–59 | 99 | 22.2 |
| >60 | 55 | 12.4 |
| Gender | ||
| Male | 79 | 17.7 |
| Female | 365 | 81.8 |
| Job category | ||
| Registered nurse | 259 | 58.1 |
| Patient care | 34 | 7.6 |
| associate | ||
| Mental health | 10 | 2.2 |
| Technician | ||
| Security | 41 | 9.2 |
| Other | 102 | 22.9 |
Table 2 summarizes participant responses to the questions related to workplace violence. Nearly 63% (n=275) had been a target of violence or aggression at work during the past year, 34% on one or two occasions and 29% several times. Respondents reported that they experienced violence most often from patients (44.2%) and patient relatives/visitors (29.5%). Hospital staff (14%) and managers (4.8%) were also identified as perpetrators. Verbal aggression was the most common type of violence reported (60%), followed by threat (36.4%), physical violence (28.8%) and use of an object or weapon (4.1%).
Table 2.
Responses to Questions on Workplace Violence and Aggression ‡ (n=446)
| n | % | |
|---|---|---|
| Have you been a target of violence or aggression at work during the past year? | ||
| No, never | 162 | 37.1 |
| Yes, once or twice | 150 | 34.3 |
| Yes, several times | 125 | 28.6 |
| Who was violent or aggressive towards you?‡‡ | ||
| Patient | 193 | 44.2 |
| Patient relative/visitor | 129 | 29.5 |
| Hospital staff | 61 | 14.0 |
| Manager/supervisor | 21 | 4.8 |
| Other | 10 | 2.3 |
| I wasn’t a target of violence | 159 | 36.4 |
| What type of violence/aggression did you experience?‡‡ | ||
| Verbal aggression | 262 | 60.0 |
| Threat | 159 | 36.4 |
| Physical violence | 126 | 28.8 |
| Use of an object or weapon | 18 | 4.1 |
| Other | 12 | 2.7 |
| I wasn’t a target of violence | 157 | 35.9 |
Violence was defined as “acts or threats of physical or verbal aggression”
Multiple responses were possible on these questions
Table 3 depicts bivariate correlations and descriptive statistics of the variables included in the study. All the predictor variables were moderately and significantly (p<.001) correlated, with coefficients ranging from .279 to .479. Work stress was positively correlated with interpersonal conflict (.301) and negatively correlated with efficiency (−.470), teamwork (−.479) and violence prevention climate (−.422).
Table 3.
Means, Standard Deviations, and Bivariate Associations between Work Stress (1), Staff Interaction (2–4) and Safety Climate Measures (5)
| M | SD | 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|---|---|
| 1 Work Stress | 39.8 | 22.40 | 1 | ||||
| 2 Interpersonal Conflict | 1.92 | .75 | .301 | 1 | |||
| 3 Efficiency | 58.3 | 21.69 | −.470 | −.279 | 1 | ||
| 4 Teamwork | 3.76 | .92 | −.290 | −.479 | .381 | 1 | |
| 51 VPC | 3.55 | .96 | −.422 | −.332 | .369 | .405 | 1 |
Note: N=446. All correlation coefficients are significant at p < .001,
Violence Prevention Climate.
For all regression analyses, variance inflation factors ranged from 1.36 to 1.48 indicating that collinearity was not a concern. Table 4 represents the logistic regression analysis with work stress, staff interaction and safety climate variables as the predictor variables and verbal violence as the dependent variable. In the first step, age, gender and job category were added to control for demographic variables. Registered nurses (OR 1.87, p ≤ .01,) and security staff (OR 4.71, p ≤ .01,) were more likely to report verbal violent events in the past year compared to other job categories. The model explained 7.8% of the variance (Nagelkerke R2 = .078). Higher ratings of work stress, added in the second step, also increased the likelihood of reporting verbal violence (OR 1.02, p<.001), with the model explaining 11.8% of the variance (Nagelkerke R2 = .118). Interpersonal conflict, work efficiency, and teamwork were added as staff interaction variables in the third step, increasing the explained variance of the model to 16.3% (Nagelkerke R2 = .163). Interpersonal conflict was positively associated with verbal violence (OR 1.56, p<.05). Neither efficiency nor teamwork was significantly associated with violence. Work stress remained significant, albeit at a lower level (OR 1.01, p<05). Violence prevention climate was inversely and strongly associated with workplace violence (OR .48, p<.001). Stress was no longer significant in the final model, while interpersonal conflict retained significance (OR 1.49, p ≤ .01). The final model explained 23.2% of the variance in verbal violence (Nagelkerke R2 = .232).
Table 4.
Summary of Logistic Regression analysis for variables associated with Verbal Violence (n=446)
| Step 1 | Step 2 | Step 3 | Step 4 | |||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Variable | OR1 | 95% CI2 | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Demographic | ||||||||
| Age (Reference 20–29) | ||||||||
| 30–39 | 1.41 | 0.72–2.75 | 1.46 | 0.74–2.88 | 1.39 | 0.69–2.79 | 1.29 | 0.62–2.67 |
| 40–49 | 0.96 | 0.53–1.71 | 1.06 | 0.59–1.93 | 1.03 | 0.56–1.90 | 0.95 | 0.51–1.78 |
| 50–59 | 0.61 | 0.33–1.12 | 0.71 | 0.38–1.32 | 0.63 | 0.33–1.21 | 0.69 | 0.35–1.35 |
| >60 | 0.55 | 0.27–1.15 | 0.65 | 0.31–1.38 | 0.65 | 0.30–1.39 | 0.72 | 0.33–1.57 |
| Gender (Reference Female) | ||||||||
| Male | 1.22 | 0.62–2.38 | 1.23 | 0.62–2.44 | 1.33 | 0.67–2.66 | 1.45 | 0.70–2.98 |
| Jobcat3 (Reference other) | ||||||||
| Registered Nurse | 1.87** | 1.14–3.09 | 1.67 | 0.99–2.79 | 1.90* | 1.12–3.23 | 1.90* | 1.10–3.28 |
| Patient Care Associate | 1.12 | 0.48–2.58 | 1.06 | 0.45–2.52 | 0.98 | 0.40–2.42 | 0.84 | 0.33–2.12 |
| Mental Health Technician | 1.07 | 0.27–4.25 | 1.20 | 0.29–4.93 | 1.15 | 0.27–4.80 | 0.92 | 0.20–4.36 |
| Security | 4.71** | 1.64–13.5 | 5.01** | 1.70–14.79 | 6.12** | 2.03–18.44 | 7.37** | 2.37–22.91 |
| Work Stress | 1.02*** | 1.01–1.03 | 1.01* | 1.01–1.03 | 1.01 | 0.99–1.02 | ||
| Staff Interaction | ||||||||
| Interpersonal Conflict | 1.56* | 1.11–2.19 | 1.49* | 1.04–2.12 | ||||
| Efficiency | 1.00 | 0.99–1.01 | 1.01 | 0.99–1.02 | ||||
| Teamwork | 0.80 | 0.60–1.06 | 0.90 | 0.66–1.21 | ||||
| Safety Climate | ||||||||
| Violence Prevention Climate | 0.48*** | 0.36–0.65 | ||||||
|
| ||||||||
| Nagelkerke R2 | 0.078 | 0.118 | 0.163 | 0.232 | ||||
OR1 = Odds ratio 95% CI2 = 95% Confidence intervals Jobcat3 = Job category
p<.05.
p<.01.
p<.001
Registered nurses and security staff were at increased risk for verbal violence in every step, but neither age nor gender was associated with verbal violence.
Table 5 summarizes the logistic regression analysis with physical violence as the dependent variable. In the first step, being older than 60 years of age reduced the risk of physical violence (OR 0.29, p<.05), while registered nurses (OR 2.89, p<.01), mental health technicians (OR 15.26, p<.01), and security staff (OR 23.11, p<.001) were all at increased risk. The demographic and job-related variables in the first step explained 22.9% of the variance in physical violence (Nagelkerke R2 = .229). In the second step, work stress was added to the model and was a significant risk factor for physical violence (OR 1.02, p<.01). The second model explained 25.7% of the variance in physical violence (Nagelkerke R2 = .257). The three staff interaction variables were added in the third step. Efficiency was inversely associated with physical violence (OR .98, p<.05), while work stress was no longer significant. Neither interpersonal conflict nor teamwork were significantly associated with physical violence. The third model explained 27.5% of the variance (Nagelkerke R2 = .275). Violence prevention climate, the safety climate variable, was added in the final step and was inversely associated with physical violence (OR 0.60, p<.05), increasing the overall explained variance to 30.4% (Nagelkerke R2 = .304). In this final model, efficiency maintained its significance (OR 0.98, p<.05).
Table 5.
Summary of Logistic Regression analysis for variables associated with Physical Violence (n=446)
| Step 1 | Step 2 | Step 3 | Step 4 | |||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Variable | OR1 | 95% CI2 | OR | 95% CI | OR | 95% C.I | OR | 95% CI |
| Demographic | ||||||||
| Age (Reference 20–29) | ||||||||
| 30–39 | 0.58 | 0.28–1.19 | 0.58 | 0.28–1.20 | 0.55 | 0.26–1.16 | 0.50 | 0.23–1.06 |
| 40–49 | 0.82 | 0.44–1.54 | 0.91 | 0.49–1.72 | 0.82 | 0.43–1.56 | 0.79 | 0.41–1.53 |
| 50–59 | 0.57 | 0.28–1.15 | 0.64 | 0.31–1.33 | 0.59 | 0.28–1.25 | 0.66 | 0.31–1.41 |
| >60 | 0.29* | 0.11–0.77 | 0.34* | 0.13–0.91 | 0.29* | 0.11–0.79 | 0.31* | 0.11–0.86 |
| Gender (Reference Female) | ||||||||
| Male | 1.89 | 0.94 3.80 | 1.98 | 0.98–4.02 | 1.93 | 0.94–3.94 | 2.05 | 0.99–4.26 |
| Jobcat3 (Reference other) | ||||||||
| Registered Nurse | 2.89** | 1.39–6.00 | 2.66** | 1.27–5.57 | 2.67* | 1.26–5.64 | 2.72* | 1.27–5.80 |
| Patient Care Associate | 2.18 | 0.75–6.30 | 2.03 | 0.68–6.03 | 2.26 | 0.74–6.90 | 2.15 | 0.68–6.74 |
| Mental Health Technician | 15.26** | 3.17–73.4 | 19.27*** | 3.78–98.18 | 18.26** | 3.48–95.81 | 18.71** | 3.35–104.49 |
| Security | 23.11*** | 7.21–74.1 | 25.32*** | 7.75–82.77 | 25.80*** | 7.67–86.78 | 30.79*** | 8.92–106.29 |
| Work Stress | 1.02** | 1.01–1.03 | 1.01 | 1.00–1.03 | 1.01 | 0.99–1.02 | ||
| Staff Interaction | ||||||||
| Interpersonal Conflict | 0.86 | 0.59–1.26 | 0.80 | 0.54–1.18 | ||||
| Efficiency | 0.98* | 0.97–0.99 | 0.98* | 0.97–0.99 | ||||
| Teamwork | 1.11 | 0.81–1.52 | 1.25 | 0.90–1.75 | ||||
| Safety Climate | ||||||||
| Violence Prevention Climate | 0.60* | 0.45–0.82 | ||||||
|
| ||||||||
| Nagelkerke R2 | 0.229 | 0.257 | 0.275 | 0.304 | ||||
OR1 = Odds ratio 95% CI2 = 95% Confidence intervals Jobcat3 = Job category
p<.05.
p<.01.
p<.001
Registered nurses (OR 2.72, p ≤ .05), mental health technicians (OR 18.71, p ≤ .01), and security staff (OR 30.79, p ≤ .001) were at increased risk for physical violence in every step of the model, while age above 60 years was protective (OR 0.31, p<.05). In an effort to better understand these demographic results, we examined the job category variable and all scales by age. Worker job categories differed significantly by age group (Chi square 59.67, p<.001), with a greater proportion of employees older than 60 among security and mental health technicians, compared to the other job categories. We also examined mean scale scores by age category, using one-way analysis of variance (ANOVA) with Bonferroni post-hoc tests. There were statistically significant differences across age groups for work stress (F=5.76, p=.000) and violence prevention climate (F=5.83, p=.000), but not for any of the staff interaction variables (interpersonal conflict F=1.08, p=.365; efficiency F=1.07, p=.370; teamwork F=2.22, p=.066). Compared to younger employees, employees older than 60 rated work stress significantly lower and violence prevention climate significantly higher.
Discussion
This study aimed to examine the effect of work stress, staff interaction and organizational safety climate variables on self-reported verbal and physical workplace violence in a sample of hospital workers. We hypothesized that all of these factors would be associated to some degree with reported violence, regardless of type, however not all variables were significant in the respective final models. When controlling for demographics, only one of the staff interaction variables, interpersonal conflict, was associated with an increased likelihood of verbal violence. In our four-step model, neither efficiency nor teamwork was significant when entered in step 3 or in the final step. Work stress, while significant in steps 2 and 3 of the model, was no longer significant when the safety climate variable was added in the final step. Violence prevention climate was inversely associated with verbal violence, with higher ratings associated with a significantly lower likelihood of verbal violence exposure. Nurses and security staff were consistently at increased risk for verbal violence in all four steps of the model, while neither age nor gender was significant.
With regard to physical violence, both efficiency and violence prevention climate were inversely associated and thus protective against physical violence. Efficiency was the only significant staff interaction variable, and it maintained significance when violence prevention climate was added to the model in the final step. Work stress, initially a positive risk factor in step 2, was no longer significant when efficiency was added to the model in step 3. As with verbal violence, nurses and security staff were at risk in all four steps of the model, although mental health technicians were also at increased risk for physical violence. Employees older than 60 had a significantly decreased risk of physical violence in all four steps. Importantly, the demographic and job category variables alone accounted for nearly 23% of the variance in physical violence, compared to less than 8% in the verbal violence regression. Thus, demographic and job category variables accounted for the greatest proportion of the overall explained variance (30%) in our model of physical violence, while neither age nor gender was significant in the final model for verbal violence.
These results suggest that organizational efforts to reduce workplace violence should include reducing conflict and incivility among hospital staff, improving work processes and work flow, and enhancing management encouragement of reporting of, and proactive response to, violent events.
Interpersonal conflict was positively and significantly associated with verbal violence. However, due to the cross-sectional study design, it is not possible to discern whether coworker conflict was a cause of, or result of, violent events. One possible explanation is that interpersonal conflict among colleagues leads to negative emotional reactions32 that can cause victims to become less engaged in their work, leading to frustrated patients who may become aggressive.40 Previous research has reported that coworker violence and incivility are common in hospital environments, often caused by work-related factors related to unprofessional behavior or conflicts regarding work organization and routines.41
Our findings regarding physical violence confirm previous studies that have identified mental health technicians,42 security personnel,42-43 and registered nurses42-43 as being at increased risk. Yet our study goes a step further in identifying high levels of work efficiency and violence prevention climate as protective, malleable organizational factors. Efficiency measures how well hospital workers plan and carry out their work, incorporating elements of coworker support and collaboration. Our findings support those of a Swedish study, where work efficiency ratings were significantly lower among hospital worker victims of patient violence, compared to non-victims.40 In a study of organizational determinants of safety climate in nursing homes, efficiency predicted nonpunitive response to errors, which indicated a more positive safety climate.17 This provides some support for the fact that both efficiency (well-functioning work processes) and violence prevention climate (management support for safety from violence) were significant inverse determinants of physical violence in the current study. The findings are in line with previous research in psychiatric settings, where employee positive perceptions of management’s commitment to safety were associated with fewer patient aggressive incidents.25 However, that study did not measure management’s commitment specifically to worker safety regarding violence. In a longitudinal study, positive violence prevention climate ratings predicted a decreased likelihood of being exposed to violence over six months.38 However, significance was only found for one subscale, which was not measured in the current study. Moreover, that study involved only nurses (n=176). In our study, working as a registered nurse or as security staff increased the likelihood of exposure to verbal and physical violence, while mental health technicians were at increased odds for physical violence. In both models, odds ratios were greatest for security staff.
Efficiency was inversely associated with physical violence, implying that high worker scores on efficiency are protective against physical violence. In recent research, organizational efficiency was negatively and significantly associated with co-worker incivility, a form of non-physical violence, among nursing staff.44-45 Based on this research, we had expected low levels of interpersonal conflict and high levels of efficiency and teamwork to protect against violence. While interpersonal conflict was associated with verbal violence, efficiency was only associated with physical violence, and teamwork was not associated with either form of violence. Our findings thus partially support previous work that found that teamwork, supportive colleagues, and perceptions of work safety were inversely related to workplace violence among Australian nurses.46 However, violence in that study was broadly defined as aggression and/or workplace harassment/bullying.
Workplace violence has been identified as a stressor for healthcare workers10 but little research has explored work stress as a possible cause of violence. Job demands, often considered a proxy for work stress,47 were significantly associated with violent threats towards physicians in a Taiwanese study,24 which supports findings in the current study. However, in that study, safety climate ratings were also significantly protective of threats, whereas in our study, work stress was only significant before the safety climate variable was added to the model for verbal violence. Regarding physical violence, work stress lost significance when efficiency was added to the model and remained insignificant when violence prevention climate was added in the final step. Our findings suggest that efficiency and violence prevention climate are stronger determinants of physical workplace violence than work stress.
Limitations
This study was cross-sectional so that it is not possible to ascertain causality, i.e., whether work stress, poor interpersonal relationships, and a low-rated violence prevention climate are causes of, or the results of, violence experienced by health care workers. A second limitation is the low response rate (23%). However, as reported, analyses revealed that questionnaire respondents did not differ significantly from non-respondents with regard to age or gender,7 which limits threats to internal validity. Moreover, a previous study of this population found that respondents did not differ significantly from non-respondents with regard to formal documentation of workplace violence events.7 Nevertheless, it is not known whether non-respondents differed from respondents in their experience of workplace violence or would have rated the independent variables (work stress, staff interaction, and safety climate) significantly differently from respondents. Finally, this study was conducted within a single hospital system among units previously identified as being at increased risk for workplace violence towards staff and may not be generalizable to other hospital settings. However, this was a large, metropolitan hospital system with urban and suburban locations, which may increase generalizability to other healthcare contexts.
Conclusion
The results of this study confirmed that staff interaction and safety climate variables were both associated with reported workplace violence among hospital workers, whereas work stress was not. Interpersonal conflict among hospital coworkers increased the likelihood of exposure to verbal violence, while efficiency among hospital coworkers decreased the likelihood of exposure to physical workplace violence. A positive violence prevention climate decreased the likelihood of both verbal and physical violence. Interventions focused on improving these organizational factors may help to reduce workplace violence towards hospital workers.
Acknowledgments
Source of Funding: This study was funded by The Centers for Disease Control-National Institute for Occupational Safety and Health [CDC-NIOSH], grant number R01 OH009948. The content is solely the responsibility of the authors and does not necessarily represent the official views of CDC-NIOSH.
Footnotes
Conflicts of Interest: The QWC survey instrument is owned and marketed by the Swedish company Springlife AB. Dr. B. Arnetz is the cofounder and co-owner of this company.
References
- 1.Dressner M. Hospital workers: an assessment of occupational injuries and illnesses Monthly Labor Review. U.S. Bureau of Labor Statistics; 2017. . Accessed December 21, 2017. [DOI] [Google Scholar]
- 2.Gates DM, Ross CS, McQueen L. Violence against emergency department workers. J Emerg Med. 2006;31(3):331–337. doi: 10.1016/j.jemermed.2005.12.028. [DOI] [PubMed] [Google Scholar]
- 3.Pompeii L, Dement J, Schoenfisch A, et al. Perpetrator, worker and workplace characteristics associated with patient and visitor perpetrated violence (Type II) on hospital workers: a review of the literature and existing occupational injury data. J Safety Res. 2013;44:57–64. doi: 10.1016/j.jsr.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 4.Phillips JP. Workplace violence against health care workers in the United States. N Engl J Med. 2016;374(17):1661–1669. doi: 10.1056/NEJMra1501998. [DOI] [PubMed] [Google Scholar]
- 5.Occupational Safety and Health Administration (OSHA) Understanding the challenge. OSHA; 2015. Workplace violence in healthcare; p. 3826. Available at: https://www.osha.gov/Publications/OSHA3826.pdf. Accessed January 19, 2017. [Google Scholar]
- 6.Bureau of Labor Statistics. Employer-reported workplace injuries and illnesses – 2016–2017. USDL-17-1482. Available at: https://www.bls.gov/news.release/osh.nr0.htm. Accessed January 19, 2017.
- 7.Arnetz JE, Hamblin L, Ager J, et al. Underreporting of workplace violence: comparison of self-report and actual documentation of incidents in hospital settings. Workplace Health Saf. 2015b;51(2):200–210. doi: 10.1177/2165079915574684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lanctot N, Guay S. The aftermath of workplace violence among healthcare workers: A systematic literature review of the consequences. Aggress Violent Behav. 2014;19:492–501. [Google Scholar]
- 9.Berry PA, Gillespie GL, Gates D, Schafer J. Novice nurse productivity following workplace bullying. J Nurs Scholarsh. 2012;44(1):80–87. doi: 10.1111/j.1547-5069.2011.01436.x. [DOI] [PubMed] [Google Scholar]
- 10.Gates DM, Gillespie GL, Succop P. Violence against nurses and its impact on stress and productivity. Nurs Econ. 2011;29(2):59–67. [PubMed] [Google Scholar]
- 11.Vessey JA, Demarco RF, Gaffney DA, Budin WC. Bullying of staff registered nurses in the workplace: A preliminary study for developing personal and organizational strategies for the transformation of hostile to healthy workplace environments. J Prof Nurs. 2009;25:299–306. doi: 10.1016/j.profnurs.2009.01.022. [DOI] [PubMed] [Google Scholar]
- 12.Gerberich SG, Church TR, McGovern PM, Hansen HE, Nachreiner NM, Geisser MS, Ryan AD, Mongin SJ, Watt GD. An epidemiological study of the magnitude and consequences of work related violence: the Minnesota Nurses’ Study. Occup Environ Med. 2004;61:495–503. doi: 10.1136/oem.2003.007294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gillespie GL, Gates DM, Miller M, Howard PK. Workplace violence in healthcare settings: risk factors and protective strategies. Rehabil Nurs. 2010;35(5):177–184. doi: 10.1002/j.2048-7940.2010.tb00045.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arnetz JE, Hamblin L, Essenmacher L, Upfal MJ, Ager J, Luborsky M. Understanding patient-to-worker violence in hospitals: a qualitative analysis of documented incident reports. J Adv Nurs. 2015a;71(2):338–348. doi: 10.1111/jan.12494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hamblin LE, Essenmacher L, Ager J, Upfal MJ, Luborsky L, Russell J, Arnetz JE. Worker-to-worker violence in hospitals: Perpetrator characteristics and common dyads. Workplace Health & Safety. 2015b;64(2):51–56. doi: 10.1177/2165079915608856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gerberich SG, Church TR, McGovern PM, Hansen H, Nackreiner NM, Geisser MS, Ryan AD, Mongin SJ, Watt GD, Jurek A. Risk factors for work-related assaults on nurses. Epidemiology. 2005;16(5):704–709. doi: 10.1097/01.ede.0000164556.14509.a3. [DOI] [PubMed] [Google Scholar]
- 17.Arnetz JE, Zhdanova LS, Elsouhag D, Lichtenberg P, Luborsky MR, Arnetz BB. Organizational climate determinants of resident safety culture in nursing homes. Gerontologist. 2011;51(6):739–749. doi: 10.1093/geront/gnr053. [DOI] [PubMed] [Google Scholar]
- 18.Flin R. Measuring safety culture in healthcare: a case for accurate diagnosis. Safety Science. 2007;45:653–667. [Google Scholar]
- 19.Sorra JS, Nieva VF. Hospital Survey on Patient Safety Culture. Rockville, MD: Agency for Healthcare Research and Quality; Sep, 2004. (AHRQ Publication No. 04-0041). (Prepared by Westat, under Contract No. 290-96-0004) Accessed December 20, 2017. [Google Scholar]
- 20.Mearns KJ, Flin R. Assessing the state of organizational safety – culture or climate? Current Psychology. 1999;18(1):5–17. [Google Scholar]
- 21.Neal A, Griffin MA, Hart PC. The impact of organizational climate on safety climate and individual behavior. Safety Science. 2000;34:99–109. [Google Scholar]
- 22.Zohar D. A group-level model of safety climate: testing the effect of group climate on microaccidents in manufacturing jobs. Journal of Applied Psychology. 2000;85(4):587–596. doi: 10.1037/0021-9010.85.4.587. [DOI] [PubMed] [Google Scholar]
- 23.McGonagle AK, Essenmacher L, Hamblin L, Luborsky M, Upfal M, Arnetz J. Management commitment to safety, teamwork, and hospital worker injuries. J Hosp Adm. 2016;5(6):564–570. doi: 10.5430/jha.v5n6p46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wu J-C, Tung T-H, Chen PY, Chen Y-L, Lin Y-W, Chen F-L. Determinants of workplace violence against clinical physicians in hospitals. J Occup Health. 2015;57:540–547. doi: 10.1539/joh.15-0111-OA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Isaak V, Vashdi D, Bar-Noy D, Kostisky H, Hirschmann S, Grinshpoon A. Enhancing the safety climate and reducing violence against staff in closed hospital wards. Workplace Health & Safety. 2017;65(9):409–416. doi: 10.1177/2165079916672478. [DOI] [PubMed] [Google Scholar]
- 26.Camerino D, Estryn-Behar M, Conway PM, van Der Heijden BIJM, Hasselhorn H-M. Work-related factors and violence among nursing staff in the European NEXT study: a longitudinal cohort study. International Journal of Nursing Studies. 2008;45:35–50. doi: 10.1016/j.ijnurstu.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 27.Magnavita N. Workplace violence and occupational stress in healthcare workers: a chicken-and-egg situation. Results of a 6-year follow-up study. Journal of Nursing Scholarship. 2014;46(5):366–376. doi: 10.1111/jnu.12088. [DOI] [PubMed] [Google Scholar]
- 28.Arnetz JE, Hamblin L, Ager J, Aranyos D, Upfal MJ, Luborsky M, Russell J, Essenmacher L. Application and implementation of the hazard risk matrix to identify hospital workplaces at risk for violence. Am J Ind Med. 2014;57(11):1276–1284. doi: 10.1002/ajim.22371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Arnetz JE, Arnetz BB. Implementation and evaluation of a practical intervention programme for dealing with violence towards health care workers. J Adv Nurs. 2000;31(3):668–680. doi: 10.1046/j.1365-2648.2000.01322.x. [DOI] [PubMed] [Google Scholar]
- 30.Arnetz BB. Physicians’ view of their work environment and organization. Psychotherapy and Psychosomatics. 1997;66:155–162. doi: 10.1159/000289127. [DOI] [PubMed] [Google Scholar]
- 31.Arnetz JE, Hasson H. Evaluation of an educational “toolbox” for improving nursing staff competence and psychosocial work environment in elderly care: Results of a prospective, non-randomized controlled intervention. International Journal of Nursing Studies. 2007;44:723–735. doi: 10.1016/j.ijnurstu.2006.01.012. [DOI] [PubMed] [Google Scholar]
- 32.Spector PE, Jex SM. Development of four self-report measures of job stressors and strain: Interpersonal Conflict at Work Scale, Organizational Constraints Scale, Quantitative Workload Inventory, and Physical Symptoms Inventory. Journal of Occupational Health Psychology. 1998;3:356–367. doi: 10.1037//1076-8998.3.4.356. [DOI] [PubMed] [Google Scholar]
- 33.Anderson LM, Pearson CM. Tit for tat? The spiraling effect of incivility in the workplace Academy of Management Review. 1999;24(3):452–471. [Google Scholar]
- 34.Anderzen I, Arnetz BB. The impact of a prospective survey-based workplace intervention program on employee health, biologic stress markers, and organizational productivity. J Occup Environ Med. 2005;47(7):671–682. doi: 10.1097/01.jom.0000167259.03247.1e. [DOI] [PubMed] [Google Scholar]
- 35.Arnetz BB, Lucas T, Arnetz JE. Organizational climate, occupational stress, and employee mental health: mediating effects of organizational efficiency. J Occup Environ Med. 2011;53(1):34–42. doi: 10.1097/JOM.0b013e3181ffo5b. [DOI] [PubMed] [Google Scholar]
- 36.Kessler SR, Spector PE, Chang C-H, Parr AD. Organizational violence and aggression: development of the three-factor Violence Climate Survey. Work & Stress. 2008:108–124. [Google Scholar]
- 37.Spector PE, Coulter M, Stockwell HG, Matz MW. Perceived violence climate: A new construct and its relationship to workplace physical violence and verbal aggression, and their potential consequences. Work & Stress. 21:117–130. [Google Scholar]
- 38.Yang LQ, Spector PE, Chang CH, Gallant-Roman M, Powell J. Psychosocial precursors and physical consequences of workplace violence towards nurses: A longitudinal examination with naturally occurring groups in hospital settings. International Journal of Nursing Studies. 2012;49:1091–1102. doi: 10.1016/j.ijnurstu.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 39.Yim O, Ramdeen KT. Hierarchical cluster analysis: comparison of three linkage measures and applicaiton to psychological data. The Quantitative Methods for Psychology. 2015;11(1):8–21. [Google Scholar]
- 40.Arnetz JE, Arnetz BB. Violence towards health care staff and possible effects on the quality of patient care. Soc Sci Med. 2001;52(3):417–427. doi: 10.1016/s0277-9536(00)00146-5. [DOI] [PubMed] [Google Scholar]
- 41.Hamblin LE, Essenmacher L, Upfal MJ, Russell J, Luborsky L, Ager J, Arnetz JE. Catalysts of worker-to-worker violence and incivility in hospitals. Journal of Clinical Nursing. 2015a;24(17):2458–2467. doi: 10.1111/jocn.12825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Arnetz JE, Aranyos D, Ager J, Upfal MJ. Development and application of a population-based system for workplace violence surveillance in hospitals. Am J Ind Med. 2011a;54:925–934. doi: 10.1002/ajim.20984. [DOI] [PubMed] [Google Scholar]
- 43.Pompeii LA, Schoenfisch AL, Lipscomb HJ, Dement JM, Smith CD, Upadhyaya M. Physical assault, physical threat, and verbal abuse perpetrated against hospital workers by patients or visitors in six U.S. hospitals. Am J Ind Med. 2015;58(11):1278–1287. doi: 10.1002/ajim.22489. [DOI] [PubMed] [Google Scholar]
- 44.Viotti S, Converso D, Hamblin L, Guidetti G, Arnetz JE. Organisational efficiency and co-worker incivility: a cross-national study of nurses in the USA and Italy. J Nurs Manag. 2018 doi: 10.1111/jonm.12587. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Viotti S, Essenmacher L, Hamblin LE, Arnetz JE. Testing the reciprocal associations among co-worker incivility, organisational inefficiency, and work-related exhaustion: a one-year, cross-lagged study. Work & Stress. doi: 10.1080/02678373.2018.1436615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hegney D, Tuckett A, Parker D, Eley RM. Workplace violence: differences in perceptions of nursing work between those exposed and those not exposed: a cross-sector analysis. Int J Nurs Pract. 2010;16(4):352–358. doi: 10.1111/j.1440-172X.2010.01829.x. [DOI] [PubMed] [Google Scholar]
- 47.Bosma H, Peter R, Siegrist J, Marmot M. Two alternative job stress models and the risk of coronary heart disease. Am J Pub Health. 1998;88:68–74. doi: 10.2105/ajph.88.1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]


