Abstract
We present a patient who experienced insufflation of air under the left eyelid when using continuous positive airway pressure (CPAP) via an oronasal mask. The patient had a lacrimal stent in place for many years, which was a predisposing factor for this complication. Lacrimal stents are frequently used in the treatment of epiphora (excessive tearing) secondary to obstruction of the lacrimal drainage system. In this case, we review the pathophysiology of air regurgitation into the eye with CPAP use and methods previously described to address this rare complication. We also present a novel intervention for this rare complication, the total face mask. By additionally covering the eyes, a total face mask allows equalization of pressure on both sides of the lacrimal system. With a total face mask, our patient was able to successfully use CPAP.
Citation:
Wrede JE, Parsons EC, Watson NF. A novel treatment for nasolacrimal air regurgitation into the eye with CPAP: the total face mask. J Clin Sleep Med. 2018;14(8):1415–1417.
Keywords: lacrimal stent, Lester Jones tube, Jones tube, canalicular tube, air reflux, air regurgitation, CPAP, positive airway pressure, total face mask
INTRODUCTION
Continuous positive airway pressure (CPAP) therapy is typically safe and well tolerated, with common side effects being discomfort or skin irritation related to mask fit or air leak around the nose or mouth. An uncommon side effect of CPAP therapy is air regurgitation into the eye, which occurs due to retrograde airflow through the lacrimal apparatus.1–11 Anatomical disruption of the lacrimal system from nasolacrimal duct surgery or lacrimal stent placement increases risk for this rare complication.
REPORT OF CASE
A 48-year-old male presented for sleep apnea evaluation with two years of snoring, unrefreshing sleep, 60-pound weight gain, and excessive daytime sleepiness with an Epworth Sleepiness Scale (ESS) score of 11/24. Pertinent past medical history included a major motor vehicle collision 32 years prior with facial fractures that required multiple surgeries including nasal bridge reconstruction. A home sleep apnea test (HSAT) revealed obstructive sleep apnea with an apnea-hypopnea index (AHI) of 26.1 events/h, with a 3% desaturation index of 25.8 events/h, and oxygen saturation nadir of 78%. Treatment was initiated with an autotitrating positive airway pressure (APAP) range of 5–20 cmH2O using an oronasal mask (commonly referred to as a full face mask).
In a subsequent clinic follow-up, the patient reported symptomatic improvement with CPAP, feeling “more rested than I have in years.” However, he reported an unusual side effect: when using CPAP, his left eyelid would “blow-up like a balloon.” When he opened his eyes, the air would escape. If he opened his eyes with the CPAP mask in place, air would consistently reflux out of his eye. On further history, the patient revealed that he had a Jones tube, a type of lacrimal stent, placed in his left eye after a motor vehicle accident (Figure 1).
Figure 1. Patient's Jones tube and associated anatomy.
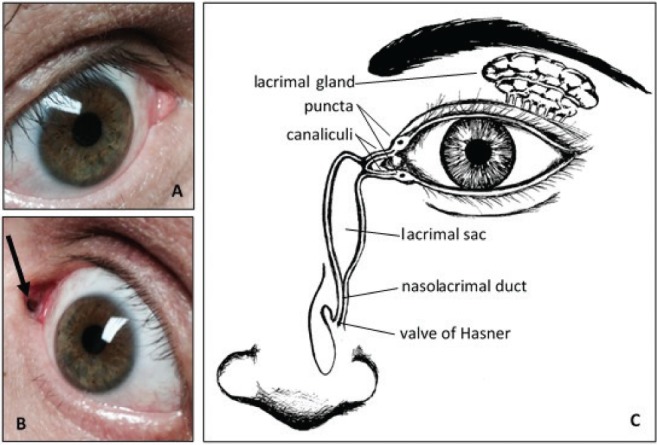
(A) Unaffected right eye. (B) Jones tube in the location of the puncta of the left eye (arrow). (C) Lacrimal drainage system anatomy. Illustration courtesy of Rebecca Kim, MD.
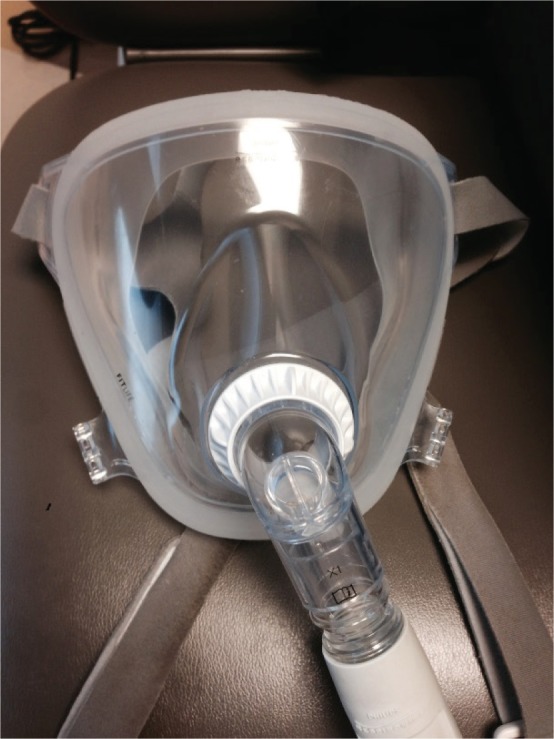
We advised the patient to use Provent nasal strips instead of APAP pending ophthalmology evaluation. The patient reported inferior clinical response to Provent compared to APAP, and ophthalmology opted not to remove the nasolacrimal duct stent, due to concerns that scarring had likely occurred since placement. We then instructed the patient to resume APAP with a so-called “total face mask,” covering the nose, mouth, and eyes (Figure 2).
Figure 2. Patient's total face mask.
On subsequent follow-up, the patient reported that he felt much better since resuming APAP; he had his old personality back and was not as tired during the day. His quality of life was much improved and he was satisfied with his treatment. When queried, he rated his satisfaction with CPAP as 10/10, sleep improvement as 10/10 and Epworth Sleepiness Scale score was now normal at 2/24. A 30-day APAP download revealed adequate adherence, with device usage 90% of nights, averaging 4 hours and 44 minutes per night, with an APAP mean pressure of 9 cmH2O and a normal residual AHI of 3.7 events/h.
DISCUSSION
The lacrimal apparatus functions to maintain a balance of tears for protection of the cornea and conjunctiva.11 Tears produced by the lacrimal gland spread across the eye through blinking, are drained via puncta in the upper and lower eyelids, then proceed through canaliculi to the lacrimal sac, after which they continue through the nasolacrimal duct into the nasopharynx via the inferior meatus, just behind the inferior nasal turbi-nate (Figure 1C). Valves and mucous membrane folds along the system, and to a lesser degree gravity, serve to encourage normal flow and impede retrograde flow through this system.11 Use of CPAP therapy with a standard nasal or oronasal mask may create sufficient pressure differential between the nose and eye to overcome these regulatory mechanisms, allowing retrograde flow of air or fluid from the nose to the eye. Patients whose lacrimal anatomy has been disrupted by surgery may be particularly at risk for this rare complication.
A Jones tube (also known as a Lester Jones tube) is a glass tube measuring approximately 1 cm in length and 3–4 mm in diameter. Similar tubes may be made of polyethylene or silicone. Jones tube placement requires a surgical procedure called a dacryocystorhinostomy (DCR), which creates a new drainage channel from the lacrimal sac to the nose. Inserted through the medial canthus, the Jones tube maintains this new drainage track to the nose.
CPAP intolerance from air regurgitation has been described as a complication of Jones tube placement and DCR. Ali et al. retrospectively identified 10 CPAP users among 205 consecutive patients undergoing DCR. Seventy percent of the CPAP users complained of air regurgitation into the eye after DCR, and 50% discontinued CPAP as a consequence of their symptoms.1 Cannon et al. performed a retrospective case review of 4 patients complaining of air regurgitation with CPAP. Two of the patients had undergone DCR only and two patients had additional Jones tube placement. Only the patient who had Jones tube removal had resolution of air regurgitation; for the others, air regurgitation persisted despite lowering or varying CPAP pressures.2
Published methods to address air regurgitation after Jones tube placement have focused on either transitioning patients to non-CPAP therapies, or physical occlusion of the tube. Plum et al. transitioned their patient to a mandibular advancement device.3 Longmire et al. reported their patient was able to avoid air reflux symptoms and discontinue CPAP through weight loss.4 Goldberg describes, after unsuccessful trials of variously inserting an angiocath, soft silicon tubing, and a piece of soft foam, ultimately the patient was successful using a wet piece of rolled up cotton taped over the tube.5 One motivated patient created his own alginate mold of his periorbital region which attached to his CPAP mask and covered his Jones tube.6
Rarely, air regurgitation has been described in patients without lacrimal instrumentation.7–9 Symptoms were controlled with a variety of surgical and nonsurgical techniques, including inferior turbinate out-fracture,9 decreased CPAP pressure,7,9 use of an oronasal mask instead of nasal mask,9 placement of a punctum plug,8 and use of a nasopharyngeal airway (ie, nasal trumpet) for nocturnal self-administration.9
A treatment that has not been previously described is use of a total face mask. This type of mask (examples include the Philips Respironics brand Total Face Mask and FitLife models) is a less frequently used mask option that covers the mouth, nose and eyes. It is recommended as an option for patients who may not be able to obtain a good seal with a nasal or oronasal mask, experience skin breakdown due to pressure on sensitive areas, or who are claustrophobic. In a patient prone to lacrimal air regurgitation, covering the eyes allows air pressure to equilibrate across the Jones tube, prevents air regurgitation, and allows successful CPAP use.
In summary, air regurgitation into the eye is a rare complication of CPAP therapy, which may be more common among those with disrupted lacrimal anatomy. A number of interventions have been trialed to overcome this complication. In our case, the use of a total face mask was an effective and well-tolerated novel solution.
DISCLOSURE STATEMENT
Work for this study was performed through the UW Medicine Sleep Center at Harborview Medical Center, Seattle, WA. All authors have seen and approved the manuscript. The authors report no conflicts of interest.
REFERENCES
- 1.Ali MJ, Psaltis AJ, Murphy J, Wormald PJ. Endoscopic dacryocystorhinostomy and obstructive sleep apnoea: the effects and outcomes of continuous positive airway pressure therapy. Clin Exp Ophthalmol. 2015;43(5):405–408. doi: 10.1111/ceo.12483. [DOI] [PubMed] [Google Scholar]
- 2.Cannon PS, Madge SN, Selva D. Air regurgitation in patients on continuous positive airway pressure (CPAP) therapy following dacrocystorhinostomy with or without Lester-Jones tube insertion. Br J Ophthalmol. 2010 Jul;94(7):891–893. doi: 10.1136/bjo.2009.166082. [DOI] [PubMed] [Google Scholar]
- 3.Plum M, Pfirman K, Endara-Bravo A. Lacrimal duct air regurgitation in an adult patient on continuous positive airway pressure therapy. J Lung Pulm Respir Res. 2016;3(6) 00107. [Google Scholar]
- 4.Longmire MR, Carter KD, Allen RC. Intolerance of jones tube placement in a patient using continuous positive airway pressure. Ophthal Plast Reconstr Surg. 2010;26:68–69. doi: 10.1097/IOP.0b013e3181b80d9d. [DOI] [PubMed] [Google Scholar]
- 5.Goldberg DS. Management of air regurgitation through a jones tube in a patient using continuous positive airway pressure. Ophthal Plast Reconstr Surg. 2011;27:e76–e77. doi: 10.1097/IOP.0b013e3181ed3820. [DOI] [PubMed] [Google Scholar]
- 6.Cartwright MJ, Frueh BR. Keratoconjunctivitis sicca in a patient with a Jones tube to treat sleep apnea. Am J Ophthalmol. 1992;114(2):234–235. doi: 10.1016/s0002-9394(14)73999-6. [DOI] [PubMed] [Google Scholar]
- 7.Zandieh S, Katz ES. Retrograde lacrimal duct airflow during nasal positive pressure ventilation. J Clin Sleep Med. 2010;6(6):603–604. [PMC free article] [PubMed] [Google Scholar]
- 8.Goktas O, Haberman A, Thelen A, Schrom T. [The punctum plug as an option for treating retrograde air flow from the lacrimal sac] Laryngorhinootologie. 2007;86:732–735. doi: 10.1055/s-2007-966511. [DOI] [PubMed] [Google Scholar]
- 9.Singh NP, Walker RJ, Cowan F, Davidson AC, Roberts DN. Retrograde air escape via the nasolacrimal system: a previously unrecognized complication of continuous positive airway pressure in the management of obstructive sleep apnea. Ann Otol Rhinol Laryngol. 2014;123(5):321–324. doi: 10.1177/0003489414525924. [DOI] [PubMed] [Google Scholar]
- 10.Harrison W, Pence N, Kovacich S. Anterior segment complications secondary to continuous positive airway pressure machine treatment in patients with obstructive sleep apnea. Optometry. 2007;78(7):352–355. doi: 10.1016/j.optm.2006.12.015. [DOI] [PubMed] [Google Scholar]
- 11.Vicinanzo MG, Allamneni C, Compton CJ, Long JA, Nabavi CB. The prevalence of air regurgitation and its consequences after conjunctivodacryocystorhinostomy and dacryocystorhinostomy in continuous positive airway pressure patients. Ophthal Plast Reconstr Surg. 2015;31(4):269–271. doi: 10.1097/IOP.0000000000000280. [DOI] [PubMed] [Google Scholar]
- 12.Maliborski A, Różycki R. Diagnostic imaging of the nasolacrimal drainage system. Part I. Radiological anatomy of lacrimal pathways. Physiology of tear secretion and tear outflow. Med Sci Monit. 2014;20:628–638. doi: 10.12659/MSM.890098. [DOI] [PMC free article] [PubMed] [Google Scholar]


