Abstract
BACKGROUND
The aim of this study was describing the sampling methods and sample size of the Isfahan Healthy Heart Program (IHHP) and its sub-studies in focus.
METHODS
The IHHP was carried out between 2000 and 2007 in urban and rural areas in 3 districts, namely Isfahan and Najafabad (as the intervention areas), and Arak (as the reference area), Iran. It consisted of the 3 phases of baseline surveys during 2000-2001, interventions between 2002 and 2005, and post-intervention surveys during 2006-2007 on 4 target groups (adults, health professionals, cardiac patients, children, and adolescents). During 2002 to 2005, 4 evaluation studies were conducted to evaluate short-term results. An ongoing cohort study entitled the Isfahan Cohort Study was performed on those aged ≥ 35 years at baseline in 2001 to access the risk of cardiovascular disease (CVD) occurrence.
RESULTS
Using stratified random cluster methods, 12514, 5891, 4793, 6096, 3012, and 9572 adults and 1946, 1999, 1427, 1223, 389, and 1992 adolescents were chosen in the 1st to 3rd phases. Furthermore, simple random sampling was used for selecting 923, 694, 1000, and 2015 health professionals and 814, 452, 420, and 502 cardiac patients. A multistage sampling method was adopted for the collection of samples from parents of preschoolers and primary school children aged 2-10 years, adolescents’ parents, and some teachers. A prospective cohort study was started on 6504 eligible individuals.
CONCLUSION
The IHHP, as a comprehensive community-based interventional trial in Iran, among the few population-based studies around the world, has reasonable sampling methods and sample size.
Keywords: Cardiovascular Disease, Sample Size, Sampling Design, Isfahan Healthy Heart Program
Introduction
Cardiovascular disease (CVD) is the leading cause of mortality and morbidity all over the world. More than 80% of deaths due to CVD take place in low- and middle-income countries.1 Moreover, the CVD health burden is increasing in almost all countries, particularly in developing nations.2
CVD is responsible for a considerable proportion of the mortality and morbidity among the Iranian population. According to reports by the Iranian Ministry of Health and Medical Education, death from CVD is the first leading cause of mortality and morbidity in Iran.3
Epidemiologic transition from infectious to chronic diseases, as well as the aging of the population, in developing countries is exacerbating the burden of chronic non-communicable diseases (CNCDs). Such diseases account for 80% of the total burden of mortality due to CNCDs in these countries. The prevention and control of CNCDs would avert 24 million deaths in low-income and middle-income countries over the next decades.4
Prevention of CVDs is the most effective way of combating the CVDs epidemic in less developed and developing nations.5 Earlier studies have revealed that interventional population-based programs were effective on improving health promotion knowledge and behaviors. The successful development and implementation of a health promotion program depends upon the identification of the scope and breadth of baseline knowledge among the targeted population members.1,6-12 Lack of a reliable design, well defined target population, good sampling design, and adequate sample size may impede all administrative efforts targeted at the promotion of prevention as well as adoption of healthy lifestyle changes.
Numerous community-based trials have been conducted in developed countries including the US and Finland and have resulted in significant decreases in the risk of CNCDs and deaths due to coronary heart disease (CHD). However, there are few reports of such trials in the developing world.8-10,12 Due to the increasing prevalence of CVD and its large burden in Iran in recent years, conducting such comprehensive interventions can provide a good pilot or feasibility study to implement large-scale preventive programs at a national level.
The Isfahan Healthy Heart Programý (IHHP) was designed and launched in 2000. This study was aimed to modify population lifestyle and risk factors of the disease and was also intended to enhance the knowledge, attitude, and practice of individuals (adults, adolescents and their parents, children and their parents, school teachers, health professionals, and cardiac patients) in relation to the risk factors of CVD. Furthermore, it introduced ways to prevent and control these diseases and their risk factors. This program provided an opportunity to assess whether lifestyle interventions are effective or not in a developing country. The program targeted individuals, the community, and environmental changes to support health behavior modification. Many report papers have been published on the whole design, methods, and evaluation components and on assessing the feasibility and outcomes of IHHP with brief referral to sample size and sampling methods.13-35 However, no comprehensive report is available regarding the sampling strategies and sample size of IHHP and its sub-studies. The current paper describes the sampling strategies, and sample size for IHHP and its sub-studies in detail.
Materials and Methods
Sampling methods and sample size
The IHHP was carried out between 2000 and 2007 in urban and rural areas in 3 districts, namely Isfahan and Najafabad (as the intervention areas) and Arak (as the reference area), Iran.14,15 The IHHP consisted of 3 phases: assessing the current situation in intervention and reference areas (baseline survey), implementing intervention activities only in the intervention areas, and assessing the post-intervention situation in the intervention and reference areas (post-intervention survey).
Phase 1: Baseline survey in 2000-2001
It was a cross-sectional survey on the current status of community in relation to knowledge, attitude, and practice (KAP) in a variety of fields, including nutrition, smoking, and physical activity, on each of the 4 target groups including adult, health professionals like physicians, nurses, health workers, and health volunteers, adolescents aged 11-18 years in intermediate and high schools, their parents and some school teachers, and cardiac patients. The study also investigated the status of cardiometabolic risk factors such as high lipid levels, hypertension, diabetes, and obesity. Blood samples were only collected from adults and adolescents.
Phase 2: Intervention activities between 2002 and 2005
The IHHP intervention phase consisted of 10 projects targeting different groups and various interventions. These projects were implemented for a period of 4 years. By using both population and high risk strategies for CVD prevention, these projects integrate the interventions and policies that address the promotion of healthy lifestyle behaviors, as major determinants of CNCDs, such as healthy diet, tobacco control, physical activity, and stress management among participants in the intervention areas. During 2002 to 2005, 4 independent evaluation studies were performed to evaluate short-term results like knowledge and behavior changes in each of the 4 target groups. In addition, random samples of parents of preschoolers and primary school children aged 2-10 years were evaluated from this phase onwards.
Phase 3: Post-intervention surveys in 2006-2007
Similar to phase 1, a study was conducted on independent random samples to determine the effects of interventions on each target group.14,15
The remainder of this section is devoted to a detailed description of the target population (adult, health professionals, adolescents aged 11-18 years in junior high school and high school, their parents and some teachers and school staff, as well as parents of preschoolers and primary school children aged 2-10 years, and cardiac patients) and sample size, sampling methods, and evaluated variables for each of the 4 target groups.
1. Adults group
Target population: adults (over 19 years old)
Sample size and sampling methods: In the adult group, a multistage sampling was conducted. Initially, quota sampling of the population of Isfahan to Najafabad was considered (i.e., 3:1). Then, stratified sampling was conducted based on age, sex, and urban and rural areas. The sample size in different age groups (19-24, 25-34, 35-44, 45-54, 55-64, and 65 years and older) were determined based on the age distribution of the population in baseline and post-intervention surveys (in evaluation studies in 2002-2005, similar to MONICA method, an equal number was considered for each age group). Furthermore, by considering the equal gender distribution of the population in Iran, an equal sample size was selected from among men and women. In addition, the number of subjects in urban and rural areas of each district was determined based on population distribution. Then, multistage cluster sampling was used based on clusters of the provincial health center. Accordingly, the clusters of each of the urban and rural areas in Isfahan, Najafabad, and Arak were randomly selected from different health centers. Then, the sample was assigned to every cluster based on the number of households covered. Households were then selected in each cluster using systematic sampling and the questionnaire was randomly completed for a person over 19 years of age in the famil.
Considering p1 = 20%, p2 = 15%, d = 0.05, and β = 10%, about 12514 and 9572 people were selected based on the proportional to size estimation formula from intervention and reference areas, in the 1st and 3rd phase, respectively. In the selection process, equal ratios in sex, accuracy of cluster sampling in both phases, and the missing rate of samples (about 30%) for cohort surveys in the 1st phase were also taken into account. Sex-based and age-based CINDI protocol sampling methods were used for sample size determination in the annual intervention phases.14,15 The total sample size and details of sampling methods in different phases of the IHHP study are presented in table 1. In addition, table 2 presents the distribution of the studied sample sizes in the adult group.
Table 1.
Sampling in the Isfahan Healthy Heart Program: Size and Method
| Target Population | Population Definition | Sample Frame | First Phase (Baseline) 2001 |
Second Phase (Impact evaluation) 2002-2005 |
Third Phase (Outcome) 2006-2007 |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sampling Method | Sample Size | Details | Sampling Method | Sample Size | Details | Sampling Method | Sample Size | Details | |||
| Adults Population | Age ≥ 19 years | Adult population in interventional and reference communities | Multistage Sampling: quota, stratified, cluster, random, probability proportionate to size, systematic, random | 12514 | Sampling based on age, sex, and residency (Urban/Rural) distribution in population | Multistage Sampling: quota, stratified, cluster, random, probability proportionate to size, systematic, random | 5891 | - The 4th phase was performed only in the interventional area | Multistage Sampling: quota, stratified, cluster, random, probability proportionate to size, systematic, random | 9572 | Sampling based on age, sex, and residency (Urban/Rural) distribution in population |
| 4793 | |||||||||||
| 6096 | - Sampling based on sex and residency (Urban/Rural) distribution in population | ||||||||||
| 3012 | - Similar to Monika’s method, an equal number was considered for each age-group | ||||||||||
| Pediatrics surveys Adolescents | Age: 11-18 years | Intermediate and high schools in interventional and reference communities | Multistage Sampling: quota, stratified, cluster, random, probability proportionate to size, random ,random | 1946 | Sampling based on grade, sex, and residency (Urban/Rural) distribution in population | Multistage Sampling: quota, stratified, cluster, random, probability proportionate to size, random ,random | 1999 | -The 4th phase was performed only in the interventional area | Multistage Sampling: quota, stratified, cluster, random, probability proportionate to size, random ,random | 1992 | Sampling based on grade, sex, and residency (Urban/Rural) distribution in population |
| 1427 | |||||||||||
| 1223 | - Sampling based on sex, and residency (Urban/Rural) distribution in population | ||||||||||
| 389 | - Similar to Monika’s method, an equal number was considered for each age-group | ||||||||||
| Pediatrics surveys Children | Age: 2-10 years | Health Centers/ kindergarten/ primary schools in interventional and reference communities | Multistage Sampling: quota, stratified, cluster, random, probability proportionate to size, random ,random | 0 | Sampling based on grade, sex, and residency (Urban/Rural) distribution in population | Multistage Sampling: quota, stratified, cluster, random, probability proportionate to size, random ,random | 1998 | -The 4th phase was performed only in the interventional area | Multistage Sampling: quota, stratified, cluster, random, probability proportionate to size, random ,random | 1914 | Sampling based on grade, sex, and residency (Urban/Rural) distribution in population |
| 1754 | |||||||||||
| 1542 | - Sampling based on sex, and residency (Urban/Rural) distribution in population | ||||||||||
| 431 | - Similar to Monika’s method, an equal number was considered for each age-group | ||||||||||
| Adolescents Parents | No limitation | Intermediate / high school in interventional and reference communities | Multistage Sampling: quota, stratified, cluster, random, probability proportionate to size, random ,random | 1946 | - | Multistage Sampling: quota, stratified, cluster, random, probability proportionate to size, random ,random | 1999 | -The 4th phase was performed only in the interventional area | Multistage Sampling: quota, stratified, cluster, random, probability proportionate to size, random ,random | 1984 | - |
| 1303 | |||||||||||
| 1163 | |||||||||||
| 342 | |||||||||||
| Teachers | No limitation | Kindergarten/primary/ intermediate / high school in interventional and reference communities | Multistage Sampling: quota, stratified, cluster, random | 398 | - | Multistage Sampling: quota, stratified, cluster, random | 201 | -The 4th phase was performed only in the interventional area | Multistage Sampling: quota, stratified, cluster, random | 425 | - |
| 327 | |||||||||||
| 436 | |||||||||||
| 181 | |||||||||||
| Health Professionals | General Physician/Nurses/Health workers | Health centers/ hospitals/ educational courses in interventional and reference communities | Random Sampling | 923 | - | Random Sampling | 694 | - | Random Sampling | 2015 | - |
| 1000 | |||||||||||
| Patients | Patients hospitalized during 9-12 months before the survey (IHD/CeVD) | Surveillance Data File for CAD and CeVD in ICRC Surveillance Department in interventional and reference communities | Random Sampling | 814 | - | Random Sampling | 452 | - | Random Sampling | 502 | - |
| 420 | |||||||||||
IHD: Ischemic heart disease; CeVD: Cerebrovascular disease; ICRC: International Committee of the Red Cross; CAD: Coronary artery disease
Table 2.
Distribution of the sample size in adult group of Isfahan Healthy Heart Program
| Isfahan Healthy Heart Program Adults Population | First Phase (Baseline) sample size 2001 | Second Phase (Impact Evaluation) sample size 2002-2005 |
Third Phase (Outcome) sample size 2006-2007 | ||||
|---|---|---|---|---|---|---|---|
| 1st | 2nd | 3rd | 4th | ||||
| Area | Intervention | 6175 (49.3) | 2994 (50.8) | 2400 (50.1) | 3014 (49.4) | 3012 (100.0) | 4719 (49.3) |
| Reference | 6339 (50.7) | 2897 (49.2) | 2393 (49.9) | 3082 (50.6) | 0(0) | 4853 (50.7) | |
| Residency | Urban | 9093 (72.7) | 4370 (74.2) | 3506 (73.1) | 4521 (74.2) | 2652 (88.0) | 6692 (69.9) |
| Rural | 3421 (27.3) | 1521 (25.8) | 1287 (26.9) | 1575 (25.8) | 360 (12.0) | 2880 (30.1) | |
| Sex | Female | 6391 (51.1) | 2993 (50.8) | 2424 (50.6) | 3112 (51.2) | 1558 (51.7) | 4786 (50.0) |
| Male | 6123 (48.9) | 2898 (49.2) | 2369 (49.4) | 2971 (48.8) | 1453 (48.3) | 4786 (50.0) | |
| Age groups (year) | 19-24 | 2310 (18.5) | 1175 (19.9) | 967 (20.2) | 971 (16.0) | 427 (14.2) | 1886 (19.7) |
| 25-34 | 3662 (29.3) | 1202 (20.4) | 969 (20.2) | 1042 (17.1) | 540 (17.9) | 2913 (30.5) | |
| 35-44 | 2717 (21.7) | 1201 (20.4) | 958 (20.0) | 1025 (16.9) | 512 (17.0) | 1898 (19.8) | |
| 45-54 | 1628 (13.0) | 1137 (19.3) | 946 (19.7) | 1030 (16.9) | 509 (16.9) | 1174 (12.3) | |
| 55-64 | 1130 (9.0) | 671 (11.4) | 501 (10.5) | 986 (16.2) | 492 (16.3) | 757 (7.9) | |
| > 65 | 1067 (8.5) | 505 (8.6) | 452 (9.4) | 1029 (16.9) | 530 (17.6) | 937 (9.8) | |
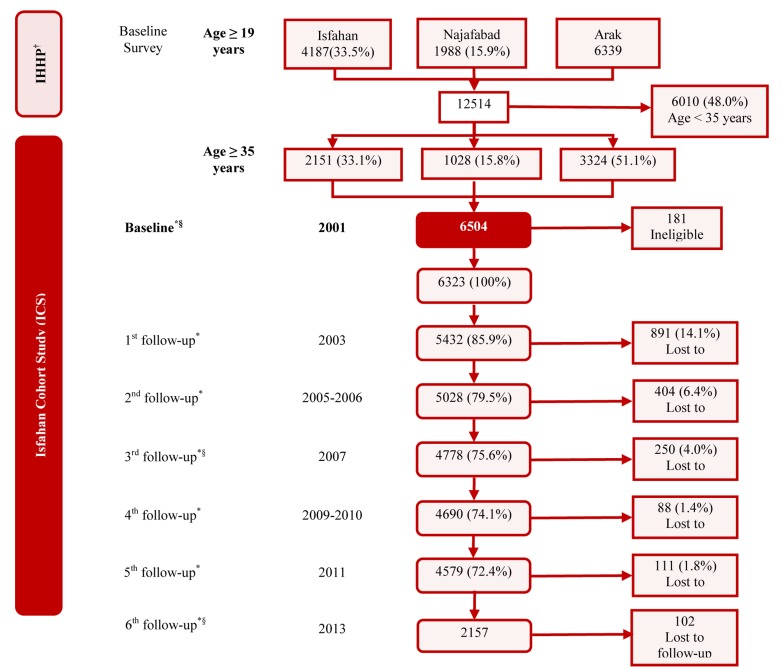
All participants aged over 35 years (n = 6504) living in both areas who took part in the 1st phase of the IHHP were asked to participate in a 10-year longitudinal study named Isfahan Cohort Study (ICS).26 This study was aimed to determine the individual impact of interventions, the incidence of cardiovascular events, and the Iranian risk assessment chart. It is essential to mention that a telephone follow-up interview was performed every 2 years. CVD events such as fatal and nonfatal myocardial function (MI) and stroke, stable and unstable angina, and sudden cardiac death were expressed in telephone interviews and were confirmed by performing verbal autopsy. In addition to the initial questionnaire of the adults’ study of the IHHP in 2000-2001 which was completed for ICS participants, a questionnaire similar to the one used at the beginning of the study was completed for them in 2006-2007 and
2013-2014. The sampling method of this study was similar to the adult sub-study of IHHP. Details of the follow-up phone calls and interviews as well as the number of people followed-up in the ICS were published elsewhere.26 The new version of the diagram of this cohort study is presented in figure 1.
Figure 1.
Isfahan Cohort Study † Isfahan Healthy Heart Program * Telephone interview asking for (CVD) events (being confirmed with medical records). § Full Interview including demographics, socioeconomic status, lifestyle and biochemical examinations were carried out.
Evaluated variables in the adults group: In this study, the questionnaires were developed based on the World Health Organization (WHO) STEPwise approach (STEPS) and measurements were designed based on WHO standards. In some parts of the questionnaire, besides maintaining the structure of STEPS, additional questions have been completed for respondents. In general, the questionnaires included demographic data (i.e., age, sex, education, occupation, and marital status), questions related to KAP on nutrition, physical activity, smoking, stress levels, and how to cope with stress as well as quality of life (QOL) and other behavioral risk factors.14,15 To determine the nutritional practice of individuals, a standard food frequency questionnaire with appropriate reliability and validity was completed.36 Furthermore, a 24-hour recall was completed for a subsample of about 2000 participants for each of the 1st and 2nd phases.37,38 Past history and physical and paraclinical examination that included questions about the history of CVD risk factors, such as diabetes, hypertension, hyperlipidemia, and family history of heart diseases, as well as Rose’s questionnaire for chest pain were also considered. For those who were over 35 years of age, an electrocardiogram (ECG) was performed and standard Minnesota codes were used for ECG interpretation and analysis. These 2 were performed in the 1st and last phases. Additionally, all cardiometabolic factors such as weight, height, waist and hip circumferences, systolic and diastolic blood pressure, cholesterol (total, LDL, and HDL), apolipoproteins A and B, triglycerides, 2-hour and fasting blood glucose, complete blood count (CBC), and C-reactive protein (CRP) were measured for all adults aged over 19 years in the 1st and last phases.14,15
2. Children, adolescents, parents, and teachers groups
Target population: Parents of preschoolers and primary school children aged 2-10 years, adolescents aged 11-18 years in intermediate and high school, adolescents’ parents, and some teachers
Sample size and sampling methods: A multistage sampling method was adopted for the collection of samples from kindergartens, preschools, primary schools, intermediate schools, and high schools, reported by the Department of Education based on the urban and rural areas of Isfahan, Najafabad, and Arak. We determined the sampling quota of Isfahan population to Najafabad (two-thirds to one third) and stratified samples based on gender distribution, level of education, and urban and rural population distribution. Then, clusters were randomly selected from schools of urban and rural areas of the intervention and reference areas. Sampling size in each school was determined with probability proportional to the size of each school. Finally, the random selections of classes from each school as well as students from the classes included in the random sampling process were conducted.
Considering the proportional sample size estimation formula and sampling accuracy of 10%, the minimum proportion of 0.3, and type I error of 5%, sample size was estimated. The sample sizes from the 1st to the 3rd phases (totally in the intervention and reference areas), were 1946, 1999, 1427, 1223, 389, and 1992 students aged 11-18 years, 1946, 1999, 1303, 1163, 342, and 1984 parents of students, and 398, 201, 327, 436, 181, and 425 teachers including managers, schoolmasters, health teachers, school counselors, and biology teachers, respectively. It should be noted that, random samples were also drawn from among 2-10-year-old children in preschools and primary schools along with one of their parents in the intervention and post intervention surveys.
In the second and third phases (totally in the intervention and reference areas), there were 1998, 1754, 1542, 431, 1914 parents of children.13-15,27,29,30,32 The total sample size and sampling details of all phases of the IHHP in the target population are presented in table 1. In addition, the distribution of the sample size in the study structure is shown in table 3; this was done based on the items involved in the sampling.
Table 3.
Distribution of the sample size in adolescents, children, and teachers of Isfahan Healthy Heart Program
| Isfahan Healthy Heart Program | First Phase (Baseline) sample size 2001 | Second Phase (Impact Evaluation) sample size 2002-2005 |
Third Phase (Outcome) sample size 2006-2007 | |||||
|---|---|---|---|---|---|---|---|---|
| 1st | 2nd | 3rd | 4th | |||||
| Adolescents | Area | Intervention | 969 (49.8) | 1000 (50.03) | 629 (44.1) | 516 (42.2) | 389 (100.0) | 972 (48.8) |
| Reference | 977 (50.2) | 999 (50.00) | 798 (55.9) | 707 (57.8) | 0 (0) | 1020 (51.2) | ||
| Residency | Urban | 1251 (64.3) | 1320 (66.00) | 1085 (76.0) | 837 (68.4) | 321 (82.5) | 1532 (76.9) | |
| Rural | 695 (35.7) | 679 (34.00) | 342 (24.0) | 386 (31.6) | 68 (17.5) | 460 (23.1) | ||
| Gender | Girl | 1001 (51.4) | 999 (50.00) | 732 (51.7) | 658 (57.7) | 193 (54.8) | 978 (49.1) | |
| Boy | 945 (48.6) | 1000 (50.00) | 683 (48.3) | 482 (42.3) | 159 (45.2) | 1014 (50.9) | ||
| Grade | Middle school | 986 (50.7) | 1000 (50.02) | 774 (54.7) | 618 (50.5) | 203 (52.2) | 1039 (52.2) | |
| High school | 960 (49.3) | 999 (49.98) | 641 (45.3) | 605 (49.5) | 186 (47.8) | 953 (47.8) | ||
| Children | Area | Intervention | 0 (0) | 1000 (50.10) | 671 (38.3) | 584 (37.9) | 431 (100.0) | 972 (50.8) |
| Reference | 998 (49.90) | 1083 (61.7) | 958 (62.1) | 0(0) | 942 (49.2) | |||
| Residency | Urban | 1998 (100.00) | 1477 (84.2) | 1206 (78.2) | 399 (92.6) | 1475 (77.1) | ||
| Rural | 277 (15.8) | 336 (21.8) | 32 (7.4) | 439 (22.9) | ||||
| Gender | Girl | 998 (49.90) | 919 (52.6) | 774 (51.1) | 194 (45.8) | 933 (48.7) | ||
| Boy | 1000 (50.10) | 829 (47.4) | 740 (48.9) | 230 (54.2) | 981 (51.3) | |||
| Grade | Preschool | 987 (49.70) | 831 (47.5) | 649 (42.1) | 155 (36.0) | 922 (48.2) | ||
| Elementary school | 1000 (50.30) | 920 (52.5) | 892 (57.9) | 275 (64.0) | 989 (51.8) | |||
| Teachers | Area | Intervention | 201 (50.5) | 200 (100.00) | 209 (63.9) | 306 (70.2) | 181 (100.0) | 193 (45.4) |
| Reference | 197 (49.5) | 0 (0) | 118 (36.1) | 130 (29.8) | 0 (0) | 232 (54.6) | ||
| Headmaster | 398 (100) | 201 (100.00) | 30 (9.2) | 53 (14.2) | 23(15.1) | 64 (15.1) | ||
| Schoolmaster | 53 (16.2) | 55 (14.7) | 36 (23.7) | 72 (16.9) | ||||
| School consultant | 10 (3.1) | 42 (11.2) | 20 (13.2) | 51 (12.0) | ||||
| Biology teacher | 9 (2.8) | 17 (4.5) | 5 (3.3) | 14 (3.3) | ||||
| Sport coach | 216 (66.1) | 26 (7.0) | 11 (7.2) | 16 (3.8) | ||||
| Health coach | 3 (0.9) | 13 (3.5) | 2 (1.3) | 5 (1.2) | ||||
| Other teachers | 0 (0) | 168 (44.9) | 55 (36.2) | 192 (45.2) | ||||
Evaluated variables in Children, adolescents, parents, and teachers groups: Due to the diversity of the studied groups, 4 types of questionnaires were designed for the following groups: parents of preschool and primary school children, intermediate and high school students, parents of intermediate school and high school students, and school teachers. After obtaining written consent from parents of children and adolescents, a questionnaire which consist of demographic questions, knowledge, attitude and practice about risk factors, as well as the importance, prevention, and control of these risk factors from childhood were completed. Then, specific questions about food frequency for all children and adolescents were completed. Measurements of weight, height, waist and hip circumferences, systolic and diastolic blood pressure, total cholesterol, LDL, HDL, triglycerides, and fasting blood glucose in the 1st and 3rd phases as well as apolipoproteins A and B in the third phase were taken from 11-18-year-old students.13-15,27,29,30,32
3. Health professionals group
Target population: Health professionals including physicians, nurses, health workers, and primary health workers
Sample size and sampling methods in health professionals group: By simple random-sampling method from among health professionals, the sample sizes for the 1st and 3rd phases were estimated as 923 and 2015 individuals, respectively (totally for both the intervention and reference areas).14,15,18,34 The total sample size and sampling details of all phases for the IHHP in this target group is presented in table 1. Similarly, the distribution of sample size in the study structure is presented in table 4.
Table 4.
Distribution of the sample size in patients and health professionals of the Isfahan Healthy Heart Program
| Isfahan Healthy Heart Program | First Phase (Baseline) sample size 2001 | Second Phase (Impact Evaluation) sample size 2002-2005 |
Third Phase (Outcome) sample size 2006-2007 | |||||
|---|---|---|---|---|---|---|---|---|
| 1st | 2nd | 3rd | 4th | |||||
| Patients | Area | Intervention | 269 (33.0) | 0 (0) | 0 (0) | 252 (55.8) | 249 (59.3) | 250 (49.8) |
| Reference | 545 (67.0) | 200 (44.2) | 171 (40.7) | 252 (50.2) | ||||
| Sex | Female | 379 (46.6) | 177 (41.5) | 169 (41.1) | 235 (47.2) | |||
| Male | 435 (53.4) | 250 (58.5) | 242 (58.9) | 263 (52.8) | ||||
| Health Professionals | Area | Intervention | 512 (55.5) | 376 (54.2) | 500 (50.0) | 1482 (73.5) | ||
| Reference | 411 (44.5) | 318 (45.8) | 500 (50.0) | 533 (26.5) | ||||
| Primary health workers | 262 (28.4) | 191 (27.5) | 0 (0) | 0 (0) | 200 (20.0) | 993 (49.3) | ||
| Junior health workers | 200 (21.7) | 94(13.6) | 0 (0) | 172 (8.5) | ||||
| Senior health workers | 149 (16.1) | 218 (31.4) | 200 (20.0) | 128 (6.3) | ||||
| Health volunteers | 312 (33.8) | 0 (0) | 0 (0) | 180 (8.9) | ||||
| Nurses | 0(0) | 0 (0) | 200 (20.0) | 542 (27.0) | ||||
| Physicians | 0 (0) | 191 (27.5) | 400 (40.0) | 0 (0) | ||||
Evaluated variables in health professionals group: To gather data, specific questionnaires, with more than 50 questions for physicians, 40 for nurses, and 50 questions for primary health workers, were used.
The questionnaires contained questions about the KAP of health care providers regarding suitable nutrition, smoking cessation, physical activity, prevention and control of CVD, and pharmacological and non-pharmacological treatments.14,15,18,34
4. Cardiac patients group
Target population: Patients with a history of myocardial infarction (MI), stroke, coronary artery bypass grafting (CABG), percutaneous coronary angioplasty (PCI), and patients with a history of hospitalization due to cardiovascular attacks
Sample size and sampling methods in cardiac patients group: In this study, simple random sampling was implemented among cardiac patients referred to medical centers. Based on the proportional to size estimation formula and the sampling accuracy of 10%, the minimum proportion of 0.3, and type I error of 5%, the sample size was estimated. The sample sizes for the 1st and 3rd phases were estimated to be 814 and 502 (totally for the intervention and reference areas), and 452 and 420 patients in the annual intervention phases, respectively.14,15,22 The total sample size and sampling details of all phases of the IHHP in the mentioned target group are provided in table 1. In addition, the distribution of sample size in the study structure is presented in table 4.
Evaluated variables in cardiac patients group: In this study, the questions regarding KAP, measurement of height, weight, systolic and diastolic blood pressure, total cholesterol, LDL, HDL, triglycerides, fasting blood glucose, apolipoproteins A and B, and CRP, as well as questions on morbidity including the number of visits to a doctor, re-hospitalization, medication, diagnostic procedures, days of absenteeism from work due to disability, open-heart surgery, and PCI were answered for each participant.14,15,22
Results
We chose 12514, 5891, 4793, 6096, 3012, and 9572 adults and 1946, 1999, 1427, 1223, 389, and 1992 adolescents using stratified random cluster method in the 1st to 3rd phases. Moreover, simple random sampling was used to select 923, 694, 1000, 2015 health professionals and 814, 452, 420, 502 cardiac patients. A multistage sampling method was adopted for collection of samples from parents of preschoolers and primary school children aged 2-10 years, adolescents’ parents and some teachers. Prospective cohort study was started on 6504 eligible people.
Discussion
CVD is a leading cause of death throughout the world, which is increasingly growing not only in industrialized, but also developing countries that are affected by significant changes in lifestyle due to rapid industrialization.39 A number of community CVD prevention programs have been implemented over the last 40 years. A systematic review reported that there were a number of well-known community CVD prevention programs such as Stanford Three Community Study, Stanford Five-City Project, The Minnesota Heart Health Program, and The North Karelia Project; but this systematic review identified an unexpectedly large number of additional programs, and many of these have not been featured in previous systematic reviews.6
The Stanford Three Community Study was conducted in 1972 to investigate the risk factors of CVD through a health promotion program in 2 cities of the State of California as the intervention and in 1 city as the reference area. In 1978, in the framework of the Stanford Three Community Study in California, a quasi-experimental study was carried out on the general population aged 12-74 years in Northern California, called the Stanford Five-City Project. This study was aimed to assess changes in the prevalence of risk factors for CVDs, and morbidity and mortality due to CVDs based on the implementation of a major community-based intervention program. This program was carried out in the form of 4 annual cross-sectional studies with independent samples, and a longitudinal study with repeated measurements using a 6-year educational intervention (1980-1986) on all people of the intervention area as well as follow-up until 1992. In this study, with random assignment, the 2 cities of Monterey (n = 43400) and Salinas (n = 80500) were considered as the intervention areas and the 3 cities of Modesto (n = 132400), San Luis Obispo (n = 343000), and Santa Maria (n = 39700) were chosen as the reference areas. In this study, households of intervention and reference areas were randomly selected, and then, all members of the households aged 12-74 years were invited to participate in the study.7,11
The Minnesota Heart Health Program is another intervention program that was conducted as a non-randomized community-based study for primary prevention of CVDs and stroke from 1980 to 1990 on the general population aged 25-74 years, children in 6th-10th grade, and employees of 119 participating companies. This 5-6-year quasi-experimental intervention program at the community and individual levels was conducted on 400 thousand people in 6 selected communities from Minnesota and North and South Dakota in Northwestern United States. In this program, the intervention and reference areas were matched in terms of population size (25,000 to 110,000), the type of community (small and medium rural and urban areas), and the distance to a metropolitan area. However, the allocation of communities to the intervention and reference areas was non-random. The sample sizes throughout the study were about 231,222 people in the intervention area and 181,149 in the reference area. In this program, risk factors and behaviors were measured before starting the intervention program; furthermore, they were annually followed-up for 6-7 years in all 6 communities. Some cross-sectional studies in the framework of the Minnesota Heart Health Program were conducted periodically with a random selection of people in each community using a 2-stage cluster sampling method. The cohort study of this program consisted of participants randomly selected from all cross-sectional studies (before the beginning of the intervention).8,10
The North Karelia Project started in 1972, as one of the world’s most successful intervention studies in Finland, it aimed to change people’s lifestyles and control and prevent the major risk factors for CVDs. After the implementation of the original project and obtaining preliminary results during 1972-1977, the experiences of this program were used to implement a national action and preventive activities throughout the country. The cross-sectional studies of this project were carried out in the province of North Karelia as the intervention area and in the province of Kuopio as a reference area, once every 5 years in 1972, 1977, 1982, 1987, and 1992. In each cross-sectional study, a random sample was selected for each province from the national population register system. In studies during 1972 and 1977, each sample contained a population of 6.6% born between the years 1913 and 1947; however, the other 3 cross-sectional studies in 1982, 1987, and 1992 consisted of people of 25-64 years of age. These samples were classified so that in each area at least 250 people were selected from each gender and each 10-year age group of 25-34, 35-44, 45-54, and 55-64. The investigated sample sizes in the 2 provinces of intervention and reference in 1972, 1977, 1982, 1987, and 1992 were 9882, 10012, 5712, 4512, and 3012, respectively.9,12
In Iran, few intervention studies have been conducted to prevent heart diseases and their risk factors. The Tehran Lipid and Glucose Study was developed to determine the risk factors for atherosclerosis; in addition, it was aimed to modify people’s lifestyle and prevent the growing trend of diabetes, dyslipidemia, and other risk factors for CVDs. The design of this study consisted of 2 main phases: the 1st phase was a cross-sectional study to determine the prevalence of risk factors for CVDs and the 2nd phase consisted of a cohort, prospective, intervention which began in January 2002. Both of the intervention and reference areas were selected from the same district in Tehran, Iran. A total of 15,005 residents of Tehran aged 3-69 years with the same age and sex distribution were selected using a multistage cluster sampling from district 13 (1 out of 22 districts) of Tehran. The participants were covered by 3 primary health care centers (out of 20 health care centers in this district) and entered the baseline cross-sectional study. People, who participated in the 1st phase of this cross-sectional study, were followed up in the intervention phase in order to improve the lifestyle of the population and prevent non-communicable diseases (NCD) risk factors. The target groups of these interventions included 5630 participants from students, housewives, and people at risk covered by 1 of the 3 sampling health care centers. The reference group included 9375 people who were covered by the other 2 health centers.39
The IHHP is the most comprehensive integrated community-based interventional study in Iran and is similar to many well-known studies specifically to the North Karelia Project in Finland. It was launched in 1999 and started in 2000 with a quasi-experimental design, a control area, and multiple levels of evaluation. The intervention areas were both urban and rural areas within Isfahan and Najafabad, while the control area was Arak located in Markazi Province which is at a distance of 375 km from the intervention areas. A notable feature of this study was the performance of various interventions on the whole population of more than 2 million in the intervention areas through 10 different projects in terms of target groups including the general population, students of primary, intermediate, and high schools (aged 2-18 years), their parents, teachers, and school staff, and cardiac patients and health professionals, including physicians, nurses, health workers, and primary health workers. Another feature was its emphasis on suitable nutrition, smoking cessation, physical activity, and copying strategies. The third notable feature was that both cross-sectional studies with independent samples were performed in the 2 pre-intervention and post-intervention phases and 4 cross-sectional studies within the intervention phase during a period of 6 years, and a 20-year longitudinal study was started in 2001 with repeated measurements to calculate the risk assessment chart for CVD occurrence. The other features were its intervention and reference areas, and collection of an immense amount of information regarding demographic characteristics, socioeconomic conditions, knowledge, attitude and practice regarding CVD risk factors, lifestyle, stress and ways to cope with it, QOL, medical and family history, physical and paraclinic examinations, and physical and biochemical measurements.
According to the established criteria about well-designed interventional population-based CVD studies in the literature review, the IHHP could be considered a reasonable study in terms of the aspect of sample size in its sub-studies as shown in table 1. Furthermore, the IHHP had reliable multistage sampling methods taking into account the structure of each sub-community. These were quota, stratified, cluster, random, probability proportionate to size, systematic and simple random in adults. They were quotas, stratified, cluster, random, probability proportionate to size, simple random, and simple random in adolescents and their parents and teachers. Moreover, simple random sampling was used in health professionals and patients with cardiac diseases. It is worth noting that the IHHP had full coverage of the included study areas in sampling and reliable sample size from each age and sex group, and residential (urban or rural) area through a well-designed sampling process.14,15,19,40-42 However, in a study such as the Minnesota Heart Health Program on adults, surveys were conducted periodically in each community with a 2-stage cluster sampling design. Initially, census blocks were randomly selected from each city, with the probability of selection proportional to the expected number of households. Geographically adjacent groups of 5 households were randomly selected from within the selected blocks. Within households, a single age-eligible adult was selected at random.8,10 In the North Karelia Project, for each cross-sectional survey in the included province, a random sample was drawn from the national population registry. The sample selection was performed in a stratified framework in which at least 250 subjects of each sex and 10 year age group (25-34, 35-44, 45-54, and 55-64 years) were chosen in each area.9,12 In the Stanford study, after considering each included city as intervention or control areas, random samples from among residents aged 18-74 years who lived in the 4 central cities in California were selected.7,11
Conclusion
The experience and results of the IHHP in Iran will support the idea that a well-planned community-based program is practical and feasible, and can have a major impact on lifestyle and risk factors to reduce CVD rates in the community.
Acknowledgments
The IHHP was supported in part by grant No 31309304 from the National Organization for Management and Budget as a national research project, the Deputy of Health in the Ministry of Health in Iran, Isfahan Cardiovascular Research Center, Isfahan Provincial Health Center, and Isfahan University of Medical Sciences. Hereby, we would like to extend our sincere gratitude and appreciation to the staff of health care centers in both Isfahan and Markazi Provinces for their collaborations, and the respectful staff of the Iranian Heart Foundation.
Footnotes
Conflicts of Interest
Authors have no conflict of interests.
REFERENCES
- 1.Gaziano T, Reddy KS, Paccaud F, Horton S, Chaturvedi V. Disease Control Priorities in Developing Countries. 2nd. Washington, DC: World Bank Publications; 2006. Cardiovascular Disease. [Google Scholar]
- 2.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khosravi A, Aghamohamadi S, Kazemi E, Pour Malek F, Shariati M. Mortality profile in Iran (29 provinces) over the years 2006 to 2010. Tehran, Iran: Ministry of Health and Medical Education; 2013. In Persian. [Google Scholar]
- 4.Abegunde DO, Mathers CD, Adam T, Ortegon M, Strong K. The burden and costs of chronic diseases in low-income and middle-income countries. Lancet. 2007;370(9603):1929–38. doi: 10.1016/S0140-6736(07)61696-1. [DOI] [PubMed] [Google Scholar]
- 5.Talaei M, Sarrafzadegan N, Sadeghi M, Oveisgharan S, Marshall T, Thomas GN, et al. Incidence of cardiovascular diseases in an Iranian population: The Isfahan Cohort Study. Arch Iran Med. 2013;16(3):138–44. [PubMed] [Google Scholar]
- 6.Pennant M, Davenport C, Bayliss S, Greenheld W, Marshall T, Hyde C. Community programs for the prevention of cardiovascular disease: a systematic review. Am J Epidemiol. 2010;172(5):501–16. doi: 10.1093/aje/kwq171. [DOI] [PubMed] [Google Scholar]
- 7.Farquhar JW, Fortmann SP, Maccoby N, Haskell WL, Williams PT, Flora JA, et al. The stanford five-city project: Design and methods. Am J Epidemiol. 1985;122(2):323–34. doi: 10.1093/oxfordjournals.aje.a114104. [DOI] [PubMed] [Google Scholar]
- 8.Luepker RV, Murray DM, Jacobs DR, Mittelmark MB, Bracht N, Carlaw R, et al. Community education for cardiovascular disease prevention: Risk factor changes in the Minnesota Heart Health Program. Am J Public Health. 1994;84(9):1383–93. doi: 10.2105/ajph.84.9.1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vartiainen E, Puska P, Pekkanen J, Tuomilehto J, Jousilahti P. Changes in risk factors explain changes in mortality from ischaemic heart disease in Finland. BMJ. 1994;309(6946):23–7. doi: 10.1136/bmj.309.6946.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Luepker RV, Rastam L, Hannan PJ, Murray DM, Gray C, Baker WL, et al. Community education for cardiovascular disease prevention. Morbidity and mortality results from the Minnesota Heart Health Program. Am J Epidemiol. 1996;144(4):351–62. doi: 10.1093/oxfordjournals.aje.a008936. [DOI] [PubMed] [Google Scholar]
- 11.Fortmann SP, Varady AN. Effects of a community-wide health education program on cardiovascular disease morbidity and mortality: The Stanford Five-City Project. Am J Epidemiol. 2000;152(4):316–23. doi: 10.1093/aje/152.4.316. [DOI] [PubMed] [Google Scholar]
- 12.Nissinen A, Berrios X, Puska P. Community-based noncommunicable disease interventions: Lessons from developed countries for developing ones. Bull World Health Organ. 2001;79(10):963–70. [PMC free article] [PubMed] [Google Scholar]
- 13.Kelishadi R, Pashmi M, Ahmadi R, Mohammad Zadeh, Sadry G, Sarrafzadegan N. Healthy Heart Program: Heart health promotion from childhood. J Qazvin Univ Med Sci. 2003;7(2):15–26. [Google Scholar]
- 14.Sarraf-Zadegan N, Sadri G, Malek AH, Baghaei M, Mohammadi FN, Shahrokhi S, et al. Isfahan Healthy Heart Programme: A comprehensive integrated community-based programme for cardiovascular disease prevention and control. Design, methods and initial experience. Acta Cardiol. 2003;58(4):309–20. doi: 10.2143/AC.58.4.2005288. [DOI] [PubMed] [Google Scholar]
- 15.Sarrafzadegan N, Baghaei A, Sadri G, Kelishadi R, Malekafzali H, Boshtam M, et al. Isfahan healthy heart program: Evaluation of comprehensive, community-based interventions for non-communicable disease prevention. Prevention and Control. 2006;2(2):73–84. [Google Scholar]
- 16.Sadeghi M, Roohafza H, Shirani S, Poormoghadas M, Kelishadi R, Baghaii A, et al. Diabetes and associated cardiovascular risk factors in Iran: The Isfahan Healthy Heart Programme. Ann Acad Med Singapore. 2007;36(3):175–80. [PubMed] [Google Scholar]
- 17.Sarrafzadegan N, Kelishadi R, Baghaei A, Hussein Sadri, Malekafzali H, Mohammadifard N, et al. Metabolic syndrome: An emerging public health problem in Iranian women: Isfahan Healthy Heart Program. Int J Cardiol. 2008;131(1):90–6. doi: 10.1016/j.ijcard.2007.10.049. [DOI] [PubMed] [Google Scholar]
- 18.Bahonar A, Khosravi A, Esmaeelian H, Babak A, Sarrafzadeghan N, Rahmati M, et al. Methods of implementing the operational phases of the health professionals education project-Isfahan Healthy Heart Program (IHHP-HPEP). ARYA Atheroscler. 2009;5(3) [Google Scholar]
- 19.Sarrafzadegan N, Kelishadi R, Esmaillzadeh A, Mohammadifard N, Rabiei K, Roohafza H, et al. Do lifestyle interventions work in developing countries? Findings from the Isfahan Healthy Heart Program in the Islamic Republic of Iran. Bull World Health Organ. 2009;87(1):39–50. doi: 10.2471/BLT.07.049841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baghaei A, Sarrafzadegan N, Rabiei K, Gharipour M, Tavasoli AA, Shirani S, et al. How effective are strategies for non-communicable disease prevention and control in a high risk population in a developing country? Isfahan Healthy Heart Programme. Arch Med Sci. 2010;6(1):24–31. doi: 10.5114/aoms.2010.13503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khosravi A, Kiani Mehr G, Kelishadi R, Shirani S, Gharipour M, Tavassoli A, et al. The impact of a 6-year comprehensive community trial on the awareness, treatment and control rates of hypertension in Iran: Experiences from the Isfahan healthy heart program. BMC Cardiovascular Disorders. 2010;10:61. doi: 10.1186/1471-2261-10-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sadeghi M, Ramezani J, Sanei H, Rabeiee K, Gharipoor M, Toghianifar N. Adherence to evidence-based therapies and modifiable risk factors in patients with coronary artery disease-the hlcp project. ARYA Atheroscler. 2006;2:3. [Google Scholar]
- 23.Gharipour M, Kelishadi R, Toghianifar N, Mackie M, Yazdani M, Noori F. Sex based pharmacological treatment in patients with metabolic syndrome: Findings from the Isfahan healthy heart program. Afr J Pharm Pharmacol. 2011;5(3):311–6. [Google Scholar]
- 24.Najafian J, Toghianifar N, Mohammadifard N, Nouri F. Association between sleep duration and metabolic syndrome in a population-based study: Isfahan Healthy Heart Program. J Res Med Sci. 2011;16(6):801–6. [PMC free article] [PubMed] [Google Scholar]
- 25.Sarrafzadegan N, Rabiei K, Alavi M, Abedi H, Zarfeshani S. How can the results of a qualitative process evaluation be applied in management, improvement and modification of a preventive community trial? The IHHP Study. Arch Public Health. 2011;69:9. doi: 10.1186/0778-7367-69-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sarrafzadegan N, Talaei M, Sadeghi M, Kelishadi R, Oveisgharan S, Mohammadifard N, et al. The Isfahan cohort study: Rationale, methods and main findings. J Hum Hypertens. 2011;25(9):545–53. doi: 10.1038/jhh.2010.99. [DOI] [PubMed] [Google Scholar]
- 27.Kelishadi R, Mohammadifard N, Sarrazadegan N, Nouri F, Pashmi R, Bahonar A, et al. The effects of a comprehensive community trial on cardiometabolic risk factors in adolescents: Isfahan Healthy Heart Program. ARYA Atheroscler. 2012;7(4):184–90. [PMC free article] [PubMed] [Google Scholar]
- 28.Mohammadifard N, Sarrafzadegan N, Nouri F, Sajjadi F, Alikhasi H, Maghroun M, et al. Using factor analysis to identify dietary patterns in Iranian adults: Isfahan Healthy Heart Program. Int J Public Health. 2012;57(1):235–41. doi: 10.1007/s00038-011-0260-x. [DOI] [PubMed] [Google Scholar]
- 29.Ahmadi A, Gharipour M, Nouri F, Sarrafzadegan N. Metabolic syndrome in Iranian youths: A population-based study on junior and high schools students in rural and urban areas. J Diabetes Res. 2013;2013:738485. doi: 10.1155/2013/738485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sarrafzadegan N, Gharipour M, Sadeghi M, Nouri F, Asgary S, Zarfeshani S. Differences in the prevalence of metabolic syndrome in boys and girls based on various definitions. ARYA Atheroscler. 2013;9(1):70–6. [PMC free article] [PubMed] [Google Scholar]
- 31.Sarrafzadegan N, Kelishadi R, Sadri G, Malekafzali H, Pourmoghaddas M, Heidari K, et al. Outcomes of a comprehensive healthy lifestyle program on cardiometabolic risk factors in a developing country: The Isfahan Healthy Heart Program. Arch Iran Med. 2013;16(1):4–11. [PubMed] [Google Scholar]
- 32.Ahmadi A, Gharipour M, Nouri F, Kelishadi R, Sadeghi M, Sarrafzadegan N. Association between adolescence obesity and metabolic syndrome: Evidence from Isfahan Healthy Heart Program. Indian J Endocrinol Metab. 2014;18(4):569–73. doi: 10.4103/2230-8210.137523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Najafian J, Mohammadifard N, Naeini FF, Nouri F. Relation between usual daily walking time and metabolic syndrome. Niger Med J. 2014;55(1):29–33. doi: 10.4103/0300-1652.128156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roohafza H, Khani A, Sadeghi M, Bahonar A, Sarrafzadegan N. Health volunteers' knowledge of cardiovascular disease prevention and healthy lifestyle following a community trial: Isfahan healthy heart program. J Educ Health Promot. 2014;3:59. doi: 10.4103/2277-9531.134761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nouri F, Sarrafzadegan N, Mohammadifard N, Sadeghi M, Mansourian M. Intake of legumes and the risk of cardiovascular disease: Frailty modeling of a prospective cohort study in the Iranian middle-aged and older population. Eur J Clin Nutr. 2016;70(2):217–21. doi: 10.1038/ejcn.2015.153. [DOI] [PubMed] [Google Scholar]
- 36.Mohammadifard N, Sajjadi F, Maghroun M, Alikhasi H, Nilforoushzadeh F, Sarrafzadegan N. Validation of a simplified food frequency questionnaire for the assessment of dietary habits in Iranian adults: Isfahan Healthy Heart Program, Iran. ARYA Atheroscler. 2015;11(2):139–46. [PMC free article] [PubMed] [Google Scholar]
- 37.Hosseini E, Lachat UGent, Mohammadifard N, Sarrafzadegan N, UGent K. Associations of dietary glycemic index and glycemic load with glucose intolerance in Iranian adults. Int J Diabetes Dev Ctries. 2014;34(2):89–94. [Google Scholar]
- 38.Mohammadifard N, Mansourian M, Sajjadi F, Maghroun M, Pourmoghaddas A, Yazdekhasti N, et al. Association of glycaemic index and glycaemic load with metabolic syndrome in an Iranian adult population: Isfahan Healthy Heart Program. Nutr Diet. 2017;74(1):61–6. doi: 10.1111/1747-0080.12288. [DOI] [PubMed] [Google Scholar]
- 39.Azizi F, Ghanbarian A, Momenan AA, Hadaegh F, Mirmiran P, Hedayati M, et al. Prevention of non-communicable disease in a population in nutrition transition: Tehran Lipid and Glucose Study phase II. Trials. 2009;10:5. doi: 10.1186/1745-6215-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mohammadifard N, Kelishadi R, Safavi M, Sarrafzadegan N, Sajadi F, Sadri GH, et al. Effect of a community-based intervention on nutritional behaviour in a developing country setting: The Isfahan Healthy Heart Programme. Public Health Nutr. 2009;12(9):1422–30. doi: 10.1017/S1368980008004230. [DOI] [PubMed] [Google Scholar]
- 41.Rabiei K, Kelishadi R, Sarrafzadegan N, Abedi HA, Alavi M, Heidari K, et al. Process evaluation of a community-based program for prevention and control of non-communicable disease in a developing country: The Isfahan Healthy Heart Program, Iran. BMC Public Health. 2009;9:57. doi: 10.1186/1471-2458-9-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sarrafzadegan N, Azadbakht L, Mohammadifard N, Esmaillzadeh A, Safavi M, Sajadi F, et al. Do lifestyle interventions affect dietary diversity score in the general population? Public Health Nutr. 2009;12(10):1924–30. doi: 10.1017/S1368980009004856. [DOI] [PubMed] [Google Scholar]