Abstract
BACKGROUND AND OBJECTIVES
Limited data are available on patients with acute coronary syndromes (ACS) and their long-term outcomes in the Arabian Gulf countries. We evaluated the clinical features, management, in-hospital, and long-term outcomes in such a population.
DESIGN AND SETTING
A 9-month prospective, multicenter study conducted in 65 hospitals from 6 countries that also included 30 day and 1-year mortality follow-up.
PATIENTS AND METHODS
ACS patients included those with ST-elevation myocardial infarction (STEMI) and non–ST-elevation acute coronary syndrome (NSTEACS), including non-STEMI and unstable angina. The registry collected the data prospectively.
RESULTS
Between October 2008 and June 2009, 7930 patients were enrolled. The mean age [standard deviation (SD)], 56 (17) years; 78.8% men; 71.2% Gulf citizens; 50.1% with central obesity; and 45.6% with STEMI. A history of diabetes mellitus was present in 39.5%, hypertension in 47.2%, and hyperlipidemia in 32.7%, and 35.7% were current smokers. The median time from symptom onset to hospital arrival for STEMI patients was 178 minutes (interquartile range, 210 minutes); 22.3% had primary percutaneous coronary intervention (PCI) and 65.7% thrombolytic therapy, with 34% receiving therapy within 30 minutes of arrival. Evidence-based medication rates upon hospital discharge were 68% to 95%. The in-hospital PCI was done in 21% and the coronary artery bypass graft surgery in 2.9%. The in-hospital mortality was 4.6%, at 30 days the mortality was 7.2%, and at 1 year after hospital discharge the mortality was 9.4%; 1-year mortality was higher in STEMI (11.5%) than in NSTEACS patients (7.7%; P<.001).
CONCLUSIONS
Compared to developed countries, ACS patients in Arabian Gulf countries present at a relatively young age and have higher rates of metabolic syndrome features. STEMI patients present late, and their acute management is poor. In-hospital evidence-based medication rates are high, but coronary revascularization procedures are low. Long-term mortality rates increased severalfold compared with in-hospital mortality.
The World Health Organization predicts that cardiovascular diseases will be the leading causes of mortality and morbidity in developing countries by the year 2020.1–4 The Gulf Heart Association (GHA) has recognized the seriousness of this issue and the devastating impact of such illnesses. Its landmark multinational study launched in May 2006, the Gulf Registry of Acute Coronary Events (Gulf RACE), demonstrated several unique features and knowledge-care gaps in the acute coronary syndrome (ACS) population in Gulf nations.5 It also identified a high prevalence of cardiovascular risk factors and low rates of revascularization procedures, but low in-hospital mortality.6
The objectives of this second phase (Gulf RACE-2) were to take another snapshot of ACS care in the Arabian Gulf region, but with a more detailed data collection on the left ventricular function and the coronary anatomy, in addition to determining the 30-day and 1-year total mortality rates. All Arabian Gulf countries were involved in both phases of the registry, except for Saudi Arabia in the previous phase and Kuwait in the currently reported phase 2.
PATIENTS AND METHODS
The data were collected from a 9-month prospective, multicenter study of Gulf RACE-2 that recruited consecutive ACS patients from 6 adjacent Middle Eastern Gulf countries (Bahrain, Saudi Arabia, Qatar, Oman, United Arab Emirates [UAE], and Yemen). Patients were recruited from 65 hospitals with a diagnosis of ACS including unstable angina (UA) and non–ST-elevation myocardial infarction (data merged as NSTEACS), and ST-elevation myocardial infarction (STEMI). An on-site cardiac catheterization laboratory was available in 43% of hospitals. The majority of hospitals (71%) had a coronary care unit on-site. No patient-specific exclusion criteria were available, and all prospective patients with ACS were thus enrolled. The study received ethical approval from the institutional ethical bodies in all participating countries. Full details of the methods have been published.5,6
The diagnosis of the different types of ACS and definitions of data variables were based on the American College of Cardiology clinical data standards.7 Central obesity was defined as a waist circumference of more than 94 cm in men and more than 80 cm in women.8 Data on additional variables were collected in the second phase of the registry compared to the previous phase, and included the following: serum creatinine before hospital discharge, serum hemoglobin A1c, fondaparinux, bivalirudin, echocardiography results (severe left ventricular [LV] dysfunction: ejection fraction [EF] <30%; moderate LV dysfunction: EF=30%–40%; mild LV dysfunction: EF=40%–55%; normal LV function: EF >55%], coronary angiogram results [left main coronary artery disease [CAD], 1-vessel disease, 2-vessel disease, 3-vessel disease), and types of coronary artery stents used (drug-eluting and/or bare-metal stents). Significant CAD was defined as ≥50% occlusion compared to the normal reference diameter in the left main, and ≥70% in other major epicardial coronary arteries.
A case report form for each patient with suspected ACS was filled out upon hospital admission by assigned physicians and/or research assistants working in each hospital, using standard definitions and completed throughout the patient’s hospital stay. Almost all the data variables were mandatory fields and completed online. All case report forms were verified by a cardiologist, and then sent online to the principal coordinating center, where they were further checked for errors before submission for final analysis. We avoided duplicate admissions to the registry by using patients’ national identification numbers and assigned “registry numbers.” A long-term mortality was obtained by either phone contacts or clinic visits. For “therapy-related timelines” in STEMI patients who underwent thrombolytic therapy (TT) or primary percutaneous coronary intervention (PCI), we excluded transferred STEMI patients because of inaccurate data from other hospitals not involved in the registry.
Data were summarized as mean (SD) if they were normally distributed; otherwise, they were summarized as the median and interquartile range (IQR). Differences between groups were assessed using the chi-square or Fisher exact tests for categorical variables, student t tests for continuous and normally distributed variables, and the Mann-Whitney U test for skewed variables. All analyses were considered significant at P<.05. The analysis was performed using SPSS software, version 17 (IBM Corp., Armonk, NY USA).
RESULTS
Study Population Characteristics
Between October 2008 and June 2009, 7930 ACS patients were enrolled. There were 3613 (45.6%) STEMI and 4317 (54.4%) NSTEACS patients. The NSTEACS patients included 2386 (55.3%) NSTEMI and 1931 (44.7%) UA patients. Table 1 shows patient baseline characteristics, treatments, and outcomes. The mean age (standard deviation [SD]) of the overall population was 56 (17) years, 71.2% were Arabian Gulf citizens, and 78.8% were men. The prevalence of CAD risk factors was high; 39.5% had diabetes mellitus (DM), 47.2% had hypertension, 52.9% were either current or ex-smokers, 18.4% were khat chewers, and 32.7% had hyperlipidemia. The mean body mass index (BMI [SD]) was 26.2 (5.3) kg/m2, and 50.1% of patients had central obesity. Upon presentation, only 19.1% arrived at the hospital in an ambulance, 84.1% had typical ischemic chest pain, 23% had clinical evidence of congestive heart failure (CHF), and 68.4% had positive serum troponin. Serum troponin was unknown in 796 (10%) patients as the treating physicians decided not to perform the test because the diagnosis of STEMI had already been made by electrocardiogram, myocardial infarction was diagnosed by elevated creatinine kinase (CK)-MB, or the test was not available at the time of admission.
Table 1.
Patient baseline characteristics, procedures, and outcomes in the study.
| Variable | n (%) | STEMI/New LBBB n (%) |
NSTEACS n (%) |
P value |
|---|---|---|---|---|
|
| ||||
| Demographics | ||||
| Age, mean (SD), years | 56 (17) | 54 (16) | 58 (17) | <.001 |
| Male, n (%) | 6253 (78.8) | 3119 (86.1) | 3134 (72.6) | <.001 |
| Arabian Gulf citizen, n (%) | 5674 (71.2) | 2366 (65.3) | 3308 (76.6) | <.001 |
| Body mass index, mean (SD), kg/m2a | 26.2 (5.8) | 25.8 (5.5) | 26.7 (6.2) | <.001 |
| Central obesity, n (%)b | 2196 (50.1) | 1057 (45.5) | 1139 (55.4) | <.001 |
| Ambulance use, n (%)c | 1325 (19.1) | 621 (19.8) | 704 (18.5) | .195 |
| Initial presentation | ||||
| Typical ischemic chest pain, n (%) | 6675 (84.1) | 3244 (89.6) | 3431 (79.5) | <.001 |
| Cardiac arrest | 47 (0.59) | 28 (0.77) | 19 (0.44) | <.001 |
| SBP, mean (SD), mm Hg | 132 (35) | 130 (40) | 138 (36) | <.001 |
| DBP, mean (SD), mm Hg | 80 (20) | 80 (20) | 80 (20) | .164 |
| HR, mean (SD), bpm | 82 (25) | 84 (26) | 81 (24) | .339 |
| Atrial fibrillation, n (%) | 166 (2.1) | 43 (1.2) | 123 (2.8) | <.001 |
| Killip class >1, n (%) | 1822 (23) | 765 (21.1) | 1057 (24.5) | <.001 |
| History | ||||
| CAD, n (%) | 4548 (57.3) | 1110 (30.6) | 3438 (79.6) | <.001 |
| PCI, n (%) | 727 (9.2) | 128 (3.5) | 599 (13.9) | <.001 |
| CABG, n (%) | 336 (4.2) | 36 (1) | 300 (6.9) | <.001 |
| CHF, n (%) | 523 (6.6) | 71 (2) | 452 (10.5) | <.001 |
| CVA/TIA, n (%) | 341 (4.3) | 118 (3.3) | 223 (5.2) | <.001 |
| PAD, n (%) | 145 (1.8) | 39 (1.1) | 106 (2.5) | <.001 |
| CRF, n (%) | 319 (4) | 43 (1.2) | 276 (6.4) | <.001 |
| Diabetes mellitus, n (%) | 3137 (39.5) | 1167 (32.2) | 1970 (45.6) | <.001 |
| Hypertension, n (%) | 3748 (47.2) | 1246 (34.4) | 2502 (58.0) | <.001 |
| Current smoking, n (%) | 2834 (35.7) | 1726 (47.6) | 1108 (25.7) | <.001 |
| Ex-smoking, d n (%) | 1363 (17.2) | 610 (16.8) | 753 (17.4) | <.001 |
| Khat chewing, n (%) | 1408 (18.4) | 983 (27.9) | 425 (10.3) | <.001 |
| Hyperlipidemia, n (%) | 2598 (32.7) | 750 (20.7) | 1848 (42.8) | <.001 |
| Laboratory findings | ||||
| Positive serum troponin, n (%)e | 5426 (68.4) | 3124 (86.5) | 2302 (53.3) | <.001 |
| Peak creatine kinase MB, ng/mLe | 49 (103) | 94 (152) | 18 (35) | <.001 |
| Total cholesterol, mmol/Le | 4.8 (1.9) | 5 (1.8) | 4.6 (1.9) | <.001 |
| Triglyceride, mmol/Le | 1.5 (1.1) | 1.6 (1.1) | 1.5 (1.1) | <.001 |
| High-density lipoprotein cholesterol, mmol/Le | 1 (0.4) | 1 (0.4) | 1 (0.4) | .042 |
| Low-density lipoprotein cholesterol, mmol/Le | 3.1 (1.6) | 3.3 (1.5) | 2.9 (1.5) | <.001 |
| Fasting serum glucose, mmol/Le | 6.3 (3.3) | 6.2 (3.3) | 6.3 (3.3) | .864 |
| HbA1c, %e | 7 (3.2) | 7 (3.6) | 7 (2.9) | .543 |
| Serum first creatinine, μmol/Lf | 88 (33.4) | 88 (30.8) | 86.3 (34.6) | <.001 |
| Serum pre-hospital discharge creatinine, μmol/Le | 88 (32) | 88 (29) | 88 (38) | .718 |
| GRACE score | ||||
| Low, n (%) | 3068 (39.2) | 1481 (41.8) | 1587 (37.1) | <.001 |
| Intermediate, n (%) | 3055 (39.0) | 1289 (36.4) | 1766 (41.3) | <.001 |
| High (%) | 1702 (21.8) | 774 (21.8) | 928 (21.7) | .884 |
| Procedures (at index hospitalization) | ||||
| Echocardiography, n (%) | 6073 (76.5) | 2881 (79.5) | 3192 (73.9) | <.001 |
| Mild LV dysfunction, n (%) | 2713 (44.7) | 1508 (52.4) | 1205 (37.8) | <.001 |
| Moderate LV dysfunction, n (%) | 1198 (19.7) | 688 (23.9) | 510 (16) | <.001 |
| Severe LV dysfunction, n (%) | 562 (9.3) | 240 (8.3) | 322 (10.1) | <.001 |
| Coronary angiography, n (%) | 2579 (32.5) | 979 (27) | 1600 (37.1) | <.001 |
| Left main disease, n (%) | 146 (5.6) | 37 (3.8) | 109 (6.8) | .001 |
| 1-vessel disease, n (%) | 762 (29.5) | 365 (37.3) | 397 (24.7) | <.001 |
| 2-vessel disease, n (%) | 626 (24.2) | 275 (28.1) | 351 (21.9) | <.001 |
| 3-vessel disease, n (%) | 771 (29.8) | 228 (23.3) | 543 (33.9) | <.001 |
| PCI, n (%)f | 1148 (21) | 456 (17.3) | 692 (24.4) | <.001 |
| CABG, n (%) | 233 (2.9) | 65 (1.8) | 168 (3.9) | <.001 |
| In-hospital outcomes | ||||
| Recurrent ischemia | 1233 (15.5) | 665 (18.4) | 568 (13.2) | <.001 |
| Recurrent MI | 172 (2.2) | 127 (3.5) | 45 (1) | <.001 |
| CHF | 1041 (13.1) | 516 (14.2) | 525 (12.2) | .006 |
| Cardiogenic shock | 458 (5.8) | 324 (8.9) | 134 (3.1) | <.001 |
| VT and/or VF | 225 (2.8) | 180 (5) | 45 (1) | <.001 |
| Nonsurgical ventilation | 370 (4.7) | 222 (6.1) | 148 (3.4) | <.001 |
| Stroke | 56 (0.7) | 40 (1.1) | 16 (0.4) | <.001 |
| Major bleeding | 47 (0.6) | 25 (0.7) | 22 (0.5) | .296 |
| Death | 362 (4.6) | 253 (7) | 109 (2.5) | <.001 |
| Median length of hospital stay, median (IQR), days | 5.0 (4.0) | 5.0 (4.0) | 4.0 (3.0) | <.001 |
| 30-day mortality | 572 (7.21) | 356 (9.85) | 216 (5) | <.001 |
| 1-year mortality | 749 (9.43) | 417 (11.51) | 332 (7.69) | <.001 |
| Total | 7930 | 3613 (45.6) | 4317 (54.4) | |
SD: Standard deviation; STEMI: ST-segment elevation myocardial infarction; LBBB: left bundle branch block; NSTEACS: non–ST-segment elevation myocardial infarction; SBP: systolic blood pressure; DBP: diastolic blood pressure; HR: heart rate; bpm: beats per minute; CAD: coronary artery disease; PCI: percutaneous coronary intervention; CABG: coronary artery bypass graft surgery; CHF: congestive heart failure; CVA/TIA: cerebrovascular accident/transient ischemic attack; PAD: peripheral arterial disease; CRF: chronic renal failure; MI: myocardial infarction; VT: ventricular tachycardia; and VF: ventricular fibrillation; LV: left ventricular.
Unknown serum troponin in 796 (10%) patients.
Data were available for 4385 patients.
Data were available for 6940 patients.
Stopped smoking more than 1 year before index hospitalization.
Median (IQR).
Data were available for PCI in 5462 patients.
Compared with STEMI patients, those with NSTEACS were more likely to be older and an Arabian Gulf citizen; have a higher BMI, central obesity, history of CAD, PCI, coronary artery bypass graft surgery (CABG), peripheral arterial disease, CHF, DM, hypertension, ex-smoking, hyperlipidemia, and/or cerebrovascular accident or transient ischemic attack; present with atrial fibrillation, Killip class >1, higher mean systolic blood pressure; higher frequency of intermediate Global Registry of Acute Coronary Events (GRACE) score category, have severe LV dysfunction, had undergone coronary angiogram, PCI, CABG, and/or left main and/or 3-vessel disease during hospitalization (P<.001 for all comparisons). However, STEMI patients were more likely to be men, current smokers, and khat chewers and to present with typical ischemic chest pain or cardiac arrest, positive serum troponin, higher peak serum CK-MB fraction, low-density lipoprotein, creatinine, and low GRACE score category (P<.001 for all comparisons).
ST-elevation myocardial infarction: presentation and management
A total of 2416 (79.3%) out of 3047 STEMI patients presented within 12 hours of symptom onset. The median time from symptom onset to hospital arrival was 178 minutes (IQR 210). A total of 1585 patients (65.7%) were treated with TT, with 34% receiving it within 30 minutes of hospital arrival, and the median door-to-needle time was 39 minutes (IQR 36). The most commonly used TT was reteplase (44.2%), followed by streptokinase (42.5%), then tenecteplase (10.2%). These drugs were administered in coronary/intensive care units in 58.2%, and by cardiology specialists in 84.4% of cases. There was no clinical evidence of reperfusion in 10.2%, and rescue PCI was done in 13.3% of these patients. Reasons for not administering TT included: symptom onset more than 12 hours before hospital presentation (48.5%), primary PCI (22.3%), absolute contraindications (10.5%), and missed diagnosis (6%). Other causes (12.8%) that the treating physicians reported included one or more of the following: “very elderly” patients, severe hypertension, prolonged resuscitation, cardiogenic shock, cardiac arrest, transient ST-segment elevation, unavailability of TT, patient and/or family refusal, and patient inability to pay for cardiac care. Regarding primary PCI, median door–to-balloon time (DBT) was 87 minutes (IQR 63), and 52.4% of the patients had a DBT of less than 90 minutes following hospital arrival.
Medications
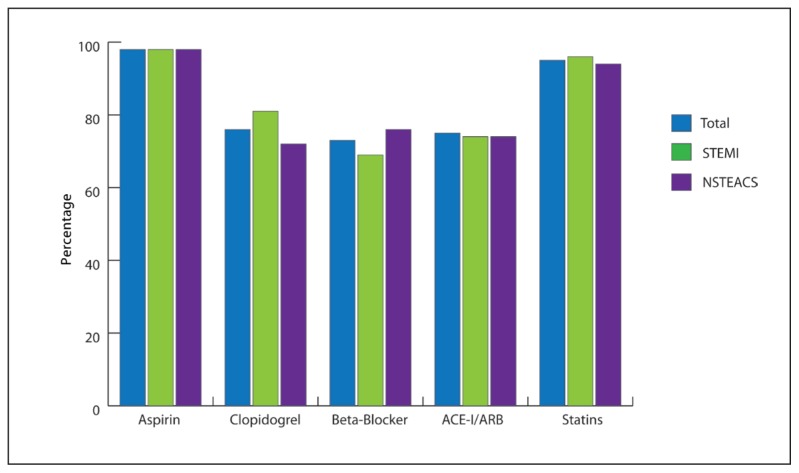
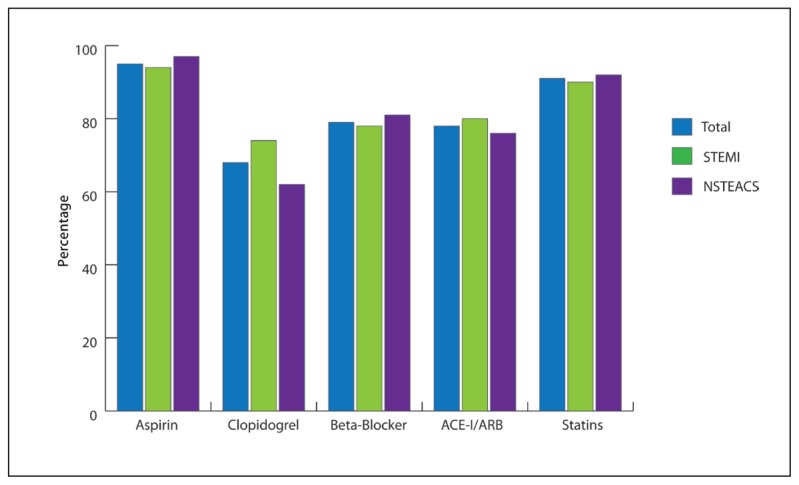
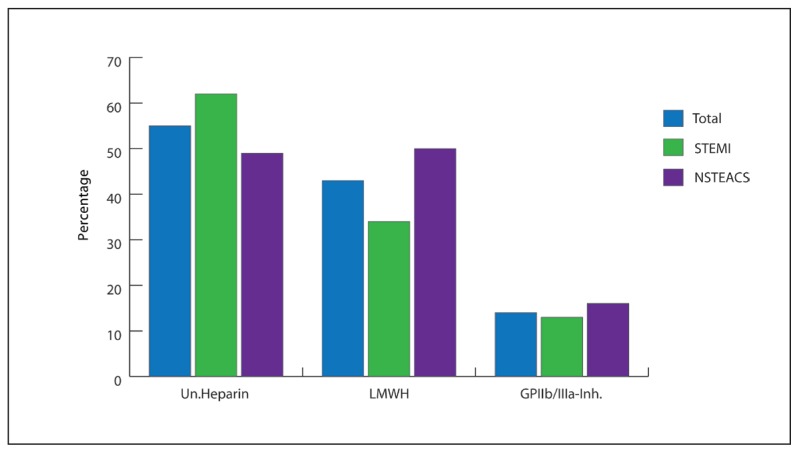
Figures 1 and 2 show the high use of evidence-based medications in the first 24 hours of hospital admission and at discharge: aspirin (98.3% and 95.4%), statins (94.7% and 91.2%), clopidogrel (76% and 68%), beta-blockers (73% and 79.2%), and angiotensin-converting enzyme inhibitors or angiotensin receptor blockers (74.8% and 78.1%). Figure 3 shows that most patients received anticoagulation therapy; for more than half, therapy was intravenous unfractionated heparin, and for less than 1%, it was either fondaparinux or bivalirudin. Intravenous glycoprotein IIb/IIIa inhibitors (GP IIb/IIIa–I) were given in 14.3%, mostly in the form of tirofiban.
Figure 1.
Medications in the first 24 hours of hospital admission. P<0.001 for clopidogrel and beta-blockers, P<.002 for statins.
Figure 2.
Medications at hospital discharge. P<.001 for aspirin, clopidogrel, beta-blockers, and ACE-I/ARB, and P<.013 for statins.
Figure 3.
Anticoagulation and GP IIb/IIIa inhibitors. P<.001 for all comparisons. Un. Heparin: unfractionated heparin; LMWH: low molecular weight heparin; GP IIb/IIIa-Inh: glycoprotein IIb/IIIa inhibitors.
Procedures and outcomes
Echocardiography was done in 76.5% of patients, with 73.7% having evidence of LV dysfunction, coronary angiography in 32.5%, PCI in 21% (scheduled PCI in 1.43%), and CABG in 2.9% (scheduled CABG in 4.7%). In PCI patients, bare-metal stents were used in 40.6%, drug-eluting stents in 56.6%, and both in 2.8%. The overall in-hospital mortality was 4.6%. The most frequent complications were recurrent ischemia (15.5%) and CHF (13.1%), whereas rates of stroke (0.7%) and major bleeding (0.6%) were very low. STEMI patients had higher in-hospital mortality and cardiovascular complications (P=.006 for CHF, and P<.001 for all other comparisons) but had similar major bleeding rates compared with NSTEACS patients (Table 1). Overall 30-day mortality was 7.2% (9.9% in STEMI, 7.1% in NSTEMI, 2.4% in UA, and unknown in 13.7%). Overall 1-year mortality was 9.4% (11.5% in STEMI, 10.1% in NSTEMI, 4.7% in UA, and unknown in 22.9%) (Table 1).
DISCUSSIONS
This report is the first to describe long-term outcomes of ACS patients in the Middle East. It provides a good representation of the clinical management of ACS patients because several hospitals (secondary and tertiary) from all geographic regions of these countries and most health care providers were involved. Our study showed that ACS patients have several unique features and outcomes compared with their counterparts in other populations (Table 2).9–23 Almost half (45.6%) of our patients had STEMI, compared with one-third in other ACS populations reported worldwide. Roger et al reported a decline in the incidence of STEMI over the last 2 decades in a Unites States (US) community-based study.24 The high prevalence of STEMI in our study is probably the result of the relatively young average age of ACS presentation (56 years), which is almost a decade younger than those of developed countries. 9–23 However, the rate of STEMI is very similar to that of ACS patients from the Far East countries, such as Malaysia,25 but less than the 60.6% rate reported in India.22 This outcome is likely the result of several factors in addition to the overall younger age of the population in developing countries,26 including the extremely high prevalence of uncontrolled CAD risk factors in the general population;27,28 further, there is the high prevalence of DM, involving 39.5% of our patients. Plausible explanations for this high rate of DM include lack of regular exercise and adopting a “western” diet.29 These changes in the Arabian culture are probably the result of oil wealth–induced “obesogenic urbanization” that has occurred at a particularly rapid pace over only a few generations.30 In addition, the high ratio of “expatriates to citizens” living in some Arabian Gulf countries, such as UAE and Qatar, also has contributed to the relatively younger age of ACS presentation. The expatriates are usually much younger, and mostly manual workers with high rates of smoking (53% current smokers in our registry) and a stressful lifestyle compared to Arabian Gulf citizens.
Table 2.
Comparison of acute coronary syndromes in developed and developing countries in the study.
| NRMIa,b (9–12) | GRACEc (13–17) | GRACEd (18) | EHS 1 and 2e (19–21) | CREATEf (22) | Gulf RACEg (6) | Gulf RACE-2h (6) | SPACEi | |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Patients, n | 2 515 106 | 102 341 | 31 982 | 16 183 | 20 937 | 8176 | 7930 | 5055 |
| Mean age (years) | 65–70 | 63–69 | 65 | 63 | 57 | 56 | 56 | 58 |
| History of DM, % | 17–35 | 20–30 | 26 | 21–27 | 30 | 40 | 40 | 58 |
| STEMI, % | 47 | 30–40 | 30 | 42–47 | 61 | 39 | 46 | 41 |
| NSTEACS, % | 53 | 60–70 | 70 | 48–51 | 39 | 61 | 54 | 59 |
| Symptom onset to hospital arrival, median (min) | 132–96j | 140–120j | 133 | 170–145j | 300 | NA | 178 | 150 |
| Door-to-needle time, median (min) | 59–29j | 40–30j | 32 | 40–37j | 50 | 45 | 39 | 52 |
| Thrombolytic therapy, % | 52–28j | 41–16j | 33 | 37–41j | 59 | 82 | 66 | 69 |
| Primary PCI, % | 2.6–43j | 15–44j | 16 | 40–58j | 8 | 8 | 22.3 | 17.5 |
| In-hospital mortality,l % | 8/5.2 | 5.4/2 | 6.2/4.6 | 5.3/2.5 | 5.6m | 6.2/1.9 | 7/2.5 | 4.5/2 |
| 30-day mortality,l % | NA | 8/3 | NA | 6.4/3.4 | 8.6/3.8 | NA | 9.9/5 | NA |
| 1-year mortality,l % | NA | 14.8k,m | NA | 7/5 | NA | NA | 11.5/7.7 | NA |
DM: Diabetes mellitus; STEMI: ST-segment elevation myocardial infarction; NSTEACS: non–ST-segment elevation myocardial infarction; NA: not available; PCI: percutaneous coronary intervention; GRACE: Global Registry of Acute Coronary Events; Gulf RACE: Gulf Registry of Acute Coronary Events; SPACE: Saudi project for assessment of coronary events;
Did not include patients with unstable angina.
National registry of myocardial infarction in the USA.
Global Registry of Acute Coronary Syndromes.
Expanded Global Registry of Acute Coronary Syndromes.
European Heart Surveys 1 and 2.
Treatment and outcomes of acute coronary syndromes in India.
Gulf Registry of Acute Coronary Events.
Gulf Registry of Acute Coronary Events-Phase 2.
Saudi Project for Assessment of Coronary Events (in press).
Data reflect temporal trends chronologically over the years.
Total mortality was derived from 1143 acute coronary syndrome patients enrolled in New Zealand.
STEMI/NSTEACS.
Total in-hospital mortality.
Our STEMI patients took an average of 178 minutes before presenting to the emergency department compared with 140 to 170 minutes in developed countries. 12,17 The infrequent patient use and/or underdevelopment of ambulance services are among the major reasons for delayed presentations. Other factors include underestimation of the importance of symptoms, absence of a universal health care system provider, traffic congestion in major cities, and long travel distances needed for patients before arrival at a major cardiac center in some Arabian Gulf countries. Moreover, just over one-third of our STEMI patients received TT within the standard 30 minutes because the majority were awaiting approval of administration of TT by the cardiology service, mostly required to receive it in the coronary/intensive care units; further, only half received faster preparations of TT, such as reteplase and tenecteplase. It is important to note that although three quarters of the hospitals are “tertiary-care” centers, and many of the emergency department consultants may not be certified emergency physicians and may prefer to have the cardiology service make the decision for revascularization therapy; this preference can result in further delay in initiating treatment (personal communication with principal investigators).
Primary PCI was done in only 22.3% of STEMI patients, a rate much lower than in developed countries, and only half of them had a DBT within the standard 90 minutes. In addition, 18.8% of STEMI patients did not receive either TT or primary PCI, and did not have an absolute contraindication to either treatment; i.e: reperfusion shortfall; nevertheless, this value is still lower than the 33% reported in the GRACE registry.13,18 The reperfusion shortfall was attributable to the fact that the treating physicians either missed the diagnosis or had the “false perception” that the patient would not benefit and might be even harmed by revascularization therapy. This finding highlights the urgent need for initiating educational programs in our region on the establishment of competent triaging systems in the emergency department, and also to improve awareness about the absolute versus relative contraindications for revascularization therapies according to the latest American College of Cardiology/American Heart Association/European Society of Cardiology guidelines. In addition, unavailability of TT and/or coronary catheterization facilities in many hospitals because of the poor economy in some of the Arabian Gulf countries should also be considered.
Similar to recent trends reported by other ACS registries,12,13,17,18 our study showed a high use of guidelines-recommended oral medications. However, rates of fondaparinux, bivalirudin, GP IIb/IIIa–I, coronary angiography, elective PCI, and CABG were much lower than those reported in developed and some Middle East countries, but similar to those in Asian countries.11,18,31,32 Less than half of the hospitals involved in our registry had an on-site cardiac catheterization laboratory. These findings reflect the need for establishing more tertiary-care hospitals with high-caliber technical and human resources that could provide more revascularization procedures in a timely fashion for ACS patients. We have reported previously that the use of coronary catheterization was related more to the country’s practice pattern and hospital characteristics than to the patient baseline risk.6,33 In addition, the elective PCI rate was surprisingly lower in STEMI than in NSTEACS patients despite the presence of more single- and double-vessel CAD in the former. The low rate of timely reperfusion in STEMI patients might have resulted in more myocardial injury, and thus less perceived benefit by the treating physicians about recanalizing the culprit coronary artery by PCI.
The overall in-hospital mortality of 4.6% is similar to contemporary data from developed countries, but lower than those reported in poor communities in India (Table 2). Overall high uses of guidelines-based therapies, in addition to the relatively younger age of ACS presentation, were probably the main reasons for the reasonably low in-hospital mortality in our study. However, we have shown previously a significant disparity in STEMI in-hospital mortality in some Arabian Gulf countries resulting from variability in a number of factors, such as timely presentation, reperfusion therapy, and use of evidence-based medications. 34,35 STEMI patients had higher in-hospital complications, but similar major bleeding compared to those with NSTEACS. This finding is similar to those of other ACS registries and is most likely related to the long time between symptom onset to hospital arrival and the below-standard door-to-needle times.
The overall mortality rate doubled at 1 year of follow-up (9.4%), however, and was even higher than the mortality rate reported in the Euro Heart Survey (Table 2). This result is alarming because our ACS patients were much younger than those in the developed countries, and yet had higher long-term mortality. This difference might be related to the low rate of coronary revascularization in addition to possible noncompliance with medical therapy and/or healthy lifestyle behaviors after hospital discharge. It is unknown as well whether the use of generic drugs by many hospitals contributed to future cardiovascular events. Furthermore, although STEMI patients had the highest 1-year mortality (11.5%), NSTEMI patients had a severalfold increase in mortality that was proportionally higher than the mortality increase in STEMI patients. This finding is in concordance with the published studies showing a comparable and even a higher long-term mortality for NSTEMI patients, likely because of older age and more cardiovascular and/or noncardiovascular comorbidities.24
Our study has several limitations. First, as with most other registries, hospital enrollment was voluntary; thus, the study results may not be representative of clinical practice in all hospitals in the region. In addition, hospitals that participated in the registry might be more enthusiastic about adherence to guidelines and quality improvement initiatives. However, the wide geographic distribution of several hospitals from different health care sectors in our study provides a reasonable overall representation of ACS care. Second, there is an inherent selection bias because of the observational nature of the study design and the possibility of missing unmeasured important covariables. Third, mortality rates might have been underestimated because of missing major adverse events, particularly ACS-related mortality that happened prior to admission to the cardiology service or unknown long-term mortality. We tried to mitigate this issue by requiring all hospitals to enroll consecutive patients and to keep a log book of ACS hospital admissions. Fourth, we did not measure potential factors that might explain the increase in the long-term mortality rates, such as nonadherence to evidence-based therapies. Finally, although we compared our data with other international ACS registries, caution has to be taken about making absolute inferences, mainly because of the patient age and timing differences between these studies and ours.
In conclusion, our study showed that our ACS patients present at a relatively young age and have high rates of DM. STEMI patients delayed a long time before presenting to the hospital, and only a few received either TT or primary PCI within the recommended time-line. In-hospital guidelines-based medication rates were high, but coronary revascularization rates were low. Long-term mortality rates increased severalfold compared with the in-hospital mortality rate, with the highest mortality in STEMI rather than NSTEACS patients, despite the former being younger and having fewer cardiovascular comorbidities. Further studies are needed to explore the underlying reasons for these findings.
Footnotes
Funding Sources
Gulf RACE is a Gulf Heart Association (GHA) project and was financially supported by the GHA, Sanofi Aventis, and the College of Medicine Research Center at King Khalid University Hospital, King Saud University, Riyadh, Saudi Arabia. The sponsors had no role in the study design, data collection, data analysis, writing of the report, or submission of the manuscript.
Gulf RACE-2 National Coordinators, investigators, and case reports data collectors
Bahrain: Haitham Amin (National Coordinator), Husam Noor, Rashid Albannai Oman: Jawad Al-Lawati (National Coordinator), Kadhim Sulaiman (National Coordinator), B. Kamath, P. P. Singh, Marei Aysha, Ali Yousif, Faisal Tamimi, Kurain Mathew, Ahmed Mosad, A. Narayan, Adel BadrEldin, Qassim Shimal, S. K. Samantray, Kamiran Dabagh, Zakaria Boghdady, K. J. Sulaiman, Sulieman Al-Sheraiqi Qatar: Nidal A. Asaad (National Coordinator), Amar Mohammad Salam UAE: Wael Almahmeed (National Coordinator), Nazar Albustani (National Coordinator), Nayan Rao, Adel A.S. Wassef, Amrish Agrawal. Yemen: Ahmed Al-Motarreb (National Coordinator), Nora Al-Sagheer (National Coordinator), Abdu hamood, Mohammed Abu Ghanem, Abd Al-Jalil AL Wazeer, Abdullah AL-Shameeri, Majed AL-Showbaki, Elham AL-Qudari, Araf Ahamed Saleh, Hanan Mojamal, Abd AL-Raheem ba Khashwen, Faiz Khoba, Abd AL-Hakim Al-Hammadi, Munir AL-Absi, Mohammad Tantawi, Khalad Alzanan, Ahmed Al-Rubaidi, Faud Ali, Abd ARakeeb Al-Ghobari, Madian Shehab, Motee AL-Awlagi. Saudi Arabia: Khalid AlHabib (Principal Investigator), Kazi Nur Asfina, Modaser Ahmad Butt, Mahmoud Hazaimeh, Najeeb Ullah Bugti, Riffat Ahmad Bukhari, Yousif Noor, Layth A. Mimish, Ahmad Nada, Tarek Kashour, Ali Khamis Mohammed, Mohammed Abdullah Raja, Murad Abdulaziz Al Swaiti, Ahmad M. AlSababha, Gamal Abdin Hussein, Muneeb Alavi, Mohamed Munir Baig, Hassan Darwish, Raza Gorzi, Aftab Ahmed, Ahmed Mohamed Abuosa, Ayman Hassan ElShiekh, Adel Mahmoud Hasanin, Ashraf Mahmoud ElKhalifa, Khalid AlNemer, Mohammed Ali, Mushabab Ayedh Al-Murayeh, Sohil Elfar, Sharif El-Bardisy, Mohamed Maghraby, Sajed Choudary, Ali Yousef, Mohamed Atteiah, Abdulaziz Sabry, Masood Gori, Tariq Ishaq Soomro, Mohammad Shoman, Shukri M. Al-Saif, Shaima Al-Omani, Hind Kamar, Attiea Saleh, Hesham Hassoun, Anas Bakheet, Adel Maria, Mabrooke Al Sharary, Emad Ibrahim, Asif Malik, Ola Abdelmaguid, Amir Taraben, Talal Issa Abd Al-Rahman.
REFERENCES
- 1.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL. Global and regional burden of disease and risk factors, 2001: Systematic analysis of population health data. Lancet. 2006;367:1747–57. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 2.Yusuf S, Reddy S, Ounpuu S, Anand S. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation. 2001;104:2746–53. doi: 10.1161/hc4601.099487. [DOI] [PubMed] [Google Scholar]
- 3.Reddy KS. Cardiovascular disease in non-Western countries. N Engl J Med. 2004;350:2438–40. doi: 10.1056/NEJMp048024. [DOI] [PubMed] [Google Scholar]
- 4.Yusuf S, Reddy S, Ounpuu S, Anand S. Global burden of cardiovascular diseases: Part II: Variations in cardiovascular disease by specific ethnic groups and geographic regions and prevention strategies. Circulation. 2001;104:2855–64. doi: 10.1161/hc4701.099488. [DOI] [PubMed] [Google Scholar]
- 5.Zubaid M, Rashed WA, Al-Khaja N, Almahmeed W, Al-Lawati J, Sulaiman K, et al. Clinical presentation and outcomes of acute coronary syndromes in the Gulf Registry of Acute Coronary Events (Gulf RACE) Saudi Med J. 2008;29:251–5. [PubMed] [Google Scholar]
- 6.Zubaid M, Rashed WA, Almahmeed W, Al-Lawati J, Sulaiman K, Al-Motarreb A, et al. Management and outcomes of Middle Eastern patients admitted with acute coronary syndromes in the Gulf Registry of Acute Coronary Events (Gulf RACE) Acta Cardiol. 2009;64:439–46. doi: 10.2143/AC.64.4.2041607. [DOI] [PubMed] [Google Scholar]
- 7.Cannon CP, Battler A, Brindis RG, Cox JL, Ellis SG, Every NR, et al. American College of Cardiology key data elements and definitions for measuring the clinical management and outcomes of patients with acute coronary syndromes. A report of the American College of Cardiology Task Force on Clinical Data Standards (Acute Coronary Syndromes Writing Committee) J Am Coll Cardiol. 2001;38:2114–30. doi: 10.1016/s0735-1097(01)01702-8. [DOI] [PubMed] [Google Scholar]
- 8.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–5. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 9.Rogers WJ, Canto JG, Barron HV, Boscarino JA, Shoultz DA, Every NR. Treatment and outcome of myocardial infarction in hospitals with and without invasive capability. Investigators in the National Registry of Myocardial Infarction. J Am Coll Cardiol. 2000;35:371–9. doi: 10.1016/s0735-1097(99)00505-7. [DOI] [PubMed] [Google Scholar]
- 10.Rogers WJ, Canto JG, Lambrew CT, Tiefenbrunn AJ, Kinkaid B, Shoultz DA, et al. Temporal trends in the treatment of over 1.5 million patients with myocardial infarction in the US from 1990 through 1999: The National Registry of Myocardial Infarction 1, 2 and 3. J Am Coll Cardiol. 2000;36:2056–63. doi: 10.1016/s0735-1097(00)00996-7. [DOI] [PubMed] [Google Scholar]
- 11.Peterson ED, Shah BR, Parsons L, Pollack CV, Jr, French WJ, Canto JG, et al. Trends in quality of care for patients with acute myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J. 2008;156:1045–55. doi: 10.1016/j.ahj.2008.07.028. [DOI] [PubMed] [Google Scholar]
- 12.Gibson CM, Pride YB, Frederick PD, Pollack CV, Jr, Canto JG, Tiefenbrunn AJ, et al. Trends in reperfusion strategies, door-to-needle and door-to-balloon times, and in-hospital mortality among patients with ST-segment elevation myocardial infarction enrolled in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J. 2008;156:1035–44. doi: 10.1016/j.ahj.2008.07.029. [DOI] [PubMed] [Google Scholar]
- 13.Budaj A, Brieger D, Steg PG, Goodman SG, Dabbous OH, Fox KA, et al. Global patterns of use of antithrombotic and antiplatelet therapies in patients with acute coronary syndromes: Insights from the Global Registry of Acute Coronary Events (GRACE) Am Heart J. 2003;146:999–1006. doi: 10.1016/S0002-8703(03)00509-X. [DOI] [PubMed] [Google Scholar]
- 14.Fox KA, Goodman SG, Klein W, Brieger D, Steg PG, Dabbous O, et al. Management of acute coronary syndromes. Variations in practice and outcome; findings from the Global Registry of Acute Coronary Events (GRACE) Eur Heart J. 2002;23:1177–89. doi: 10.1053/euhj.2001.3081. [DOI] [PubMed] [Google Scholar]
- 15.Steg PG, Goldberg RJ, Gore JM, Fox KA, Eagle KA, Flather MD, et al. Baseline characteristics, management practices, and in-hospital outcomes of patients hospitalized with acute coronary syndromes in the Global Registry of Acute Coronary Events (GRACE) Am J Cardiol. 2002;90:358–63. doi: 10.1016/s0002-9149(02)02489-x. [DOI] [PubMed] [Google Scholar]
- 16.Tang EW, Wong CK, Herbison P. Global Registry of Acute Coronary Events (GRACE) hospital discharge risk score accurately predicts long-term mortality post acute coronary syndrome. Am Heart J. 2007;153:292–35. doi: 10.1016/j.ahj.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 17.Eagle KA, Nallamothu BK, Mehta RH, Granger CB, Steg PG, Van de Werf F, et al. Trends in acute reperfusion therapy for ST-segment elevation myocardial infarction from 1999 to 2006: We are getting better but we have got a long way to go. Eur Heart J. 2008;29:609–17. doi: 10.1093/eurheartj/ehn069. [DOI] [PubMed] [Google Scholar]
- 18.Goodman SG, Huang W, Yan AT, Budaj A, Kennelly BM, Gore JM, et al. The expanded Global Registry of Acute Coronary Events: Baseline characteristics, management practices, and hospital outcomes of patients with acute coronary syndromes. Am Heart J. 2009;158:193–201. doi: 10.1016/j.ahj.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 19.Hasdai D, Behar S, Wallentin L, Danchin N, Gitt AK, Boersma E, et al. A prospective survey of the characteristics, treatments and outcomes of patients with acute coronary syndromes in Europe and the Mediterranean basin; the Euro Heart Survey of Acute Coronary Syndromes (Euro Heart Survey ACS) Eur Heart J. 2002;23:1190–201. doi: 10.1053/euhj.2002.3193. [DOI] [PubMed] [Google Scholar]
- 20.Lenzen MJ, Boersma E, Bertrand ME, Maier W, Moris C, Piscione F, et al. European Society of Cardiology. Management and outcome of patients with established coronary artery disease: the Euro Heart Survey on coronary revascularization. Eur Heart J. 2005;26:1169–79. doi: 10.1093/eurheartj/ehi238. [DOI] [PubMed] [Google Scholar]
- 21.Mandelzweig L, Battler A, Boyko V, Bueno H, Danchin N, Filippatos G, et al. The second Euro Heart Survey on acute coronary syndromes: Characteristics, treatment, and outcome of patients with ACS in Europe and the Mediterranean Basin in 2004. Eur Heart J. 2006;27:2285–93. doi: 10.1093/eurheartj/ehl196. [DOI] [PubMed] [Google Scholar]
- 22.Xavier D, Pais P, Devereaux PJ, Xie C, Prabhakaran D, Reddy KS, et al. Treatment and outcomes of acute coronary syndromes in India (CREATE): A prospective analysis of registry data. Lancet. 2008;371:1435–42. doi: 10.1016/S0140-6736(08)60623-6. [DOI] [PubMed] [Google Scholar]
- 23.AlHabib KF, Hersi A, AlFaleh H, Kurdi M, Arafah M, Youssef M, et al. The Saudi project for assessment of coronary events (SPACE) registry: Design and results of a phase I pilot study. Can J Cardiol. 2009;25:e255–8. doi: 10.1016/s0828-282x(09)70513-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Roger VL, Weston SA, Gerber Y, Killian JM, Dunlay SM, Jaffe AS, et al. Trends in incidence, severity, and outcome of hospitalized myocardial infarction. Circulation. 2010;121:863–9. doi: 10.1161/CIRCULATIONAHA.109.897249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chin SP, Jeyaindran S, Azhari R, Wan Azman WA, Omar I, Robaayah Z, et al. Acute Coronary Syndrome (ACS) Registry - Leading the charge for National Cardiovascular Disease (NCVD) Database. Med J Malaysia. 2008;63:29–36. [PubMed] [Google Scholar]
- 26.The International Bank for Reconstruction and Development/The World Bank. World Development Report. 2007. pp. 288–9. [Google Scholar]
- 27.Al-Elq AH. Current practice in the management of patients with type 2 diabetes mellitus in Saudi Arabia. Saudi Med J. 2009;30:1551–6. [PubMed] [Google Scholar]
- 28.Eledrisi M, Alhaj B, Rehmani R, Alotaibi M, Mustafa M, Akbar D, et al. Quality of diabetes care in Saudi Arabia. Diabetes Res Clin Pract. 2007;78:145–6. doi: 10.1016/j.diabres.2007.02.017. [DOI] [PubMed] [Google Scholar]
- 29.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case control study. Lancet. 2004;364:937–52. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 30.Guy GW, Nunn AVW, Thomas LE, Bell JD. Obesity, diabetes and longevity in the Gulf: Is there a Gulf Metabolic Syndrome? IJDM. 2009;1:43–54. PLEASE PROVIDE FULL JOURNAL NAME. [Google Scholar]
- 31.Granger CB, Steg PG, Peterson E, López-Sendón J, Van de Werf F, Kline-Rogers E, et al. Medication performance measures and mortality following acute coronary syndromes. Am J Med. 2005;118:858–65. doi: 10.1016/j.amjmed.2005.01.070. [DOI] [PubMed] [Google Scholar]
- 32.Gupta M, Chang WC, Van de Werf F, Granger CB, Midodzi W, Barbash G, et al. International differences in hospital revascularization and outcomes following acute myocardial infarction: A multilevel analysis of patients in ASSENT-2. Eur Heart J. 2003;24:1640–50. doi: 10.1016/s0195-668x(03)00433-0. [DOI] [PubMed] [Google Scholar]
- 33.Panduranga P, Sulaiman K, Al-Zakwani I, Zubaid M, Rashed W, Al-Mahmeed W, et al. Utilization and determinants of in-hospital cardiac catheterization in patients with acute coronary syndrome from the Middle East. Angiology. 2010;61:744–50. doi: 10.1177/0003319710369794. [DOI] [PubMed] [Google Scholar]
- 34.Al-Mallah MH, Alsheikh-Ali AA, Almahmeed W, Sulaiman K, Al Suwaidi J, Ridha M, et al. Missed opportunities in the management of ST-segment elevation myocardial infarction in the Arab Middle East: Patient and physician impediments. Clin Cardiol. 2010;33:565–71. doi: 10.1002/clc.20802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Thalib L, Zubaid M, Rashed W, Almahmeed W, Al-Lawati J, Sulaiman K, et al. Regional variability in hospital mortality in patients hospitalized with ST-segment elevation myocardial infarction (STEMI): Findings from the Arabian Gulf Registry of Acute Coronary Events (Gulf RACE) Med Princ Pract. 2011;20:225–30. doi: 10.1159/000323595. [DOI] [PubMed] [Google Scholar]