Abstract
BACKGROUND AND OBJECTIVES
Media attention on 2009 H1N1 vaccination has been negative. Information on the willingness of health care workers (HCWs) to accept vaccination against the 2009 pandemic influenza is sparse. Thus, we undertook this study to investigate the attitude of HCWs toward this vaccine and possible factors associated with vaccine acceptance.
DESIGN AND SETTING
Cross-sectional observational study of HCWs conducted at Saudi Aramco Medical Services Organization (SAMSO) in February 2009.
PATIENTS AND METHODS
A self-administered questionnaire was distributed to 250 individuals and 161 (64.4%) were completed.
RESULTS
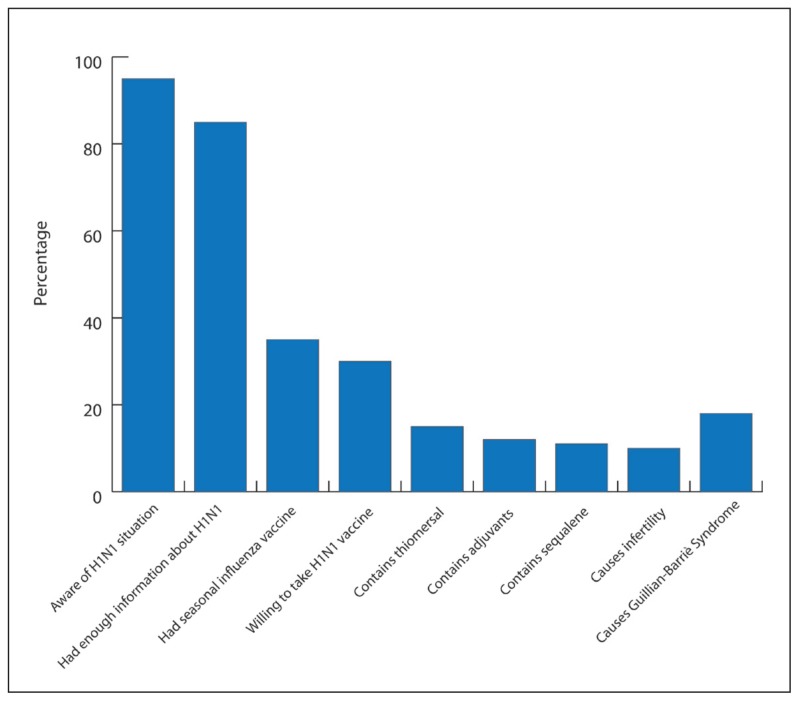
Of the total respondents, 66 (41%) were Arab, 55 (34.2%) were Asian/Far East, and 40 (24.8%) were of other nationalities. A total of 65 (40.4%) responses were from physicians and nurses, and 96 (59.6%) were from other HCWs. Of all the responders, 152 (94.4%) were aware of the H1N1 influenza situation, and 135 (83.9%) stated they had received enough information about the current situation. Of all the respondents, 59 (36.6%) stated that they received the seasonal influenza vaccination in 2008–2009, and 50 (31.1%) expressed their willingness to take the 2009 H1N1 vaccine. A total of 24 (14.9%) stated that the vaccine contains thiomersal, 21 (13%) stated that the vaccine contains adjuvants, 19 (11.8%) stated it contains squalene, 17 (10.6%) thought the vaccine causes infertility, and 29 (18%) thought the vaccine causes Guillain-Barré syndrome. In a multivariate analysis, the following factors were noted to be important in choosing to be vaccinated: being Asian, not being a doctor or a nurse, and previous acceptance of the seasonal influenza vaccine (P≤.01).
CONCLUSIONS
The acceptance of the current 2009 pandemic H1N1 vaccine was low. Important factors associated with the increasing H1N1 influenza vaccine acceptance include being Asian, not being a doctor or a nurse, and previous acceptance of the seasonal influenza vaccine.
Laboratory-confirmed cases of the 2009 pandemic influenza A (H1N1) have been reported in more than 213 countries and overseas territories or communities, with at least 16 455 deaths. According to recommendations from the World Health Organization (WHO), all countries should immunize their health care workers (HCWs) as a first priority to protect the vital health infrastructure. Information on the willingness of HCWs to accept vaccination against the 2009 pandemic influenza is sparse.1,2 Consequently, the goal of our study was to investigate the attitude of HCWs toward this vaccine and possible factors associated with vaccine acceptance.
PATIENTS AND METHODS
A cross-sectional observational study of HCWs was conducted at Saudi Aramco Medical Services Organization (SAMSO) in February 2009, once the pandemic 2009 H1N1 vaccine became available. The self-administered survey was distributed and HCWs were encouraged to complete the survey. A returned and completed form was taken as consent to participate in the survey.
The questionnaire was composed of four sections. The first section addressed demographic data, age, and profession. The second section contained information regarding the participant awareness and perceived risk of the 2009 H1N1 influenza, awareness of H1N1 influenza, whether they had enough information about the current situation, and how seriously they thought the H1N1 infection would affect their health. In addition, the last section contained questions related to the belief that the current H1N1 vaccine contained thiomersal, adjuvants, or squalene, or whether the vaccine might cause infertility or Gullian-Barré syndrome. The study was approved by the Public Relations Department of Saudi Aramco (Number 10-1089).
Data analysis was completed using the SPSS version 10.0 (IBM Corp., Armonk, NY USA). Statistical analyses used chi-square tests for comparison between categorical variables. Bivariate analysis was used to examine associations between vaccination status and other independent variables.
RESULTS
A total of 250 survey sheets were distributed and 161 (64.4%) were completed. Of the total respondents, 66 (41%) were Arab, 55 (34.2%) were Asian/Far East, and 40 (24.8%) were of other nationalities. A total of 65 (40.4%) were physicians and nurses, and 96 (59.6%) were from other HCWs that included technicians (13.6%) and administrators (10.5%). Of all the respondents, 152 (94.4%) stated they were aware of the H1N1 influenza situation and 135 (83.9%) stated they had received enough information about the current situation (Figure 1).
Figure 1.
Percentage of all respondents who answered positively to specific questions.
Of the total, 31 (19%) thought that the pandemic would last less than 6 months, 42 (26%) thought the pandemic would last less than 1 year, 23 (14.3%) thought more than 1 year, and the remaining (40.4%) were not sure of the duration of the pandemic. When asked about the effect of H1N1 on one’s own health, 57 (35.4%) thought that H1N1 would extremely affect their health, 68 (42.2%) thought it would somewhat affect their health, 13 (8.01%) thought it would not affect their health, and 23 (14.3%) were not sure of the effect. When asked about the risk of catching H1N1 disease, 45 (29.8%) felt it was low, 45 (28%) felt it was medium, 57 (35.4%) felt it was high, and 11 (6.8%) were not sure. Of all the respondents, 59 (36.6%) stated that they received the seasonal influenza vaccination in 2008–2009, and 50 (31.1%) expressed their willing to take the 2009 H1N1 vaccine. A total of 24 (14.9%) stated that the vaccine contains thiomersal, 21 (13%) stated that the vaccine contains adjuvants, 19 (11.8%) that it contains squalene, 17 (10.6%) thought the vaccine causes infertility, and 29 (18%) thought the vaccine causes Guillain-Barre Syndrome. In a bivariate analysis, nationality, profession, and the acceptance of the seasonal influenza vaccine were factors associated with choosing to take the vaccination (P=.01) (Table 1). In addition, these factors remained significant in a multivariate analysis (Table 2).
Table 1.
Bivariate analysis of associations between H1N1 vaccination acceptance and respondent characteristics.
| Category | Would take H1N1 vaccine, number (%) | Would not take H1N1 vaccine, number (%) | P value |
|---|---|---|---|
|
| |||
| Gender | |||
| Male | 19 (38) | 33 (29.7) | .36 |
| Female | 31 (62) | 78 (70.3) | |
| Nationality | .032 | ||
| Arab | 10 (20) | 56 (50.5) | |
| Asian | 28 (56) | 27 (24.3) | |
| European | 1 (2) | 16 (14.4) | |
| North American | 6 (12) | 5 (4.5) | |
| Others | 5 (10) | 7 (6.3) | |
| Job category | .002 | ||
| Physicians/Nurses | 11 (22) | 54 (48.6) | |
| Others | 39 (78) | 57 (51.4) | |
| Aware of the current situation | 1.0 | ||
| Yes | 47 (94) | 105 (94.6) | |
| No | 3 (6) | 6 (5.4) | |
| Enough information about the current situation | 1.0 | ||
| Yes | 42 (84) | 94 (84.7) | |
| No | 8 (16) | 17 (15.3) | |
| Duration of the epidemic | .77 | ||
| Short (<6 months) | 12 (24) | 2 (19.8) | |
| Medium (0.5-1 year) | 13 (26) | 29 (26.1) | |
| Long (>1 year) | 4 (8) | 16 (14.4) | |
| unsure | 21 (42) | 44 (39.6) | |
| Effect of H1N1 on own health | .17 | ||
| No effect | 3 (6) | 10 (9) | |
| Some effect | 19 (38) | 50 (45) | |
| Very serious | 22 (44) | 34 (30.6) | |
| Do not know | 6 (12) | 17 (15.3) | |
| Are you at risk of H1N1 infection? | .93 | ||
| High | 19 (38) | 38 (34.2) | |
| Medium | 14 (28) | 31 (27.9) | |
| Low | 14 (28) | 34 (30.6) | |
| Do not know | 3 (6) | 8 (7.2) | |
| Did you take seasonal influenza vaccine? | |||
| Yes | 34 (68) | 25 (22.5) | <.001 |
| No | 16 (32) | 86 (77.5) | |
| H1N1 vaccine contains/causes | |||
| Thiomersal | 4 (8) | 20 (18) | .15 |
| Adjuvants | 3 (6) | 18 (16.2) | .083 |
| Squalene | 2 (4) | 17 (15.3) | .061 |
| Infertility | 5 (10) | 12 (10.8) | 1.0 |
| Guillain-Barre Syndrome | .93 | ||
Table 2.
Multivariate analysis of significant factors associated with acceptance of vaccination against pandemic H1N1 influenza among health care workers.
| Category | Odds ratio (95% CI) |
|---|---|
|
| |
| Nationality | 2.5 (2.26-15.2) |
| Profession | 3.4 (1.45-8.07) |
| Seasonal influenza vaccine acceptance | 7.86 (3.5-17.62) |
DISCUSSIONS
Vaccination is one of the potentially effective measures that can reduce mortality and morbidity from pandemic influenza.2 The intention to accept vaccination against H1N1 influenza in our study was 31% at WHO alert phase 6, and with the availability of the vaccine free of charge. Similarly, in a previous study from Greece, less than 50% of HCWs were willing to accept the vaccine.2 In another study from Greece, the percentage of the public participants answering that they would probably not/definitely not accept the vaccine was between 47.1% in week 35 and 63.1% in week 44.3 In another study from Hong Kong, 45% of the public participants indicated their intention to take the free vaccination against influenza A/H1N1.4
In our study, only 36.6% of the respondents stated they had received the 2008–2009 seasonal influenza vaccine. The finding was consistent with our previous study showing that only 41% of HCWs received the seasonal influenza vaccination.5 Acceptance of the seasonal influenza vaccine was an important factor in acceptance of the pandemic H1N1 vaccine. A positive attitude toward seasonal influenza vaccination is a strong determinant for accepting the pandemic influenza vaccine as reported for H5N11,6 and pandemic influenza A (H1N1) vaccines.2 Similarly, in a survey of the Australian public, respondents who were vaccinated against seasonal influenza and those who perceived the 2009 pandemic (H1N1) to be severe were significantly more willing to accept vaccination.7
The perception that the H1N1 pandemic is not serious was perceived by 58.5% of the respondents. In addition, 54% felt that the impact of the H1N1 on their health is not severe. Consequently, these factors were not associated with the rate of the acceptance of the H1N1 vaccine. In New York, USA, some HCWs argued that influenza was not a health emergency and that the H1N1 influenza virus was not as serious as smallpox. Such perceptions may have resulted in the low acceptance of the vaccine.8 In a previous study, the main reason for the low acceptance of the vaccine was the perception that the 2009 pandemic influenza A (H1N1) is not a serious illness.1 In a study from Australia, most (78%) of the Australian public who responded to telephone interviews considered pandemic (H1N1) 2009 to be a mild disease, and 25% regarded themselves as being at increased risk of infection.7 In another study from India, 34.5% of an Indian population felt that their health would be seriously affected if they contracted Influenza A (H1N1).9 In the same study, 47.4% of an Indian population felt that they did not have enough information about the pandemic.9 In contrast of the total HCWs in our study, 83.9% stated they had received enough information about the current situation. HCWs also had misconceptions about the side effects of the H1N1 vaccine. However, this information was not associated with vaccine acceptance or vaccine rejection.
In conclusion, the low acceptance rate of the pandemic vaccine among international HCWs is alarming since HCWs are the example for patients and the public. Different strategies are needed to increase the awareness of HCWs. In addition, vaccination strategies against influenza A (H1N1) should include special efforts to disseminate information regarding the importance of the vaccine and its efficacy. The use of the internet to spread information should be utilized to increase the awareness and remove misconceptions about the influenza vaccine. Conducting specific educational programs to address concerns of HCWs and to promote the use of influenza vaccine is needed. Although, the current study was conducted on a specific population that may not necessarily be a representative of all health care providers, the study shows a general trend of a lower acceptance of the influenza vaccine by HCWs in general.
REFERENCES
- 1.Rachiotis G, Mouchtouri VA, Kremastinou J, Gourgoulianis K, Hadjichristodoulou C. Low acceptance of vaccination against the 2009 pandemic influenza A(H1N1) among health care workers in Greece. Euro Surveill. 2010;15 pii:19486. [PubMed] [Google Scholar]
- 2.Chor JS, Ngai KL, Goggins WB, Wong MC, Wong SY, Lee N, et al. Willingness of Hong Kong health care workers to accept pre-pandemic influenza vaccination at different WHO alert levels: Two questionnaire surveys. BMJ. 2009;339:3391. doi: 10.1136/bmj.b3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sypsa V, Livanios T, Psichogiou M, Malliori M, Tsiodras S, Nikolakopoulos I, et al. Public perceptions in relation to intention to receive pandemic influenza vaccination in a random population sample: Evidence from a cross-sectional telephone survey. Euro Surveill. 2009;14 pii:19437. [PubMed] [Google Scholar]
- 4.Lau JT, Yeung NC, Choi KC, Cheng MY, Tsui HY, Griffiths S. Acceptability of A/H1N1 vaccination during pandemic phase of influenza A/H1N1 in Hong Kong: Population based cross-sectional survey. BMJ. 2009;339:b4164. doi: 10.1136/bmj.b4164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Al-Tawfiq JA, Antony A, Abed MS. Attitudes towards influenza vaccination of multinationality health care workers in Saudi Arabia. Vaccine. 2009;27:5538–41. doi: 10.1016/j.vaccine.2009.06.108. [DOI] [PubMed] [Google Scholar]
- 6.Pareek M, Clark T, Dillon H, Kumar R, Stephenson I. Willingness of health care workers to accept voluntary stockpiled H5N1 vaccine in advance of pandemic activity. Vaccine. 2009;27:1242–7. doi: 10.1016/j.vaccine.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 7.Eastwood K, Durrheim DN, Jones A, Butler M. Acceptance of pandemic (H1N1) 2009 influenza vaccination by the Australian public. Med J Aust. 2010;192:33–6. doi: 10.5694/j.1326-5377.2010.tb03399.x. [DOI] [PubMed] [Google Scholar]
- 8.Stewart AM. Mandatory vaccination of health care workers. N Engl J Med. 2009;361:2015–7. doi: 10.1056/NEJMp0910151. [DOI] [PubMed] [Google Scholar]
- 9.Kamate SK, Agrawal A, Chaudhary H, Singh K, Mishra P, Asawa K. Public knowledge, attitude and behavioral changes in an Indian population during the Influenza A (H1N1) outbreak. J Infect Dev Ctries. 2009;4:7–14. doi: 10.3855/jidc.501. [DOI] [PubMed] [Google Scholar]