Abstract
For cancer survivors, who also often present with co-existing health conditions, exercise testing is often performed using submaximal protocols incorporating linear heart rate response for estimating cardiorespiratory capacity and assessing exercise tolerance. However, use of beta-blockers medications, during sub-maximal protocols based on linear HR response can be problematic. Rating of perceived exertion (RPE), which takes into account an individual’s overall perception of effort, can be used as a complementary tool that does not rely solely on heart rate response to increased workload. We compared heart rate response (VO2HR) and self-rating of perceived exertion (VO2RPE) in a graded submaximal exercise test (GXT) in 93 endometrial cancer survivors. Results of the GXT were stratified according to whether participants were taking beta-blocker (BB) medications or not (non-BB). Among non-BB participants, there was no difference between the mean VO2HR and the mean VO2RPE estimates of cardiorespiratory capacity (mlO2/ /kg/min), (20.4 and 19.3, respectively; p = 0.166). Among BB participants, the mean VO2HR approached significant difference than the mean VO2RPE, (21.7 mlO2/ /kg/min and 17.6 mlO2/ /kg/min, respectively; p = 0.087). Bland-Altman plots for both methods showed a proportional bias for the non-BB group; but not the BB group. Our results suggest that sub-maximal protocols based on Borg’s Rating of Perceived exertion (RPE) produce differing results from sub-maximal protocols based on HR response when applied to clinical population taking BB medications. Using RPE instead of HR for participants on BB medications, may be a better method for assessing exercise tolerance for estimating cardiorespiratory capacity in sub-maximal exercise testing.
Keywords: cardiorespiratory fitness, exercise testing, perceived effort
INTRODUCTION
Currently there are approximately 14.5 million U.S. cancer survivors, a number projected to continue to escalate dramatically (American Cancer Society, 2014; National Cancer Institute, 2013). Many cancer survivors tend to decrease their activity levels after diagnosis, and even for those who had been active, few return to their former levels of activity after treatment (Bourke et al, 2014; Courneya and Friedenreich, 1997; Schmitz et al, 2010). Adopting and maintaining a physically active lifestyle is an important intervention for cancer survivors because it can improve their emotional well-being (Benton, Schlairet, and Gibson, 2014; Courneya, 2003; Cuevas et al, 2014) and physical functioning (Hughes et al, 2015; Schmitz et al, 2010; Winters-Stone et al, 2012), as well as reduce the risk of other chronic diseases such as: cardiovascular disease (Kirkham et al, 2016; LaCroix et al, 1996); and cancer recurrence (Ballard-Barbash et al, 2012; Holmes et al, 2005; Schmitz et al, 2010).
For survivors to benefit from structured exercise, both exercise testing and recommended exercise programs need to be safe and at levels consistent with their medical history and current physical functional capacity. Although previously sedentary participants, are generally healthy for exercise programs, they often can have high levels of apprehension and concerns with the novelty of strenuous exertion as can be encountered during exercise testing. Use of sub-maximal protocols can help with such apprehension. Moreover, where medical supervision is limited, sub-maximal protocols may also be safer as well as more practical.
Another key consideration in designing exercise programs for cancer survivors is as an accurate assessment of the individual’s cardiorespiratory capacity. The gold standard assessment of cardiorespiratory capacity is measured maximal oxygen uptake (VO2max) (American College of Sports Medicine, 2013) utilizing ventilatory expired gases analyses at maximal effort. VO2max is determined by measuring volumetric oxygen consumption, in open circuit spirometry with cardiac monitoring, during increasing workloads until oxygen consumption plateaus.
Maximal exercise testing is typically performed for cardiopulmonary diagnostic purposes such as in individuals with high risk for significant cardiopulmonary disease (American College of Sports Medicine, 2013) or for purposes for the need for precise accuracy of true VO2max such as in testing for athletic programs (McArdle, Katch, and Katch, 2010). Maximal exercise testing may not be warranted for exercise programming for populations with high rates of comorbidity, with little or no previous exercise experience, or with other important factors that can make reaching a true VO2max an unreasonable expectation (Hautala et al, 2013). Factors can include fear of the novel physical exertion experience, lack of motivation to reach true maximal effort, lack of medical supervision and participant individual physical limitations (e.g. orthopedic issues). Thus for many practical reasons, VO2max is often estimated from submaximal exercise protocols (American College of Sports Medicine, 2013). Many protocols that estimate VO2max from sub-maximal testing rely on heart rate responding linearly to increases in workload up to the point of anaerobic threshold (Coquart et al, 2009; Lambrick, Faulkner, Rowlands, and Eston, 2009). However, for those individuals taking medications that can alter cardiovascular responses to workload (e.g. beta-blockers), the accuracy of estimating VO2max from sub-maximal protocols based on linear heart rate response can be called into question (Gauri et al, 2001), such as a blunted heart rate response from such medications that can result in an over-estimation of cardiorespiratory capacity (Tsai, Huang, Chen, and Ting, 2015). Alternative methods for estimating VO2max in cancer survivors that do not rely specifically on linear increases in heart rate with increased workload therefore warrant further investigation. In this study we wanted to compare such an alternative method based on rating of perceived exertion with heart rate response in participants taking beta-blocker medications.
Beta-blockers are a commonly used class of medications that alter cardiovascular responses to changes in physical effort. They work by blocking norepinephrine and epinephrine from beta receptors on tissue. When these beta receptors are blocked, nerve impulses are affected, resulting in a reduced response to increasing workload demands. Most BB medications are classified as “cardioselective”, indicating the selectivity to the myocardium; whereas, other BB medications are classified as non-selective affecting peripheral responses to the medication as well as the myocardium.
The Borg Rating of Perceived Exertion (RPE) scale is often used as an alternative to heart rate for measuring the intensity of physical activity (Borg, 1970). RPE, which has a linear relationship with oxygen uptake (Borg, 1982) is a validated measure for exercise intensity while assessing overall perceived physical and mental exertion from physical activity (Borg, 1998). This method has been validated in a variety of clinical populations such as: cardiac patients (Goss et al, 2011; Hautala et al, 2013; Tsai, Huang, Chen, and Ting, 2015); obese women (Coquart et al, 2009); as well as a variety of healthy populations (Lambrick, Faulkner, Rowlands, and Eston, 2009; Scherr et al, 2013), with correlations between VO2max and RPE ranging from 0.67 to 0.97. In our study we wanted to compare use of heart rate (VO2HR) and use of rating of perceived exertion (VO2RPE) in sub-maximal GXT in 93 post-treatment endometrial cancer survivors.
To investigate this comparison between methods, we conducted a secondary analyses of physiological responses during a graded cycle sub-maximal exercise test (GXT) conducted at baseline for 93 post-treatment endometrial cancer survivors who agreed to participate in a six month exercise intervention testing determinants of exercise adherence (Basen-Engquist et al, 2011). Data from the sub-maximal GXT were stratified according to whether participants were taking beta-blockers (BB) medications or not (non-BB). The purpose of this study was to investigate an alternative method for estimating VO2max in cancer survivors that does not rely specifically on linear increases in heart rate. We hypothesized that there would be no difference between VO2HR and VO2RPE estimates among participants in the non-BB group, but that estimated VO2HR would be higher than estimated VO2RPE for the BB group due to medically induced blunted heart rate response.
METHODS
We conducted a secondary analysis of baseline GXT data from a six-month exercise study for 100 previously sedentary post-treatment endometrial cancer survivors (Basen-Engquist et al, 2013). As part of baseline assessments, we conducted a submaximal graded cycle ergometer stress test with open circuit spirometry respiratory gas-exchange analysis for 93 of the 100 enrolled participants (detailed below). The primary goal of the parent study was concerned with how Social Cognitive Theory (Bandura, 1986) constructs relates to physical activity, so the GXT was designed to provide an exercise stimulus between cognitive tasks during the baseline assessment (Basen-Engquist et al, 2011). In addition, the GXT was used to provide an estimate of cardiorespiratory fitness while assessing individual exercise tolerance at intensity levels slightly higher than would be initially prescribed.
Participants
Participants were 100 previously sedentary women who had been diagnosed with stage I-IIIa endometrial cancer within the past 5 years and had been finished with treatment for at least 6 months with no evidence of current disease. Participants were excluded if they were physically active at moderate or greater intensity activity for at least 30 minutes on 5 or more days per week or vigorous intensity activity for at least 20 minutes on 3 or more days per week and had maintained that level of activity for 6 months or longer. Participants meeting this criteria were excluded as the primary objective of the parent study was to determine Social Cognitive Theory determinants of exercise adherence for sedentary endometrial cancer survivors for whom engaging in levels of physical activity meeting public health guidelines would be a novel behavior. Enrollment was contingent on a signed release from patients’ physicians indicating that they were sufficiently healthy to participate in a home-based exercise program and had no absolute contraindications for exercise testing as defined by ACSM’s Guidelines for Exercise Testing and Prescription (American College of Sports Medicine, 2009).
Participants were recruited from the gynecologic oncology clinic at The University of Texas MD Anderson Cancer Center (n = 59), MD Anderson’s outreach sites (n = 36), and a private gynecologic oncology practice in Houston, Texas (n = 5). All participants received a gift card worth $40 for completing the baseline assessments. The MD Anderson Institutional Review Board (IRB) approved all study procedures prior to recruiting any participants. Participants who were able to perform the exercise stress test at an adequate intensity to enable estimation of VO2max were split into two groups (beta-blocker and non-beta-blocker) according to whether or not they were taking any medication categorized as a beta-blocker.
GXT Procedures
Participants’ height (cm), weight (kg), resting electrocardiogram (ECG), resting blood pressure (mmHg) and resting heart rate in beats per minute (bpm) were recorded. If the participant did not present with any contraindications to exercise testing (American College of Sports Medicine, 2009), she was asked to complete a graded submaximal cycle ergometer exercise test (GXT). As this was the first exercise testing protocol initiated in a new facility and with the anticipated level of co-morbidity of our study population, cycle ergometry was chosen over a treadmill protocol to lessen participants’ risk of falling, to facilitate12-lead ECG monitoring and to facilitate blood pressure monitoring.
Before participants were tested, they received a detailed explanation of the procedure for the GXT, including how to interpret the Borg RPE scale (Borg, 1998) mounted on a 12” x 18” framed scale on the wall in front of the participants. We used the 15-point Borg RPE scale, which ranges from 6 (“no exertion at all”) to 20 (“maximal exertion”). Each participant was shown how to signal if for any reason she wished to immediately stop the GXT.
During the duration of the GXT, participants were connected to a Cardiac Science Quinton Q5000+ (Bothell, WA) for continuous 12-lead ECG monitoring and a SunTech Medical Tango+ (Morrisville, NC) automated blood pressure cuff interfaced to the Quinton was used for measuring blood pressure. Participants were connected with open-circuit spirometry to a ParvoMedics TrueOne 2400 (Sandy, UT) metabolic measurement system for measuring breath-by-breath respiratory gas exchange and ventilatory responses. The ParvoMedics controlled the resistance on a Lode Corival (Groningen, The Netherlands) exercise cycle per a specifically developed protocol detailed below.
Each participant began by pedaling for 60 seconds at no resistance on the cycle. This was followed by a warm-up phase of pedaling for 120 seconds at 20 watts (W) of resistance. Then the exercise phase began with one W of resistance added every six seconds to the initial 20W. Participants were encouraged to maintain a cadence of 60 ± 5 RPM during the exercise phase. Heart rate signal from the Quinton Q5000+ was interfaced with the metabolic cart. Continuous respiratory gas exchange breath-by-breath analysis of the metabolic cart included heart rate, breath-by-breath measurements of VO2 (mL/kg/min), VO2 (L/min), VCO2 (L/min), VE (L/min), VE/VO2, VE/VCO2, and Respiratory Exchange Ratio (RER) (VCO2/VO2) where VO2 is volume of oxygen (L/min), VE is minute ventilation (L/min), and VCO2 is volume of carbon dioxide (L/min). Blood pressure and RPE were recorded every 2 minutes. Resistance increased by one W every six seconds until the participant reached either: a sustained RER greater than 1.0; reached 85% of her age-predicted maximum heart rate; was unable to maintain the pedaling cadence of 60 RPM; presented with any abnormal blood pressure response or arrhythmia; or if the participant gave the signal that she wished to stop the test.
After reaching the exercise phase target point(s), resistance was dropped to 20W while the participant completed a “cool-down” recovery phase. Respiratory gas exchange, ventilatory response and heart rate continued to be monitored continuously while blood pressure and RPE were recorded every minute. Once the participant cooled down for a minimum of 2 minutes, the GXT was stopped and the equipment removed.
Statistical Analysis
We calculated VO2maxHR via ordinary least squares regression analysis using each participants’ respiratory gas exchange and ventilatory response test data. To smooth out the inherently noisy breath-by-breath data, 30-second average heart rate and VO2 levels were used in the regression analysis. Heart rates were linearly regressed onto corresponding VO2 (mlO2/kg/min) levels during the period from the beginning of the exercise phase (resistance greater than 21 W) to the exercise phase end point. This regression generated the prediction equation of VO2 level based on the linear relationship between VO2 and heart rate in the exercise phase. This linear relationship was then extrapolated to each participant’s age-predicted maximum heart rate (220 – current age) (Fox, Naughton, and Haskell, 1971) to predict VO2maxHR (mlO2/kg/min).
We used a similar linear regression procedure to calculate VO2maxRPE but RPE instead of HR was regressed onto corresponding VO2 (mlO2/kg/min) levels. As stated, RPE was collected every 2 minutes during the exercise phase. RPE was recorded into the Parvo metabolic cart each time participants identified their current RPE. Thus we paired the time the RPE was collected to the closest 30-second VO2 (mlO2/kg/min) average as indicated on the Parvo metabolic cart readout. A regression equation similar to one used for the VO2maxHR method, was created to regress the RPE level on VO2 levels during the exercise phase. The RPE was then extrapolated to a “maximum” RPE of 19, and predicted VO2max level for each participant was calculated on the basis of a linear relationship between VO2 and RPE. We used an RPE of 19 instead of 20 as the maximum point of an RPE level of 19 has been suggested as a more realistic RPE level for maximal effort during exercise testing (Faulkner, Parfitt, and Eston, 2007).
Treatment of Data
Participants who were taking beta-blocker (BB) medications or not (non-BB) were compared for responses in heart rate, RPE, VO2, RER and blood pressure during a GXT at start of the exercise phase (21W resistance), at 40W resistance, at 60W resistance and test termination criteria. The mean VO2maxHR was compared with the mean VO2maxRPE using paired-sample t-tests. The VO2max data were calculated using Microsoft Excel (Redmon, WA). Bland-Altman plots were generated to assess the level of agreement between both methods of VO2max estimates. Analyses of variables of interest were conducted using SPSS V 21.0 (Statistical Package for the Social Sciences), (SPSS, Inc., Chicago, Ill.).
RESULTS
Descriptive statistics for all 100 participants are shown in Table 1. Of the 100 participants, 7 were unable to perform the exercise stress test at an adequate intensity to enable estimation of VO2max. Of the remaining 93 participants, 70 reported they were not taking beta-blockers (non-BB), and 23 reported they were taking beta blocker (BB) medications. In our study 21 of the 23 participants were taking cardioselective BB medication; results from the GXT for the other two participants that were taking non-cardioselective BB were compared and found not to differ and therefore were included in the results.
Table 1.
Characteristics of Endometrial Cancer Survivors Enrolled in an Exercise Program (n = 100)
| Characteristic | Percent |
|---|---|
| Ethnicity | |
| Hispanic | 12 |
| Non-Hispanic | 86 |
| Data Missing | 2 |
| Race | |
| White | 84 |
| African American | 7 |
| Asian | 5 |
| American Indian | 1 |
| Pacific Islander | 0 |
| Other | 3 |
| Agea | |
| 40 y | 8 |
| 40–49 y | 12 |
| 50–59 y | 34 |
| 60–69 y | 35 |
| ≥ 70 y | 11 |
| Education | |
| Greater than bachelor’s degree | 17 |
| 4-year college degree | 24 |
| Some college | 36 |
| Technical/vocational degree | 8 |
| High school degree | 13 |
| Did not complete high school | 2 |
| BMIb | |
| < 25.0 kg/m2 (normal weight) | 15 |
| 25.0–29.9 kg/m2 (overweight) | 21 |
| 30.0–34.9 kg/m2 (class I obese) | 25 |
| 35.0–39.9 kg/m2 (class II obese) | 11 |
| ≥ 40.0 kg/m2 (class III obese) | 28 |
Mean [SD], 57.1 [11.1] years; range, 25.0–76.0 years.
Mean [SD], 34.3 [9.4] kg/m2; range 18.7–53.2 kg/m2.
The mean age of the BB group was 59.74 years (range, 40–76 years), and the mean age of the non-BB group was 55.87 years (range, 25–78 years; p = 0.149). The mean BMIs for the BB group and the non-BB group were 35.53 kg/m2 and 32.87 kg/m2, respectively (p = 0.191). Both groups were similar in demographic characteristics.
Table 2 details the physiological responses for BB and non-BB groups as they completed the GXT. This includes at the start of the exercise phase (21W), approximately half way through (40W) closer to the end (60W) and end of exercise phase. The resultant predictions of VO2max are also shown. For the non-BB group, 70 participants were tested; for the BB group 23 participants were tested. The number of participants completing each level of intensity differed and so noted in the table. As expected, the resting heart rate for the BB group (64.5 bpm) was significantly lower than that for the non-BB group (72.5 bpm, p < 0.001). This difference in HR between the two groups remained significant (lower for BB group) at 21W, 40W, 60W and at the end of exercise phase. The mean maximum heart rate achieved during the exercise test for the BB group (112.2 bpm) was significantly lower than that for the non-BB group (130.9 bpm, p < 0.001). However, RPE was not different between groups at any level of intensity. The BB group difference in a lower VO2 peak than the non-BB group approached significance (11.4 mlO2/kg/min versus 13.6 mlO2/kg/min, p = 0.052). Also approaching significant difference, was the lower watt resistance achieved for the BB-group compared to the non-BB group, (68.2W versus 77.1W, p = 0.075). Thus, though there was no significant difference in VO2 peak estimation between groups as noted below, the BB group had significantly lower heart rate at all workloads.
Table 2.
Physiological Responses During Sub-Maximal Cycle Exercise Test
| Variable | Non-BB Mean (SD) | BB-Group Mean (SD) | p |
|---|---|---|---|
| Age | 56.03 (11.6) | 59.96 (8.11) | 0.121 |
| BMI | 33.53 (9.14) | 36.70 (10.1) | 0.146 |
| Resting | n = 75 | n = 23 | |
| HR | 72.48 (9.51) | 64.48 (9.70) | <0.001 |
| SBP | 130.2 (18.2) | 134.2 (19.4) | 0.349 |
| DBP | 76.9 (8.44) | 73.8 (12.0) | 0.157 |
| 21W (Start Exercise Phase) | n = 70 | n = 23 | |
| HR | 95.85 (20.2) | 84.91 (14.0) | 0.020 |
| RPE | 9.59 (2.15) | 8.95 (1.70) | 0.227 |
| VO2 | 7.95 (2.06) | 7.27 (1.52) | 0.161 |
| SBP | 145.8 (23.8) | 151.6 (18.6) | 0.317 |
| DBP | 77.8 (10.6) | 75.8 (10.0) | 0.452 |
| RER | 0.82 (0.07) | 0.86 (0.11) | 0.047 |
| 40 W | n = 68 | n = 20 | |
| HR | 101.8 (19.6) | 91.85 (14.9) | 0.039 |
| RPE | 10.9 (2.28) | 10.6 (2.21) | 0.607 |
| VO2 | 9.12 (2.46) | 8.09 (1.57) | 0.075 |
| SBP | 153.6 (23.8) | 152.6 (17.8) | 0.859 |
| DBP | 76.1 (10.4) | 77.8 (9.88) | 0.505 |
| RER | 0.86 (0.07) | 0.90 (0.11) | 0.060 |
| 60 W | n = 53 | n = 15 | |
| HR | 112.8 (14.2) | 99.2 (20.7) | 0.005 |
| RPE | 12.4 (2.22) | 12.5 (2.20) | 0.855 |
| VO2 | 11.2 (3.96) | 10.2 (1.82) | 0.345 |
| SBP | 162.9 (21.8) | 162.5 (21.1) | 0.943 |
| DBP | 78.6 (9.82) | 76.9 (10.8) | 0.571 |
| RER | 0.92 (0.07) | 0.93 (0.11) | 0.775 |
| End of Testing Phase | n = 70 | n = 23 | |
| Wattage Achieved | 77.1 (21.0) | 68.2 (19.3) | 0.075 |
| HR | 130.9 (19.4) | 112.2 (20.6) | <0.001 |
| RPE | 13.5 (2.6) | 13.2 (2.4) | 0.619 |
| VO2peak | 13.6 (5.2) | 11.4 (3.5) | 0.052 |
| SBP | 175.5 (22.4) | 168.8 (34.6) | 0.285 |
| DBP | 79.5 (12.0) | 79.3 (12.8) | 0.942 |
| RER | 1.03 (0.07) | 1.02 (0.10) | 0.836 |
| Estimated VO2max | n = 70 | n=19 | |
| VO2maxHR | 20.4 (4.8) | 21.7 (6.5) | 0.308 |
| VO2maxRPE | 19.3 (7.3) | 17.6 (6.2) | 0.421 |
Note: BMI=Body Mass Index; HR = Heart Rate; SBP = Systolic Blood Pressure; DBP = Diastolic Blood Pressure RPE = Rating of Perceived Exertion; VO2= volume of oxygen uptake mlO2/kg/min; RER = Respiratory Exchange Ratio.
Among non-BB participants, there was no difference between the mean VO2HR and the mean VO2RPE estimates of cardiorespiratory capacity (VO2max), (20.4 and 19.3, respectively; p = 0.166), (Table 2). Among BB participants, the mean VO2HR approached significant difference from the mean VO2RPE, (21.7 and 17.6, respectively; p = .087). To better assess these two methods, Bland-Altman plots were created, (Figures 1 and 2). The non-BB group indicated a proportional bias with a negative slope (B = −.310, p = 0.004; B =−.423, p < 0.001, respectively).
Figure 1. Bland-Altman plot non-BB group VO2maxHR & VO2maxRPE.
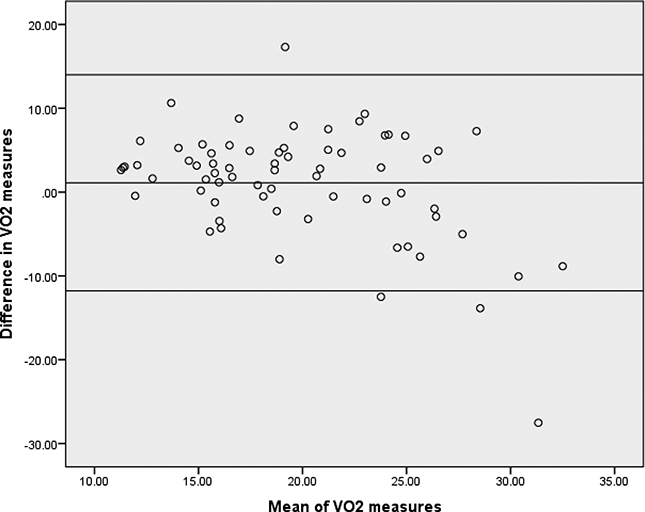
Note: Mean difference = 1.11; standard deviation= 6.57;
95% confidence limits: upper = 13.99, lower = −11.78
Regression coefficient B = −0.423, p < 0.001.
Figure 2. Bland-Altman plot BB group VO2maxHR & VO2maxRPE.
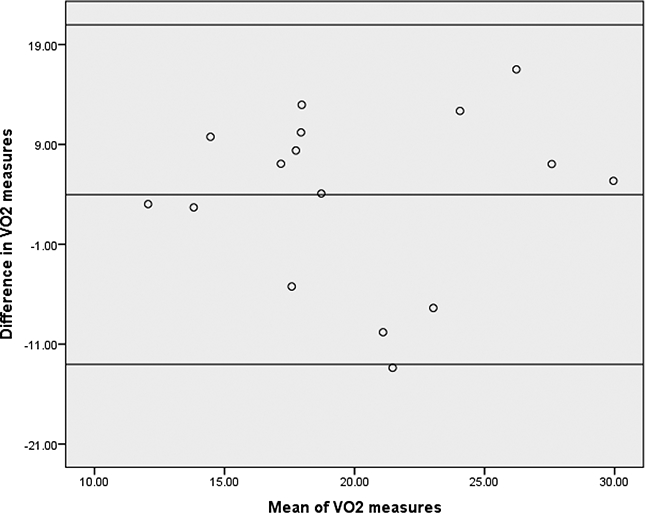
Note: Mean difference = 3.98; standard deviation= 8.67;
95% confidence limits: upper = 20.97; lower = −13.02
Regression coefficient B= 0.045, p = 0.868.
The bias seems to be greater where the mean for both methods is higher, i.e. where estimated VO2max max is higher. Bias was not evident in the BB group (B = 0.045, p = 0.868). An interpretation of these results is the use of HR for estimating VO2max for on BB medications may be a preferred method to using RPE, especially for those with greater cardiorespiratory capacity.
Exercise stage termination criteria is detailed in Table 3. There were similar percentage of participants in the BB group (56.5%) and the non-BB group (55.1%) that reached an RER ≥ 1.0 as the primary criteria for stopping the exercise stage. Eighteen (26.1%) of non-BB group participants reached 85% of age-predicted maximum HR; whereas, only two of the BB group participants did (8.7%). Three of the non-BB group participants reached both criteria of 85% HR and RER ≥ 1.0 whereas no BB-group participants did. As illustrated on Table 3, similar % of participants in both groups were unable to maintain cadence, were stopped due to high blood pressure, or indicated the desire to stop the test.
Table 3.
Test Termination Criteria Group Comparison
| Variable |
Non-BB
n = 70 n (%) |
BB n = 23 n (%) |
|---|---|---|
| Reached RER ≥ 1.0 | 38 (55.1) | 13 (56.5) |
| Reached 85% of age predicted HR | 18 (26.1) | 2 (8.7) |
| Reached both RER & HR | 3(4.3) | 0 (0.0) |
| Unable to maintain cadence | 4 (5.8) | 2 (8.7) |
| High blood pressure response | 4 (5.8) | 2 (8.7) |
| Participant wanted to stop | 2 (2.7) | 1 (4.3) |
| Other | ||
| (equipment malfunction) | 1 (4.3) | |
| (no supervision – test stopped at 70%) | 1 (4.3) | |
| (GXT test stopped early by tech) | 1 (1.3) | 1 (4.3) |
DISCUSSION
We examined physiological responses using continuous heart rate monitoring and breath: breath respiratory gas exchange analysis in sedentary (i.e. not moderately active ≥ 30 minutes on ≥ 5 days per week or vigorously active ≥ 20 minutes on ≥ 3 days per week) post-treatment endometrial cancer survivors performing a ramped sub-maximal cycle ergometry exercise stress test. Results were stratified according to beta blocker medications usage and we used the physiological response data to estimate VO2max (mlO2/kg/min) using two methods: heart rate response and RPE.
Resting heart rate and heart rate response during the GXT were different between groups. However, both groups self-reported no differences in levels of perceived exertion (RPE) during the GXT. The two methods of estimating VO2max did not differ in the non-BB group (p = 0.166) and approached significant difference in the BB group (p = 0.087). We acknowledge that without participants performing a maximal stress test to reach a true VO2max, it is not possible to determine which method (HR or RPE) is a more accurate method of estimating VO2max from a sub-maximal GXT for participants taking BB medications. From a practical standpoint, however, there are indeed many instances where a maximal stress test is not the preferred option, (e.g. need for medical supervision) or justified in terms of participant risk and comfort.
Our results suggest that RPE can be used as a viable alternative method to heart rate response for assessing exercise tolerance when use of heart rate is not always possible to collect or not always as accurate in sub-maximal protocols as in the case of participants on BB medications where heart rate response is blunted.
Our argument is based on our GXT results that as exercise intensity increased both groups responded with similar RPE regardless/independent of beta blocker medications usage but presented with different heart rate responses. In the case of those on BB medications heart rate response during exercise is in fact blunted (American College of Sports Medicine, 2013; Eston and Connolly, 1996; Tang et al, 2016; Tsai, Huang, Chen, and Ting, 2015), which could result in an overestimation of cardiorespiratory capacity in sub-maximal protocols. Our results suggest that RPE may be a viable alternative approach for estimating cardiorespiratory capacity in sub-maximal protocols, as both our groups reported similar RPE values at all workloads but the BB-blocker group recorded lower heart rate responses at all workloads when compared to the non-BB blocker group.
Our results should be interpreted in light of several limitations. First, we performed a submaximal stress test with stopping points short of maximal effort. The comparison of the two methods would be more valid with a truly maximal stress test. This is an important area for future clinical research: comparing submaximal methods of estimating VO2max with maximal testing specific for populations such as post-treatment cancer survivors. For our study we opted for submaximal testing as the main focus of the GXT was to provide a consistent, structured exercise stimulus between cognitive assessments. VO2max was not the study’s main endpoint and we had scheduling challenges to secure the necessary medical supervision for maximal testing of higher at-risk participants (American College of Sports Medicine, 2009). Thus, for our given circumstances and the overarching objectives of the parent study a sub-maximal protocol was the preferred choice. Other researchers and clinicians may face similar issues. Use of RPE versus heart rate to estimate cardiorespiratory capacity in these applications may be a viable alternative.
RPE is often used as additional information during submaximal and maximal exercise testing (American College of Sports Medicine, 2013; Coquart et al, 2014). RPE has been used as a guideline for exercise termination as well as exercise prescription in populations on BB medication (Eston and Connolly, 1996; Tang et al, 2016; Tsai, Huang, Chen, and Ting, 2015). Our results provide support for RPE as a preferred alternative for post-treatment endometrial cancer survivors on BB in assessing exercise tolerance and thus applicable in estimating cardiorespiratory capacity and subsequent exercise prescription.
We also acknowledge a limitation that this was the first exposure to the concept of RPE for almost all our participants. Therefore, our participants may not have been able to accurately anchor their level of exertion on the basis of the RPE scale. Finally, our participants had cardiorespiratory capacity in the lowest percentiles of published norms (American College of Sports Medicine, 2013), so they spent a relatively small amount of time in the exercise phase of the testing protocol (approximately 7–9 minutes). Therefore, we had fewer data collection points with which to generate a prediction regression equation.
However, despite these limitations our results do suggest that using RPE to assess exercise tolerance and estimate cardiorespiratory capacity is a viable alternative in sub-maximal exercise test protocols in endometrial cancer survivors using BB-medications. Further research evaluating the use of RPE as a criterion for maximal VO2max testing for special populations such as post-treatment cancer survivors is warranted.
ACKNOWLEDGEMENT
This study was supported by R01 CA 109919, R25T CA 057730, R25E CA 056452, K01 CA 134550, U54CA153511, U30 CA 016672 (PROSPR Shared Resource) and the Center for Energy Balance in Cancer Prevention and Survivorship, Duncan Family Institute for Cancer Prevention and Risk Assessment.
Footnotes
Declaration of Interest
The authors report no conflicts of interest.
REFERENCES
- American Cancer Society; 2014. Cancer Facts and Figures. Atlanta, GA, American Cancer Society. [Google Scholar]
- American College of Sports Medicine 2009. ACSM’s Guidelines for Exercise Testing and Prescription (8th ed). Philadelphia, PA, Lippincott Williams & Wilkins. [Google Scholar]
- American College of Sports Medicine 2013. ACSM’s Guidelines for Exercise Testing and Prescription (9th ed). Philadelphia. PA, Lippincott Williams & Wilkins. [DOI] [PubMed] [Google Scholar]
- Ballard-Barbash R, Friedenreich CM, Courneya KS, Siddiqi SM, McTiernan A, Alfano CM 2012. Physical activity, biomarkers, and disease outcomes in cancer survivors: A systematic review. Journal of the National Cancer Institute 104: 815–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A 1986. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ, Prentice-Hall. [Google Scholar]
- Basen-Engquist K, Carmack CL, Li Y, Brown J, Jhingran A, Hughes DC, Perkins HY, Scruggs S, Harrison C, Baum G, Bodurka DC, Waters A 2013. Social-cognitive theory predictors of exercise behavior in endometrial cancer survivors. Health Psychology 32: 1137–1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basen-Engquist K, Carmack CL, Perkins H, Hughes D, Serice S, Scruggs S, Pinto B, Waters A 2011. Design of the steps to health study of physical activity in survivors of endometrial cancer: Testing a social cognitive theory model. Psychology of Sport and Exercise 12: 27–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benton MJ, Schlairet MC, Gibson DR 2014. Change in quality of life among breast cancer survivors after resistance training: Is there an effect of age? Journal of Aging and Physical Activity 22: 178–185. [DOI] [PubMed] [Google Scholar]
- Borg G 1970. Perceived exertion as an indicator of somatic stress. Scandinavian Journal of Rehabilitation Medicine 2: 92–98. [PubMed] [Google Scholar]
- Borg G 1982. Ratings of perceived exertion and heart rates during short-term cycle exercise and their use in a new cycling strength test. International Journal of Sports Medicine 3: 153–158. [DOI] [PubMed] [Google Scholar]
- Borg G 1998. Borg’s Perceived Exertion and Pain Scales. Champaign, IL, Human Kinetics. [Google Scholar]
- Bourke L, Homer KE, Thaha MA, Steed L, Rosario DJ, Robb KA, Saxton JM, Taylor SJ 2014. Interventions to improve exercise behaviour in sedentary people living with and beyond cancer: A systematic review. British Journal of Cancer 110: 831–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coquart JB, Garcin M, Parfitt G, Tourny-Chollet C, Eston RG 2014. Prediction of maximal or peak oxygen uptake from ratings of perceived exertion. Sports Medicine 44: 563–578. [DOI] [PubMed] [Google Scholar]
- Coquart JB, Lemaire C, Dubart AE, Douillard C, Luttenbacher DP, Wibaux F, Garcin M 2009. Prediction of peak oxygen uptake from sub-maximal ratings of perceived exertion elicited during a graded exercise test in obese women. Psychophysiology 46: 1150–1153. [DOI] [PubMed] [Google Scholar]
- Courneya KS 2003. Exercise in cancer survivors: An overview of research. Medicine and Science in Sports and Exercise 35: 1846–1852. [DOI] [PubMed] [Google Scholar]
- Courneya KS, Friedenreich CM 1997. Relationship between exercise pattern across the cancer experience and current quality of life in colorectal cancer survivors. Journal of Alternative and Complementary Medicine 3: 215–226. [DOI] [PubMed] [Google Scholar]
- Cuevas BT, Hughes DC, Parma DL, Trevino-Whitaker RA, Ghosh S, Li R, Ramirez AG 2014. Motivation, exercise, and stress in breast cancer survivors. Supportive Care in Cancer 22: 911–917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eston R, Connolly D 1996. The use of ratings of perceived exertion for exercise prescription in patients receiving beta-blocker therapy. Sports Medicine 21: 176–190. [DOI] [PubMed] [Google Scholar]
- Faulkner J, Parfitt G, Eston R 2007. Prediction of maximal oxygen uptake from the ratings of perceived exertion and heart rate during a perceptually-regulated sub-maximal exercise test in active and sedentary participants. European Journal of Applied Physiology 101: 397–407. [DOI] [PubMed] [Google Scholar]
- Fox SM, Naughton JP, Haskell WL 1971. Physical activity and the prevention of coronary heart disease. Annals of Clinical Research 3: 404–432. [PubMed] [Google Scholar]
- Gauri AJ, Raxwal VK, Roux L, Fearon WF, Froelicher VF 2001. Effects of chronotropic incompetence and beta-blocker use on the exercise treadmill test in men. American Heart Journal 142: 136–141. [DOI] [PubMed] [Google Scholar]
- Goss FL, Robertson RJ, Haile L, Nagle EF, Metz KF, Kim K 2011. Use of ratings of perceived exertion to anticipate treadmill test termination in patients taking beta-blockers. Perceptual and Motor Skills 112: 310–318. [DOI] [PubMed] [Google Scholar]
- Hautala AJ, Kiviniemi AM, Karjalainen JJ, Piira OP, Lepojarvi S, Makikallio T, Huikuri HV, Tulppo MP 2013. Peak exercise capacity prediction from a submaximal exercise test in coronary artery disease patients. Frontiers in Physiology 4: 243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes MD, Chen WY, Feskanich D, Kroenke CH, Colditz GA 2005. Physical activity and survival after breast cancer diagnosis. JAMA 293: 2479–2486. [DOI] [PubMed] [Google Scholar]
- Hughes DC, Darby N, Gonzalez K, Boggess T, Morris RM, Ramirez AG 2015. Effect of a six month yoga exercise intervention on fitness outcomes for breast cancer survivors. Physiotherapy Theory and and Practice 31: 451–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkham AA, Bland KA, Sayyari S, Campbell KL, Davis MK 2016. Clinically relevant physical benefits of exercise interventions in breast cancer survivors. Current Oncology Reports 18: 12. [DOI] [PubMed] [Google Scholar]
- LaCroix AZ, Leveille SG, Hecht JA, Grothaus LC, Wagner EH 1996. Does walking decrease the risk of cardiovascular disease hospitalizations and death in older adults? Journal of the American Geriatrics Society 44: 113–120. [DOI] [PubMed] [Google Scholar]
- Lambrick DM, Faulkner JA, Rowlands AV, Eston RG 2009. Prediction of maximal oxygen uptake from submaximal ratings of perceived exertion and heart rate during a continuous exercise test: The efficacy of RPE 13. European Journal of Applied Physiology 107: 1–9. [DOI] [PubMed] [Google Scholar]
- McArdle WD, Katch FI, Katch VL 2010. Exercise Physiology: Nutrition, Energy, and Human Performance (7th ed). Philadelphia, PA, Lippincott Williams & Wilkins. [Google Scholar]
- National Cancer Institute 2013 Estimated U.S. Cancer Prevalence Counts: Method. http://cancercontrol.cancer.gov/ocs/prevalence/prevalence.html#prevalence-projections.
- Scherr J, Wolfarth B, Christle JW, Pressler A, Wagenpfeil S, Halle M 2013. Associations between Borg’s rating of perceived exertion and physiological measures of exercise intensity. European Journal of Applied Physiology 113: 147–155. [DOI] [PubMed] [Google Scholar]
- Schmitz KH, Courneya KS, Matthews C, Demark-Wahnefried W, Galvao DA, Pinto BM, Irwin ML, Wolin KY, Segal RJ, Lucia A, Schneider CM, von Gruenigen VE, Schwartz AL 2010. American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Medicine and Science in Sports and Exercise 42: 1409–1426. [DOI] [PubMed] [Google Scholar]
- Tang LH, Zwisler AD, Taylor RS, Doherty P, Zangger G, Berg SK, Langberg H 2016. Self-rating level of perceived exertion for guiding exercise intensity during a 12-week cardiac rehabilitation programme and the influence of heart rate reducing medication. Journal of Science and Medicine in Sport 19: 611–615. [DOI] [PubMed] [Google Scholar]
- Tsai SW, Huang YH, Chen YW, Ting CT 2015. Influence of beta-blockers on heart rate recovery and rating of perceived exertion when determining training intensity for cardiac rehabilitation. Journal of the Chinese Medical Assocition 78: 520–525. [DOI] [PubMed] [Google Scholar]
- Winters-Stone KM, Dobek J, Bennett JA, Nail LM, Leo MC, Schwartz A 2012. The effect of resistance training on muscle strength and physical function in older, postmenopausal breast cancer survivors: A randomized controlled trial. Journal of Cancer Survivorship 6: 189–199. [DOI] [PMC free article] [PubMed] [Google Scholar]


