Abstract
Background
Tele-rehabilitation for stroke survivors has emerged as a promising intervention for remotely supervised administration of physical, occupational, speech and other forms of therapies aimed at improving motor, cognitive and neuropsychiatric deficits from stroke.
Objective
To provide an updated systematic review on the efficacy of tele-rehabilitation interventions for recovery from motor, higher cortical dysfunction and post-stroke depression among stroke survivors.
Methods
We searched PubMed and Cochrane library from January 1, 1980 to July 15, 2017 using the following keywords: Telerehabilitation stroke”, “Mobile health rehabilitation”, “Telemedicine stroke rehabilitation”, Telerehabilitation. Our inclusion criteria were randomized controlled trials, pilot or feasibility trials that included an intervention group that received any tele-rehabilitation therapy for stroke survivors compared with a control group on usual or standard of care.
Results
This search yielded 49 abstracts. By consensus between two investigators, 22 publications met the criteria for inclusion and further review. Tele-rehabilitation interventions focused on motor recovery (n=18), depression or caregiver strain (n=2) and higher cortical dysfunction (n=2). Overall, tele-rehabilitation interventions were associated with significant improvements in recovery from motor deficits, higher cortical dysfunction and depression in the intervention groups in all studies assessed but significant differences between intervention versus control groups were reported in 8 out of 22 studies in favor of tele-rehabilitation group while the remaining studies reported non-significant differences.
Conclusion
This updated systematic review provides evidence to suggest that tele-rehabilitation interventions have either better or equal salutary effects on motor, higher cortical and mood disorders compared with conventional face-to-face therapy.
Keywords: Tele-rehabilitation, post-stroke recovery, motor function, higher cortical dysfunction
INTRODUCTION
Rehabilitation after stroke requires the inputs of several skilled health personnel including physiatrists, physiotherapists, speech therapists and occupational therapists. These human resources are often unavailable engendering inadequate recovery from physical limitations among stroke survivors. Furthermore, supervised rehabilitation is often challenged by transportation restrictions of getting to hospitals and inconvenience. (1). Home-based tele-rehabilitation- defined as the use of telecommunication devices (such as telephone, videophone) by a clinician to provide evaluation and distance support for disabled persons living at home- (2,3)- provide a viable avenue to meet the rehabilitation needs of stroke survivors in resource-limited rural settings in developed countries as well as Low-and-Middle Income countries where stroke burden is rapidly escalating. (4,5)
Evidence of the efficacy of tele-rehabilitation after stroke has begun to accrue from randomized controlled trials. A meta-analysis in 2015 by Chen et al, involving 7 RCTs, assessed whether tele-rehabilitation led to improvement in abilities of activities of daily living of stroke patients at home and found no significant differences in abilities of activities of daily living and motor function between groups from pooled data. (6) An updated appraisal of the literature is justified since the last review was conducted 2 years ago and more studies using novel approaches have since been published. Furthermore, TR has been deployed for the home management of higher cortical dysfunction and depression after stroke in addition to physical rehabilitation of motor deficits.
METHODS
We searched PubMed and Cochrane Library from January 1, 1980 to June 30, 2017 using the following keywords: “Telerehabilitation stroke”, “Mobile health rehabilitation”, “Telemedicine stroke rehabilitation”, Telerehabilitation. We employed a systematic search methodology and study selection process.
Eligibility for inclusion were:
Randomized controlled trials, pilot or feasibility trials, that reported the utilization of tele-rehabilitation for stroke survivors and a control group or usual care group.
Rehabilitation interventions and assessments by telemedicine, telecommunication media, and intervention programs including phone, videoconferencing, telerehabilitation system, robot-assisted rehabilitation, and virtual and augmented reality therapy.
Comparator groups were conventional rehabilitation, no rehabilitation.
Minimum cumulative duration of rehabilitation intervention of 2 weeks.
Exclusion criteria
Literature reviews, meta-analysis, commentaries, concept papers on Tele-rehabilitation after stroke.
Search items were based on appropriate Medical subject headings and other headings including stroke, cerebrovascular accident, post-stroke, telerehabilitation, rehabilitation, telemedicine, home. No language restrictions were imposed on the searches or the identified studies. The articles included in this study underwent independent appraisal, data abstraction by 2 investigators (U.U. and F.S.S.) and B.O. served as arbiter for consensus. The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement was followed for the systematic review.
Outcome measures
Common outcome measures used to assessed outcomes after tele-rehabilitation interventions included Barthel Index (BI) scale7, the Berg Balance Scale (BBS)8, Functional Independence Measure scale9. Other assessments of motor function were Fugl-Meyer Extremity test10, Wolf Motor Function Test, Timed Up and Go test, Nine Peg Test11, Action Research Arm Test,12 walking speed and Ashworth scale13, health-related quality of life (e.g. EuroQol-5 Dimension [EQ-5D]14, Short Form Health Survey15), caregivers stress (e.g. Caregivers’ Strain Index16), satisfaction (such as Satisfaction with Stroke Care Questionnaire17, satisfaction questionnaire), cognitive function (e.g. Mini-mental State Examination).
RESULTS
The search identified 1,331 records of which 49 were thought to be eligible based on their titles and abstract. The full texts of the 49 articles were retrieved and reviewed and 22 studies were deemed to fulfill the predefined inclusion criteria for the systematic review as shown in Figure 1. Eighteen (18) studies assessed the effect of tele-rehabilitation on motor function18–23,25,28–30,32–39, two were on depression26,31 and two on higher cortical dysfunction namely aphasia27 and hemi-neglect24. Studies were conducted in the United States (n=7), Italy (n=3), China (n=2), Spain (n=2), United Kingdom (n=2), Australia (n=1), Brazil (n=1), Malaysia (n=1), Netherlands (n=1), South Korea (n=1), and Thailand (n=1). Among the studies that focused on motor rehabilitation, the duration of the intervention ranged between two weeks to 24 weeks with sample size in the intervention group ranging between 5 and 51. (Table 1) Among 18 studies on motor deficits, 11 studies assessed interventions on mobility or movement limitations imposed by hemiparesis18,19,21–23,25,29,30,32,33,35-, 6 studies centered interventions on upper limb limitations20,28,36–39 and 1 on ankle disability from stroke34. In general, all studies reviewed reported improvements in motor disabilities in the intervention groups receiving tele-rehabilitation as well as the control group in most primary and secondary outcome measures. However 7 out of the 18 studies on motor dysfunction reported significant improvements over time in the intervention group compared with comparator control groups.19–21,25,28,33,34 In addition, the study by Lloréns R et al which assessed cost-effectiveness of tele-rehabilitation showed that the in-clinic intervention resulted in more expenses than the telerehabilitation program (654.72 $ per person)30.
Figure 1.
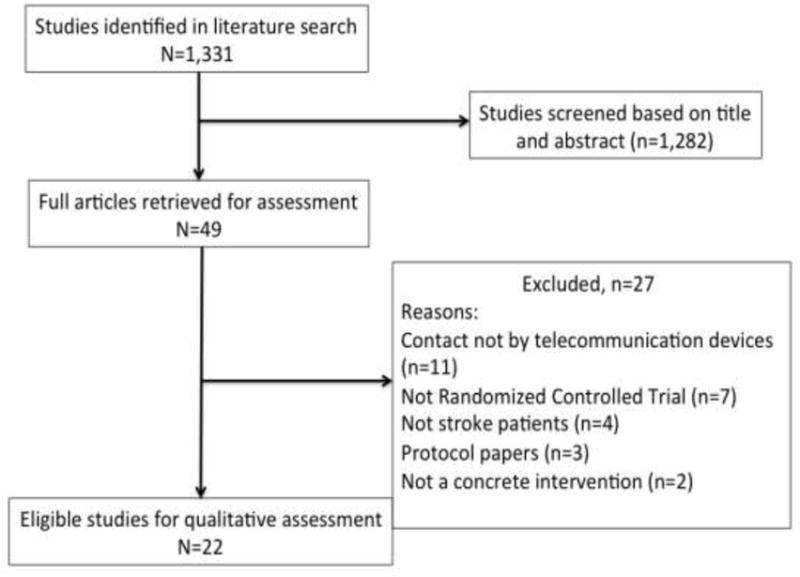
Flow diagram of assessment of studies identified in the systematic review.
Table 1.
Characteristics and outcomes of randomized controlled trials of studies included the systematic review.
| Author, year, country | Objectives | Intervention | Telerehabilitation Technology device | Population | Deficits and Outcome category measured | Results |
|---|---|---|---|---|---|---|
| Chen et al, 2017 China [18] |
1. To evaluate the effects of home-based tele-supervised rehabilitation on physical function for stroke survivors 2. To determine if rehabilitation therapy can relieve the burden on caregivers |
Physical exercises and electromyography-triggered neuromuscular stimulation (ETNS) versus Conventional therapy 12 weeks intervention |
Phone-based | Intervention Group (I.G.): n = 27 Control Group (C.G.): n=27 |
HEMIPLEGIA (Motor) Modified Barthel Index (MBI), Berg Balance Scale (BBS), Modified Rankin Scale (mRS), Caregiver Strain Index, Root mean square (RMS) of extensor carpi radialis longus and tibialis anterior muscle |
Both groups demonstrated significant effects within groups over the 3 time points in increasing MBI, BBS, RMS value of extensor carpi radialis longus and tibialis anterior, and decreasing Caregiver Strain Index (P < .001). No significant between-group differences. Percentage of participants with MRS grades 0 and 1 in 2 groups increased over time without significant difference between the groups |
|
| ||||||
| da Fonseca, et al, 2017 Brazil [19] |
Assess the therapeutic effect of virtual reality associated with conventional physiotherapy on gait balance and the occurrence of falls after a stroke |
Virtual Reality therapy program versus Conventional treatment 10 weeks intervention |
Computer-based | I.G. n=14 C.G. n=13 |
HEMIPARESIS (Motor) Dynamic Gait Index, Number of falls |
Improved gait balance and reduced occurrence of falls in both groups. Improved gait balance in the I.G. vs C.G (P = .047) Reduction in falls in the I.G. vs C.G. (P = .049) Intergroup analysis: no difference in the two outcomes |
| Choi et al., 2016 South Korea [20] |
To develop and evaluate the feasibility and effectiveness of a mobile game-based upper extremity virtual reality program for stroke patients |
Virtual Reality Rehab program on Smartphone and a tablet PC (MoU-Rehab) vs Conventional OT 2 weeks intervention |
Phone-based | I.G. n=12 C.G: n=12 |
UPPER LIMB DYSFUNCTION (Motor) Fugl–Meyer Assessment of the upper extremity [FMA-UE], Brunnström stage [B-stage] for the arm and the hand, Manual muscle testing [MMT], Modified Barthel Index (MBI), EuroQol-5 Dimension [EQ-5D], Beck Depression Inventory [BDI], Satisfaction questionnaire |
A greater improvement in the FMA-UE, B-stage, and MMT found after treatment with the MoU-Rehab than with conventional therapy Improvements in the MBI, EQ-5D, and BDI was not significantly different between the two groups Experimental group completed treatment without adverse effects, and were generally satisfied with MoU-Rehab |
| Lorna Paul, 2016 UK [21] |
To evaluate the potential effectiveness of STARFISH in stroke survivors | Mobile phone app-based behavioral change intervention (STARFISH) vs Usual care 6 weeks intervention |
Phone-based | I.G. n=16 C.G. n=8 |
PHYSICAL ACTIVITY (Motor) Physical activity, Sedentary time, Fatigue Severity Scale, Instrumental Activity of Daily Living Scale, Ten-Meter Walk Test, Stroke Specific Quality of Life Scale, and Psychological General Well-Being Index |
Average daily step count increased by 39.3% in the I.G. and reduced by 20.2% in the C.G. (P = 0.005 for group-time interaction) Similar patterns of data and group-time interaction were seen for walking time (P = 0.002) and fatigue (P = 0.003) No significant group–time interactions for other outcome measures |
|
| ||||||
| van den Berg et al, 2016, Australia [22] | To investigate the effects of Caregiver-Mediated Exercises program commenced in hospital plus e-health support on self-reported mobility. |
Caregiver-mediated training program with e-health support versus Usual care 8 weeks intervention |
Tablet-based | I.G., n=31 C.G., n=32 |
MOBILITY CHALLENGES (Motor) Stroke Impact Scale mobility domain, Length of stay, Other Stroke Impact Scale domains, readmissions, motor impairment, strength, walking ability, balance, mobility, (extended) activities of daily living, Psychosocial functioning, Self-efficacy, Quality of life, and fatigue |
ITT: No between-group difference in Stroke Impact Scale mobility (P = 0.6); Careers reported less fatigue (4.6, confidence interval [CI] 95% 0.3–8.8; P = 0.04) and higher self-efficacy (−3.3, CI 95% −5.7 to −0.9; P = 0.01) at week 12 Per-protocol analysis: I.G. demonstrated a trend toward improved mobility (−9.8, CI 95% −20.1 to 0.4; P=0.06), significantly improved extended activities of daily living scores at week 8 (−3.6, CI 95% −6.3 to −0.8; P=0.01) and week 12 (3.0, CI 95% −5.8 to −0.3; P=0.03), a 9-day shorter length of stay (P=0.046), and fewer readmissions over 12 months (P < 0.05) |
|
| ||||||
| Wolf, et al. 2015 USA [23] |
To determine the efficacy of a home-based telemonitored robotic-assisted therapy as part of a home exercise program (HEP) compared with a dose-matched HEP-only intervention among individuals underserved stroke survivors < 6 months |
Robotic-Assisted Therapy (The Hand Mentor Pro robotic device) + HEP versus HEP 8 weeks intervention |
Computer-based | I.G., n= 47 C.G., n= 45 |
PERSISTENT HEMIPARESIS (Motor) Action Research Arm Test (ARAT), Wolf Motor Function Test (WMFT), Fugl-Meyer Assessment |
Both groups demonstrated improvement across all upper extremity outcomes |
| Aparicio- López, et al. 2015, Spain [24] | To evaluate whether combination of computerized cognitive rehabilitation with right hemifield eye-patching (RHEP) in patients with left spatial neglect after stroke is better than computerized cognitive rehabilitation applied in isolation |
Computerized cognitive rehabilitation (Guttmann, NeuroPersonalTrainer® telerehabilitation platform) + RHEP vs Cognitive rehabilitation program 15 one-hour interventions |
Computer-based | Combination treatment (TC), N= 13 Single treatment (ST), N= 15 |
VISUO-SPATIAL NEGLECT (Higher cortical function) Bell Cancelation Test, Figure Copying of Ogden (FCO), Line Bisection, Baking Tray Task (BTT), Reading Task, Catherine Bergego Scale (CBS) |
Both the ST and the TC group showed improvements in neuropsychological examination protocol although there were no differences pre- and post-treatment on the functional scale in either group No statistically significant differences were observed in intergroup comparison |
|
| ||||||
| Chumbler et al, 2015, USA [25] | To determine the effect of a multifactorial stroke telerehabilitation (STeleR) in-home intervention on falls-related self-efficacy and patient satisfaction |
Functionality based exercises and adaptive strategies (STeleR) Intervention vs Usual care 3 months intervention |
Phone-based | STeleR Group: n=25 Usual Care Group: n=23 |
FALLS (Motor) Falls Self Efficacy Falls Efficacy Scale Stroke-Specific Patient Satisfaction with Care (SSPSC) scale, |
STeleR group showed significant improvements in their satisfaction with hospital care, P =.029) compared with control group. No improvements in fall-related self-efficacy. |
| Linder et al, 2015, USA [26] | To determine the effects of home-based robot-assisted rehabilitation coupled with a Home Exercise Program (HEP) compared with a HEP alone on depression and quality of life in people after stroke |
Robot-assisted therapy plus HEP versus HEP 8 weeks intervention |
Phone-based monitoring of intervention | Robot-assisted therapy and HEP, n= 51 HEP, n= 48 participants | DEPRESSION (Neuropsychiatric) Stroke Impact Scale (SIS), Center for Epidemiologic Studies Depression Scale (CES–D) |
Significant changes in all but one domain on the SIS and the Center for CES-D for both groups. |
|
| ||||||
| Woolf et al., 2016, UK [27] | To test the feasibility of a face to face versus remotely delivered word finding therapy for people with aphasia |
Word finding therapy (I) remote therapy delivered from a University lab (Mainstream video conferencing) (II) clinical site (Mainstream video conferencing)/ (III) face to face therapy/ (IV) an attention control condition. 4 weeks intervention |
Video-conferencing | I group: 5 patients II group: 5 patients III group: 5 patients IV group: 5 patients |
APHASIA (Higher cortical function) Recruitment and attrition rates, Participant observations and interviews, Treatment fidelity checking Tests of picture naming and naming in conversation |
Compliance and satisfaction with the intervention was good Treatment fidelity was high for both remote and face to face delivery (1251/1421 therapist behaviors were compliant with the protocol) Participants who received therapy improved on picture naming significantly more than controls (mean numerical gains: 20.2 (remote from University); 41 (remote from clinical site); 30.8 (face to face); 5.8 (attention control); P <.001) There were no significant differences between groups in the assessment of conversation. |
| Benvenuti et al., 2014, Italy [28] | To evaluate the safety, acceptance, adherence, and effectiveness of a community-based exercise program for upper limb paresis in patients with chronic stroke and the effects of telerehabilitation monitoring in kiosks distributed through the community |
Home Exercise Program (Carr and Shepherd “Motor Learning Program” + kiosk) versus Usual care 3 month intervention |
Tele-monitoring at kiosks | Treatment Group, n= 45 Usual Care Group, n=143 |
UPPER LIMB PARESIS (Motor) Upper extremity impairments Motricity Index, Nine-Hole Peg Test, Wolf Motor Function Test (WMFT), Nottingham Extended ADLs (NEADL), Barthel Index, Short Physical Performance Battery, Stroke Impact Scale (SIS) |
Patients in the experimental group demonstrated significant gains in arm function as measured by the WMFT (P <.0001), 9-Hole Peg Test (P <.009), Motricity Index (P <.0001), and NEADL (P <.002) The intervention received high satisfaction ratings and produced no adverse events Only 30% of the subjects attended kiosks regularly Outcomes for this group did not differ significantly from those who only practiced at home |
| Lin et al., 2014, Republic of China [29] | To evaluate the effect of a bidirectional and multiuser telerehabilitation system on balance and satisfaction in patients with chronic stroke living in long-term care facilities (LTCFs) |
Physical exercise Telerehabilitation Program (The 3D animation exercise videos + 3D interactive games) versus Conventional therapy 4 weeks intervention |
Computer-based | Telerehabilitation (Tele) group, n= 12 patients Conventional therapy group, n=12 patients |
DYSFUNCTION OF BALANCE AND FUNCTIONAL ACTIVITY (Motor) Berg Balance Scale (BBS), Barthel Index (BI), Telerehabilitation satisfaction |
Training programs conducted for both the Tele and Conventional groups showed significant effects within groups on the participant BBS as well as the total and self-care scores of BI No significant difference between groups could be demonstrated The satisfaction of participants between the Tele and the Conventional groups also did not show significant difference |
|
| ||||||
| Lloréns R et al, 2014, Spain [30] | To evaluate the clinical effectiveness of a Virtual reality -based telerehabilitation program in the balance recovery of hemiparetic individuals post-stroke in comparison to an inclinic program; to compare the subjective experiences; to contrast the costs |
Virtual reality based Telerehabilitation system at home versus Telerehabilitation system at clinic - twenty 45-minute training sessions 3× a week intervention |
Computer-based | I.G., n= 15 C.G., n= 16 |
RESIDUAL HEMIPARESIS (Motor) Berg Balance Scale (BBS), Balance and gait subscales of the Performance- Oriented Mobility Assessment, Brunel Balance Assessment (BBA), The System Usability Scale and the Intrinsic Motivation Inventory, Expenses in dollars for cost |
Significant improvement in both groups from the initial to the final assessment in the BBS (P=0.001), in the balance (P=0.006) and gait subscales (P=0.001) of the Tinetti Performance- Oriented Mobility Assessment, and in the BBA (P=0.002; and P=0.001). No significant differences between groups in any balance scale, nor in the feedback questionnaires. With regards to subjective experiences, both groups considered the VR system similarly usable and motivating. The in-clinic intervention resulted in more expenses than the telerehabilitation program (654.72 $ per person). |
| Smith et al., 2012, USA [31] | To develop and test the efficacy of a web-based intervention for alleviating depression in male stroke survivors and their spousal caregivers (CG) that blends both peer and professional support. |
Web-based intervention for alleviating depression Intervention condition at home (Professional Guide, Educational Videos, Online Chat Sessions, E- mail and Message Board, and Resource Room) versus Information-only control condition at home (minimal support with individualized access to relevant online information) 11 weeks intervention |
Videos and messaging | I.G., n=15 C.G., n=17 |
DEPRESSION (Neuropsychiatrie) 20-item CESD, PHQ-9, 9 items from the Mastery Scale, 10-item Self-Esteem Scale, 11 items from the MOS Social Support Survey, Credibility/Expectancy Questionnaire |
At posttest and one month later, CGs in the intervention group reported significantly lower depression than CGs in the control group with baseline depression controlled There was no significant effect on depression among SSs Although no significant treatment effects for either SSs or CGs were found on the secondary outcomes, post-treatment changes on some constructs were significantly correlated with change in depression |
|
| ||||||
| Redzuan et al., 2012, Malaysia [32] | To evaluate the effectiveness of an intervention using video to deliver therapy at home for patients with stroke |
Video-Based Physical Therapy Program (Digital videodisk containing therapy techniques) versus Weekly outpatient therapy sessions 3 month intervention |
Videos | I.G., n= 44 C.G., n= 46 |
HEMIPLEGIC STROKE (Motor) Modified Barthel Index (MBI) score, Incidence of poststroke complications Caregiver Strain Index |
No significant differences with regard to the number of patients with improved MBI score, complication rate, or Caregiver Strain Index score between the 2 groups Both groups had significant increases in the MBI score at 3 months (P <.001 for both groups) Regression analysis revealed that only stroke severity significantly influenced the MBI score (P <.001), complication rate (P <.01), and caregiver stress level (P <.05). |
|
| ||||||
| Chaiyawat, et al. 2012, Thailand [33] | To develop and examine the effectiveness of individual 6-month home rehabilitation program in ischemic stroke patients upon disability and quality of life at 2 years. |
Home-based physical exercise program Interventional care (Audiovisual materials) versus Usual care 6 month intervention |
Videos | I.G., n=30 C.G., n= 30 |
POST-STROKE DISABILITY (Motor) Barthel’s Index (BI), Modified Rankin Score (mRS) and Utility index (EQ-5D), Disability and quality of life |
At 2 years, the BI was significantly improved in the I.G. more than C.G. (97.2 ± 2.8 vs. 76.4 ± 9.4, P < 0.001) The good outcome, defined as BI 95–100, or mRS 0 or 1. For BI, there were 29 patients (96.7%) in I.G. vs 12 patients (42.9%) in C.G. (95% CI, 42.0, 85.0, P = 0.03) For mRS, there were 28 patients (93.3%) in intervention group vs 9 patients (32.1%) in usual care group (95% CI, 38.2, 87.0, P = 0.02) Number needed to treat for good outcome in mRS was 2.0 (95% CI: 1.0, 1.3) The mean (SD) of utility index in intervention group and control group were 0.9 ± 0.02 and 0.7 ± 0.04 respectively (P = 0.03) There was no significant interaction in baseline characteristics and treatment outcome. |
|
| ||||||
| Deng, et al. 2012, USA [34] | To explore the feasibility of using telerehabilitation to improve ankle dorsiflexion during the swing phase of gait in people with stroke and to compare complex versus simple movements of the ankle in promoting behavioral change and brain reorganization |
Complex/Simple movement training 20 days intervention |
Computer-based | Track Group: 8 patients Move Group: 8 patients |
PARETIC ANKLE (Motor) 10-m walk test and motion capture system, Ankle tracking during fMRI |
Dorsiflexion during gait was significantly larger in the track group compared with the move group (P=.017) For fMRI, although the volume, percent volume, and intensity of cortical activation failed to show significant changes, the frequency count of the number of participants showing an increase versus a decrease in these values from pretest to posttest measurements was significantly different between the 2 groups, with the track group decreasing and the move group increasing (P=.0014) |
| Chumbler, et al. 2012, USA [35] | To examine a telerehabilitation intervention that uses telehealth technology to improve outcomes of patients post-stroke after discharge home |
Physical exercise program Stroke telerehabilitation (STeleR) [home televisits, in-home messaging devices (IHMD) and telephone intervention] versus Usual care 3 months intervention |
Phone-based | STeleR Group: 25 participants Usual Care Group: 23 participants |
PHYSICAL DYSFUNCTION AND DISABILITY (Motor) Motor subscale of the Telephone Version of Functional Independence Measure (FONEFIM) Function scales of the Late-Life Function and Disability Instrument (LLFDI), 3 subscales of the LLFDI Function Component: upper extremity function, basic lower extremity function, and advanced lower extremity function |
FEONFEIM and LLFDI improved for the STeleR group and declined for the usual care group (not statistically significant) Secondary Outcomes: At 6 months, compared with the usual care group, the STeleR group showed statistically significant improvements in 4 of the 5 LLFDI disability component subscales (P 0.05), and approached significance in 1 of the 3 Function component subscales (P 0.06) |
|
| ||||||
| Piron, et al. 2009, Italy [36] | To compare the effects of a traditional rehabilitation therapy with an innovative rehabilitative Virtual Reality-based technique provided at distance by telemedicine | Telerehabilitation system (motor tasks and video consulting system) versus Conventional physiotherapy 4 week intervention |
Video-based | TeleRehab group: 18 patients Control group: 18 patients |
PARETIC UPPER LIMB (Motor) Fugl-Meyer Upper Extremity scale, ABILHAND scale, Ashworth scale |
Both rehabilitative therapies significantly improved all outcome scores after treatment, but only the Fugl-Meyer Upper Extremity scale showed differences in the comparison between groups. |
|
| ||||||
| Huijgen, et al. 2008, Netherlan ds [37] | To investigate the feasibility of the Home Care Activity Desk (HCAD) training system for clinical use by comparing its clinical outcomes with usual care |
Home Care Activity Desk training system-exercise versus Usual care 4 week intervention |
Not clear | I.G., n= 11 C.G., n= 5 |
ARM/HAND DYSFUNCTION (Motor) Action Research Arm Test and the Nine-Hole Peg Test, Visual Analogue Scale |
There were no significant differences between the two groups on the outcome measures (ARAT and NHPT); in both groups, patients maintained or even improved their arm/ hand function The HCAD training was found to be as feasible as usual care in terms of clinical outcomes, and both therapists and patients were satisfied with the HCAD intervention |
|
| ||||||
| Piron et al., 2008, Italy [38] | To assess how the presence or absence of the therapist affected patient satisfaction in the VR sessions as compared to patient satisfaction experienced in the Tele-VR sessions. |
Virtual reality (VR) therapy program (3D motion tracking system) at home versus hospital based therapy - 4 weeks intervention |
Video-based | Tele-VR group: 5 patients VR group: 5 patients |
ARM MOTOR IMPAIRMENT (Motor) Multidimensional, disease and treatment specific satisfaction questionnaire, Fugl-Meyer scale, Upper Extremity (Fugl-Meyer UE) score |
Tele-VR treated patients showed median values equal to or higher than the VR group patients in all 12 items investigated, except one In motor performance, the Tele-VR group improved significantly (P 0.05), while the VR group showed no significant change Patients assigned to the Tele-VR group were able to engage in therapy at home and the videoconferencing system ensured a good relationship between the patient and the physical therapist whose physical proximity was not required |
|
| ||||||
| Carey et al., 2007, USA [39] | To compare 2 telerehabilitation training strategies, repetitive tracking movements versus repetitive simple movements, to promote brain reorganization and recovery of hand function |
Computerized tracking training versus Movement training 2 week intervention |
Computer-based | Track group (TG): 10 patients Move group (MG):10 patients |
PARETIC HAND - FINGER EXTENSION DISABILITY (Motor) Box and Block test, Jebsen Taylor test, and Finger range of motion, along with a finger-tracking activation paradigm during fMRI. |
The TG showed significant improvement in all 4 behavioral tests; the MG improved in the Box and Block and Jebsen Taylor tests A consistent group pattern of brain reorganization was not evident The move group, after crossing over, did not show further significant improvements |
VR=Virtual Reality; OT=Occupational Therapy; ITT=Intention to treat analysis; I.G.=Intervention Group; C.G.= Control Group; HEP=Home Exercise Program.
Two studies assessed tele-rehabilitation intervention for recovery from higher cortical dysfunction after stroke namely aphasia27 and visuo-spacial neglect using the Guttmann NeuroPersonalTrainer® cognitive telerehabilitation program24. Both studies demonstrated feasibility of the interventions with improvements in higher cortical deficits assessed albeit not significantly different from the comparator groups. Finally, the two studies assessing the effects of tele-rehabilitation on resolution of depression among stroke survivors or care givers demonstrated improvement in both intervention and control population but non-significant differences between the two populations.26,31
DISCUSSION
In this systematic review of literature, we show that tele-rehabilitation for motor and higher cortical deficits as well as post-stroke depression appear to be as effective as in-person therapies if not better. Most studies identified in this review were of limited sample size with duration of interventions lasting two to three months which may be short given that most recovery after stroke peaks at month 6 to 12 months of ictus. Although the review by Chen et al in 2015 found no significant differences in abilities of activities of daily living and motor function between groups from pooled data, 4 out of the 5 studies that have since been published after their review has shown evidence of efficacy in favor of the Tele-rehabilitation group.18–22
The routine implementation of telemedicine for post-stroke rehabilitation could be especially important for regions around the world with a paucity of socioeconomic resources, including under-resourced areas of high-income countries, where neuro-rehab experts and facilities are virtually non-existent. In particular, the findings of this updated systematic review may have important implications for Low-and-Middle Income countries in sub-Saharan Africa where tele-neurology has been proposed as a promising avenue to explore40,41 due to the severe shortage of skilled personnel in the midst of an enormous burden of stroke which is associated with high mortality4,5,42, post-stroke depression43, vascular cognitive impairment44 and stigma45. Phone-based interventions have indeed demonstrated potential efficacy suggesting signals for blood pressure control among stroke survivors in Ghana46,47 as well as feasibility for post-stroke rehabilitation48–50. Future trials on the feasibility, efficacy and cost-effectiveness of tele-rehabilitation in SSA and indeed in other Low-and-Middle Income Countries where stroke burden is burgeoning51,52 are warranted. Larger, well-powered, longer-term studies are needed to establish the routine utility of tele-rehabilitation for stroke survivors globally.
Acknowledgments
Sources of funding: National Institute of Health- National Institute of Neurological Disorders & Stroke; R21 NS094033; National Institute of Health- Forgarty International Center R21 TW010479-01.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: All authors have none to declare.
References
- 1.Koh GCH, Saxena SK, Fong NP, Yong D, Ng TP. The effect of participation rate in supervised and unsupervised community rehabilitation on functional outcomes of post-stroke patients at one year: a cohort study with repeated measures. IV Singapore Public Health & Occupational Medicine Conference Programme and Abstracts; 2009. [Google Scholar]
- 2.Schwamm LH, Holloway RG, Amerenco P, Audebert HJ, Bakas T, Chumbler NR, et al. A review of the evidence for the use of telemedicine within stroke systems of care: a scientific statement from the American Heart Association/American Stroke Association. Stroke. 2009;40:2616–2634. doi: 10.1161/STROKEAHA.109.192360. [DOI] [PubMed] [Google Scholar]
- 3.Johannson T, Wild C. Telerehabilitation in stroke care- a systematic review. J Telemed Telecare. 2011;17:1–6. doi: 10.1258/jtt.2010.100105. [DOI] [PubMed] [Google Scholar]
- 4.Feigin VL, Roth GA, Naghavi M, Parmar P, Krishnamurthi R, Chugh S, et al. Global burden of stroke and risk factors in 188 countries, during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet Neurol. 2016;15(9):913–924. doi: 10.1016/S1474-4422(16)30073-4. [DOI] [PubMed] [Google Scholar]
- 5.Sarfo FS, Akassi J, Awuah D, Adamu S, Nkyi C, Owolabi M, et al. Trends in Stroke admission & mortality rates from 1983 to 2013 in Central Ghana. J Neurol Sci. 2015 Oct 15;357(1-2):240–5. doi: 10.1016/j.jns.2015.07.043. [DOI] [PubMed] [Google Scholar]
- 6.Chen J, Jin W, Zhang XX, Xu W, Liu XN, Ren CC. Telerehabilitation approaches for stroke patients: systematic review and meta-analysis of Randomized Controlled Trials. J Stroke Cerebrovasc Dis. 2015;24(12):2660–8. doi: 10.1016/j.jstrokecerebrovasdis.2015.09.014. [DOI] [PubMed] [Google Scholar]
- 7.Shah S, Vanclay F, Cooper B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol. 1989;42:703–709. doi: 10.1016/0895-4356(89)90065-6. [DOI] [PubMed] [Google Scholar]
- 8.Berg K, Wood-Dauphinee S, Williams JI. The balance scale: reliability assessment with elderly residents and patients with an acute stroke. Scand J Rehabil Med. 1995;27:27–36. [PubMed] [Google Scholar]
- 9.Kidd D, Stewart G, Baldry J, et al. The Functional Independence Measure: a comparative validity and reliability study. Disabil Rehabil. 1995;17:10–14. doi: 10.3109/09638289509166622. [DOI] [PubMed] [Google Scholar]
- 10.Fugl-Meyer AR, Jaasko L, Leyman I, et al. The post-stroke hemiplegic patient: A method for evaluation of physical performance. Scand J Rehabil Med. 1975;7:13–31. [PubMed] [Google Scholar]
- 11.Wade DT. Measuring arm impairment and disability after stroke. Int Disabil Stud. 1989;11:89–92. doi: 10.3109/03790798909166398. [DOI] [PubMed] [Google Scholar]
- 12.Lyle RC. A performance test for assessment of upper limb function in physical rehabilitation treatment and research. Int J Rehabil Res. 1981;4:483–492. doi: 10.1097/00004356-198112000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Bohannon RW, Smith MB. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther. 1987;67:206–207. doi: 10.1093/ptj/67.2.206. [DOI] [PubMed] [Google Scholar]
- 14.EuroQol Group. EuroQol- a new facility for the measurement of health-related quality of life. Health Policy (Amsterdam, Netherlands) 1990 Dec 01;16(3):199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 15.Haley SM, McHorney CA, Ware JJ. Evaluation of the MOS SF-36 physical functioning scale (PF-10): Unidimensionality and reproducibility of the Rasch item scale. J Clin Epidemiol. 1994;47:671–684. doi: 10.1016/0895-4356(94)90215-1. [DOI] [PubMed] [Google Scholar]
- 16.Robinson BC. Validation of a caregiver strain index. J Gerontol. 1983;38:344–348. doi: 10.1093/geronj/38.3.344. [DOI] [PubMed] [Google Scholar]
- 17.Larsen DL, Attkisson CC, Hargreaves WA, et al. Assessment of client/patient satisfaction: development of a general scale. Eval Program Plann. 1979;2:197–207. doi: 10.1016/0149-7189(79)90094-6. [DOI] [PubMed] [Google Scholar]
- 18.Chen J, Jin W, Dong WS, Jin Y, Qiao FL, Zhou YF, et al. Effects of Home-based Telesupervising Rehabilitation on Physical Function for Stroke Survivors with Hemiplegia A Randomized Controlled Trial. Am J Phys Med Rehabil. 2017;96:152–160. doi: 10.1097/PHM.0000000000000559. [DOI] [PubMed] [Google Scholar]
- 19.Pedreira da Fonseca E, Ribeiro da NM, Pinto EB. Therapeutic Effect of Virtual Reality on Post-Stroke Patients: Randomized Clinical Trial. J Stroke Cerebrovasc Dis. 2017;26(1):94–100. doi: 10.1016/j.jstrokecerebrovasdis.2016.08.035. [DOI] [PubMed] [Google Scholar]
- 20.Choi YH, Ku J, Lim H, Kim YH, Paik NJ. Mobile game-based virtual reality rehabilitation program for upper limb dysfunction after ischemic stroke. Restor Neurol Neurosci. 2016 May 2;34(3):455–63. doi: 10.3233/RNN-150626. [DOI] [PubMed] [Google Scholar]
- 21.Paul L, Wyke S, Brewster S, Sattar N, Gill JM, Alexander G, et al. Increasing physical activity in stroke survivors using STARFISH, an interactive mobile phone application: a pilot study. Top Stroke Rehabil. 2016 Jun;23(3):170–7. doi: 10.1080/10749357.2015.1122266. [DOI] [PubMed] [Google Scholar]
- 22.van den Berg M, Crottey M, Liu E, Killington M, Kwakkel G, van Wegen E, et al. Early Supported Discharge by Caregiver-Mediated Exercises and E-Health Support After Stroke: A Proof-Of-Concept Trial. Stroke. 2016;47(7):1885–1892. doi: 10.1161/STROKEAHA.116.013431. [DOI] [PubMed] [Google Scholar]
- 23.Wolf SL, Sahu K, Bay RC, Buchanan S, Reiss A, Linder S, et al. The HAAPI (Home Arm Assistance Progression Initiative) Trial: A Novel Robotics Delivery Approach in Stroke Rehabilitation. Neurorehabil Neural Repair. 2015 Nov-Dec;29(10):958–68. doi: 10.1177/1545968315575612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aparicio-López C, García-Molina A, García-Fernández J, López-Blázquez R, Enseñat-Cantallops A, Sánchez-Carrión R, et al. Combination treatment in the rehabilitation of visuo-spatial neglect. Psicothema. 2016 May;28(2):143–9. doi: 10.7334/psicothema2015.93. [DOI] [PubMed] [Google Scholar]
- 25.Chumble NR, Li X, Quigley P, Morey MC, Rose D, Griffiths P, et al. A randomized controlled trial on Stroke telerehabilitation: The effects on falls self-efficacy and satisfaction with care. J Telemed Telecare. 2015 Apr;21(3):139–143. doi: 10.1177/1357633X15571995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Linder SM, Rosenfeldt AB, Bay RC, Sahu K, Wolf SL, Alberts JL. Improving Quality of Life and Depression After Stroke Through Telerehabilitation. Am J Occup Ther. 2015 Mar-Apr;69(2):1–10. doi: 10.5014/ajot.2015.014498. 6902290020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Woolf C, Caute A, Haigh Z, Galliers J, Wilson S, Kessie A, et al. A comparison of remote therapy, face to face therapy and an attention control intervention for people with aphasia: a quasi-randomised controlled feasibility study. Clin Rehabil. 2016 Apr;30(4):359–73. doi: 10.1177/0269215515582074. [DOI] [PubMed] [Google Scholar]
- 28.Benvenuti F, Stuart M, Cappena V, Gabella S, Corsi S, Taviani A, et al. Community-Based Exercise for Upper Limb Paresis: A Controlled Trial With Telerehabilitation. Neurorehabilitation and Neural Repair. 2014;28(7):611–620. doi: 10.1177/1545968314521003. [DOI] [PubMed] [Google Scholar]
- 29.Lin KW, Chen CH, Chen YY, Huang WT, Lai JS, Yu SM, et al. Bidirectional and Multi-User Telerehabilitation System: Clinical Effect on Balance, Functional Activity, and Satisfaction in Patients with Chronic Stroke Living in Long-Term Care Facilities. Sensors (Basel) 2014 Jul;14(7):12451–12466. doi: 10.3390/s140712451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lloréns R, Noé E, Colomer C, Alcañiz M. Effectiveness, usability, and cost-benefit of a virtual reality-based telerehabilitation program for balance recovery after stroke: a randomized controlled trial. Archives of Physical Medicine and Rehabilitation. 2014 doi: 10.1016/j.apmr.2014.10.019. [DOI] [PubMed] [Google Scholar]
- 31.Smith GC, Egbert N, Dellman-Jenkins M, et al. Reducing depression in stroke survivors and their informal caregivers: a randomized clinical trial of a Web-based intervention. Rehabil Psychol. 2012;57:196–206. doi: 10.1037/a0029587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Redzuan NS, Engkasan JP, Mazlan M, et al. Effectiveness of a video-based therapy program at home after acute stroke: a randomized controlled trial. Arch Phys Med Rehabil. 2012;93:2177–2183. doi: 10.1016/j.apmr.2012.06.025. [DOI] [PubMed] [Google Scholar]
- 33.Chaiyawat P, Kulkantrakorn K. Effectiveness of home rehabilitation program for ischemic stroke upon disability and quality of life: a randomized controlled trial. Clin Neurol Neurosurg. 2012;114:866–870. doi: 10.1016/j.clineuro.2012.01.018. [DOI] [PubMed] [Google Scholar]
- 34.Deng H, Durfee WK, Nuckley DJ, Rheude BS, Severson AE, Skluzacek KM, et al. Complex Versus Simple Ankle Movement Training in Stroke Using Telerehabilitation: A Randomized Controlled Trial. Phys Ther. 2012 Feb;92(2):197–209. doi: 10.2522/ptj.20110018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chumbler NR, Quigley P, Li X, Morey M, Rose D, Sanford J, et al. Effects of Telerehabilitation on Physical Function and Disability for Stroke Patients a Randomized, Controlled Trial. Stroke. 2012;43:2168–2174. doi: 10.1161/STROKEAHA.111.646943. [DOI] [PubMed] [Google Scholar]
- 36.Piron L, Turolla A, Agostini M, et al. Exercises for paretic upper limb after stroke: a combined virtual-reality and telemedicine approach. J Rehabil Med. 2009;41:1016–102. doi: 10.2340/16501977-0459. [DOI] [PubMed] [Google Scholar]
- 37.Huijgen BC, Vollenbroek-Hutten MM, Zampolini M, et al. Feasibility of a home-based telerehabilitation system compared to usual care: arm/hand function in patients with stroke, traumatic brain injury and multiple sclerosis. J Telemed Telecare. 2008;14:249–56. doi: 10.1258/jtt.2008.080104. [DOI] [PubMed] [Google Scholar]
- 38.Piron L, Turolla A, Tonin P, Piccione F, Lain L, Dam M. Satisfaction with care in post-stroke patients undergoing a telerehabilitation programme at home. Journal of Telemedicine and Telecare. 2008;14:257–60. doi: 10.1258/jtt.2008.080304. [DOI] [PubMed] [Google Scholar]
- 39.Carey JR, Durfee WK, Bhatt E, Nagpal A, Weinstein SA, Anderson KM, Lewis SM. Comparison of finger tracking versus simple movement training via telerehabilitation to alter hand function and cortical reorganization after stroke. Neurorehabil Neural Repair. 2007;21:216–232. doi: 10.1177/1545968306292381. [DOI] [PubMed] [Google Scholar]
- 40.Sarfo FS, Adamu S, Awuah D, Ovbiagele B. Tele-neurology in Sub-Saharan Africa: a systematic review of the literature. J Neurol Sci. 2017;380:196–199. doi: 10.1016/j.jns.2017.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sarfo FS, Ovbiagele B. Mobile Health for Stroke: A promising concept for research and practice. mHealth. 2017;3:4. doi: 10.21037/mhealth.2017.02.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sarfo FS, Awuah DO, Nkyi C, Akassi J, Opare-Sem OK, Ovbiagele B. Recent patterns and predictors of neurological mortality among hospitalized patients in Central Ghana. J Neurol Sci. 2016;363:217–224. doi: 10.1016/j.jns.2016.02.041. [DOI] [PubMed] [Google Scholar]
- 43.Sarfo FS, Jenkins C, Singh A, Owolabi M, Ojagbemi A, Adusei N, Saulson R, Ovbiagele B. Post-stroke depression in Ghana: characteristics and correlates. J Neurol Sci. 2017;379:261–265. doi: 10.1016/j.jns.2017.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sarfo FS, Akassi J, Adamu S, Obese V, Ovbiagele B. Burden and predictors of vascular cognitive impairment among long-term Ghanaian stroke survivors. J Stroke Cerebrovasc. 2017;26(11):2553–2562. doi: 10.1016/j.jstrokecerebrovasdis.2017.05.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sarfo FS, Nichols M, Qanungo S, Teklehaimanot A, Singh A, Mensah N, et al. Stroke-related stigma among West Africans: Patterns and predictors. J Neurol Sci. 2017;375:270–274. doi: 10.1016/j.jns.2017.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sarfo FS, Treiber F, Gebregziabher M, Adamu S, Patel S, Nichols M, et al. PINGS (Phone-based Intervention under Nurse Guidance after Stroke): Interim results of a pilot randomized controlled trial. Stroke. 2018;49(1):236–239. doi: 10.1161/STROKEAHA.117.019591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sarfo FS, Treiber F, Jenkins C, Patel S, Gebregziabher, Singh A, et al. Phone-based Intervention under Nurse Guidance after stroke (PINGS): study protocol for a randomized controlled trial. Trials. 2016;17(1):436. doi: 10.1186/s13063-016-1557-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sarfo FS, Adusei N, Ampofo M, Kpeme FK, Ovbiagele B. Pilot trial of a tele-rehab intervention to improve outcomes after stroke in Ghana: a feasibility and user satisfaction study. J Neurol Sci. 2018;387:94–97. doi: 10.1016/j.jns.2018.01.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sarfo FS, Ovbiagele B. Response by Sarfo and Ovbiagele to letter regarding “potential role of tele-rehabilitation to address barriers to implementation of physical therapy among West African stroke survivors: A cross-sectional survey. J Neurol Sci. 2017;382:162–163. doi: 10.1016/j.jns.2017.09.038. [DOI] [PubMed] [Google Scholar]
- 50.Sarfo FS, Adamu S, Awuah D, Sarfo-Kantanka O, Ovbiagele B. Potential role of tele-rehabilitation to address barriers to implementation of physical therapy among West African stroke survivors: A cross-sectional survey. J Neurol Sci. 2017;381:203–208. doi: 10.1016/j.jns.2017.08.3265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Owolabi MO, Sarfo F, Akinyemi R, Gebregziabher M, Akpa O, Akpalu A, et al. Dominant modifiable risk factors for stroke in Ghana and Nigeria (SIREN): a case-control study. Lancet Glob Health. 2018;6(4):e436–e446. doi: 10.1016/S2214-109X(18)30002-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sarfo FS, Ovbiagele B, Gebregziabher M, Wahab K, Akinyemi R, Akpalu O, et al. Stroke among young west Africans: evidence from the SIREN (Stroke Investigative Research and Educational Network) Large Multisite case-control study. Stroke. 2018 Apr 4; doi: 10.1161/STROKEAHA.118.020783. pii: STROKEAHA.118.020783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sarfo FS, Akassi J, Kyem G, Adamu S, Awuah D, Kantanka OS, et al. Long-term outcomes of stroke in a Ghanaian Outpatient clinic. J Stroke Cerebrovasc Dis. 2018;27(4):1090–1099. doi: 10.1016/j.jstrokecerebrovasdis.2017.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]


