Abstract
This study focused on: 1) whether disparities in timely receipt of substance use services can be explained in part by the characteristics of the community in which the clients reside; and 2) whether the effect of community characteristics on timely receipt of services was similar across racial/ethnic groups. The sample was composed of adults receiving publicly-funded outpatient treatment in Washington State. Treatment data were linked to data from the U.S. Census. The outcome studied was “Initiation and Engagement” in treatment (IET), a measure noting timely receipt of services at the beginning of treatment. Community characteristics studied included community level economic disadvantage and concentration of American Indian, Latino, and Black residents in the community. Black and American Indian clients were less likely to initiate or engage in treatment compared to non-Latino white clients, and American Indian clients living in economically disadvantaged communities were at even greater risk of not initiating treatment. Community economic disadvantage and racial/ethnic make-up of the community were associated with treatment initiation, but not engagement, although they did not entirely explain the disparities found in IET.
Keywords: treatment, disparities, community, quality
Introduction
Increasing evidence suggests that racial/ethnic disparities in treatment services and outcomes for substance use disorders (SUDs) exist. Although SUDs appear to be equally prevalent among Whites, Latinos, and Blacks (prevalence rates of roughly 8%),1 this disorder exerts a disproportionate impact on the health of certain minority groups, including more severe alcohol problems among Latinos than among Whites,2 higher rates of injuries attributable to alcohol among American Indians, and disproportionately high rates of alcohol-attributable injury and mortality for Blacks and Latinos.3 The criminal justice consequences are also disproportionate. Blacks are more likely to be arrested for drug possession than are Whites although the rates of past month illicit drug use is similar.1,4 American Indians have the highest rates of SUDs (15%), and have among the highest rates of drug-induced mortality.5,6 Given the disproportionate negative impact of SUDs on racial/ethnic minority populations, it is critical that SUD treatment be equitable.
Unadjusted rates of treatment utilization might suggest that, among individuals in need of treatment, Blacks are more likely to access treatment.1 However after controlling for other individual factors related to criminal justice involvement and socioeconomic status, Black-White disparities in treatment access exist.7 Latinos are also less likely to access treatment than Whites when adjusting for criminal justice involvement and socioeconomic status.7
Even when treatment is accessed in publicly funded specialty settings, Black, Latino, and American Indian clients are less likely to initiate or engage in treatment. For example, a study examining a sample of individuals receiving publicly-funded treatment in Oklahoma identified disparities in outpatient treatment initiation for Black clients.8 Another study found that Black clients were less likely to engage in treatment than White clients in New York, and American Indian clients were less likely to engage in treatment in Washington state.9 Similar disparities have been found when examining racial/ethnic differences in treatment completion.10–12 These studies and others examining disparities in treatment have been focused on individual factors, such as types of substances used, socioeconomic characteristics, criminal justice involvement, and insurance status.7,13 Less is known about the influence of community characteristics on disparities in access to treatment services and the quality of those services. Therefore, this study sought to examine how the community characteristics of a client’s residence may be associated with quality indicators for the care of SUDs, and whether differences in community characteristics may account for racial/ethnic inequities.
Community characteristics and SUD treatment
Community characteristics are emerging as an important factor in the study of racial/ethnic disparities in the receipt of treatment services for SUDs. For example, counties with higher proportion of uninsured and Black residents are less likely to have SUD treatment facilities that accept Medicaid.14 Given that minorities are overrepresented in Medicaid, this is likely to limit their access to treatment. Community characteristics may also influence racial/ethnic disparities after treatment begins. Neighborhood disadvantage, broadly defined as an indicator of high rates of poverty and unemployment and low levels of education and financial assets of residents within a residential area, has been associated with the likelihood of clients completing treatment. In Los Angeles county, the level of disadvantage of the neighborhood where a treatment agency was located explained a significant portion of racial/ethnic differences in treatment completion.15 In a national sample, however, while racial/ethnic differences did exist by geographic area, these differences were explained in large part by racial/ethnic differences in the main substance used.12 This demonstrates the importance of considering both individual and community factors when examining disparities.
A growing body of evidence suggests the impact of living in a disadvantaged neighborhood is greater for racial/ethnic minorities than for White residents. Neighborhood disadvantage has been observed to be significantly related to heavy drinking by Blacks, but not by Whites.16 Also, Black men report greater alcohol-related consequences in health, employment, and other domains, compared with White men.17 Among adolescents, differences at the metropolitan area level substantially contributed to the lower rates of treatment completion in Hispanics compared to Whites.18 However, among Black and White adolescents, metropolitan variables did not contribute substantially to the Black-White treatment completion gap, suggesting that area level factors may impact groups differently.18
The conceptual framework for this study was informed by the Andersen Behavioral Model of Health Services Utilization,19 which hypothesizes that service utilization is influenced by both individual and contextual factors. Two community constructs that have been shown to be associated with SUD treatment access were the focus of this study: community indicators of economic disadvantage and racial/ethnic make-up. The current study expands this research to focus on disparities once clients have begun treatment.
The widely-used treatment performance measure initiation and engagement in treatment (IET) was used to assess how community characteristics may impact access to timely services as well as inequities in care. IET is a process measure indicating whether clients are receiving timely services in the early stages of SUD treatment. Endorsed by the National Quality Forum,20 the measure is included in the Healthcare Effectiveness Data and Information Set (HEDIS) as a performance measure for private health plans,21 and is used by Medicaid and the Veterans Health Administration22 to monitor care. The HEDIS IET measureis a two stage process. The first stage, treatment initiation, is the process of receiving treatment within 14 days of a diagnosis. This treatment can be received in either an inpatient alcohol or other drug admission, outpatient visit, intensive outpatient encounter, or partial hospitalization. Among clients who initiate treatment, engagement is the process of having two or more additional services within 30 days of the initiation service.21 IET is also used by several states in their publicly funded systems, modified to focus on episodes that begin with outpatient treatment.23,24 Among adults, IET in outpatient SUD treatment is associated with a reduction in substance use and criminal justice involvement, improved employment outcomes, and a reduction in subsequent admissions to detoxification services.22,25–27 Previous studies of state-funded treatment for adults suggested that Black and American Indian clients had a lower likelihood of receiving the services needed for meeting the IET criteria compared to White clients.8,9 Few studies have examined the association of IET with outcomes separately by race/ethnicity. However, a recent study found that although IET was generally associated with lower likelihood of an arrest after beginning treatment, this was not the case for Black, Latino, or American Indian clients in some states.9
To assess whether disparities exist, the Institute of Medicine definition was applied. Disparities are differences in the quality of health care that are not based on individual preferences, clinical need, or appropriateness of intervention.28 In this definition, differences that are attributable to the healthcare, legal, or regulatory system or to socioeconomic status (SES) are disparities and should be considered unfair.29 Using data from the State of Washington’s publicly-funded treatment services for individuals with SUDs, this research applied the IET measure to explore racial/ethnic disparities in timeliness of services and the influence of community characteristics. Washington State was chosen for several reasons: previous research documented disparities in IET, the State has a well-established treatment data collection system, and the Stata presented the opportunity to convert client addresses to census tracts allowing for the use of Census data. The goals of the present study were to:
Determine whether racial/ethnic disparities in IET exist
Examine whether characteristics of client’s community of residence were associated with IET and whether those community characteristics account for any of the disparities detected; and
Test whether community characteristics had a differential impact on IET based on client’s race/ethnicity.
Although other recent studies have examined racial/ethnic disparities in IET, to the best of our knowledge, this is the first study to examine the potential influence of community factors on the likelihood that clients will initiate or engage in treatment. This is also the first study to examine the extent to which differences in residential community characteristics account for disparities in IET, and whether the influence of community characteristics on IET varies by client’s race/ethnicity.
Methods
Data Sources
This study used client- and community-level data from Washington State. Data on client characteristics and treatment services (dates and types of SUD services received) were obtained from Washington’s Behavioral Health Administration (BHA). These e data on individuals receiving publicly funded substance use treatment is reported by SUD treatment providers. BHA converted client addresses to census tracts and removed all client identifiers prior to releasing the data for this study. Community-level data were derived from the 2010 U.S. Census and the American Community Survey (five-year averages from 2009–2013). These data were linked to the client treatment data using the census tract from the clients’ place of residence at admission. This study was approved by the Brandeis University and the Washington State Institutional Review Boards.
Sample
The sample consisted of adult clients ages 18+ who received publicly funded treatment, and who had a new outpatient (OP) treatment episode in Washington in 2012. For these analyses, a new OP treatment episode is defined as an OP admission with no other SUD services in the prior 60 days.24 The admission visit is considered the index visit. A total of 8,951 adult clients had an index visit during 2012. To ensure sufficient size for reliable analyses, the sample was restricted to clients who were part of the four largest racial/ethnic groups in the treatment sample: Whites, American Indians, Blacks, and Latinos. Thus, 594 (6.6%) clients from other racial/ethnic groups were excluded. If a client had more than one treatment episode during the year only their first episode was included. Due to missing information within the data, the analytic models were based on 8,239 clients.
Variables
Dependent variables
The outcomes of interest were modified versions of the HEDIS specifications21 for treatment initiation and engagement for clients with an OP treatment service as their index visit. Among such clients, OP treatment initiation is defined as having at least one SUD treatment service within 14 days after the index visit. Engagement is defined as receiving at least two additional SUD treatment services within 30 days of the initiation visit.
Independent variables
The main independent client-level variable is race/ethnicity as represented by a set of self-reported indicators. The BHA admission form asks about Latino origin and race/ethnicity. Race/ethnicity categories represented 16 subgroups and national origins and clients could respond positively to all that applied. Clients responding positively to any Latino category were categorized as Latino regardless of their race response. Among clients who reported not being Latino, those who reported being White and no other race/ethnicity were considered White and those who reported being Black and no other race/ethnicity were considered Black. Non-Latino clients who reported being both American Indian and White were considered American Indian since nationally nearly half of American Indians report multiple races, yet of multiracial groups, they are the least likely to consider themselves multiracial.30,31 Clients who were from other racial/ethnic groups and those who were multiracial (with the exception above) were excluded from the sample.
Community variables
Communities were defined at the census tract level. Census tracts are small and stable geographic units, and have been recommended as the geographic unit for monitoring disparities in health outcomes.32,33 Three variables were used as indicators of racial/ethnic composition, using standardized distributions: percent of census tract residents who are Latino, non-Latino American Indian, and non-Latino Black. Following from previous studies examining the relationship between community characteristics and substance use or treatment, additional census tract characteristics were also included, namely the percentage of: female-headed households with children, unemployed, living in poverty, households with annual income >$75,000 (recoded), and residents in management/professional occupations (recoded; for employed civilian population, ages 16+).15,16,34–36 Factor analysis was conducted to reduce these observed variables into latent variables or factors which are more easily interpretable. There was only one factor which accounted for a substantial proportion of the variation in the data (eigen value > 1), deemed “community economic disadvantage”. Correlations between the four community variables, and correlations between the community and individual variables were all less than r =0.5.
Co-variates
Individual-level covariates were chosen based on prior findings that they are associated with SUD treatment utilization or IET. These included gender, referral to treatment by the criminal justice system, and type of substance use during the past month, as a proxy for severity (for alcohol, cocaine, heroin, methamphetamines, opioids, and other substances). Socio-economic status (SES) variables were included in a sensitivity analyses: education, homelessness, and employment status. This information was collected by treatment staff at admission. The number of days between the index and initiation visit was calculated and then included in the engagement analyses, as reduced wait time is clinically important and has been shown to be a strong predictor of engagement.9,37
Analyses
Descriptive analyses were performed to examine variation by race/ethnicity with respect to clients’ sociodemographic and substance use characteristics at treatment admission and the study outcomes. Following these preliminary analyses, Heckman probit models38 adjusted for clustering by census tract were used to examine whether racial/ethnic disparities existed, and if so, whether clients’ community characteristics accounted for these disparities and whether the effect of community characteristics varied by race/ethnicity. This model was used because treatment engagement is conditional on treatment initiation, which introduces selection bias when considering individuals who have already initiated as compared with the broader population of people who begin a new outpatient treatment episode. The Huber/White Sandwich estimator in Stata’s Heckprob procedure corrects for clustering of people within census tracts and provides a more robust estimate of the standard error.
In these models, treatment initiation was the outcome for the first stage and treatment engagement was the outcome for the second. To avoid a specification issue, in a Heckman probit model some variables must be included in the first stage which are not subsequently included in the second stage. While all client-covariates were included in the first stage of the study models, in the second stage we considered removing variables related to past month drug use variables since they are less likely to have an influence on engagement than on initiation. We excluded variables assessing past month methamphetamine use and “other drug” use since they were the only variables not significant at p<.25 in preliminary logistic regressions of engagement run separately for each client-level variable.39 The variable “days to initiation” was only included in the second stage.
The analytic plan used results from three model specifications to examine the impact of race/ethnicity and community characteristics on IET. Model 1 focused on the examination of racial/ethnic disparities in the two outcomes, while controlling only for client-level covariates. In keeping with the IOM definition of disparities and measurement of this definition, the models do not control for socio-economic variables such as employment, education, and homeless status.28,29 Model 2 built off the initial model and additionally controlled for client’s community of residence characteristics. This model allowed examination of the effects of inclusion of community characteristics on Model 1 estimates of client race/ethnicity variables, indicating whether community characteristics accounted for the racial/ethnic disparities in either outcome. A final specification (Model 3) added interaction terms of individual’s race/ethnicity and community economic disadvantage to examine whether community characteristics had a differential impact on IET based on client’s race/ethnicity. The analysis only included interactions with community economic disadvantage to limit the number of interactions and reduce the likelihood of spurious findings.
Sensitivity analyses
As mentioned earlier, SES variables may reduce the apparent effects of race/ethnicity and it is recommended that they be excluded in the assessment of disparities.40 However, to determine whether SES variables at the client level (employment status, homeless status, and education level) may be in the causal pathway of disparities, we also re-ran all models adding these variables.
Results
Client Characteristics
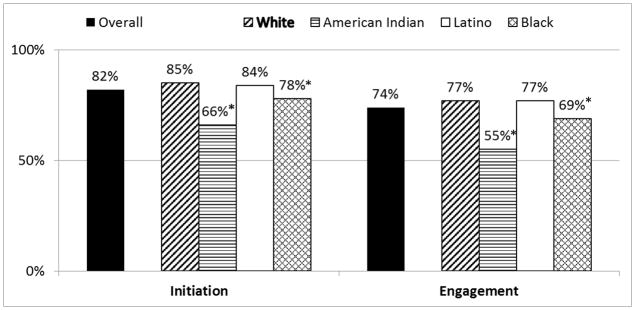
The majority of clients were White (67%), while American Indians (14%), Latinos (11%), and Blacks (8%) accounted for smaller proportions of the analytic sample. Descriptions of the client characteristics for the overall analytic sample and each of the four racial/ethnic groups are included in Table 1. Racial/ethnic groups differed significantly in almost all client characteristics at treatment admission. For example, women constituted a larger proportion of White and American Indian clients (42.5% and 43%, respectively) compared with Latino and Black clients (27.1% and 28.9%, respectively). American Indian (70.6%) and Latino (69%) clients were more likely to have been referred to treatment from the criminal justice system. Black clients were significantly more likely to report the use of alcohol (39.3%), marijuana (30.7%), and cocaine (13%) in the past month compared with their White, American Indian, or Latino counterparts. White clients were significantly more likely to report the use of methamphetamine (10.4%), opiates (13.4%), and other substances (3.4%) in the past month compared with their Black, American Indian, and Latino counterparts. The overall unadjusted initiation and engagement rates were 82% and 74%, respectively, and they too differed by race/ethnicity. American Indian clients had the lowest initiation and engagement rates (66% and 55%, respectively), while White clients had the highest rates (85% and 77%, respectively; see Figure 1).
Table 1.
Client Characteristics at Treatment Admission
| Entire Sample(N=8,239) | Whites (W) (N=5,516) | American Indian/Alask a Native (AI/AN) (N =1,158) | Latino s (L) (N =867) | Black s (B) (N=698) | Racial/Ethnic Group Differencesb | |
|---|---|---|---|---|---|---|
|
| ||||||
| % | % | % | % | % | ||
| Client demographics | ||||||
| Female | 39.8 | 42.5 | 43.0 | 27.1 | 28.9 | W, AI/AN >B, L |
| Socioeconomic status | ||||||
| Education | ||||||
| Less than H.S. | 29.1 | 24.8 | 33.3 | 50.8 | 29.9 | L > B, AI/AN > W |
| H.S. Grad | 55.8 | 58.0 | 57.6 | 39.3 | 56.0 | W, AI/AN, B > L |
| More than H.S. | 8.5 | 9.6 | 5.5 | 5.4 | 7.7 | W > AI/AN, L |
| Vocational training | 6.6 | 7.6 | 3.6 | 4.5 | 6.3 | W, B > |
| Homeless/at risk of | 14.5 | 15.3 | 8.0 | 8.8 | 26.4 | AI/AN; W > L B > W > L, |
| Unemployed | 78.2 | 81.1 | 71.7 | 62.2 | 85.7 | AI/AN B > W >AI/AN > L |
| Treatment referral and Substance use | ||||||
| Referral Source | ||||||
| Criminal Justice | 58.3 | 54.3 | 70.6 | 69.0 | 56.5 | AI/AN, L > W,B |
| Past month usea | ||||||
| Alcohol | 29.8 | 28.5 | 30.2 | 30.1 | 39.3 | B > W,AI/AN, L |
| Marijuana | 21.9 | 21.6 | 20.2 | 18.9 | 30.7 | B >W, AI/AN,L |
| Cocaine | 3.3 | 2.5 | 2.1 | 2.2 | 13.0 | B > W,AI/AN, L |
| Methamphetamines | 8.4 | 10.4 | 4.8 | 5.5 | 2.0 | W > L, AI/AN > B |
| Opiates | 12.1 | 13.4 | 13.4 | 6.7 | 6.3 | W, AI/AN > L,B |
| Other substance | 2.9 | 3.4 | 1.6 | 2.1 | 2.4 | W > AI/AN |
NOTES:
Substance was listed as a primary, secondary, or tertiary drug and frequency of use was one or more times in the past month or during the month of highest use in the last year.
Differences at the p<.05 level using a Bonferroni correction for multiple comparisons.
Figure 1.
Unadjusted Treatment Initiation and Engagement by Race/Ethnicity
*Significantly lower initiation/engagement rates than Whites for the overall p < .05 level, using a Bonferroni correction for multiple comparisons
Community Characteristics
Clients in our sample resided in a total of 1,284 census tracts. The community variable % of residents who are American Indians ranged from 0.4% to 87.1% (Mean=6.8, s.d. = 13.1). The community variable % of residents who are Latinos ranged from 1% to 88% (Mean = 13.1, s.d. = 14.6), and % of residents who are Black ranged from 0% to 39.3% (mean = 3.9, s.d.= 5.8). Community economic disadvantage is a standardized variable, and thus we describe it by rurality. The mean for this variable was 0.81 (s.d. = 0.54) in rural areas (N = 969), and 0.35 (s.d. = 0.84) in non-rural areas (N = 7,270).
Treatment Initiation
Table 2 shows the results of the three Heckman probit model specifications predicting treatment initiation. After adjustment for other client-level characteristics, Black (Coeff = −0.247, 95% CI: −0.362, 0.132, p< 0.01) and American Indian clients (Coeff = −0.646, 95% CI: −0.805, −0.487, p< 0.01) had a significantly lower likelihood of treatment initiation than White clients (Model 1). After controlling for community-level predictors, the disparities in treatment initiation among Black (Coeff = −0.137, 95% CI: −0.254, −0.019, p < 0.05) and American Indian clients (Coeff: −0.366, 95% CI: −0.497, −0.234, p< 0.01) were reduced particularly for American Indians, but remains significant (Model 2).
Table 2.
Results of two-stage probit regression examining predictors of treatment initiation (first stage)
| Model 1. | Model 2. | Model 3. | ||||
|---|---|---|---|---|---|---|
| Variable | Individual Characteristics | Individual + Community Characteristics | Individual +Community + Interactions of Race/Ethnicity X Community | |||
| Coeff. | (95% CI) | Coeff. | (95% CI) | Coeff. | (95% CI) | |
| Stage 1. Predicting Treatment Initiation | ||||||
|
| ||||||
| Individual Characteristics | ||||||
| Race/Ethnicity (ref:White) | ||||||
| American Indian | −0.646** | (−0.805, −0.487) | −0.366** | (−0.497, −0.234) | −0.241** | (−0.382, −0.099) |
| Latino | −0.064 | (−0.188, 0.060) | 0.068 | (−0.060, 0.197) | −0.001 | (−0.132, 0.133) |
| Black | −0.247** | (−0.362, −0.132) | −0.137* | (−0.254, −0.019) | −0.154* | (−0.281, −0.028) |
| Female Gender | −0.046 | (−0.115, 0.023) | −0.064 | (−0.133, 0.005) | −0.064 | (−0.133, 0.005) |
| Referral from CJ | 0.058 | (−0.013, 0.129) | 0.085* | (0.016, 0.154) | 0.090* | (0.022, 0.158) |
| Past month use | ||||||
| Alcohol | −0.005 | (−0.074, 0.064) | 0.003 | (−0.067, 0.073) | 0.004 | (−0.066, 0.075) |
| Marijuana | −0.013 | (−0.093, 0.067) | −0.029 | (−0.111, 0.052) | −0.031 | (−0.112, 0.050) |
| Cocaine | −0.062 | (−0.229, 0.105) | −0.003 | (−0.171, 0.164) | 0.008 | (−0.160, 0.175) |
| Opioids | 0.014 | (−0.090, 0.118) | −0.002 | (−0.11, 0.10) | −0.012 | (−0.114, 0.090) |
| Methamphetamines | 0.077 | (−0.050, 0.204) | 0.027 | (−0.111, 0.164) | 0.030 | (−0.105, 0.165) |
| Other drugs | −0.189* | (−0.363, −0.016) | −0.190* | (−0.375, −0.006) | −0.178 | (−0.361, 0.006) |
| Community Variables | ||||||
| Economic Disadvantage | --- | --- | 0.168** | (0.113, 0.222) | 0.174** | (0.115, 0.233) |
| % American Indian | --- | --- | −0.012** | (−0.016, −0.009) | −0.011** | (−0.014, −0.007) |
| % Black | --- | --- | −0.014** | (−0.021, −0.008) | −0.014** | (−0.021, −0.008) |
| % Latino | --- | --- | −0.012** | (−0.015, −0.008) | −0.011** | (−0.015, −0.008) |
| Interactions of Community Characteristics and Client’s Race/ethnicity | ||||||
| Economic Disadvantage X American Indian | --- | --- | --- | --- | −0.255** | (−0.378, −0.131) |
| Economic Disadvantage X Black | --- | --- | --- | --- | 0.055 | (−0.071, 0.181) |
| Economic Disadvantage X Latino | --- | --- | --- | --- | 0.103 | (−0.025, 0.231) |
p< .05;
p< .01
Note: Using standardized distributions for community variables
Clients living in economically disadvantaged communities were more likely to initiate treatment (Coeff: 0.168, 95% CI: 0.113, 0.222, p< 0.01), controlling for concentration of Black, Latino, and American Indian residents in the community and individual covariates. However, clients living in communities with a higher concentration of American Indian residents (Coeff: −0.012, 95% CI: −0.016, −0.009, p< 0.01), communities with a higher concentration of Black residents (Coeff: −0.014, 95% CI: −0.021, −0.008, p< 0.01), and/or communities with higher concentration of Latino residents (Coeff: −0.012, 95% CI: −0.015, −0.008 p< 0.01) had a lower likelihood of initiating treatment (Model 2). Model 3 shows the examination of whether the effects of economic disadvantage differed based on client’s race/ethnicity by including interactions. American Indian clients living in economically disadvantaged communities were at a significantly higher risk of not initiating treatment (Coeff: −0.255, 95% CI: −0.378, −0.131, p< 0.01) compared to White clients in those communities. The interactions between Black and Latino race/ethnicity and community economic disadvantage were not significant.
Treatment engagement
Table 3 presents the results predicting treatment engagement, the outcome of the second stage of Heckman probit models. Compared to White clients, Black (Coeff: −0.237, 95% CI: −0.395, −0.078, p< 0.01) and American Indian clients (Coeff: −0.505, 95% CI: −0.805, −0.205, p< 0.01) were significantly less likely to engage, when controlling for individual covariates only (Model 1). After controlling for the community characteristics of where clients live (Model 2), the disparities in treatment engagement between American Indian (Coeff: −0.213, 95% CI: −0.418, −0.008, p< 0.05) and White clients remained significant. The disparity between Black and White clients in treatment engagement was no longer statistically significant, though this change is unlikely to be significant since there is overlap in the 95% Confidence Intervals between the two models. Additionally, none of the community level predictors were statistically significant predictors of treatment engagement (Model 2) and the effects of economic disadvantage on treatment engagement did not vary based on client’s race/ethnicity (Model 3).
Table 3.
Results of two-stage probit regression examining predictors of treatment engagement (second stage)
| Model 1. | Model 2. | Model 3. | ||||
|---|---|---|---|---|---|---|
| Variable | Individual Characteristics | Individual + Community Characteristics | Individual + Community + Interactions of Race/Ethnicity X Community | |||
| Coeff. | (95% CI) | Coeff. | (95% CI) | Coeff. | (95% CI) | |
| Stage 2: Predicting Treatment Engagement | ||||||
|
| ||||||
| Individual Characteristics | ||||||
| Race/Ethnicity (ref:White) | ||||||
| American Indian | −0.505** | (−0.805, −0.205) | −0.213* | (−0.418, −0.008) | −0.190* | (−0.376, −0.004) |
| Latino | 0.009 | (−0.141, 0.159) | 0.079 | (−0.072, 0.231) | 0.011 | (−0.147, 0.170) |
| Black | −0.237** | (−0.395, −0.078) | −0.102 | (−0.269, 0.064) | −0.137 | (−0.313, 0.039) |
| Days between index and initiation | −0.057** | (−0.082, −0.032) | −0.063** | (−0.075, −0.050) | −0.062** | (−0.075, −0.050) |
| Female Gender | 0.005 | (−0.098, 0.088) | 0.002 | (−0.098, 0.103) | 0.003 | (−0.097, 0.102) |
| Referral from CJ | 0.203** | (0.101, 0.306) | 0.216** | (0.109, 0.324) | 0.215** | (0.110, 0.320) |
| Use in last month | ||||||
| Alcohol | −0.057 | (−0.147, 0.033) | −0.058 | (−0.155, 0.039) | −0.056 | (−0.153, 0.041) |
| Marijuana | −0.076 | (−0.181, 0.029) | −0.088 | (−0.194, 0.019) | −0.088 | (−0.195, 0.018) |
| Cocaine | −0.114 | (−0.355, 0.126) | −0.072 | (−0.327, 0.182) | −0.059 | (−0.313, 0.194) |
| Opioids | −0.157* | (−0.291, −0.023) | −0.191** | (−0.316, −0.066) | −0.194** | (−0.318, −0.070) |
| Community Variables | ||||||
| Economic Disadvantage | --- | --- | 0.053 | (−0.051, 0.156) | 0.031 | (−0.075, 0.137) |
| % American Indian | --- | --- | −0.005 | (−0.012, 0.002) | −0.005 | (−0.010, 0.001) |
| % Black | --- | --- | −0.009 | (−0.019, 0.001) | −0.009 | (−0.018, 0.001) |
| % Latino | --- | --- | −0.004 | (−0.011, 0.002) | −0.005 | (−0.011, 0.001) |
| Interactions of Community Characteristics and Client’s Race/ethnicity | ||||||
| Economic Disadvantage X American Indian | --- | --- | --- | --- | −0.035 | (−0.241, 0.171) |
| Economic Disadvantage X Black | --- | --- | --- | --- | 0.109 | (−0.072, 0.291) |
| Economic Disadvantage X Latino | --- | --- | --- | --- | 0.147 | (−0.022, 0.316) |
= p< .05;
= p< .01;
Note: Using standardized distributions for community variables
Sensitivity analyses
The addition of the SES variables (employment, education, and homeless status) did not change the disparities observed in initiation or engagement (results not shown). Education was not associated with initiation or engagement, and employment was negatively associated with treatment initiation only in Model 1. Homeless status was negatively associated with both treatment initiation and treatment engagement in all three models (p < .05).
DISCUSSION
Blacks, Latinos, and American Indians experience consequences for their substance use and substance use disorders disproportionately compared with those suffered by their White counterparts.2–6 Yet, they are less likely to enter treatment than Whites when socioeconomic factors and criminal justice referrals are taken into account.7 To avoid further inequities, it is essential to minimize disparities once clients enter treatment, however this study indicates that racial/ethnic disparities in SUD treatment exist. Specifically, Black and American Indian clients in Washington State are less likely to receive timely services than White clients at the beginning of a treatment episode, as measured by initiation and engagement (IET). These inequities persist after adjusting both for individual characteristics and for community economic disadvantage and racial/ethnic composition of the community in which clients reside.
The disparities found in IET are consistent with prior research, including studies using older data from Washington State showing disparities in treatment initiation among American Indians.9 Community characteristics did not fully account for the disparities we found in IET, but they appear to be a contributing factor particularly with respect to treatment initiation among American Indians. For this group, there was a substantial reduction in the estimate when community characteristics were added to the models, and confidence intervals overlapped only minimally. Findings from prior research show that community characteristics account in part for disparities in treatment completion. For example, neighborhood disadvantage explained about a third of the Black-White disparity in treatment completion in Los Angeles county facilities15 and racial/ethnic composition has been shown to be associated with lower treatment completion among minority adolescents.18 This study contributes to the literature by using a standardized performance measure and an earlier phase of treatment.
The large disparities in IET observed between American Indian and White clients need further exploration. Our findings suggest that variables at the area-level such as economic conditions of the community may be negatively impacting retention in the early stages of treatment for American Indians. Disparities among this group may also be due to geographic location. Almost 30% of American Indians in our sample lived in rural areas, whereas the proportion of clients living in rural areas for other racial/ethnic groups in our sample ranged from 2%–17% (data now shown). Rural areas in general tend to have lower access to treatment, and lower access and higher distances to treatment may impact whether American Indian clients can return for services easily. Additionally, these disparities may be attributable to limited resources at the client, provider, and system level. Providers have identified several barriers to delivering quality services to this population. These include challenges related to delivering clinical services (e.g., client trauma history and mistrust of service system, socioeconomic barriers faced by clients), limitations of the infrastructure of treatment settings (e.g., provider turnover, fatigue and burnout, lack of resources in the treatment setting), and the shortfalls of the greater service/treatment system (e.g., lack of sufficient aftercare resources, the employment of treatments inappropriate to the population).41 Providers also express concern that many of the current evidence-based practices conflict with American Indian traditions and healing practices.42
Furthermore, financial constraints at the system and individual levels are likely to contribute to disparities in IET. Programs serving American Indian and Alaskan Native clients report increased use of evidence-based practices when directly receiving funding from the Indian Health Service42, but while nearly all of the programs serving this population report being tribally owned,43 the Indian Health Services spends significantly less per capita for treatment services than the state does for the general population.44 American Indian clients themselves report financial and logistical barriers to attending treatment (e.g., cost of services, transportation, and child care).45 More research is needed to better understand how best to support treatment facilities that serve American Indians, and to develop treatments that are culturally appropriate. Lowering the financial barriers related to delivering and receiving treatment is also vital for reducing disparities experienced by this population.
Apart from the client’s own race/ethnicity, the characteristics of the communities where clients reside also influenced whether services were provided in a timely manner. Clients residing in areas having higher proportions of Latino, Black, and American Indian residents were found to be less likely to initiate treatment. Racial composition of a community is a proxy for segregation, which is generally associated with poorer health outcomes and disparities in health care.46,47 Areas with higher concentrations of racial/ethnic minorities may be home to lower-performing treatment programs with lower overall IET rates. Additionally, communities of color tend to have a higher density of outlets for the sale of liquor, wine and beer.48,49 Living near an alcohol outlet is associated with lower likelihood of continuing to outpatient treatment after being discharged from a residential program.50 Higher density of alcohol outlets in minority communities may also contribute to lower IET rates for some minority groups.
Minority clients may also be traveling farther or longer for treatment. Since travel time is negatively associated with continuity of treatment,34 it would be useful to determine whether Black and American Indian clients travelled farther or longer to attend treatment. Travel time is difficult to measure in Washington State, where there are large urban centers, yet much of the state is rural. Additionally, research in general medical care indicates that even when Black patients lived closer to higher-quality treatment services, they were more likely to receive treatment at a low-quality setting, suggesting that travel time may interact with other factors such as mistrust of certain providers. 51 Access to transportation is likely to play a role in early treatment participation, and future research should focus on the effects of travel time on IET. Future studies should also examine whether access to treatment services is correlated with such factors as access to public transportation or individual car ownership, and how travel time may differ by race/ethnicity.
Many of the census tracts in Washington with higher concentrations of American Indian residents and Latino residents are in rural areas. Clients residing there may lack easy access to transportation making visits to the treatment facility more difficult. Additionally, communities with a higher proportion of minority residents may have fewer treatment agencies, or the agencies found in such communities may have more limited treatment capacity and resources. If treatment facilities with lower capacity and funding are more likely to be found in census tracts that are disproportionately minority or poor, that fact may impact initiation and engagement, decreasing the likelihood of continuing treatment.34 Future studies should explore these connections.
Contrary to what one might expect, clients residing in “economically disadvantaged” areas were more likely to initiate treatment. This finding is inconsistent with prior research where clients living in communities with other indicators of economic disadvantage (e.g., percent vacant housing) were less likely to have continuity of care from residential to outpatient treatment.50 Why this is so is unclear. As already noted, clients residing in communities which are not predominantly White often must travel long distances to access treatment,52,53 and this can negatively affect treatment continuity.34 Additionally, the sample in the current study consists of clients who receive publicly-funded treatment, and thus are likely to have low or no incomes. It may be that clients with low incomes living in economically disadvantaged areas with lower economic assets are eligible for services from treatment facilities that are good at addressing the needs of the people in that community. On the other hand, clients with low incomes who live in more affluent areas may be obtaining services in facilities less responsive to their needs, or they may need to travel further to find facilities with state contracts. Future studies should undertake geospatial analyses of treatment facilities and their IET rates.
The positive effect of living in an economically disadvantaged community on timely access to services was not the same across all groups. In fact, American Indian clients living in economically disadvantaged communities were at the highest risk of not receiving timely services within the first two weeks of their treatment admission. We are not aware of studies that have examined the interaction between client’s race/ethnicity and community disadvantage on quality or timeliness of SUD services. Other research shows that the effects of community characteristics on use of health services and health outcomes including alcohol use are not the same across all racial/ethnic groups.16,51,54,55 Particular attention should be paid to addressing the needs of American Indian clients living in poorer communities and examine whether lower likelihood of engagement differs if the community is also predominantly American Indian.
Although community characteristics were associated with the likelihood of treatment initiation, they were not associated with likelihood of engagement among those who initiated treatment. This suggests that place of residence plays a stronger role in the very early stages of treatment, and less so once a client has returned for treatment at least once.
The current study is the first study we are aware of that includes residential community characteristics in the examination of disparities in IET. There are several limitations to this study. First, the study sample included only clients receiving publicly-funded SUD treatment. Although this may limit the generalizability of findings to the public sector, SUD treatment has historically received two thirds of its funding from the public sector and this percentage is expected to grow.56,57 Second, because we used data from only one state, results may not be generalizable to other states. Disparities in SUD treatment vary by state,9 and as policies and funding related to SUDs vary widely by state, it is important that these issues be examined at the state or local level. Furthermore, the racial/ethnic categories used were broad, and treatment quality could differ by subgroups (e.g., Latino national origin, or particular American Indian tribe). Studies in states where minorities make up a larger proportion of the population may permit such comparisons. Additionally, we lacked data on whether clients suffered from a co-occurring mental health disorder, although co-occurring disorders are common among those with SUDs.58 Such clients may have more difficulty initiating or engaging in treatment. Rates of co-occurring disorders vary by race/ethnicity59 and this may have influenced the disparities we found. Finally, IET only measures one aspect of the treatment process and does not assess suitability of the treatment approaches or the quality of encounters.
Implications for Behavioral Health
Inequities in IET must be addressed in view of the evidence that IET is associated with better treatment outcomes, including reduced substance use, lower rates of involvement in the criminal justice system and higher rates employment.22,25,26 Thus eliminating inequality in IET may also help improve these outcomes. State substance use treatment agencies can play a critical role by monitoring performance measures such as IET by race/ethnicity to assess inequities in treatment. The findings of this study suggest that state agencies might also wish to examine differences in receipt of services at the community level. Because clients may be attending treatment outside of the community in which they reside, state treatment agencies may want to examine where clients live and where they attend treatment, the accessibility of treatment facilities, and where facilities with high initiation and engagement rates are located relative to communities with higher concentrations of racial/ethnic minorities. Treatment providers themselves should also monitor quality indicators by race/ethnicity to determine whether rates for IET and other performance rates are similar across racial/ethnic groups within their treatment facility.
The fact that disparities in treatment engagement and initiation remained after adjusting for community socioeconomic disadvantage and racial/ethnic composition suggests that other factors must account for these disparities. Future research examining inequities in SUD treatment should explore other possible factors, such as facility or clinician characteristics, differences in strength of therapeutic alliance, and additional barriers experienced by certain groups in returning to treatment. This study focused on inequities in care among clients who have already begun treatment. Nationally, Black, Latino, and American Indians who have a need for treatment are less likely to access treatment in the first place.7 Recent studies have shown that where you live impacts access to SUD treatment.14,60 Examining disparities in quality indicators which also consider barriers to treatment access may show even greater inequities.
Conclusion
In view of the known disproportionate negative consequences of SUDs experienced by racial/ethnic minorities, it is critical that timely SUD treatment be available to all groups. This study shows that racial/ethnic inequities in SUD treatment exist and that economic and racial/ethnic makeup of the geographic community of where clients reside do not explain these disparities. Future studies should examine the mechanisms by which this occurs, and state administrators, researchers, treatment providers, and consumers should join forces to design interventions to address them.
Acknowledgments
This research was supported by the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health under award number R03AA023390. The content is the sole responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or of the participating state.The authors would like to thank Can Du from the Behavioral Health Administration in the Washington State Department of Social and Health Services for her comments on an earlier version of the manuscript.
Footnotes
Conflict of Interest
The authors have no conflict of interests to declare.
References
- 1.SAMHSA. 2015 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2016. [Google Scholar]
- 2.Schmidt LA, Ye Y, Greenfield TK, et al. Ethnic disparities in clinical severity and services for alcohol problems: results from the National Alcohol Survey. Alcoholism, clinical and experimental research. 2007;31(1):48–56. doi: 10.1111/j.1530-0277.2006.00263.x. [DOI] [PubMed] [Google Scholar]
- 3.Keyes KM, Liu XC, Cerda M. The role of race/ethnicity in alcohol-attributable injury in the United States. Epidemiologic Reviews. 2012;34:89–102. doi: 10.1093/epirev/mxr018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Snyder HN, Mulako-Wangota J. Bureau of Justice Statistics. Arrests by Race and Age in the U.S 2012. [December 30, 2015];Generated using the Arrest Data Analysis Tool. 2015 at www.bjs.gov.
- 5.Calcaterra S, Glanz J, Binswanger IA. National trends in pharmaceutical opioid related overdose deaths compared to other substance related overdose deaths: 1999–2009. Drug and alcohol dependence. 2013;131(3):263–270. doi: 10.1016/j.drugalcdep.2012.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mack K. Drug-induced deaths - United States, 1999–2010. Morbidity and Mortality Weekly Report. 2013 Nov 22;62(Suppl 3):161–163. [PubMed] [Google Scholar]
- 7.Cook BL, Alegría M. Racial-ethnic disparities in substance abuse treatment: The role of criminal history and socioeconomic status. Washington, D C. 2011;62(11):1273–1281. doi: 10.1176/appi.ps.62.11.1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Acevedo A, Garnick DW, Lee MT, et al. Racial and ethnic differences in substance abuse treatment initiation and engagement. Journal of ethnicity in substance abuse. 2012;11(1):1–21. doi: 10.1080/15332640.2012.652516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Acevedo A, Garnick DW, Dunigan R, et al. Performance measures and racial/ethnic disparities in the treatment of substance use disorders. Journal on the Studies of Alcohol & Drugs. 2015;76(1):57–67. [PMC free article] [PubMed] [Google Scholar]
- 10.Saloner B, Le Cook B. Blacks and Hispanics are less likely than whites to complete addiction treatment, largely due to socioeconomic factors. Health Affairs. 2013;32(1):135–145. doi: 10.1377/hlthaff.2011.0983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guerrero EG, Marsh JC, Duan L, et al. Disparities in completion of substance abuse treatment between and within racial and ethnic groups. Health services research. 2013;48(4):1450–1467. doi: 10.1111/1475-6773.12031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mennis J, Stahler GJ. Racial and Ethnic Disparities in Outpatient Substance Use Disorder Treatment Episode Completion for Different Substances. Journal of substance abuse treatment. 2016;63:25–33. doi: 10.1016/j.jsat.2015.12.007. [DOI] [PubMed] [Google Scholar]
- 13.Lundgren LM, Amaro H, Ben-Ami L. Factors Associated with Drug Treatment Entry Patterns Among Hispanic Women Injection Drug Users Seeking Treatment. Journal of Social Work Practice in the Addictions. 2005;5(1–2):157–174. [Google Scholar]
- 14.Cummings JR, Wen H, Ko M, et al. Race/ethnicity and geographic access to Medicaid substance use disorder treatment facilities in the United States. JAMA Psychiatry. 2014;71(2):190–196. doi: 10.1001/jamapsychiatry.2013.3575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jacobson JO, Robinson P, Bluthenthal RN. A multilevel decomposition approach to estimate the role of program location and neighborhood disadvantage in racial disparities in alcohol treatment completion 1982. 2007;64(2):462–476. doi: 10.1016/j.socscimed.2006.08.032. [DOI] [PubMed] [Google Scholar]
- 16.Karriker-Jaffe KJ, Zemore SE, Mulia N, et al. Neighborhood disadvantage and adult alcohol outcomes: differential risk by race and gender. Journal on the Studies of Alcohol and Drugs. 2012;73(6):865–873. doi: 10.15288/jsad.2012.73.865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jones-Webb R, Snowden L, Herd D, et al. Alcohol-related problems among black, Hispanic and white men: the contribution of neighborhood poverty. Journal of studies on alcohol. 1997;58(5):539–545. doi: 10.15288/jsa.1997.58.539. [DOI] [PubMed] [Google Scholar]
- 18.Saloner B, Carson N, Le Cook B. Explaining racial/ethnic differences in adolescent substance abuse treatment completion in the United States: a decomposition analysis. Journal of Adolescent Health. 2014;54(6):646–653. doi: 10.1016/j.jadohealth.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Andersen RM, Davidson PL, Kominski GF. Improving Access to Care in America: Individual and Contextual Indicators. In: Andersen RM, Rice TH, Kominski GF, editors. Changing the U.S. Health Care System: Key Issues in Health Services Policy and Management. San Francisco: Jossey-Bass Inc; 2007. pp. 3–32. [Google Scholar]
- 20.National Quality Forum. [Accessed 12/8/10];NQF Endorsed Standards. 2009 http://www.qualityforum.org/MeasureDetails.aspx?SubmissionID=1245.
- 21.National Committee for Quality Assurance. [Accessed 01/06/13];NCQA HEDIS 2016. 2016 http://www.ncqa.org/HEDISQualityMeasurement/HEDISMeasures/HEDIS2016.aspx.
- 22.Harris AH, Humphreys K, Bowe T, et al. Does meeting the HEDIS substance abuse treatment engagement criterion predict patient outcomes? Journal of Behavioral Health Services Research. 2010;37(1):25–39. doi: 10.1007/s11414-008-9142-2. [DOI] [PubMed] [Google Scholar]
- 23.Garnick DW, Lee MT, Horgan C, et al. Lessons from five states: public sector use of the Washington Circle performance measures. Journal of substance abuse treatment. 2011;40(3):241–254. doi: 10.1016/j.jsat.2010.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Garnick DW, Lee MT, Horgan CM, et al. Adapting Washington Circle performance measures for public sector substance abuse treatment systems. Journal of substance abuse treatment. 2009;36(3):265–277. doi: 10.1016/j.jsat.2008.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dunigan R, Acevedo A, Campbell K, et al. Engagement in outpatient substance abuse treatment and employment outcomes. Journal of Behavioral Health Services Research. 2014;41(1):20–36. doi: 10.1007/s11414-013-9334-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Garnick DW, Horgan CM, Acevedo A, et al. Criminal justice outcomes after engagement in outpatient substance abuse treatment. Journal of substance abuse treatment. 2014;46(3):295–305. doi: 10.1016/j.jsat.2013.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Acevedo A, Garnick D, Ritter G, et al. Admissions to detoxification after treatment: Does engagement make a difference? Substance Abuse. 2016;37(2):364–371. doi: 10.1080/08897077.2015.1080784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2002. [PubMed] [Google Scholar]
- 29.Cook BL, McGuire TG, Zuvekas SH. Measuring trends in racial/ethnic health care disparities. Medical Care Research and Review. 2009;66(1):23–48. doi: 10.1177/1077558708323607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Norris T, Vines P, Hoeffel E. [Accessed May 5, 2017];Census Briefs: The American Indian and Alaska Native Population: 2010. 2012 https://www.census.gov/content/dam/Census/library/publications/2012/dec/c2010br-10.pdf.
- 31.Cohn D. [Accessed May 5, 2017];American Indian and white, but not ‘multiracial’. 2015 http://www.pewresearch.org/fact-tank/2015/06/11/american-indian-and-white-but-not-multiracial/
- 32.Krieger N, Chen JT, Waterman PD, et al. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures--the public health disparities geocoding project. American Journal of Public Health. 2003;93(10):1655–1671. doi: 10.2105/ajph.93.10.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.U.S. Census Bureau. [Accessed March 3, 2017];Geographic Terms and Concepts - Census Tract. 2012 https://www.census.gov/geo/reference/gtc/gtc_ct.html.
- 34.Mennis J, Stahler GJ, Baron DA. Geographic Barriers to Community-Based Psychiatric Treatment for Drug-Dependent Patients. Annals of the Association of American Geographers. 2012;102(5):1093–1103. [Google Scholar]
- 35.Molina KM, Alegria M, Chen CN. Neighborhood context and substance use disorders: a comparative analysis of racial and ethnic groups in the United States. Drug and alcohol dependence. 2012;125(Suppl 1):S35–43. doi: 10.1016/j.drugalcdep.2012.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Karriker-Jaffe KJ. Neighborhood socioeconomic status and substance use by U.S. adults. Drug and alcohol dependence. 2013;133(1):212–221. doi: 10.1016/j.drugalcdep.2013.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lee MT, Garnick DW, O'Brien PL, et al. Adolescent treatment initiation and engagement in an evidence-based practice initiative. Journal of substance abuse treatment. 2012;42(4):346–355. doi: 10.1016/j.jsat.2011.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.StataCorp. Heckman two-stage procedure. Stata Statistical Software: Release 11. College Station, TX: StataCorp LP; 2009. [Google Scholar]
- 39.Hosmer D, Lemeshow S, Sturdivant R. Applied Logistic Regression. 3. Hoboken, New Jersey: Wiley & Sons; 2013. [Google Scholar]
- 40.Cook BL, McGuire TG, Zaslavsky AM. Measuring racial/ethnic disparities in health care: methods and practical issues. Health services research. 2012;47(3 Pt 2):1232–1254. doi: 10.1111/j.1475-6773.2012.01387.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Legha R, Raleigh-Cohn A, Fickenscher A, et al. Challenges to providing quality substance abuse treatment services for American Indian and Alaska native communities: perspectives of staff from 18 treatment centers. BMC psychiatry. 2014;14(1):181. doi: 10.1186/1471-244X-14-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Novins DK, Croy CD, Moore LA, et al. Use of evidence-based treatments in substance abuse treatment programs serving American Indian and Alaska Native communities. Drug and alcohol dependence. 2016;161:214–221. doi: 10.1016/j.drugalcdep.2016.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rieckmann T, Moore LA, Croy CD, et al. A National Study of American Indian and Alaska Native Substance Abuse Treatment: Provider and Program Characteristics. Journal of substance abuse treatment. 2016;68:46–56. doi: 10.1016/j.jsat.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 44.McFarland BH, Gabriel RM, Bigelow DA, et al. Organization and financing of alcohol and substance abuse programs for American Indians and Alaska Natives. American Journal of Public Health. 2006;96(8):1469–1477. doi: 10.2105/AJPH.2004.050575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kropp F, Lilleskov M, Richards J, et al. Client and provider views on access to care for substance-using American Indians: perspectives from a Northern Plains urban clinic. American Indian and Alaska native mental health research (Online) 2014;21(2):43. doi: 10.5820/aian.2101.2014.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kramer MR, Hogue CR. Is segregation bad for your health? Epidemiologic Reviews. 2009;31:178–194. doi: 10.1093/epirev/mxp001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.White K, Haas JS, Williams DR. Elucidating the role of place in health care disparities: the example of racial/ethnic residential segregation. Health services research. 2012;47(3 Pt 2):1278–1299. doi: 10.1111/j.1475-6773.2012.01410.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Romley JA, Cohen D, Ringel J, et al. Alcohol and Environmental Justice: The Density of Liquor Stores and Bars in Urban Neighborhoods in the United States. Journal of studies on alcohol and drugs. 2007;68(1):48–55. doi: 10.15288/jsad.2007.68.48. [DOI] [PubMed] [Google Scholar]
- 49.Berke EM, Tanski SE, Demidenko E, et al. Alcohol retail density and demographic predictors of health disparities: a geographic analysis. American Journal of Public Health. 2010;100(10):1967. doi: 10.2105/AJPH.2009.170464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stahler GJ, Mazzella S, Mennis J, et al. The effect of individual, program, and neighborhood variables on continuity of treatment among dually diagnosed individuals. Drug and alcohol dependence. 2007;87(1):54–62. doi: 10.1016/j.drugalcdep.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 51.Dimick J, Ruhter J, Sarrazin MV, et al. Black patients more likely than whites to undergo surgery at low-quality hospitals in segregated regions. Health Affairs. 2013;32(6):1046–1053. doi: 10.1377/hlthaff.2011.1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Guerrero EG, Kao D, Perron BE. Travel distance to outpatient substance use disorder treatment facilities for Spanish-speaking clients. International Journal of Drug Policy. 2013;24(1):38–45. doi: 10.1016/j.drugpo.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rosenblum A, Cleland CM, Fong C, Kayman DJ, Tempalski B, Parrino M. Distance traveled and cross-state commuting to opioid treatment programs in the United States. Journal of environmental and public health. 2011;2011:1–10. doi: 10.1155/2011/948789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gaskin DJ, Dinwiddie GY, Chan KS, McCleary R. Residential segregation and disparities in health care services utilization. Medical Care Research Review. 2012;69(2):158–175. doi: 10.1177/1077558711420263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dinwiddie GY, Gaskin DJ, Chan KS, Norrington J, McCleary R. Residential segregation, geographic proximity and type of services used: evidence for racial/ethnic disparities in mental health. Social science & medicine. 2013;80:67–75. doi: 10.1016/j.socscimed.2012.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mark TL, Levit KR, Vandivort-Warren R, Buck JA, Coffey RM. Changes In US spending on Mental Health And Substance Abuse Treatment, 1986-2005, and implications for policy. Health affairs. 2011;30(2):284–292. doi: 10.1377/hlthaff.2010.0765. [DOI] [PubMed] [Google Scholar]
- 57.Mark TL, Levit KR, Yee T, Chow CM. Spending on mental and substance use disorders projected to grow more slowly than all health spending through 2020. Health affairs. 2014;33(8):1407–1415. doi: 10.1377/hlthaff.2014.0163. [DOI] [PubMed] [Google Scholar]
- 58.Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: 2013. NSDUH Series H-44, HHS Publication No. (SMA) 13-4795. [Google Scholar]
- 59.Substance Abuse and Mental Health Services Administration. Racial and Ethnic Minority Populations. [Accessed 9/14, 2017];Specific Populations 2016. https://www.samhsa.gov/specific-populations/racial-ethnic-minority.
- 60.Archibald ME, Putnam Rankin C. A spatial analysis of community disadvantage and access to healthcare services in the U.S. Social science & medicine. 2013;90:11–23. doi: 10.1016/j.socscimed.2013.04.023. [DOI] [PubMed] [Google Scholar]