Abstract
Background
The international medical community has repeatedly called attention to the harms resulting from benzodiazepine use in older adults, yet use persists and is in fact highest among older adults. The global Choosing Wisely campaign has generated renewed momentum to redress this prescribing practice.
Objectives
To detail annual trends in benzodiazepine incidence and prevalence in older adults between 2010 and 2016 across three health jurisdictions.
Design
Observational multi-jurisdictional cohort study with harmonized study protocol.
Setting
The United States (U.S. (veterans population)); Ontario, Canada; and Australia.
Participants
All beneficiaries ≥ 65 years of age (8,270,000 people).
Measurements
Annual incidence and prevalence of benzodiazepine use stratified by age group (65–74, 75–84 and 85+ years) and sex. We performed multiple regression analyses to assess whether rates of incident and prevalent use changed significantly over time.
Results
Over the study period, we observed a significant decrease in incident benzodiazepine use in the U.S. (2.6% to 1.7%) and Ontario (6.0% to 4.4%) but not in Australia (7.0% to 6.7%). We found significant declines in prevalent use in all jurisdictions, (9.2% to 7.3% in the U.S, 18.2% to 13.4% in Ontario and 20.2% to 16.8% in Australia). While incidence and prevalence increased with age in Ontario and Australia, they decreased with advancing age in the U.S. Incidence and prevalence was higher among women in all jurisdictions.
Conclusion
Consistent with other international studies, there have been small but significant reductions in the incidence and prevalence of benzodiazepine use in older adults across all three jurisdictions, with the exception of incidence in Australia. However, use remains inappropriately high – particularly in those 85 and older – and this warrants further attention from clinicians and policy makers.
Keywords: Benzodiazepines, older adults, Choosing Wisely, Australia, Ontario, United States
INTRODUCTION
Benzodiazepine use in older adults has been associated with a number of harms including increased risk of falls, hip fracture, impaired cognition, all-cause mortality, overdose, and substance use disorder (1–5). As a result, the American Geriatrics Society Beers Criteria and STOPP/START Screening Tools for Geriatric Medicine advise to avoid benzodiazepine use in older adults (6, 7). Most recently, this potentially inappropriate prescribing has been addressed by the Choosing Wisely (CW) International campaign (8), as well as by country-specific CW programs in the United States (U.S.), Canada, and Australia (9–12). Despite this, rates of new and continuing benzodiazepine use in older adults remain higher than in younger age groups (13, 14).
Benzodiazepine use in older adults has been previously described in the U.S., Canada, and Australia (13–16), as well as in several European countries (17). However, differing data sources, methods and time periods make comparisons between studies challenging. Moreover, most studies have not been population-based or have used episode rather than person-level data, impeding analysis of patterns of individual use. In addition, there have been no studies detailing the extent of this low-value practice across multiple jurisdictions since the start of the Choosing Wisely Campaign.
The aim of this study is to detail trends in annual benzodiazepine incidence and prevalence in older adults from 2010 to 2016 using a common methodology across three jurisdictions: the U.S., Ontario, and Australia.
METHODS
Study settings and data
We used prescription claims data from three jurisdictions for this observational study: 1) the Veterans Health Administration of the U.S. Department of Veterans Affairs (VA); 2) the Ontario Drug Benefit (ODB) program; and 3) the Australian Pharmaceutical Benefits Scheme (PBS). Each of these three systems capture prescription claims for enrolled beneficiaries and have been used previously to describe changes in medication utilization in their respective jurisdictions (18–20). While each of these three jurisdictions may provide access to subsidized medicines for a wide age range of people, we limited our analysis to beneficiaries ≥65 years of age, as older adults are the focus of the Choosing Wisely benzodiazepine recommendations (9–12). This study was based on a common protocol and analyses were harmonized across all three individual databases.
Study population
The study population consisted of all people 65 and older in each of the three jurisdictions from 1 January 2010 until 31 December 2016, apart from the U.S. where data was only available until 8 December 2016. The study denominator for each year included any individual that was alive for part of the year and had at least one prescription claim for any medicine. We restricted all analyses to people for whom we had complete capture of prescription claims across the study period; in the Australian cohort this meant restricting the population to people who were concession card holders for the entire period (18).
Medicines of interest
We identified benzodiazepine derivatives – as defined by the Anatomical Therapeutic Chemical (ATC) classification system (i.e., classes N03AE, N05BA, and N05CD) – subsidized within each jurisdiction. The specific benzodiazepines available within each jurisdiction varied (Supplementary Table S1); we excluded intravenous formulations.
Measures and statistical analysis
Characteristics of study populations
We report the sex and age group (65–74, 75–84, and ≥85 years) of all people ≥65 years with at least one prescription claim between 2010 and 2016 by jurisdiction. In addition we report these characteristics for people ≥65 years with at least one benzodiazepine claim over this study period.
Annual incidence and prevalence
We determined yearly incident and prevalent benzodiazepine use in each jurisdiction from 2010 to 2016 (Supplementary Figure S1). We estimated incident (new) use by identifying persons with a benzodiazepine prescription claim during a given calendar year and no prescription claims for a benzodiazepine during the previous 12 months. We estimated prevalent use by identifying persons with at least one prescription claim for a benzodiazepine within a given calendar year. We present incidence and prevalence in each jurisdiction overall and further stratified by age (65–74, 75–84, and ≥85 years) and sex. The denominator for each jurisdiction was the number of people within the corresponding age or sex category that had a prescription claim for any medication during a given year. Incidence and prevalence were expressed as per 100-population.
To determine whether annual incidence and prevalence changed year on year in each jurisdiction, we used multiple Poisson regression to model the number of people with new or prevalent benzodiazepine use each year. Along with study year, we adjusted the model for age group, sex, and the log of the denominator (i.e., total number of people) as an offset term. We reported fixed effects as rate ratios with 95% confidence intervals. Due to significant over-dispersion, as assessed by the Lagrange multiplier test, a negative binomial distribution was used to produce more accurate parameter estimates.
All analyses were performed with SAS, version 9.3 (SAS Institute Inc.) and Stata version 12 (Statacorp).
Ethics and data access approval
The analyses for this study were approved by the: Institutional Review Board of the VA Ann Arbor Healthcare System; the Research Ethics Board at Sunnybrook Health Sciences Centre; and the New South Wales Population and Health Services Research Ethics Committee and Department of Human Services. The data remained within each jurisdiction.
RESULTS
There were differences in age and sex strata among all three study populations (Table 1). Of note there were more people in the older age groups (75–84 and 85+ years) in the Australian study population compared to the other jurisdictions. While the Australian and Ontarian study populations had similar proportions of men and women, the U.S. VA population was almost entirely male.
Table 1.
Characteristics of the three study populations (2010–2016).
| U.S. (/1000 people) | Ontario (/1000 people) | Australia (/1000 people) | |
|---|---|---|---|
| Study population, n | 3888 | 2595 | 1787 |
| Age, n (%) | |||
| 65–74 | 2442 (62.8) | 1736 (66.9) | 888 (49.7) |
| 75–84 | 1049 (27.0) | 626 (24.1) | 646 (36.1) |
| 85+ | 398 (10.2) | 234 (9.0) | 254 (14.2) |
| Sex, n (%) | |||
| Female | 78 (2.0) | 1420 (54.7) | 1010 (56.5) |
| Male | 3810 (98.0) | 1175 (45.3) | 777 (43.5) |
|
| |||
| ≥1 benzodiazepine dispensed, n (%) | 527 (13.6) | 686 (26.4) | 332 (18.6) |
| Age, n (%) | |||
| 65–74 | 360 (68.3) | 357 (52.0) | 141 (42.5) |
| 75–84 | 125 (23.6) | 221 (32.3) | 128 (38.7) |
| 85+ | 43 (8.1) | 108 (15.7) | 62 (18.8) |
| Sex, n (%) | |||
| Female | 14 (2.6) | 439 (64.0) | 221 (66.7) |
| Male | 513 (97.4) | 247 (36.0) | 111 (33.3) |
Annual incidence and prevalence
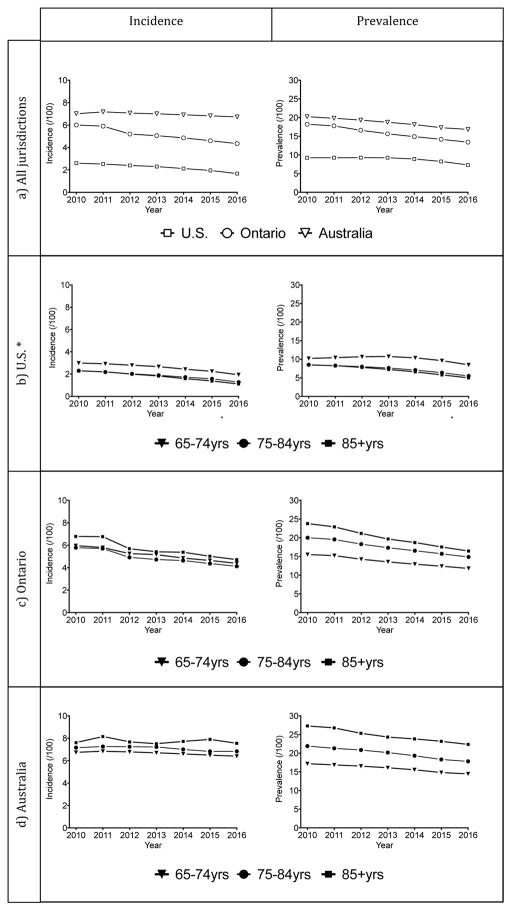
Our estimates of annual incidence and prevalence by jurisdiction are presented in Figure 1 (data available in Supplementary Table S2). We observed a significant linear decline in incident benzodiazepine use in the U.S, (2.6% in 2010 to 1.7% in 2016). The decline in incident benzodiazepine use in Ontario (from 6.0% in 2010 to 4.4% in 2016) was also significant over the entire study period but there was a greater decline between 2011 and 2012 compared to prior and subsequent years. We did not observe a statistically significant change in incident benzodiazepine use in Australia over the study period from (7.0% in 2010 to 6.7% in 2016). (Figure 1, Supplementary Table S3).
Figure 1.
Incidence and prevalence of benzodiazepine dispensing a. in all jurisdictions, b. U.S. c. Ontario, and d. Australia.
*U.S. data available through 8 December 2016; incidence and prevalence calculated accordingly.
There was a significant decline in prevalent benzodiazepine use in all jurisdictions between 2010 and 2016, decreasing from 9.2% to 7.3% in the U.S, 18.2% to 13.4% in Ontario and 20.2% to 16.8% in Australia. The rate of this decline was relatively linear for all jurisdictions.
In general, age-stratified trends followed similar trajectories within jurisdictions (Figure 1b). For both Ontario and Australia, people aged 85 years or older had the highest prevalence followed by 75–84 year olds and then by 65–74 year olds (Figure 1c and 1d respectively). In the U.S, this pattern was reversed, with 65–74 year olds having the highest prevalence. Annual incidence was similar across age groups for Ontario and Australia, while the 65–74 year olds consistently had the highest incident use in the U.S. VA data. Differences in incidence and prevalence between age groups within each jurisdiction were supported by our multiple regression analyses across all jurisdictions (Supplementary Table S3).
Women had the highest incident and prevalent benzodiazepine use across the study period in all three jurisdictions and trends for men and women followed similar trajectories (Supplementary Figure S2). This observation was supported in our multiple regression analyses, where female sex was significantly associated with increased rates of both incident and prevalent benzodiazepine prescriptions, irrespective of jurisdiction (Supplementary Table S3).
DISCUSSION
The U.S., Canada, and Australia were early adopters of the Choosing Wisely campaign (in 2012, 2014 and 2015 respectively) and all emphasize that benzodiazepines should not be prescribed to older persons. Hence we have used a standardized methodology to measure annual incident and prevalent benzodiazepine use between 2010 and 2016 in these jurisdictions. While using a standardized methodology facilitates comparisons of annual trends between jurisdictions, differences in underlying study populations make direct comparisons of absolute incidence and prevalence challenging. However, we found small but statistically significant decreases in benzodiazepine incidence and prevalence across all three jurisdictions, with the exception of incidence in Australia, which did to reach statistical significance. In addition, among older adults, incidence and prevalence were highest in those aged 85 and older in Ontario and Australia, but decreased with advancing age in the U.S. VA population.
It is unclear whether the decrease in benzodiazepine use observed in the U.S. VA population in this study applies more broadly to the general U.S. population. Prevalence figures in this study are similar to those of the general U.S. population in 2008 based on a national prescription database covering around 60% of all retail pharmacy prescriptions (14). However, the decreasing use over time found here is in contrast to recent non-VA U.S. studies demonstrating stable or increasing in use. Analysis of the nationally-representative Medical Expenditure Panel Survey suggested an increase in the prevalence of benzodiazepine use among older adults between 1996 and 2013 (from 4.1% to 5.6% of older adults), although this increase appeared to plateau in the last three years of the study (21). A separate analysis of U.S. ambulatory clinic visits to primary care providers found an increase in visits in which benzodiazepines were prescribed to older adults between 2003 and 2012 (from 5.6% to 8.7% of visits) (22). While overall prevalence in the VA would be expected to be lower than the general population because the population is predominantly male, and fewer men are prescribed benzodiazepines (14), our observed trends persisted following stratification by sex. There have been a number of VA-specific policy and education initiatives focused on safe psychotropic prescribing as well as treatment guidelines (e.g., for PTSD) that may have all contributed to the observed reductions in benzodiazepine prescribing within the VA system (23). It is also conceivable that prescribing has declined more recently in the non-VA U.S. population, but this is yet to be demonstrated.
Our findings of decreasing benzodiazepine use in Australia and Ontario are consistent with previous studies in these jurisdictions (15, 24) and may also be the result of recent initiatives in each jurisdiction to address this practice (20, 25).
The decreases in benzodiazepine use in older adults generally described worldwide are likely to be in response to safety concerns and lack of evidence of effectiveness. Benzodiazepine related “Z-drugs” such as zopiclone and zolpidem were not measured in this study but there are concerns that they are being used in preference to conventional benzodiazepines, putatively because of perceptions of a superior safety profile and this warrants further investigation (26).
Despite the modest decreases in benzodiazepine incidence and prevalence seen in our study, the rates of benzodiazepine use in older adults remain high, in spite of consistent messaging about the hazards of using benzodiazepines in this population. Ongoing use may be related to provider’s tendency to minimize the risks of prescribing to older adults (27), and even patients may do the same (28). Limited access to non-pharmacological alternatives such as psychotherapy (29) and limited physician time (14) are other factors associated with ongoing benzodiazepine initiation.
As demonstrated previously in the general U.S. population (14), as well as for Australia and Ontario in this study, benzodiazepine use typically increases with age, so that rates are highest among the oldest individuals. This is particularly concerning as potential harms may be even greater among those aged 85 and older. It is unusual that in the U.S. VA population, the 65–74 year old age group have the highest rates of use. This may be related to aging of Vietnam-era veterans, who have more diagnosed depression and anxiety than earlier veteran cohorts.
In Ontario, there was a marked decline in incidence between 2011 and 2012. This may be a result of the implementation of the province’s Narcotics Safety and Awareness Act (November 2011) and Narcotics Monitoring System program (May 2012), a two-pronged approach to limit potentially inappropriate benzodiazepine use (20). Similar real-time prescription drug monitoring programs are becoming increasingly prevalent in the U.S., in an effort to limit prescription drug abuse and potentially reduce overdose risk (30). Despite their benefits, prescription drug monitoring programs are unlikely to be nuanced enough to pinpoint potentially inappropriate use as opposed to abuse (5). Australia is yet to implement national prescription drug monitoring or other similar dedicated policy efforts, which might partially explain the lack of change in new use of benzodiazepines in the elderly. At a clinical level, limiting the conversion of new-use to chronic use may be the most effective initial step in reducing the prevalence of benzodiazepine use, as ceasing chronic use can be more challenging. This could be achieved by explicitly limiting the duration of new prescriptions and by not routinely providing repeat prescriptions. For people who have been using benzodiazepines for a long-time, a discussion around the risks and benefits of continued therapy and attempts to gradually dose reduce might be the best strategy (31).
LIMITATIONS
Only subsidized medicines are captured within this study, meaning that the prevalence of benzodiazepine use may be underestimated if patients obtain prescriptions outside of the subsidising program. In Australia, unrecorded private prescribing accounts for up to 10% of all benzodiazepine prescriptions (32) and this may also be an issue for the Ontarian and U.S. VA programs. In addition, restricting the Australia study cohort to people who were continuous concession cardholders may limit the generalizability of the results, as this population tends to be older and have greater comorbidity than the general population. Similarly, while the U.S. study cohort is the largest population in this analysis, it is limited to older adults receiving care in the VA healthcare system. While it was not the intention of this study to identify ‘true’ new use (i.e. first ever use), it should be noted that the 12-month look back used to classify incident use might overestimate ‘true’ new use. We did not measure benzodiazepine related Z-drugs because these were not consistently subsidized across all jurisdictions. There were significant differences in the age and sex strata of the three populations and benzodiazepine sub-populations reflecting differences in organizational structures, though these were accounted for in our regression models of trends over time. Finally, other information such as treatment duration, clinical indication, and co-morbidity was not available consistently across all three jurisdictions, so it is not possible to compare and adjust for these differences between populations.
CONCLUSION
In this analysis across three countries, incident and prevalent benzodiazepine use amongst older adults has decreased in the VA system in the U.S. and Ontario, and prevalent use has decreased in Australia. Our findings are generally consistent with separate international studies that have used varying methods. However, use in the respective older adult populations remains high and warrants further attention from clinicians and policy makers. A detailed description of the methodology used to measure low-value prescribing practice, as well as a description of historical trends for this practice, facilitates harmonization of methodologies across countries and jurisdictions to allow other jurisdictions to benchmark this practice using the same methodology. This also paves the way for future internationally coordinated efforts to decrease low-value care by investigating the motivations for prescribing and the effectiveness of initiatives used to limit benzodiazepine use using gold standard methods such as interrupted time series analyses.
Supplementary Material
Supplementary Table S1: List of benzodiazepines available in each jurisdiction
Supplementary Figure S1: Flow chart outlining incidence and prevalence calculation
Supplementary Figure S2: Incidence and prevalence in each jurisdiction stratified by sex
Supplementary Table S2: Raw incidence and prevalence data in each jurisdiction
Supplementary Table S3: Results of multivariable negative binomial regression modelling
IMPACT STATEMENT.
We certify that this work is novel. We have used a harmonized study protocol to measure annual incident and prevalent benzodiazepine use in older adults across three jurisdictions – the U.S. (veterans population), Ontario and Australia – from 2010 to 2016. The currency of this study relates to the nomination of this practice as a top priority by the global Choosing Wisely campaign. We are not aware of any studies measuring benzodiazepine use in the elderly on a jurisdictional level since the start of the Choosing Wisely campaign. Employing large datasets and a standardized protocol facilitates comparisons of trends in this practice at a population level. We hope the modest decreases in incidence and prevalence demonstrated here will galvanise clinicians and policy makers to take action to make further reductions.
Acknowledgments
Funding Sources
National Health and Medical Research Council (NHMRC) Centre for Research Excellence in Medicines and Ageing (CREMA), Project Grant for measuring low-value care for targeted policy action and Postgraduate award. VA Office of Reporting, Analytics, Performance, Improvement and Deployment (RAPID). The Institute for Clinical Evaluative Sciences (ICES) and the Ontario Ministry of Health and Long-Term Care (MOHLTC).
Funding
This research was supported by the National Health and Medical Research Council (NHMRC) Centre for Research Excellence in Medicines and Ageing (CREMA), a Project Grant for measuring low-value care for targeted policy action and JB received funding support from an NHMRC Postgraduate award. We thank the Department of Human Services Australia for supplying the data. Partial funding for this study was provided by the VA Office of Reporting, Analytics, Performance, Improvement and Deployment (RAPID). DTM was funded by the Beeson Career Development Award Program (NIA 5K08AG04832, the American Federation for Aging Research, The John A. Hartford Foundation, and The Atlantic Philanthropies). This study was supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded in part by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). AGE receives salary support as the HCF Research Foundation Professorial Fellow, receives consulting/sitting fees from Cancer Australia, NPS MedicineWise (facilitator of Choosing Wisely Australia), the Australian Commission on Safety and Quality in Health Care (Atlas of Health Care Variation Advisory Group), the Queensland Government Department of Health, and the Australian Government Department of Health as an appointee to the MBS Review Taskforce.
Footnotes
Conflict of Interest
None to declare
Author Contributions
JB performed Australian analyses, all regression analyses and drafted the manuscript. DM project managed U.S. data analysis and reviewed the manuscript. RVI performed U.S. data analysis. ZB project managed Ontarian data analysis and reviewed the manuscript. GM performed Ontarian data analysis. EK, SB and AE assisted in drafting the manuscript using their jurisdictional perspectives. SP reviewed all drafts of the manuscript and took overall responsibility for the project direction.
References
- 1.Tannenbaum C, Paquette A, Hilmer S, Holroyd-Leduc J, Carnahan R. A systematic review of amnestic and non-amnestic mild cognitive impairment induced by anticholinergic, antihistamine, GABAergic and opioid drugs. Drugs & Aging. 2012;29(8):639–58. doi: 10.1007/BF03262280. [DOI] [PubMed] [Google Scholar]
- 2.Palmaro A, Dupouy J, Lapeyre-Mestre M. Benzodiazepines and risk of death: Results from two large cohort studies in France and UK. European Neuropsychopharmacology. 2015;25(10):1566–77. doi: 10.1016/j.euroneuro.2015.07.006. [DOI] [PubMed] [Google Scholar]
- 3.Wagner AK, Zhang F, Soumerai SB, Walker AM, Gurwitz JH, Glynn RJ, et al. Benzodiazepine use and hip fractures in the elderly: who is at greatest risk? Archives of Internal Medicine. 2004;164(14):1567–72. doi: 10.1001/archinte.164.14.1567. [DOI] [PubMed] [Google Scholar]
- 4.Lader M. Benzodiazepines revisited—will we ever learn? Addiction. 2011;106(12):2086–109. doi: 10.1111/j.1360-0443.2011.03563.x. [DOI] [PubMed] [Google Scholar]
- 5.Maree RD, Marcum ZA, Saghafi E, Weiner DK, Karp JF. A systematic review of opioid and benzodiazepine misuse in older adults. The American Journal of Geriatric Psychiatry. 2016;24(11):949–63. doi: 10.1016/j.jagp.2016.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Campanelli CM. American Geriatrics Society Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults: The American Geriatrics Society 2012 Beers Criteria Update Expert Panel. Journal of the American Geriatrics Society. 2012;60(4):616. doi: 10.1111/j.1532-5415.2012.03923.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gallagher P, Ryan C, Byrne S, Kennedy J, O’Mahony D. STOPP (Screening Tool of Older Person’s Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. International Journal of Clinical Pharmacology and Therapeutics. 2008;46(2):72–83. doi: 10.5414/cpp46072. [DOI] [PubMed] [Google Scholar]
- 8.Levinson W. Webinar. Washington: Academy of Health; 2015. [Accessed July 2017]. Searching for effective innovations I: reducing low-value care. Available from: http://www.academyhealth.org/Events/events.cfm?ItemNumber=16876. [Google Scholar]
- 9.Canadian Geriatrics Society. [Accessed July 2017];Five Things Physicians and Patients Should Question. 2014 Available from: http://www.choosingwiselycanada.org/recommendations/geriatrics/
- 10.Canadian Psychiatric Association. [Accessed July 2017];Thirteen Things Physicians and Patients Should Question. 2015 Available from: http://www.choosingwiselycanada.org/recommendations/psychiatry/
- 11.American Geriatrics Society. [Accessed July 2017];Ten Things Clinicians and Patients Should Question. 2015 Available from: http://www.choosingwisely.org/societies/american-geriatrics-society/
- 12.Australia and New Zealand Society for Geriatric Medicine. [Accessed July 2017];Five Things Physicians and Patients Should Question. 2016 Available from: http://www.choosingwisely.org.au/recommendations/anzsgm.
- 13.Maust DT, Kales HC, Wiechers IR, Blow FC, Olfson M. No End in Sight: Benzodiazepine Use in Older Adults in the United States. Journal of the American Geriatrics Society. 2016;64(12):2546–53. doi: 10.1111/jgs.14379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Olfson M, King M, Schoenbaum M. Benzodiazepine use in the United States. JAMA psychiatry. 2015;72(2):136–42. doi: 10.1001/jamapsychiatry.2014.1763. [DOI] [PubMed] [Google Scholar]
- 15.Islam M, Conigrave K, Day C, Nguyen Y, Haber P. Twenty-year trends in benzodiazepine dispensing in the Australian population. Internal Medicine Journal. 2014;44(1):57–64. doi: 10.1111/imj.12315. [DOI] [PubMed] [Google Scholar]
- 16.Iaboni A, Bronskill SE, Reynolds KB, Wang X, Rochon PA, Herrmann N, et al. Changing pattern of sedative use in older adults: a population-based cohort study. Drugs & Aging. 2016;33(7):523–33. doi: 10.1007/s40266-016-0380-3. [DOI] [PubMed] [Google Scholar]
- 17.Huerta C, Abbing-Karahagopian V, Requena G, Oliva B, Alvarez Y, Gardarsdottir H, et al. Exposure to benzodiazepines (anxiolytics, hypnotics and related drugs) in seven European electronic healthcare databases: a cross-national descriptive study from the PROTECT-EU Project. Pharmacoepidemiology and Drug Safety. 2015 doi: 10.1002/pds.3825. [DOI] [PubMed] [Google Scholar]
- 18.Mellish L, Karanges EA, Litchfield MJ, Schaffer AL, Blanch B, Daniels BJ, et al. The Australian Pharmaceutical Benefits Scheme data collection: a practical guide for researchers. BMC Research Notes. 2015;8(1):634. doi: 10.1186/s13104-015-1616-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kales HC, Zivin K, Kim HM, Valenstein M, Chiang C, Ignacio RV, et al. Trends in antipsychotic use in dementia 1999–2007. Archives of General Psychiatry. 2011;68(2):190–7. doi: 10.1001/archgenpsychiatry.2010.200. [DOI] [PubMed] [Google Scholar]
- 20.Gomes T, Juurlink D, Yao Z, Camacho X, Paterson JM, Singh S, et al. Impact of legislation and a prescription monitoring program on the prevalence of potentially inappropriate prescriptions for monitored drugs in Ontario: a time series analysis. CMAJ Open. 2014;2(4):E256–E61. doi: 10.9778/cmajo.20140027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bachhuber MA, Hennessy S, Cunningham CO, Starrels JL. Increasing benzodiazepine prescriptions and overdose mortality in the United States, 1996–2013. Am J Public Health. 2016;106(4) doi: 10.2105/AJPH.2016.303061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maust D, Blow F, Wiechers I, Kales H, Marcus S. National Trends in Antidepressant, Benzodiazepine, and Other Sedative-Hypnotic Treatment of Older Adults in Psychiatric and Primary Care. The Journal of Clinical Psychiatry. 2017;78(4):e363. doi: 10.4088/JCP.16m10713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wiechers IRHR, Katz I. VA Office of Mental Health Operations. West Haven, CT: Northeast Program Evaluation Center; 2016. Psychotropic Drug Safety Initiative: Phase 1 Evaluation of Impact. [Google Scholar]
- 24.Brett JKE, Daniels B, Buckley NA, Schneider C, Nassir A, Zoega H, McLachlan AJ, Pearson SA. Psychotropic medication use in Australia, 2007 to 2015: Changes in annual incidence, prevalence and treatment exposure. Aust N Z J Psychiatry. 2017 doi: 10.1177/0004867417721018. [DOI] [PubMed] [Google Scholar]
- 25.Westbury J, Tichelaar L, Peterson G, Gee P, Jackson S. A 12-month follow-up study of “RedUSe”: a trial aimed at reducing antipsychotic and benzodiazepine use in nursing homes. International Psychogeriatrics. 2011;23(08):1260–9. doi: 10.1017/S1041610211000421. [DOI] [PubMed] [Google Scholar]
- 26.Siriwardena AN, Qureshi Z, Gibson S, Collier S, Latham M. GPs’ attitudes to benzodiazepine and ‘Z-drug’prescribing: a barrier to implementation of evidence and guidance on hypnotics. Br J Gen Pract. 2006;56(533):964–7. [PMC free article] [PubMed] [Google Scholar]
- 27.Cook JM, Marshall R, Masci C, Coyne JC. Physicians’ perspectives on prescribing benzodiazepines for older adults: a qualitative study. Journal of General Internal Medicine. 2007;22(3):303–7. doi: 10.1007/s11606-006-0021-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mah L, Upshur RE. Long term benzodiazepine use for insomnia in patients over the age of 60: discordance of patient and physician perceptions. BMC Family Practice. 2002;3(1):9. doi: 10.1186/1471-2296-3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lamberg L. Despite effectiveness, behavioral therapy for chronic insomnia still underused. JAMA. 2008;300(21):2474–5. doi: 10.1001/jama.2008.719. [DOI] [PubMed] [Google Scholar]
- 30.Paulozzi LJ, Kilbourne EM, Desai HA. Prescription drug monitoring programs and death rates from drug overdose. Pain Medicine. 2011;12(5):747–54. doi: 10.1111/j.1526-4637.2011.01062.x. [DOI] [PubMed] [Google Scholar]
- 31.Brett J, Murnion B. Management of benzodiazepine misuse and dependence. Australian Prescriber. 2015;38(5):152. doi: 10.18773/austprescr.2015.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hollingworth SA, Siskind DJ. Anxiolytic, hypnotic and sedative medication use in Australia. Pharmacoepidemiology and Drug Safety. 2010;19(3):280–8. doi: 10.1002/pds.1899. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1: List of benzodiazepines available in each jurisdiction
Supplementary Figure S1: Flow chart outlining incidence and prevalence calculation
Supplementary Figure S2: Incidence and prevalence in each jurisdiction stratified by sex
Supplementary Table S2: Raw incidence and prevalence data in each jurisdiction
Supplementary Table S3: Results of multivariable negative binomial regression modelling