Abstract
Background
Surgical outcomes following isolated posterior cruciate ligament reconstruction (PCLR) have been noted to be less satisfactory than the anterior cruciate ligament. Limited understanding of optimal rehabilitation has been implicated as a contributing factor.
Hypothesis/Purpose
The purpose of this review was to gather the literature related to isolated PCLR rehabilitation, extract and summarize current rehabilitation guidelines, identify timeframes and functional measurements associated with common rehabilitation topics and provide recommendations for future research.
Study Design
Literature review.
Methods
A literature review was performed for scientific publications that include a detailed rehabilitation program following isolated PCLR, published between January 2005 and March 2018. Data related to weight-bearing, knee range of motion (ROM), brace usage, specific exercise recommendations and suggestions for return to running and sport activities were extracted and categorized.
Results
A total of 44 articles met inclusion criteria. Post-operative weight-bearing was discussed in 35 articles with recommendations ranging from no restriction to 12 weeks of limitations. Forty-two articles recommended the use of immediate post-operative bracing, the majority of which positioned the knee in full extension, with duration of use ranging from one to 12 weeks post-operatively. Although 30 articles offered detailed descriptions of ROM activity, there was significant variability in timing of initiation, angular excursion and progression of range of motion. Suggested timeframes for returning to sports activity ranged from four to 12 months, with only four articles providing specific objective strength or functional performance criteria necessary for progression.
Conclusions
There is substantial variation in nearly all aspects of published descriptors of rehabilitation following isolated PCLR. Most protocols are based upon biomechanical principles and clinical expertise, relying solely on timeframe from surgery to support rehabilitation decision making. Evidence to compare patient outcomes with specific loading, ROM progression and exercise strategies is currently lacking. Only a small number of protocols incorporate the use of specific objective performance goals to facilitate return to sport decision making.
Keywords: PCL reconstruction, physical therapy, posterior cruciate ligament, rehabilitation
Introduction
The posterior cruciate ligament (PCL) functions as the primary restraint against posterior tibial translation at the knee.1 PCL injuries typically involve high energy trauma to the anterior proximal tibia, with motor vehicle accidents (dashboard injury) and sports related trauma accounting for the majority of injuries.1-3 The incidence of acute PCL injuries has been reported as 1-44% of acute knee injuries, however, isolated PCL tears without additional knee ligament injury are less common.4 Several authors have reported good outcomes with conservative (i.e. non-operative) management in cases with grade I or II isolated PCL injuries.5 However, surgical management may be indicated for patients with acute grade III PCL injuries, with continued knee pain or instability despite conservative treatment.6,7 Although PCL injuries rarely occur in isolation,8,9 they occur most often in athletes from a fall on a hyper-flexed knee during sports activity.3,10
Outcomes following PCL reconstruction (PCLR) are inconsistent in terms of restoring normal knee function and kinematics.5 This may be related to a lower frequency of PCL surgeries, the complex anatomy of the bundles comprising the PCL, and disagreement on the ideal method of surgical reconstruction technique.7,11,12 However, post-operative rehabilitation may also play a fundamental role in outcomes following PCLR.13-15 Effective post-operative rehabilitation is essential for optimizing graft healing, obtaining a functionally stable knee, encouraging safe recovery of athletic activity, and minimizing the risk of re-injury.13,16 Quadriceps and hamstring strength deficits have been identified at two years post-PCLR which can limit optimal graft protection and sport performance.17 There are several aspects of rehabilitation that are commonly discussed in the literature, including the use of early post-operative bracing, weight-bearing status, range of motion (ROM) restrictions, timing of initiation of hamstring exercise, and criteria for return to running and sports activities.5,18,19 However, timeframes for implementing these rehabilitation factors are reported with high variability, and there is currently no consensus regarding an optimal rehabilitation program.5,18,19
The first step in addressing these issues is to fully understand the collection of published post-operative PCLR rehabilitation guidelines in the literature. Therefore, the purpose of this review was to gather the literature related to isolated PCLR rehabilitation, extract and summarize current rehabilitation guidelines, identify timeframes and functional measurements associated with common rehabilitation topics and provide recommendations for future research.
METHODS
Search Strategy
A comprehensive search of PubMed, Embase and Cochrane internet databases was performed in order to identify relevant articles. The combination of search terms utilized were “posterior cruciate ligament reconstruction” OR “PCL” AND “rehabilitation” OR “physical therapy”. Due to the evolving strategies for PCL reconstruction surgical techniques and the impact this may have on rehabilitation strategies, this search was limited to articles published from January 2005 to March 2018. All identified references were exported to EndNote reference management software (Version X7; Thompson Reuters Corporation, New York, NY).
STUDY SELECTION
Following removal of duplicate citations, titles and abstracts were screened by two independent reviewers (M.S. and E.G.) for relevance and full-text analysis. Thereafter, full text articles were assessed for eligibility by the same team of reviewers using predetermined eligibility criteria. Eligible articles included information on isolated PCLR only. Studies with multi-ligament or other concomitant surgical procedures were excluded. Selected articles had to specifically outline post-operative rehabilitation guidelines within human subjects and had to be in English language. This literature review is inclusive of studies from Level V to Level I (case reports, case-control designs, cohort studies, prospective studies and randomized controlled trials). Previous literature and systematic review articles were excluded.
ASSESSMENT OF STUDY QUALITY/RISK OF BIAS IN INDIVIDUAL STUDIES
Studies were classified according to Oxford Centre for Evidence Based Medicine (CEBM) Levels of evidence. A formal assessment of risk of bias was not performed as the information extracted for this review was unrelated to the type of study design or each study's reported results. Thus, for the purposes of this review paper, all extracted data is of equal relevance, irrespective of study quality.
DATA EXTRACTION
Data extraction was performed by M.S. and E.G. and was agreed on by consensus. Any data related to study design, subject characteristics (age, sex), surgical technique including graft choice, details of rehabilitation including weight-bearing status, use of post-operative brace or other immobilization, knee range of motion guidelines, specific strengthening exercise instructions with particular attention to the initiation of hamstring specific strengthening exercises, and criterion for advancement through return to advanced rehabilitation and sports activities was extracted and is outlined in Table 1.
Table 1.
Summary of Included Studies' Recommendations on Rehabilitation Milestones and Timeframes following PCL Reconstruction
| Author, year | Level of Evidence* | Weight-bearing | Brace | Range of Motion | Hamstring | Running, agility, plyometrics | Return to Sport |
|---|---|---|---|---|---|---|---|
| Accadbled F et al., 2013 | IV | PWB initially; FWB by 9 wk | Long leg cast × 6 wk; hinged knee brace × 6 wk | Run: 6 mo | 9 mo | ||
| Adler GC. 2013 | IV | Extension brace × 1 wk | Delayed; > 1 wk | ||||
| Bovid KM et al., 2013 | IV | Early, limited and protected ROM | 9-12 mo | ||||
| Cavanaugh JT, 2015 | V | TTWB × 2 wk; PWB × 6 wk; FWB by 7 wk | Extension brace × 6 wk | Immediate; 0-90˚ | 6 wk (active) | Agility: 5 mo; Run: 4 mo‡; Plyo: 4 mo | 24 wk§ |
| Chahla J, 2016 | V | NWB × 6 wk; FWB by 7 wk | PCL brace (Jack brace or Rebound brace) × 6 mo† | Immediate; 0-90˚ | Agility: 6 mo; Run: 6 mo‡; Plyo: 6 mo | ||
| Chen & Gao 2009 | IV | WBAT | Extension brace × 4 wk | Delayed; > 5 wk | Run: 4 mo | ||
| Chuang TY et al., 2011 | IV | WBAT | Extension brace × 12 wk, unlocked | Delayed; > 4 wk | 9 mo | ||
| Deie M et al., 2015 | III | “Fixed” brace × 2 wk, PCL brace until 6 mo | Run: 6 mo | 10-12 mo | |||
| Eguchi A et al., 2014 | IV | NWB × 3 wk; PWB | Extension brace × 1 wk | Delayed; > 1 wk | Run: 4 mo | ||
| Fanelli GC et al., 2007 | V | NWB × 6 wk; PWB × 3 wk; FWB by 10 wk | Extension brace × 4 wk; unlocked 4-6 wk | Delayed; > 3 wk | 9-12 mo | ||
| Fanelli GC et al., 2009 | V | NWB × 5 wk; PWB × 4 wk; FWB by 10 wk | Extension brace × 5 wk; unlocked, d/c brace at 10 wk; PCL brace | Delayed; > 6 wk | Agility: 25 wk | 37 wk | |
| Fanelli GC et al., 2010 | V | NWB × 5 wk; PWB × 4 wk; FWB by 10 wk | Extesnion brace × 3 wk; unlocked | Delayed; > 4 wk | 6 mo (resisted OKC) | 6 mo | |
| Fanelli GC et al., 2010 | V | NWB × 5 wk; PWB × 4 wk; FWB by 10 wk | Extension brace × 5 wk, d/c brace at 10 wk; PCL brace | Delayed; > 5 wk | 9 mo | ||
| Fanelli GC et al., 2015 | V | NWB × 3 wk; PWB × 2 wk; FWB by 6 wk | Extension brace × 3 wk, d/c brace at 10 wk | Delayed; > 3 wk | 9 mo | ||
| Fanelli GC, 2008 | V | NWB × 6 wk; PWB × 3 wk; FWB × 10 wk | Extension brace × 3 wk; unlocked | Delayed; > 4 wk | 6 mo (resisted OKC) | 6 mo | |
| Garofolo R et al., 2006 | IV | NWB × 2 days; PWB × 7 wk; FWB by 8 wk* | Extension × 3 wk | Delayed; > 3 days | 3 mo (resisted OKC) | 9 mo | |
| Gill et al., 2012 | IV | PWB × 5 wk; FWB by 6 wk | Extension brace × 2 wk; unlocked, d/c brace at 6; functional brace at 12 | Immediate; passive | 18 wk | ||
| Giombini et al., 2007 | V | PWB × 4 wk; FWB by 5 wk | Extension brace × 2 wk; unlocked | Delayed; > 4 days | 12 wk (“actively put to work”) | Agility: 7 mo; Run: 5 mo‡; Plyo: 7 mo | 8 mo§ |
| Goudie et al 2010 | IV | TTWB × 6 wk; PWB × 3 wk; FWB by 10 wk | Extension brace | Immediate, auto-assisted ROM exercise | 3 - 9 mo | ||
| Hermans et al 2009 | IV | PWB × 7 wk; FWB by 8 wk | Brace locked in 15˚ flexion × 4 wk | Delayed; > 4 wk | 9 mo§ | ||
| Huang et al 2010 | IV | NWB × 2 wk; PWB × 3 wk; FWB by 6 wk | General: 3 mo; competitive: 4 mo | ||||
| Johnson, D 2009 | V | PWB × 5 wk; FWB by 6 wk | Extension splint immobilization | 12 mo | |||
| Kim et al 2009 | III | PWB × 6 wk; FWB by 7 wk | Extension brace × 2 wk; PCL brace × 6 wk | Delayed; > 2 wk | 6 mo | ||
| Lee & Jung 2013 | V | WBAT | Extension brace | ||||
| Li et al 2015 | IV | NWB × 6 wk; PWB × 5 wk; FWB by 12 wk | Extension brace × 4 wk, d/c brace at 12 wk | Immediate; 0-90˚ | 6 mo | 6 mo (light), 9 mo (full) | |
| Lim et al 2010 | III | PWB × 7 wk; FWB by 8 wk | Extension brace × 6 wk | Passive in prone | 4 mo | 9 mo | |
| Lim et al 2015 | III | PWB × 6 wk; FWB by 7 wk | Extension brace × 6 wk, d/c brace at 12 wk | Immediate; 0-90˚ | 12 wk | Run: 12 wk | 9 mo |
| MacGillivray JD et al., 2006 | III | TTWB × 4 wk; PWB × 2 wk; FWB by 7 wk | Extension brace × 4 wk | “Early post-operative period”: 0-90˚ (passive) | 9 mo | ||
| Maruyama et al 2012 | III | PWB × 2 wk; FWB by 3 wk | Extension brace | Run: 6 mo | 8 mo | ||
| Marx et al 2009 | V | PWB × 4 wk; FWB by 5 wk | Extension brace × 4 wk | Delayed; > 4 wk | 4 mo | Run: 6 mo | 9 mo |
| Puh et al 2014 | V | Extension brace × 4 wk; unlocked | Immediate; 0-90˚ (passive in prone) | ||||
| Quelard et al 2010 | IV | TTWB × 1 wk; PWB × 1 wk; FWB by 3 wk | Extension brace × 45 days | Immediate; 0-90˚ | 6 mo (resisted OKC) | Run: 90 days | 8 mo |
| Ranalletta et al 2010 | V | WBAT | Brace unlocked to 90˚ | Immediate; 0-90˚ | Agility: 7 mo; Run: 5 mo | 9 mo | |
| Seon JK et al., 2006 | III | NWB × 7 wk; PWB × 4 wk; FWB by 12 wk | Extension brace × 4 wks, d/c brace at 12 wk | Run: 6 mo | |||
| Spiridonov et al 2011 | IV | NWB × 6 wk; FWB by 7 wk | Jack PCL brace × 6 mo† | Immediate; 0-90˚ | Run: 6 mo‡ | 9 mo | |
| Stannard & McKean 2009 | III | WBAT | Extension brace × 1 wk; unlocked | Immediate, no restriction | Run: 6 mo | 6 mo | |
| Taylor & Miller 2009 | V | WBAT | Extension brace | Begun in prone | Discouraged | Run: 4 mo | 6 mo |
| Tornese et al 2008 | II | Extension brace × 1 wk; unlocked, d/c brace at 6 wk | Immediate; 0-90˚ | Medium impact: 8 mo; High impact: 9 mo§ | |||
| Wong et al 2009 | II | PWB × 6 wk; FWB by 7 wk | Extension brace × 4 wk | 6 wk | 6-12 mo | ||
| Wu et al 2007 | IV | PWB × 6 wk; FWB by 7 wk | Extension brace × 1 wk | Immediate; 0-90˚ | 6 wk | 6 mo (light), 9 mo (full) | |
| Xu et al 2014 | III | LARS - PWB × 4 wk; FWB by 5 wk; HTG -NWB × 2 wk, PWB weeks × 7 wk; FWB by 10 wk | Protective brace × 8 wk | Delayed; LARS > 1 wk; HTG > 3 wk (0-90˚) | LARS: RTS: 2 mo (light), 4 mo (full); HTG: RTS: 4 mo (light), 10 mo (full) | ||
| Zayni et al 2011 | III | Extension brace × 45 days | 6 mo | Run: 150 days | 7 mo | ||
| Zhao & Huangfu, 2007 | IV | Extension brace × 2 mo | Delayed, > 3 wk (0-120˚) | Run: 3 mo | |||
| Zhao et al, 2008 | IV | Extension brace × 2 mo | Delayed, > 3 wk (0-120˚) | Run: 3 mo | 12 mo |
Abbreviations: wk, week(s); mo, month(s); NWB, Non-weight-bearing; PWB, TTWB, toe touch weight-bearing; partial weight-bearing (20-80% full weight-bearing); FWB, Full weight-bearing; LARS, Ligament Advanced Reinforcement System; HTG, Hamstring Tendon Autograft; d/c, discharge; ROM, range of motion; plyo, plyometrics; *, Level of evidence based on Oxford Centre for Evidence Based Medicine - Levels of Evidence; †, additional criteria prior to discharge of brace; ‡, additional criteria prior to running; §, additional criteria prior to return to sport
DATA ANALYSIS
Data related to the purpose of this review was tabulated and reported only using frequency distribution.
RESULTS
The search strategy retrieved a total of 378 studies. After screening 54 full-text articles for eligibility, 44 were included in the review. (Figure 1).
Figure 1.
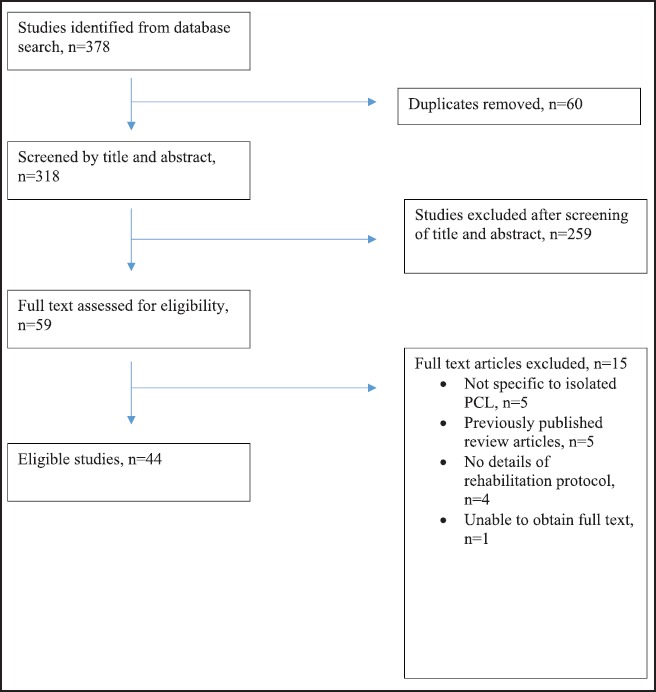
Flowchart outlining literature search for the current review.
STUDY QUALITY/TYPE
The included studies were classified by level of evidence based on the Oxford Centre for Evidence-based Medicine – Levels of Evidence (I-V). Of the 44 studies, there were 2 level II studies, 10 level III studies, 17 level IV studies and 15 level V studies. There were no studies identified that specifically evaluated differences between rehabilitation techniques after PCLR.
WEIGHT-BEARING PRECAUTIONS
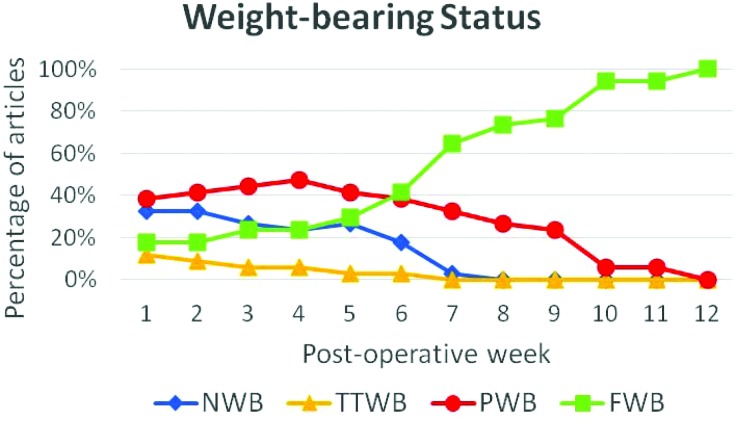
There were 35 (80%) articles that discussed a specific weight-bearing progression, with all studies recommending a progression based on timeframe following surgery.6,16,17,20-50 Recommendations for non-weight-bearing (NWB) immediately after surgery was included in 12 articles, with duration ranging from two to eight weeks post-operatively.6,16,24-28,32,36,44,45,51 Four studies recommended toe-touch weight-bearing (TTWB) status initially, ranging from 10 days to six weeks.17,21,39,42 Fourteen studies recommended immediate partial or progressive weight-bearing (PWB, ranging from 20-80% full weight-bearing)20,29-31,33,34,37,38,40,41,48-50,52 and six studies suggested full weight-bearing or weight-bearing as tolerated (FWB) immediately following surgery.22,23,35,43,46,47 For studies utilizing restricted weight-bearing status following surgery, only two gave specific details regarding the timeframe for progression to FWB, which ranged from 10 days to 12 weeks .42,44 (Figure 2).
Figure 2.
Percentage of articles (n = 34) recommending a particular weight-bearing status based on post-operative timeframe (weeks).
Abbreviations: NWB: non-weight-bearing; TTWB: toe touch weight-bearing, PWB: partial weight-bearing (ranging from 20-80% of full weight-bearing); FWB: full weight-bearing.
POST-OPERATIVE BRACING
There were 42 articles (95%) that discussed the use of immediate post-operative bracing.6,16,17,20-31,33-59 Thirty of these articles recommended maintaining the knee in full extension while also providing specific timeframes for weaning or discontinuing use of the brace.6,16,21-30,34,36-39,41,42,44,46,48,49,51-53,55-59 Fifteen of these articles recommended unlocking the brace prior to discharging the patient from the brace,16,23-28,30,36,37,44,46,52,55,56 while the other fifteen did not specify unlocking the brace.21,22,29,34,38,39,41,42,48,49,51,53,57-59 Of the studies recommending unlocking the brace, only four provided specific ranges (degrees) for wearing the brace, which initially ranged from 30-90˚ between one and four weeks post-operatively.30,52,55,56 The timeframe to discontinue brace usage after being locked in extension varied from 1 to 8 weeks post-operatively.49,51,53,58,59 Additionally, one study recommended unlocking the brace at 12 weeks, but was not specific with timeframe for removing the brace.23 Other studies discontinued the brace between six and 12 weeks after the brace was unlocked.16,24,28,30,36,37,44,52,56 Details regarding specific time periods or knee position for brace usage were missing from eight articles.17,20,33,35,40,47,50,54 One author allowed for immediate unrestricted knee motion up to 90 ° flexion within a brace43 while another recommended locking the knee in 15 ° of flexion for a period of eight weeks after surgery.31 While most articles described the use of a simple hinged knee brace, two studies6,45 recommended a PCL specific brace.
RANGE OF MOTION
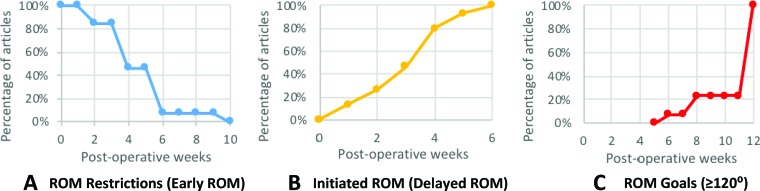
Thirty-five articles (80%) discussed ROM recommendations following PCLR.6,16,17,21-31,34,36-39,41-43,45-47,49-53,55,56,58-60 Four studies recommended passive ROM exercises,38,39,52,55 one with auto assisted ROM exercise,17 and the remaining studies were non-specific with type of ROM exercise. Five of these articles did not give details regarding specific timeframes for initiation of ROM exercises.17,38,39,47,60 The remaining articles were classified into two groups based upon the point in rehabilitation that ROM exercises began. The “early ROM” articles were defined as those allowing for immediate ROM exercises post-operatively, while the “delayed ROM” articles were those that initially deferred ROM exercises until a set post-operative time period. (Figure 3)
Figure 3.
Percentage of articles discussing ROM exercise and goals based on post-operative timeframe (weeks). A) Each article allowing immediate ROM exercise to ≤ 90˚ (n = 13) was progressed beyond this restriction between two and 10 weeks post-operatively. B) Articles initially delaying knee ROM (n = 15) allowed the onset of ROM exercise between one and six weeks. C) Articles recommending a ROM goal of ≥ 120˚ (n = 13) ranged from six to 12 weeks post-operatively.
Early Range of Motion
There were 19 studies that allowed for early ROM following PCLR.6,17,21,29,30,36-39,42,43,45-47,49,52,55,56,60 Despite all allowing for early knee motion, there were many differences in degrees of motion allowed and progression timeframes. Two articles allowed for unrestricted ROM based upon patient comfort.17,46 Recommendations for immediate ROM exercises within a limited range of 0 to ≤ 90˚ of knee flexion was included in 13 articles.6,21,29,30,36,37,42,43,45,49,52,55,56 (Figure 3) From this restricted knee motion, ROM exercise was permitted beyond 90˚ after two to 10 weeks. Two studies allowed for early protected ROM but failed to give specific details regarding motion restrictions and time for progression.39,60 Two articles recommended early ROM exercises specifically performed in the prone position without stating restrictions for knee motion. 38,47
Delayed Range of Motion
There were 16 studies that recommended delayed ROM following PCLR.16,22-28,31,34,41,50,51,53,58,59 Xu and colleagues50 were the only authors who differentiated recommendations based upon graft type, delaying ROM exercise for one week if undergoing a “Ligament Advanced Reinforcement System” (LARS procedure) and delaying three weeks with hamstring tendon autograft (HTG) procedure. The onset of ROM exercises in the remaining 15 studies varied from one to six weeks post-operatively. There were two studies that began ROM within the first week following PCLR,51,53 2 articles after two weeks,34,59 three after three weeks,25,28,58 five after four weeks,16,23,24,31,41 two after five weeks22,26 and one after six weeks.27 (Figure 3) Once ROM was initiated, some articles did limit the degree of allowable knee motion to 60°,23 ≤ 90°,22,34 and ≤ 120˚.58,59 There were 10 articles that allowed for unrestricted motion once ROM exercises began.16,24-28,31,41,51,53
Range of Motion Goals
With such variation in onset and progression of ROM exercises, articles were further analyzed for discussion of specific goals for knee ROM milestones. Two articles recommended achieving 60° knee flexion by four to five weeks post-operatively,23,30 13 recommended a goal of 90˚ as early as two weeks or as late as 12 weeks post-operatively,21-23,30,36,37,42,45,49,50,52,55,56 and seven recommended 120-130˚ by two to three months.21,22,36,37,42,43,49 Goals for achieving full knee ROM ranged from as early as six weeks52 to three months post-surgery.23,30,56,60
STRENGTHENING EXERCISES
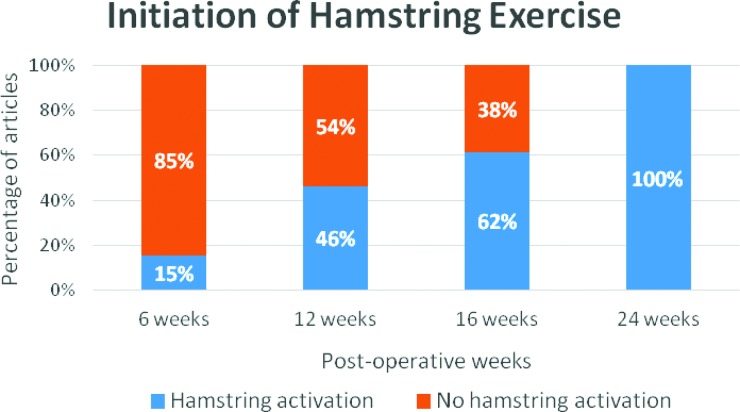
Hamstring Strengthening
Fifteen studies (34%) described recommendations for initiating isolated hamstring exercise following PCLR.16,17,21,24,29,30,36-38,41,42,47-49,57 Three of these articles recommended hamstring exercises beginning at six weeks post-operatively,21,48,49 with one study specifying “active” knee flexion only.21 The remaining articles delayed hamstring specific exercises for longer time periods with four studies delaying until 3 three months,17,29,30,37 two studies delaying until four months38,41 and five studies delaying until six months post-surgery.16,24,36,42,57 Four studies specifically recommended delaying open kinetic chain (OKC) knee flexion, ranging from three to six months.24,26,29,42 Taylor & Miller recommended hamstring activation being “discouraged” in the early post-operative period, but did not specify when hamstring exercise could begin.47 (Figure 4)
Figure 4.
Percentage of articles (n = 13) discussing initiation of resisted hamstring exercise at a particular post-operative timeframe (weeks). For each post-operative timeframe, the percentage of articles are demonstrated as allowing hamstring activation (blue) or not allowing hamstring activation (orange) with strengthening exercises.
Quadriceps Strengthening
There were 11 studies (41%) that outlined specific recommendations for isolated quadriceps strengthening (i.e. OKC knee extension) as part of the PCLR rehabilitation program.17,21,24,26,29,30,32,33,35,36,46 The initiation of OKC quadriceps exercises occurred at two weeks,32 four weeks,29,33,36 six weeks,17,21 11 weeks,24,26 and five months.46 Two studies recommended OKC exercises, but did not specify timeframes for initiation.35,54
Functional Strengthening
Twenty-three articles (52%) included specific recommendations in regards to timing for the initiation of closed kinetic chain (CKC) exercise.6,16,17,21,23-26,29,30,33-38,41,42,44-46,52,60 Three articles allowed CKC exercises immediately following surgery.21,46,52 Eighteen articles recommended initiating CKC exercises at four weeks,29 six to seven weeks,6,17,30,33,34,36,38,41,42,45 11-12 weeks,16,23-26,37 and four months60 following PCLR. Two articles specifically mentioned utilizing CKC exercises but were non-specific with regards to timing for initiation.35,44
Several authors recommended a restricted range of knee excursion once CKC exercises were initiated.21,24,26,30,35,36,42,45 Four studies limited knee flexion depth to 30-45˚,24,26,30,35 while another four studies permitted knee flexion to 60-70˚.21,36,42,45
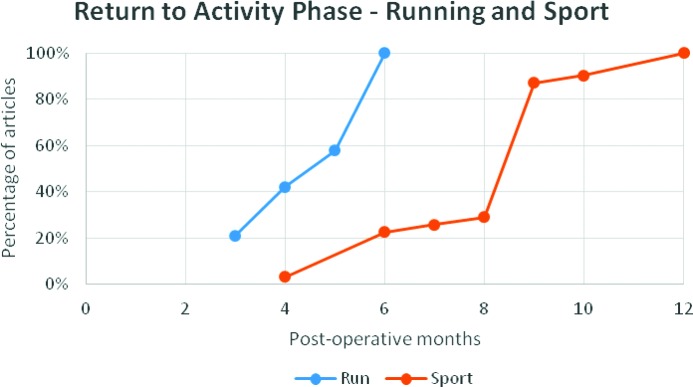
RETURN TO RUNNING, AGILITY AND PLYOMETRIC ACTIVITY
Nineteen studies (43%) provided specific recommendations for initiating running after PCLR.6,20-22,30,37,40-47,51,54,57-59 All studies indicated time from surgery was an important consideration to begin this progression, with time requirements ranging from three to six months post-surgery. (Figure 5) There were four articles that outlined additional criteria to initiate running. 6,21,30,45 Two of them required < 2 mm of posterior tibial translation relative to the contralateral limb, assessed with kneeling radiographs.6,45 Other criteria included full knee ROM,21,30 the absence of pain/swelling,21 satisfactory quality of movement on a stair descent test,30 and limb strength symmetry of at least 75%.30
Figure 5.
Percentage of articles recommending initiation of running (n = 19 articles, orange) and return to sport (n = 31 articles, blue) activities based on post-operative timeframe (months).
Limited information was available regarding rehabilitation progression to plyometrics and agility activities. Two articles provided time based recommendations for beginning plyometric exercise at four months and seven months post-operatively,21,30 while three studies recommended beginning agility activities at five to seven months post-operatively.21,27,43
RETURN TO SPORTS
There were 36 articles (82%) that discussed recommendations for resuming sports activities following PCLR.16,20,21,23-34,36-43,45-52,54,56,57,59,60 (Figure 5) Time from surgery was once again cited as a frequent standard for progression with time requirements of four to five months,32,52 six to seven months,21,24,26,46-48,57 eight to nine months,16,20,23,25,27-31,36-43,45,49,56,60 and 10-12 months33,51,54,59 all cited. Kim et al specifically indicated “low impact” sports could begin at six months post-operatively, but did not comment on any further progression beyond this level of play.34 Xu and colleagues50 discussed different timeframes for returning to sports depending upon graft type, recommending return to sports at four months for LARS and 10 months for HTG.
There were four studies that identified specific goals for strength and functional performance prior to returning to full sports participation.21,30,31,56 All of these articles recommended quadriceps or hamstring limb symmetry goals of > 85% for strength. Functional performance testing using single leg hopping tasks were recommended by three authors, with limb symmetry goals from 85-90%.21,30,56 Tornese and colleagues recommended that strength and functional performance goals be achieved prior to participation in medium impact sports at eight months post-operatively and high impact sports at nine months.56
DISCUSSION
Effective rehabilitation after PCLR is an essential component for optimizing post-surgical outcomes and resuming desired levels of athletic performance. The results of this review illustrate that recommendations for specific components of rehabilitation, functional performance testing, and resumption of activity following PCLR are highly variable. In addition, there are currently no studies that directly compare the efficacy or associated outcomes of these various aspects of rehabilitation protocols and current rehabilitation recommendations are based on low level evidence. This is in striking contrast to intervention strategies (i.e. therapeutic exercises) and performance assessment after anterior cruciate ligament reconstruction (ACLR) which have been more thoroughly investigated.61,62
WEIGHT-BEARING
Within the current review, weight-bearing recommendations ranged from no restriction to 12 weeks of limited weight transfer through the limb (Figure 2). The degree of weight transferred through the operated limb is an important rehabilitation consideration because of the need to minimize stress on the PCL graft, while still maintaining optimal health of joint cartilage and to stimulate bone tunnel healing.63 Recently, Mook and colleagues analyzed the effects of simulated load variations on acquired PCL graft laxity and found that while PWB status had no effect on graft laxity, FWB in early rehabilitation did correlate with significantly increased graft laxity.64 They concluded that rehabilitation protocols should avoid early post-operative weight-bearing as this may contribute to graft laxity and an unstable knee complex. Although this review does suggest some evidence favoring delayed weight-bearing exists, many questions regarding optimal loading after PCLR remain. Future clinical and laboratory-based research studies are necessary to determine optimal post-operative weight-bearing and progression following PCLR.
BRACING AND RANGE OF MOTION
There appeared to be the most consensus among authors regarding the need for protected mobility after PCLR, with 95% of articles recommending a period of bracing post-operatively. The use of bracing was typically coupled with specific recommendations regarding knee motion exercises after surgery. The principle theory for restricting knee motion following PCLR lies in biomechanical studies that have demonstrated tension in portions of the PCL, increasing with increasing knee flexion motion,43,65,66 and notions that early flexion mobilization after PCLR may be associated with graft stretching and knee instability.64 In accordance, the majority of studies included in this review support a gradual, flexion ROM program after PCLR.
Despite global adherence to this principle, there is significant variability in ROM exercise prescription related to the timing of introducing motion exercises (immediate versus delayed) and the degree of allowable motion permitted. In addition, there was variation in positional preferences, with some protocols specifically limiting knee ROM exercises to prone only and utilization of posterior tibial supports out of further concern for graft stress.21,30,37,55
Currently, there are no studies evaluating the effect of different ROM protocols on clinical outcomes after PCLR. While graft protection is important, unnecessarily restricting knee motion could lead to difficulty restoring knee motion, prolonged rehabilitation, increased likelihood of arthrofibrosis and limited patient satisfaction.67,68 Research studies comparing outcomes associated with early versus delayed knee motion and varying ROM exercise protocols are necessary in order to provide clinicians with improved evidence to empower clinical decision making regarding this important aspect of rehabilitation.
STRENGTHENING EXERCISES
Exercise selection is an important consideration following knee surgery in order to properly balance the goals of graft protection with muscular activation and strengthening.69,70 The initiation of isolated hamstring strengthening after PCLR is among one of the most highly debated aspects of rehabilitation. Contraction of the hamstrings can create deleterious posterior shear forces within the tibiofemoral joint, compromising the integrity of healing PCL graft.71 As a result, hamstring contraction and strengthening exercises have been discouraged in the early phases of PCLR rehabilitation. Although most articles agreed upon this principle of deferring resisted hamstring exercises, there were only 14 studies providing specific recommendations to initiate hamstring exercise. Additionally, timing for beginning hamstring strengthening was highly variable, ranging from six weeks to six months.21,24,26,36,42,48,49,57 Further research is necessary to more fully understand the implications of varying types of hamstring exercises and the timing of initiation of those exercises on graft integrity and knee stability. Research of this nature will help direct rehabilitation professionals in more precise exercise prescription for optimizing hamstring strength recovery, which is necessary for normalizing knee biomechanics and promoting return to activities after surgery.72
With regard to initiating OKC or CKC exercises, there were some common trends that emerged during this review. Nearly half of the studies emphasized quadriceps strengthening as an important aspect of rehabilitation, likely due to the role quadriceps strength has in maintaining knee stability, providing PCL graft protection, resuming athletic activity and reducing the potential for subsequent knee injuries.69,70,73-75 Restricted knee flexion motion from 0-50˚ with both OKC and CKC exercises has been found to minimize strain on the PCL.13,37,71 Exercises allowing proper co-contraction of quadriceps and hamstrings muscle groups (e.g. mini-squats, short arc leg press) are commonly recommended within this protective range to balance strengthening gains and graft protection.37,71,76 Despite this understanding, the results of this review show a large degree of variation in onset and permitted joint excursion with both OKC and CKC strengthening exercises. Future laboratory studies are needed to better understand the effects of specific OKC and CKC exercises on PCL graft integrity, while clinical research is needed to determine optimal timing and strength gains produced through varying exercise prescriptions. This information is essential as some studies have identified persistent quadriceps weakness up to 24 months following PCLR and deficits in quadriceps strength may lead to sub-optimal functional outcomes.17,21,30,31,56 Optimizing exercise prescription through evidence informed practice may help improve outcomes within this population.
LATE PHASE REHABILITATION AND RETURN TO SPORTS
As the majority of PCLR surgeries occur in athletes, it is important to incorporate appropriate and safe return of higher level activities into the rehabilitation program.10 The results of this review indicate that the decision to initiate a running, agility and plyometric training program was frequently based on timeframe from surgery alone. Only two studies recommended objective strength criteria be achieved in order to initiate a running program.30,31 Quadriceps and hamstring strength criteria have been frequently cited as requirements for activity progression following ACLR, as deficits in strength may lead to reduced knee stability when progressing to these activities.77-80 Thigh muscle strength deficits similar to those found after ACLR have also been reported following PCLR,17,75,81 however, specific strength goals seem to be under-utilized to support rehabilitation progression post-PCLR.
With regards to return to unrestricted sports, most protocols included within this review once again relied heavily upon time-based criteria, which were highly variable, ranging from four to 12 months post-operatively. There were nine studies that outlined some type of strength and/or functional goals to support the decision to return to sport,6,20,21,27,30,31,39,45,48 however, only three of these articles included enough detail for practical clinical application.21,30,31 Although outcomes with return to sport have not been commonly researched after PCLR, a combination of timeframe, strength and functional performance measures (e.g. unilateral hop tests) have been advocated as screening tools post-ACLR to help reduce risk of re-injury upon return to sports.70,79,82 Similar goals of optimizing strength return and functional performance while allowing adequate time for graft maturity, would likely contribute to optimal outcomes following PCLR. However, more research is needed to provide specific recommendations and better support this theory.
There are several limitations to this review. First, the current literature review consisted of rehabilitation protocols following isolated PCLR only. Concomitant injuries and additional procedures are common within this population and may require different rehabilitation strategies than those discussed in this review. In addition, the level of evidence outlining rehabilitation recommendations following PCLR is weak, as it is currently based primarily on principles of physiological healing, biomechanical modeling and personal opinion. Research related to rehabilitation following PCLR is not as common as other knee injuries, likely due to the low incidence of PCL injury. Thus, the results of this review should be interpreted within the context of literature available for review. In addition, multiple entries with the same primary author(s) were included within this study. Although this decision may bias the results of this review towards specific authors, the authors of this review chose to include these studies as the protocols outlined under the same primary author did have specific differences within them, and it was felt inclusion of these articles gave the most accurate reflection of what exists within the published literature. Nonetheless, it should be noted that this decision may bias the results of this review towards the opinions of those authors. Finally, this review included literature published only within the past 10 years. The authors felt that this limitation was necessary in order to limit any differences in rehabilitation protocols that may exist due to evolving surgical techniques and graft types. However, it should be noted that any pre-existing literature beyond our inclusion criteria was not included within this review.
CONCLUSION
Post-surgical rehabilitation strategies and effective decision making for safe return to sports are important considerations for sports medicine practitioners, as athletes represent a large proportion of those undergoing PCL reconstuction.8,9,3,10 Currently, only low level evidence exists to support rehabilitation recommendations following PCLR. Although there is some level of agreement in the literature related to restrictions in weight-bearing, range of motion, brace usage or strengthening exercise prescription, there is no consensus regarding optimal administration and specific application of these factors. The majority of rehabilitation progression goals were based on post-operative timeframes, with few articles outlining specific objective criteria to provide for more detailed clinical decision making. Additional studies should be conducted to prospectively evaluate rehabilitation protocols in order to establish improved rehabilitation guidelines incorporating graft protection, optimal loading, exercise strategies and readiness to return to higher level activities.
REFERENCES
- 1.Wind WM Jr. Bergfeld JA Parker RD. Evaluation and treatment of posterior cruciate ligament injuries: revisited. Am J Sports Med. 2004;32(7):1765-1775. [DOI] [PubMed] [Google Scholar]
- 2.McAllister DR Petrigliano FA. Diagnosis and treatment of posterior cruciate ligament injuries. Curr Sports Med Rep. 2007;6(5):293-299. [PubMed] [Google Scholar]
- 3.Schulz MS Russe K Weiler A Eichhorn HJ Strobel MJ. Epidemiology of posterior cruciate ligament injuries. Arch Orthop Trauma Surg. 2003;123(4):186-191. [DOI] [PubMed] [Google Scholar]
- 4.Shelbourne KD Davis TJ Patel DV. The natural history of acute, isolated, nonoperatively treated posterior cruciate ligament injuries. A prospective study. Am J Sports Med. 1999;27(3):276-283. [DOI] [PubMed] [Google Scholar]
- 5.Bedi A Musahl V Cowan JB. Management of Posterior Cruciate Ligament Injuries: An Evidence-Based Review. J Am Acad Orthop Surg. 2016;24(5):277-289. [DOI] [PubMed] [Google Scholar]
- 6.Chahla J Nitri M Civitarese D Dean CS Moulton SG LaPrade RF. Anatomic Double-Bundle Posterior Cruciate Ligament Reconstruction. Arthroscopy Techniques. 2016;5(1):e149-e156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Montgomery SR Johnson JS McAllister DR Petrigliano FA. Surgical management of PCL injuries: indications, techniques, and outcomes. Curr Rev Musculoskelet Med. 2013;6(2):115-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fanelli GC. Posterior cruciate ligament injuries in trauma patients. Arthroscopy. 1993;9(3):291-294. [DOI] [PubMed] [Google Scholar]
- 9.Fanelli GC Edson CJ. Posterior cruciate ligament injuries in trauma patients: Part II. Arthroscopy. 1995;11(5):526-529. [DOI] [PubMed] [Google Scholar]
- 10.Owesen C Sivertsen EA Engebretsen L Granan LP Årøen A. Patients with isolated PCL injuries improve from surgery as much as patients with ACL injuries after 2 years. Orthop J Sports Med. 2015;3(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hammoud S Reinhardt KR Marx RG. Outcomes of posterior cruciate ligament treatment: a review of the evidence. Sports Med Arthrosc. 2010;18(4):280-291. [DOI] [PubMed] [Google Scholar]
- 12.Johnson D. Posterior cruciate ligament: A literature review. Curr Orthop Pract. 2010;21(1):27-31. [Google Scholar]
- 13.Escamilla RF Macleod TD Wilk KE Paulos L Andrews JR. Cruciate ligament loading during common knee rehabilitation exercises. J Eng Med. 2012;226(9):670-680. [DOI] [PubMed] [Google Scholar]
- 14.Rigby JM Porter KM. Posterior cruciate ligament injuries. Trauma. 2010;12(3):175-181. [Google Scholar]
- 15.LaPrade CM Civitarese DM Rasmussen MT LaPrade RF. Emerging updates on the posterior cruciate ligament: A review of the current literature. Am J Sports Med. 2015;43(12):3077-3092. [DOI] [PubMed] [Google Scholar]
- 16.Fanelli GC Beck JD Edson CJ. Current concepts review: the posterior cruciate ligament. J Knee Surg. 2010;23(2):61-72. [DOI] [PubMed] [Google Scholar]
- 17.Goudie EB Will EM Keating JF. Functional outcome following PCL and complex knee ligament reconstruction. The Knee. 2010;17(3):230-234. [DOI] [PubMed] [Google Scholar]
- 18.Kim JG Lee YS Yang BS Oh SJ Yang SJ. Rehabilitation after posterior cruciate ligament reconstruction: A review of the literature and theoretical support. Arch OrthopTraumatol Surg. 2013;133(12):1687-1695. [DOI] [PubMed] [Google Scholar]
- 19.Pierce CM O'Brien L Griffin LW Laprade RF. Posterior cruciate ligament tears: functional and postoperative rehabilitation. Knee Surg Sports Traumatol Arthrosc. 2013;21(5):1071-1084. [DOI] [PubMed] [Google Scholar]
- 20.Accadbled F Knorr J Sales de Gauzy J. All inside transtibial arthroscopic posterior cruciate ligament reconstruction in skeletally immature: surgical technique and a case report. Orthop Traumatol Surg Res. 2013;99(3):361-365. [DOI] [PubMed] [Google Scholar]
- 21.Cavanaugh JT Saldivar A Marx RG. Postoperative rehabilitation after posterior cruciate ligament reconstruction and combined posterior cruciate ligament reconstruction-posterior lateral corner surgery. Oper Tech Sports Med. 2015;23(4):372-384. [Google Scholar]
- 22.Chen B Gao S. Double-bundle posterior cruciate ligament reconstruction using a non-hardware suspension fixation technique and 8 strands of autogenous hamstring tendons. Arthroscopy. 2009;25(7):777-782. [DOI] [PubMed] [Google Scholar]
- 23.Chuang TY Ho WP Chen CH Shieh MH Liau JJ Huang CH. Non-hardware posterior cruciate ligament reconstruction using knot/press-fit technique with periosteum-enveloped hamstrings tendon autograft. Am J Sports Med. 2011;39(5):1081-1089. [DOI] [PubMed] [Google Scholar]
- 24.Fanelli GC. Posterior cruciate ligament rehabilitation: how slow should we go? Arthroscopy. 2008;24(2):234-235. [DOI] [PubMed] [Google Scholar]
- 25.Fanelli GC. Arthroscopic transtibial tunnel posterior cruciate ligament reconstruction. Oper Tech Sports Med. 2015;23(4):289-297. [Google Scholar]
- 26.Fanelli GC Beck JD Edson CJ. Double bundle posterior cruciate ligament reconstruction: Surgical technique and results. Sports Med Arthrosc Rev. 2010;18(4):242-248. [DOI] [PubMed] [Google Scholar]
- 27.Fanelli GC Boyd JL Heckler MW. How I Manage Posterior Cruciate Ligament Injuries. Oper Techn Sports Med. 2009;17(3):175-193. [Google Scholar]
- 28.Fanelli GC Edson CJ Reinheimer KN Garofalo R. Posterior cruciate ligament and posterolateral corner reconstruction. Sports Med Arthrosc Rev. 2007;15(4):168-175. [DOI] [PubMed] [Google Scholar]
- 29.Garofalo R Jolles BM Moretti B Siegrist O. Double-bundle transtibial posterior cruciate ligament reconstruction with a tendon-patellar bone-semitendinosus tendon autograft: clinical results with a minimum of 2 years' follow-up. Arthroscopy. 2006;22(12):1331-1338 e1331. [DOI] [PubMed] [Google Scholar]
- 30.Giombini A Ciatti R Di Cesare A Tranquilli C. Rehabilitation after posterior cruciate ligament surgery. Medicina dello Sport. 2007;60(4):531-545. [Google Scholar]
- 31.Hermans S Corten K Bellemans J. Long-term results of isolated anterolateral bundle reconstructions of the posterior cruciate ligament: a 6- to 12-year follow-up study. Am J Sports Med. 2009;37(8):1499-1507. [DOI] [PubMed] [Google Scholar]
- 32.Huang JM Wang Q Shen F Wang ZM Kang YF. Cruciate ligament reconstruction using LARS artificial ligament under arthroscopy: 81 Cases report. Chinese Med J. 2010;123(2):160-164. [PubMed] [Google Scholar]
- 33.Johnson D. Posterior Cruciate Ligament Injuries: My Approach. Oper Techn Sports Med. 2009;17(3):167-174. [Google Scholar]
- 34.Kim SJ Kim TE Jo SB Kung YP. Comparison of the clinical results of three posterior cruciate ligament reconstruction techniques. J Bone Joint Surg Am. 2009;91(11):2543-2549. [DOI] [PubMed] [Google Scholar]
- 35.Lee YS Jung YB. Posterior cruciate ligament: Focus on conflicting issues. Clin Orthop Surg. 2013;5(4):256-262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li B Shen P Wang JS Wang G He M Bai L. Therapeutic effects of tibial support braces on posterior stability after posterior cruciate ligament reconstruction with autogenous hamstring tendon graft. Eur J Phys Rehabil Med. 2015;51(2):163-170. [PubMed] [Google Scholar]
- 37.Lim BO Shin HS Lee YS. Biomechanical comparison of rotational activities between anterior cruciate ligament- and posterior cruciate ligament-reconstructed patients. Knee Surg Sports Traumatol Arthrosc. 2015;23(4):1231-1238. [DOI] [PubMed] [Google Scholar]
- 38.Lim HC Bae JH Wang JH, et al. Double-bundle PCL reconstruction using tibial double cross-pin fixation. Knee Surg Sports Traumatol Arthrosc. 2010;18(1):117-122. [DOI] [PubMed] [Google Scholar]
- 39.MacGillivray JD Stein BE Park M Allen AA Wickiewicz TL Warren RF. Comparison of tibial inlay versus transtibial techniques for isolated posterior cruciate ligament reconstruction: minimum 2-year follow-up. Arthroscopy. 2006;22(3):320-328. [DOI] [PubMed] [Google Scholar]
- 40.Maruyama Y Shitoto K Baba T Kaneko K. Evaluation of the clinical results of posterior cruciate ligament reconstruction -a comparison between the use of the bone tendon bone and semitendinosus and gracilis tendons. Sports Med Arthrosc Rehab Ther Technol. 2012;4(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Marx RG Shindle MK Warren RF. Management of posterior cruciate ligament injuries. Op Techn Sports Med. 2009;17(3):162-166. [Google Scholar]
- 42.Quelard B Sonnery-Cottet B Zayni R, et al. Isolated posterior cruciate ligament reconstruction: Is non-aggressive rehabilitation the right protocol? Orthop Traumatol Surg Res. 2010;96(3):256-262. [DOI] [PubMed] [Google Scholar]
- 43.Ranalletta A Ranalletta M Suarez F Tanoira I Rossi W. Arthroscopic single-bundle posterior cruciate ligament reconstruction. Techn in Knee Surg. 2010;9(4):216-224. [Google Scholar]
- 44.Seon JK Song EK. Reconstruction of isolated posterior cruciate ligament injuries: a clinical comparison of the transtibial and tibial inlay techniques. Arthroscopy. 2006;22(1):27-32. [DOI] [PubMed] [Google Scholar]
- 45.Spiridonov SI Slinkard NJ LaPrade RF. Isolated and combined grade-III posterior cruciate ligament tears treated with double-bundle reconstruction with use of endoscopically placed femoral tunnels and grafts: Operative technique and clinical outcomes. J Bone Joint Surg Am. 2011;93(19):1773-1780. [DOI] [PubMed] [Google Scholar]
- 46.Stannard JP McKean RM. Anatomic PCL reconstruction: the double bundle inlay technique. Op Tech Sports Med. 2009;17(3):148-155. [Google Scholar]
- 47.Taylor ED Miller MD. Posterior cruciate ligament injuries: the university of virginia experience. Op Techn Sports Med. 2009;17(3):135-140. [Google Scholar]
- 48.Wong T Wang CJ Weng LH, et al. Functional outcomes of arthroscopic posterior cruciate ligament reconstruction: Comparison of anteromedial and anterolateral trans-tibia approach. Arch Orthop Trauma Surg. 2009;129(3):315-321. [DOI] [PubMed] [Google Scholar]
- 49.Wu CH Chen AC Yuan LJ, et al. Arthroscopic reconstruction of the posterior cruciate ligament by using a quadriceps tendon autograft: a minimum 5-year follow-up. Arthroscopy. 2007;23(4):420-427. [DOI] [PubMed] [Google Scholar]
- 50.Xu X Huang T Liu Z, et al. Hamstring tendon autograft versus LARS artificial ligament for arthroscopic posterior cruciate ligament reconstruction in a long-term follow-up. Arch Orthop Trauma Surg. 2014;134(2):1753-1759. [DOI] [PubMed] [Google Scholar]
- 51.Eguchi A Adachi N Nakamae A Usman MA Deie M Ochi M. Proprioceptive function after isolated single-bundle posterior cruciate ligament reconstruction with remnant preservation for chronic posterior cruciate ligament injuries. Orthop Traumatol Surg and Res. 2014;100(3):303-308. [DOI] [PubMed] [Google Scholar]
- 52.Gill TJt Van de Velde SK Carroll KM Robertson WJ Heyworth BE. Surgical technique: aperture fixation in PCL reconstruction: applying biomechanics to surgery. Clin Orthop Relat Res. 2012;470(3):853-860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Adler GG. All-inside posterior cruciate ligament reconstruction with a graftlink. Arthroscopy Techniques. 2013;2(2):e111-e115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Deie M Adachi N Nakamae A Takazawa K Ochi M. Evaluation of single-bundle versus double-bundle PCL reconstructions with more than 10-year follow-up. Sci World J. 2015;2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Puh U Majcen N Hlebš S Rugelj D. Effects of Wii balance board exercises on balance after posterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2014;22(5):1124-1130. [DOI] [PubMed] [Google Scholar]
- 56.Tornese D Bandi M Volpi P, et al. Patellar tendon graft vs. Semitendinosus and Gracilis graft for posterior cruciate ligament reconstruction: An isokinetic and functional study one year after the operation. Isokin Ex Sci. 2008;16(2):133-137. [Google Scholar]
- 57.Zayni R Hager JP Archbold P, et al. Activity level recovery after arthroscopic PCL reconstruction: a series of 21 patients with a mean follow-up of 29 months. The Knee. 2011;18(6):392-395. [DOI] [PubMed] [Google Scholar]
- 58.Zhao J Huangfu X. Arthroscopic single-bundle posterior cruciate ligament reconstruction: Retrospective review of 4- versus 7-strand hamstring tendon graft. The Knee. 2007;14(4):301-305. [DOI] [PubMed] [Google Scholar]
- 59.Zhao J Xiaoqiao H He Y Yang X Liu C Lu Z. Sandwich-style posterior cruciate ligament reconstruction. Arthroscopy. 2008;24(6):650-659. [DOI] [PubMed] [Google Scholar]
- 60.Bovid KM Salata MJ Vander Have KL Sekiya JK. Arthroscopic posterior cruciate ligament reconstruction in a skeletally immature patient: A new technique with case report. J Arthrosc Rel Surg. 2010;26(4):563-570. [DOI] [PubMed] [Google Scholar]
- 61.Kruse LM Gray B Wright RW. Rehabilitation after anterior cruciate ligament reconstruction: a systematic review. J Bone Joint Surgery Am. 2012;94(19):1737-1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Logerstedt DS Scalzitti D Risberg MA, et al. Knee stability and movement coordination impairments: Knee ligament sprain revision 2017. J Orthop Sports Phys Ther. 2017;47(11):A1-A47. [DOI] [PubMed] [Google Scholar]
- 63.Edson CJ Fanelli GC Beck JD. Postoperative rehabilitation of the posterior cruciate ligament. Sports Med Arthrosc Rev. 2010;18(4):275-279. [DOI] [PubMed] [Google Scholar]
- 64.Mook WR Civitarese D Turnbull TL, et al. Double-bundle posterior cruciate ligament reconstruction: a biomechanical analysis of simulated early motion and partial and full weightbearing on common reconstruction grafts. Knee Surg Sports Traumatol Arthrosc. 2016. [DOI] [PubMed] [Google Scholar]
- 65.Papannagari R DeFrate LE Nha KW, et al. Function of posterior cruciate ligament bundles during in vivo knee flexion. Am J Sports Med. 2007;35(9):1507-1512. [DOI] [PubMed] [Google Scholar]
- 66.DeFrate LE Gill TJ Li G. In vivo function of the posterior cruciate ligament during weightbearing knee flexion. Am J Sports Med. 2004;32(8):1923-1928. [DOI] [PubMed] [Google Scholar]
- 67.Noyes FR Mangine RE Barber S. Early knee motion after open and arthroscopic anterior cruciate ligament reconstruction. Am J Sports Med. 1987;15(2):149-160. [DOI] [PubMed] [Google Scholar]
- 68.Logerstedt DS Snyder-Mackler L Ritter RC Axe MJ Godges JJ, Orthopaedic section of the american physical therapist association. Knee stability and movement coordination impairments: knee ligament sprain. J Orthop Sports Phys Ther. 2010;40(4):A1-A37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Palmieri-Smith RM Thomas AC Wojtys EM. Maximizing quadriceps strength after ACL reconstruction. Clin Sports Med. 2008;27(3):405-424, vii-ix. [DOI] [PubMed] [Google Scholar]
- 70.Kyritsis P Bahr R Landreau P Miladi R Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50(15):946-951. [DOI] [PubMed] [Google Scholar]
- 71.Toutoungi DE Lu TW Leardini A Catani F O'Connor JJ. Cruciate ligament forces in the human knee during rehabilitation exercises. Clinical biomechanics (Bristol, Avon). 2000;15(3):176-187. [DOI] [PubMed] [Google Scholar]
- 72.Thomas AC McLean SG Palmieri-Smith RM. Quadriceps and hamstrings fatigue alters hip and knee mechanics. J Appl Biomech. 2010;26(2):159-170. [DOI] [PubMed] [Google Scholar]
- 73.Hirokawa S Solomonow M Lu Y Lou ZP D'Ambrosia R. Anterior-posterior and rotational displacement of the tibia elicited by quadriceps contraction. Am J Sports Med. 1992;20(3):299-306. [DOI] [PubMed] [Google Scholar]
- 74.Hoher J Vogrin TM Woo SL Carlin GJ Aroen A Harner CD. In situ forces in the human posterior cruciate ligament in response to muscle loads: a cadaveric study. J Orthop Res. 1999;17(5):763-768. [DOI] [PubMed] [Google Scholar]
- 75.Otzel DM Chow JW Tillman MD. Long-term deficits in quadriceps strength and activation following anterior cruciate ligament reconstruction. Phys Ther Sport. 2015;16(1):22-28. [DOI] [PubMed] [Google Scholar]
- 76.Markolf KL O'Neill G Jackson SR McAllister DR. Effects of applied quadriceps and hamstrings muscle loads on forces in the anterior and posterior cruciate ligaments. Am J Sports Med. 2004;32(5):1144-1149. [DOI] [PubMed] [Google Scholar]
- 77.Adams D Logerstedt DS Hunter-Giordano A Axe MJ Snyder-Mackler L. Current concepts for anterior cruciate ligament reconstruction: a criterion-based rehabilitation progression. J Orthop Sports Phys Ther. 2012;42(7):601-614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Greenberg EM Albaugh J Ganley TJ Lawrence JT. Rehabilitation considerations for all epiphyseal acl reconstruction. Int J Sports Phys Ther. 2012;7(2):185-196. [PMC free article] [PubMed] [Google Scholar]
- 79.Joreitz R Lynch A Rabuck S Lynch B Davin S Irrgang J. Patient-specific and surgery-specific factors that affect return to sport after ACL reconstruction. Int J Sports Phys Ther. 2016;11(2):264-278. [PMC free article] [PubMed] [Google Scholar]
- 80.Yellin JL Fabricant PD Gornitzky A, et al. Rehabilitation following anterior cruciate ligament tears in children: A systematic review. J Bone Joint Surg Rev. 2016;4(1). [DOI] [PubMed] [Google Scholar]
- 81.Lepley LK Palmieri-Smith RM. Quadriceps strength, muscle activation failure, and patient-reported function at the time of return to activity in patients following anterior cruciate ligament reconstruction: A cross-sectional study. J Orthop Sports Phys Ther. 2015;45(12):1017-1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Grindem H Snyder-Mackler L Moksnes H Engebretsen L Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50(13):804-808. [DOI] [PMC free article] [PubMed] [Google Scholar]