Abstract
Background
With the increasing number of individuals participating in sports every year, injury - specifically anterior cruciate ligament (ACL) injury - remains an inherent risk factor for participants. The majority of ACL injuries occur from a non-contact mechanism, and there is a high physical and financial burden associated with injury. Understanding the risk factors for ACL injury may aid in the development of prevention efforts.
Purpose
The purpose of this review was to synthesize and appraise existing literature for risk factors associated with non-contact anterior cruciate ligament (ACL) injury in both sexes.
Study Design
Systematic review.
Methods
An electronic literature search was conducted utilizing the MEDLINE database and The Cochrane library for articles available through February 2016. All titles and abstracts were reviewed and full text articles meeting eligibility criteria were assessed in detail to determine inclusion or exclusion. Articles reviewed in full text were reviewed for scientific evidence of risk factors for ACL injury. Results from studies were extracted and initially classified as either intrinsic or extrinsic risk factors, and then further categorized based upon the evidence presented in the studies meeting inclusion criteria. Data extracted from eligible studies included general study characteristics (study design, sample characteristics), methodology, and results for risk factors included.
Results
Principal findings of this systematic review identified the following risk factors for ACL injury in both sexes: degrading weather conditions, decreased intercondylar notch index or width, increased lateral or posterior tibial plateau slope, decreased core and hip strength, and potential genetic influence.
Conclusions
Neuromuscular and biomechanical risk factors may be addressed through neuromuscular preventative training programs. Though some extrinsic and other inherent physiological factors tend to be non-modifiable, attempts to improve upon those modifiable factors may lead to a decreased incidence of ACL injury.
Level of Evidence
2a.
Keywords: anterior cruciate ligament, ACL, risk factor, injury, rupture.
INTRODUCTION
Over 212 million individuals worldwide participate in competitive or leisure time sports activities.1 There is an inherent risk of injury for sport participants, due to the nature of competition and the physiological requirements placed on the body.2-4 While contact may play a factor, over 70% of anterior cruciate ligament (ACL) injuries occur with a non-contact mechanism,5-7 with an estimated 100,000 Injuries per year within the National Collegiate Athletic Association (NCAA) alone.8 A review of ACL injuries from the NCAA revealed that the highest rate of injury in men occurred in football (0.17 per 1000 Athlete-Exposures [A-E]), while for women, basketball and lacrosse show the highest rate of injury (0.23 per 1000 A-E).9 Surgical reconstruction stands as the most common treatment option for complete ACL rupture.10 The cost of ACL injury comes in the form of lost participation time as well as monetary cost of reconstructive surgery. The cost of a reconstructive ACL surgery averages $12,740,10 with lifetime societal costs (e.g. disability, decreased productivity) upwards of $38,000.11
Due to the high individual and societal costs associated with ACL injury, and the catastrophic impact to an individual's quality of life, prevention of this condition should continue to be a primary concern. Prevention begins with an understanding of risk factors associated with ACL injury. Risk factors that predispose an individual for injury are categorized as intrinsic or extrinsic. Intrinsic factors, those inherent to the individual, are further subdivided as either modifiable or non-modifiable. Modifiable risk factors are those that may be altered in the individual (e.g. muscular strength or flexibility). Non-modifiable risk factors include those which are intrinsic and cannot be controlled by the individual (e.g. anatomical structure).12 Extrinsic risk factors are those that are outside of the control of the individual (e.g. playing surface). Due to extrinsic and non-modifiable intrinsic factors, the risk of ACL injury will always exist. The opportunity to reduce the prevalence of ACL injury may be achieved by employing preventative measures derived from the knowledge of modifiable risk factors.13,14 Currently, preventative programs have shown promise for the reduction of ACL injury risk in sport.13,14 Previously, systematic reviews have addressed the risk factors associated with only one sex,15,16 with insignificant cross comparison. Aggregating the current literature of risk factors for ACL injury for both sexes provides the unique opportunity to address factors across the population, and to identify those that require more individualistic approaches. Therefore, the purpose of this systematic review was to synthesize and appraise existing literature for risk factors associated with non-contact ACL injury in both sexes.
METHODOLOGY
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement for systematic reviews was utilized for reporting in this study.17 Initial criterion for inclusion in this review was observational, prospective, or retrospective human studies which investigated risk factors for injury to the ACL. Additional inclusion criteria included those written in the English language and those with a level of evidence between I and IV.18 Studies that did not utilize non-contact ACL injury as an outcome or did not use ACL injured participants were excluded. Studies identifying secondary or tertiary factors related to ACL injury were excluded. Both diagnostic and therapeutic studies were excluded; i.e. studies investigating roles of preventative interventions investigating potential risk reduction. Studies that did not present significant findings of association of risk from potential factors were excluded. Previous systematic review, meta-analyses, and review articles were excluded. Studies not written in the English language were excluded, and there were no population restrictions utilized during the search.
Data Sources
An electronic literature search was conducted utilizing the MEDLINE database and The Cochrane library for all articles available through February 2016. The literature search was conducted utilizing search strategies (inclusion & exclusion) and keywords modeled from prior systematic reviews, and these are summarized in Table 1.15
Table 1.
Systematic search strategies and keywords.
| Database | Search | Keywords |
|---|---|---|
| Pubmed | 1 | (risk) OR risk of |
| 2 | (injury OR injuries OR tear OR tears OR tearing OR rupture OR rupture OR sprain OR sprains) | |
| 3 | (anterior cruciate ligament or ACL) | |
| 4 | (((((prospective) OR randomized controlled trial) OR cohort) OR Case control) OR case-control) OR longitudinal | |
| 5 | #1 AND #2 AND #3 AND #4 | |
| 6 | reconstruction | |
| 7 | #5 NOT #6 | |
| 8 | (animals) NOT (animals AND humans) | |
| 9 | #7 NOT #8 | |
| 10 | ((editorial) OR letter) OR comment) | |
| 11 | #9 NOT #10 | |
| 12 | #9 NOT #10: Filters: English | |
| Cochrane | 1 | (risk) OR risk of |
| 2 | MeSH descriptor: [Anterior Cruciate Ligament] explode all trees | |
| 3 | anterior cruciate ligament OR ACL (word variations have been searched) | |
| 4 | #2 or #3 | |
| 5 | MeSH descriptor: [Wounds and Injuries] explode all trees | |
| 6 | injuries OR injury OR tear OR tears OR tearing OR rupture OR ruptures OR sprain OR sprains (word variations have been searched) | |
| 7 | #5 or #6 | |
| 8 | prospective OR randomized controlled trial OR cohort OR case control OR case-control (word variations have been searched) | |
| 10 | animals NOT (animals AND humans) | |
| 11 | editorial OR letter OR comment | |
| 12 | #1 AND #4 AND #7 AND #8 NOT #10 NOT #11 |
Study Selection & Data Extraction
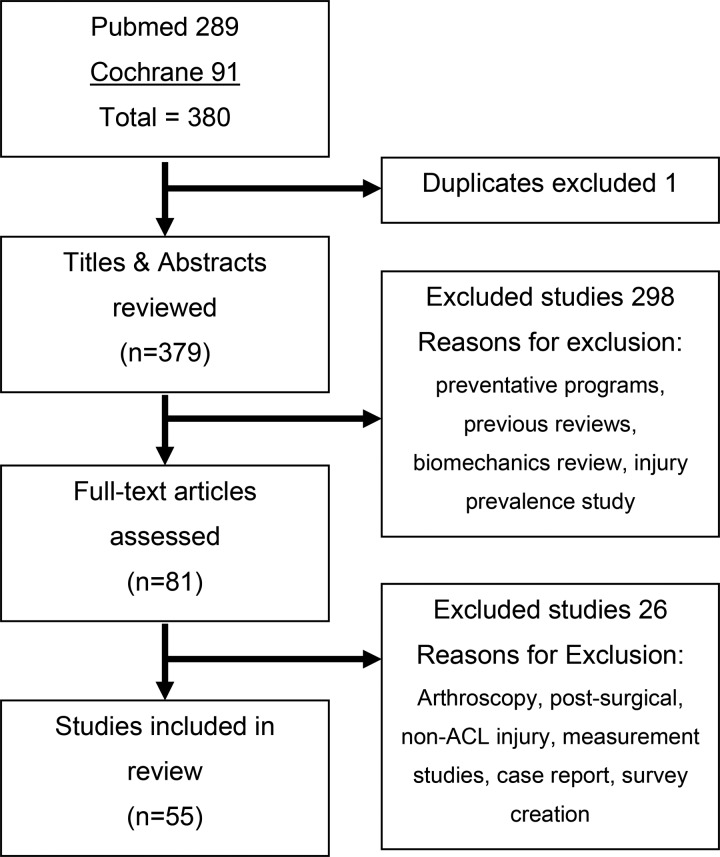
All titles and abstracts were reviewed and full text articles meeting eligibility criteria were assessed in detail to determine inclusion or exclusion. Abstracts and articles were reviewed for inclusion by two authors, and upon any discrepancies, a third author would provide a ruling. The search of the literature resulted in a total of 381 references; of which one was a duplicate and another 301 studies were excluded (Figure 1). A total of 79 full text articles were reviewed, 55 of which met criteria for inclusion and were subsequently incorporated. Articles reviewed in full text were reviewed for the presence of inclusion criteria, specifically for scientific evidence of risk factors for potential ACL injury. Results from studies were extracted and initially classified as either intrinsic or extrinsic risk factors. Extrinsic risk factors were further categorized in to weather, playing surface, sport level, ski type, and participation level. Intrinsic risk factors were labeled as anatomical, neuromuscular, biomechanical, physiologic, and genetic.15 Data extracted from eligible studies included general study characteristics (study design, sample characteristics), methodology, and results for risk factors included.
Figure 1.
PRISMA Diagram.
Assessment of quality
Assessment of risk of bias for the studies included was performed utilizing previously established criteria from Alentorn-Geli et al. (Table 2).15 A quality score was assigned for each study included, utilizing each ‘yes’ as one point toward the studies score and other responses receiving no points.15 Higher quality scores indicated studies with a greater methodological rigor.
Table 2.
Assessment of risk of bias.
| Author | A | B | C | D | E | F | G | H | I | J | K | L | M | No | Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Alentorn-Geli 201553 | No | No | Yes | U | No | No | U | No | U | U | U | U | U | Yes | 2 |
| Beynnon 200660 | No | No | Yes | No | No | No | Yes | U | U | U | No | U | NA | Yes | 3 |
| Beynnon 2014a35 | No | U | U | No | U | U | Yes | Yes | U | U | No | U | U | Yes | 3 |
| Beynnon 2014b42 | No | No | Yes | U | No | U | U | Yes | U | U | Yes | Yes | U | No | 4 |
| Beynnon 2014c24 | No | No | U | No | No | No | U | Yes | No | U | No | U | NA | U | 1 |
| Bisson 201034 | No | U | U | No | U | U | Yes | Yes | U | U | U | U | U | Yes | 3 |
| Chaudhari 200948 | No | U | Yes | U | U | U | U | Yes | U | NA | No | NA | NA | Yes | 3 |
| Dare 201541 | No | U | U | Yes | U | U | U | Yes | U | U | No | U | No | Yes | 3 |
| Everhart 201029 | No | No | Yes | No | U | Yes | Yes | Yes | No | U | No | U | NA | U | 4 |
| Fernández-Jaén 201528 | No | No | Yes | U | No | No | U | No | U | U | No | U | NA | Yes | 2 |
| Flynn 200571 | No | No | U | U | No | No | No | No | No | U | No | U | NA | No | 0 |
| Hägglund 201659 | Yes | U | U | U | U | U | No | Yes | No | U | No | U | NA | Yes | 3 |
| Hewett 200555 | Yes | U | Yes | U | U | U | U | No | U | U | No | U | U | Yes | 3 |
| Khayambashi 201651 | Yes | U | No | U | U | U | Yes | Yes | U | U | Yes | Yes | U | No | 5 |
| Khoschnau 200863 | No | No | U | U | U | No | U | No | U | U | No | U | NA | Yes | 1 |
| Kramer 200745 | Yes | No | Yes | No | Yes | Yes | No | No | No | NA | NA | Yes | NA | Yes | 6 |
| LaPrade 199426 | Yes | U | U | No | U | U | U | No | U | U | No | U | U | Yes | 2 |
| Lefevre 201361 | No | U | No | U | U | U | U | U | No | U | No | U | U | No | 0 |
| Lund-Hanssen 199431 | No | U | U | U | U | U | U | No | U | U | No | U | NA | Yes | 1 |
| Mannion 201469 | No | U | U | U | U | U | U | Yes | No | U | No | U | U | Yes | 2 |
| Myer 200952 | Yes | U | Yes | No | U | U | U | Yes | U | U | No | U | NA | U | 3 |
| Myer 201557 | Yes | U | No | U | U | U | U | No | U | U | No | U | NA | U | 1 |
| Nilstad 201469 | Yes | No | No | U | U | U | No | Yes | No | U | No | U | NA | No | 2 |
| O'Connell 201567 | No | U | U | U | U | U | U | No | U | U | No | U | U | Yes | 1 |
| Orchard 199919 | U | No | U | U | U | U | U | No | No | U | No | U | NA | U | 0 |
| Orchard 200520 | No | No | U | U | U | U | U | Yes | No | U | No | U | NA | U | 1 |
| Parkkari 200823 | Yes | U | NA | NA | U | U | Yes | No | No | Yes | No | U | NA | U | 3 |
| Pope 200222 | Yes | U | U | U | No | U | U | No | U | NA | No | U | U | Yes | 2 |
| Posthumus 2009a65 | No | U | No | No | U | U | U | No | No | NA | No | NA | NA | Yes | 1 |
| Posthumus 201066 | No | No | Yes | No | No | No | No | No | U | U | No | U | NA | Yes | 2 |
| Posthumus 2009b64 | No | No | Yes | U | No | No | No | Yes | U | U | No | U | NA | U | 2 |
| Posthumus 201268 | No | No | Yes | No | No | No | No | Yes | U | U | No | U | NA | Yes | 3 |
| Quatman 201156 | Yes | U | U | U | No | No | U | No | U | NA | No | NA | NA | Yes | 2 |
| Raschner 201249 | No | U | U | No | U | U | No | U | U | U | No | U | NA | U | 0 |
| Ruedl 200962 | No | U | Yes | U | U | U | No | Yes | U | U | No | U | U | No | 2 |
| Ruedl 201121 | No | No | No | U | U | U | U | No | No | U | No | U | U | Yes | 1 |
| Ruedl 201272 | No | No | No | No | No | No | U | Yes | No | NA | NA | NA | NA | Yes | 2 |
| Saper 201644 | No | U | U | No | U | U | U | Yes | No | U | No | NA | NA | Yes | 2 |
| Shaw 201533 | No | U | U | U | U | U | U | Yes | U | U | No | U | NA | Yes | 2 |
| Simon 201032 | No | U | U | U | U | U | U | Yes | U | NA | No | NA | NA | Yes | 2 |
| Souryal 199325 | Yes | No | U | NA | U | Yes | Yes | Yes | No | U | No | Yes | Yes | No | 6 |
| Stijak 201446 | No | No | U | U | U | U | U | Yes | U | U | No | U | NA | Yes | 2 |
| Sturnick 2014a36 | U | U | U | U | U | U | Yes | Yes | U | NA | No | NA | NA | U | 2 |
| Sturnick 2014b37 | Yes | U | U | U | U | U | U | Yes | U | U | No | U | NA | Yes | 3 |
| Sturnick 201530 | No | U | U | U | No | No | U | No | U | U | No | U | U | Yes | 1 |
| Tainaka 201458 | No | No | Yes | U | Yes | U | U | Yes | U | U | No | U | NA | U | 3 |
| Terauchi 201139 | No | No | U | U | No | No | U | Yes | U | U | No | U | NA | Yes | 2 |
| Todd 201040 | No | No | U | NA | U | No | Yes | Yes | No | U | NA | Yes | NA | U | 3 |
| Uhorchak 200312 | Yes | No | U | No | Yes | Yes | Yes | Yes | No | U | Yes | Yes | Yes | No | 8 |
| Vyas 201143 | No | No | No | U | U | U | U | No | U | U | No | U | NA | Yes | 1 |
| Whitney 201447 | No | No | U | No | No | No | U | Yes | U | U | No | U | NA | U | 1 |
| Xiao 201627 | No | U | Yes | U | U | U | Yes | No | No | U | No | U | NA | Yes | 3 |
| Zazulak 200750 | Yes | No | Yes | U | Yes | Yes | Yes | No | No | U | No | U | Yes | U | 6 |
| Zebis 200954 | Yes | No | U | No | U | U | Yes | No | U | U | No | U | No | Yes | 3 |
| Zeng 201438 | No | U | Yes | U | Yes | Yes | Yes | Yes | U | U | No | U | NA | Yes | 6 |
Column Abbreviations: A = Prospective study; B = Concealed/blind group assignment; C = Group similarities at baseline; D = participant blinding; E = data collector blinding; F = outcome assessor blinding; G = previous knee injuries excluded; H = results specified for non-contact; I = no influence of other risk factors; J = acceptable compliance; K = dropout reasons reported; L = acceptable dropout rate; M = duration of intervention comparable; N = intention to treat analysis. Yes = criteria was explained and acceptable (1 point); No = criteria missing or not acceptable (0 points); U = Unknown, criteria not explained or unclear; NA = not applicable (0 points).
RESULTS
Summary of risk of bias
In general, studies involved in this systematic review appear to have a moderate risk of bias. Of the involved studies, there was a high proportion of unreported information relating to the assessment of risk of bias and quality score.
Extrinsic Risk Factors
There were a total of 10 risk factors identified which were subsequently categorized as extrinsic: five related to weather, two to playing surface, one sport level, one ski type, and one participation level (Table 3).
Table 3.
Summary of risk factors.
| Category | Risk Factora | Sex | N | Qualityb | Studies | Risk assessment | 95% CI |
|---|---|---|---|---|---|---|---|
| Extrinsic | |||||||
| Weather conditions | During snowfall (skiing) | F | 1 | 1 (0) | Ruedl 201121 | ORc: 16.63 | 1.8-152.1 |
| Icy conditions (skiing) | F | 1 | 1 (0) | Ruedl 201121 | ORc: 24.33 | 6.8-86.5 | |
| High 28 day evaporation rate | M | 1 | 0 (0) | Orchard 199919 | RRd: 2.8 | 1.53-5.10 | |
| No rainfall during match (wet ground) | M | 1 | 1 (0) | Orchard 200520 | RRd: 1.55 | 0.46-5.19 | |
| Low previous year rainfall | M | 2 | 0.5 (0-1) | Orchard 199919 Orchard 200520 | RRd: 1.93 RRd: 1.5 | 1.13-3.34 0.97-2.32 | |
| Playing surface | Rubber matting (military obstacle course) | B | 1 | 2 (0) | Pope 200222 | - | - |
| Bermuda Grass | M | 1 | 1 (0) | Orchard 200520 | RRd: 1.87 | 1.26-2.77 | |
| Sport level | College level (compared to high school) | B | 1 | 1 (0) | Beynnon 2014c24 | RRd: 2.38 | 1.55-3.54 |
| Ski Type | Traditional skis | F | 1 | 1 (0) | Ruedl 201121 | ORc: 10.49 | 2.0-54.5 |
| Sport participation | Greater weekly sport participation (> 4 time/week) | B | 1 | 3 (0) | Parkkari 200823 | HRe: Female: 8.5 HRe: Male: 4.0 | 4.3-16.4 2.7-6.1 |
| Intrinsic | |||||||
| Anatomic | Non-dominant leg injury | F | 2 | 2.5 (2-3) | Hägglund 201656 Ruedl 201273 | - ORc: 2.0 | - 1.0-3.8 |
| Generalized join laxity | B | 2 | 7 (6-8) | Uhorchak 200312 Kramer 200745 | RRd: 2.8 - | - - |
|
| Genu Recurvatum | F | 1 | 6 (0) | Kramer 200745 | - | - | |
| Decreased ACL width | B | 1 | 2 (0) | Stijak 201446 | - | - | |
| Increased ACL length | B | 1 | 2 (0) | Stijak 201446 | - | - | |
| ACL volume (decreased) | B | 2 | 1.5 (1-3) | Chaudhari 200948 Whitney 201447 |
- ORc: 0.817 |
- 0.72-0.93 |
|
| Decreased notch width or notch width index | B | 11 | 2.9 (1-8) | Everhart 201029 Fernández-Jaén 201528 LaPrade 199426 Lund-Hanssen 199431 Shaw 201533 Simon 201032 Souryal 199325 Sturnick 201530 Uhorchak 200312 Whitney 201447 Xiao 201627 |
- ORc: 0.87 ORc: 66.0 ORc: 7.0 - - - ORc: 1.5 RRd: 3.8 ORc: 0.70 - |
-0.82-0.92 20-218 2-24 - - - - - 0.57-0.85 - |
|
| Greater alpha angle | B | 1 | 2 (0) | Fernández-Jaén 201528 | ORc: 1.049 | 1.01-1.08 | |
| Increased tibial tuberosity to trochlear groove distance | B | 1 | 2 (0) | Saper 201644 | - | - | |
| Increased medial tibial plateau depth | B | 3 | 4 (2-3) | Beynnon 2014a35 Beynnon 2014b42 Bisson 201034 |
-ORc: 1.15 - |
- 1.04-1.27 - |
|
| Increased lateral tibial plateau depth | M | 1 | 3 (0) | Bisson 201034 | - | - | |
| Anatomic | Increased lateral or posterior tibial plateau slope | B | 9 | 2.8 (1-6) | Beynnon 2014a35 Bisson 201034 Dare 201541 Simon 201032 Sturnick 2014b37 Sturnick 201530 Terauchi 201139 Todd 201040 Zeng 201438 |
- - - - ORc: Female: 1.155 ORc: 1.324 - - - |
- - - - 1.07-1.25 1.14-1.55 - - - |
| Increased femoral plateau angle | F | 1 | 2 (0) | Terauchi 201139 | - | - | |
| Increased medial tibial slope (open physis) | B | 1 | 1 (0) | Vyas 201143 | - | - | |
| Conflicting Evidence | Decreased medial tibial spine width/volume | B | 2 | 5 (2-8) | Sturnick 2014a36 Uhorchak 200312 |
ORc: Male: 1.5 - | - - |
| Increased thickness of intercondylar notch bony ridge | B | 2 | 2.5 (1-4) | Everhart 201029 Whitney 201447 |
- ORc: 1.273 | - 0.97-1.67 | |
| Lateral middle cartilage slope | B | 2 | 1.5 (1-3) | Sturnick 2014b37 Sturnick 201530 |
- Multiple | - - | |
| Neuromuscular | Decreased resistance to fatigue | M | 1 | 2 (0) | Alentorn-Geli 201554 | - | - |
| Altered EMG muscular pre-activity | F | 1 | 3 (0) | Zebis 200955 | |||
| Core stability | F | 1 | 6 (0) | Zazulak 200751 | Multiple | - | |
| Decreased knee abductor strength | B | 1 | 5 (0) | Khayambashi 201652 | ORc: 1.12 | 1.05-1.20 | |
| Decreased hip external rotation strength | B | 1 | 5 (0) | Khayambashi 201652 | ORc: 1.23 | 1.08-1.39 | |
| Decreased hamstring strength | F | 1 | 3 (0) | Myer 200952 | - | - | |
| Multi-Factor strength | B | 1 | 0 (0) | Raschner 201250 | Multiple | - | |
| Illiotibial band flexibility | F | 1 | 6 (0) | Kramer 200745 | - | - | |
| Biomechanical | Increased knee abduction moment and angle on landing | F | 2 | 2 (1-3) | Hewett 200560 Myer 201557 |
- - | - - |
| Increased knee valgus on landing | F | 2 | 2.5 (2-3) | Hewett 200560 Quatman 201161 |
- Multiple | - - | |
| Decreased hip external (ER) & internal (IR) rotation | B | 1 | 3 (0) | Tainaka 201463 | ORc: IR: 0.18 ORc: ER: 0.23 | 0.10-0.34 0.14-0.39 | |
| Physiologic | Increased BMI | F | 2 | 5.5 (3-8) | Uhorchak 200312 Hägglund 201659 |
RRd: 2.0 ORc: 2.4 | - 0.96-6.0 |
| Increased body weight | F | 1 | 8 (0) | Uhorchak 200312 | RRd: 1.9 | - | |
| Menstrual pre-ovulatory phase | F | 3 | 2 (2-3) | Beynnon 200657 Lefevre 201361 Ruedl 200959 Ruedl 201121 |
ORc: 3.22 - ORc: 2.59 ORc: 1.88 |
1.09-9.52 - 1.2-5.5 0.92-3.88 |
|
| Onset of Menarche | F | 1 | 3 (0) | Hägglund 201656 | ORc: 6.68 | 0.90-49.83 | |
| Sex | B | 2 | 1.5 (1-2) | Beynnon 2014c24 Fernández-Jaén 201528 |
RRd: Female: 2.10 ORc: Male: 2.22 |
1.34-3.27 1.47-3.33 |
|
| Age (>14) | B | 1 | 3 (0) | Hägglund 201656 | ORc: 4.59 | 1.77-11.9 | |
| Genetic | Genetic Factor(s) (e.g. COL1A1 polymorphism, COL3A1 AA genotype, GG genotype of DCN rs516115, etc.) |
B | 6 | 1.5 (1-3) | Khoschnau 200864 Mannion 201469 O'Connell 201568 Posthumus 2009a66 Posthumus 2009b65 Posthumus 201067 Posthumus 201269 |
ORc: 0.15 Multiple - ORc: 0.031 ORc: 6.6 ORc: 2.4 - |
0.0-0.68 - - <0.01-1.46 1.5-29.7 1.0-5.5 - |
| Other | Prior ACL injury | F | 1 | 2 (0) | Nilstad 201471 | ORc: 9.08 | 1.90-43.44 |
| Ankle Sprain History | F | 1 | 6 (0) | Kramer 200745 | - | - | |
| Familial predisposition (history) | F | 2 | 1.5 (0-3) | Flynn 200572 Hägglund 201656 |
- ORc: 3.57 |
- 1.0-2.97 |
|
F = female, M = male, B = both female & male, ACL = anterior cruciate ligament, N = number of studies, BMI = body mass index, EMG = electromyography
a Risk for ACL injury if factor present; b From assessment of risk of bias (Table 2), presented as Median (range); c Odds ratio; d Relative risk; e Hazard ratio
Three studies identified risk factors for ACL injury stemming from weather conditions. Two studies by Orchard et al.19,20 examined the weather conditions surrounding matches of Australian football over several years of match play. It was determined that a high evaporation rate for 28 days leading up to the match date placed individuals at a higher risk for injury (RR = 2.8).19 Both studies reported that low rainfall in the year preceding matches increased the risk of injury (RR = 1.5 to 1.93).19,20 Additionally, the absence of rainfall during matches placed those playing at a higher risk of injury (RR = 1.55).20 The last weather-related study reported female recreational skiers were at an increased risk of injury while in icy snow conditions (OR = 24.33) or while skiing during snowfall (OR = 16.63).21
Two studies identified the type of playing surface as a risk factor for injury. In 2002, Pope et al.22 found that rubber matting on a military obstacle course was correlated with the number of ACL injuries sustained in the Australian army (χ2 = 4.76).22 Orchard et al.20 found that in Australian football, individuals participating on fields with Bermuda grass are at an increased risk (RR = 1.87).20 Other risk factors included: the use of traditional skis (versus carving skis) for recreational female skiers (OR = 10.49),21 increased sport participation sessions per week (adolescents; < 3 days per week female and male Hazard Ratio = 2.0; > 4 days per week, female, male Hazard Ratio = 8.5, 4.0),23 and individuals who participated in collegiate sports were at an increased risk of injury compared to high school sport participants (RR = 2.38).24
The identified weather-related and playing surface factors are out of an individual's control, however, some of these factors (i.e. playing surface) may be modified by the overseeing organizations. The risk factor of participation level may be modified by an individual (i.e. self-regulating participation), though typically this along with sport level may be predetermined and interlinked factors. The type of ski use in recreational skier is modifiable and reliant on individual choice.
Intrinsic Risk Factors
There were a total of 37 risk intrinsic factors identified in the review of literature. The risk factors were further subdivided in to 17 anatomic, eight neuromuscular, six physiologic, three biomechanical, and one genetic. The final two risk identified factors did not align with prior categorizations (Table 3).
Anatomic Factors
In multiple studies it has been reported that individuals who sustain ACL injury have intercondylar notch stenosis or a narrow intercondylar notch as determined by notch width index.25-29 Furthermore, for each millimeter decrease in the anterior intercondylar notch width females were at an increased risk (OR = 1.5) compared to males.30 This risk factor has been reported in various populations, such as female handball players with a narrow intercondylar notch (OR = 7.0).31 In both female and male army cadets, a narrow notch width (determined by notch width index one standard deviation below the mean) (OR = 3.8) increases the risk of ACL injury.12 One study demonstrated that individuals with a narrow intercondylar notch inlet (where ACL enters intercondylar notch posteriorly) was smaller for ACL injured individuals, and this measurement alone demonstrated a positive predictive value of 70%.32 Additionally, in the pediatric population individuals who sustained ACL injury have a significantly smaller notch width index when compared to their uninjured peers.33
An increased posterior or lateral tibial slope was identified in nine studies as more prevalent in individuals with an ACL deficient knee when compared to uninjured peers.32,34-41 Two studies presented conflicting data with ACL injured individuals having either an increased (OR = 1.324)30 or decreased (OR = 1.155)37 lateral compartment middle cartilage slope. Additionally, one study specified that females with an increased lateral slope are 1.2 times as likely to sustain injury.42 Individuals who had an open lower extremity physis were categorized into the pediatric population, and in those individuals with an open physis an increased medial tibial slope has been identified as an additional risk factor.43 One study identified an increased femoral plateau angle (defined as the angle between a line tangent to the anterior femoral cortex and a line extended from the peaks of the medial tibial plateau) to be present in those female individuals who have suffered ACL injury.39 Increases of an individual's alpha angle (measured from sagittal view films, intercondylar notch roof by the long axis of femur),28 distance between their tibial tuberosity and trochlear groove,44 depth of the medial tibial plateau,33-35 depth of the lateral tibial plateau,34 and a generalize joint laxity may predispose athletes for injury to the ACL.12,45 The presence of genu recurvatum is related to a history of ACL injury, and may be a secondary factor in generalized joint laxity.45 Characteristics related directly to the ligament, a decreased width,46 decreased volume (size of ligament),47,48 and an increased length were reported to be predisposing factors for injury.46 There is also conflicting evidence regarding the bony ridge within the intercondylar notch as a risk factor. Two studies reported that a decreased medial tibial spine width or volume (OR = 1.5 for each 100mm decrease) placed individuals at increased likelihood of injury,12,36 while two other studies found an increased thickness of the bony ridge in the intercondylar notch (OR = 1.614) to increase likelihood of injury.29,47 It may be generally agreed that risk factors related to an individual's anatomical structure are non-modifiable.49
Neuromuscular Factors
Raschner et al.50 reported that a multi-factor analysis of measures of muscular strength may be critical for prevention of injury in both male and female youth ski racers.50 Furthermore, Zazulak et al.51 demonstrated that the ability to control core and trunk motion in reaction to perturbations in collegiate female athletes may predict injury.51 Other studies identified that strength deficits of the hip abductors and external rotators relative to body weight were predisposing individuals for injury (OR = 1.12).52 Specifically in female athletes, decreased hamstring strength is a predisposing factor for injury, when compared to healthy matched control males.53 The use of tensiomyography (TMG) (measurement of contractile properties of muscle) in male soccer players revealed a decreased resistance to fatigue of the hamstrings group,54 and the potential for imbalance between the hamstrings and quadriceps muscle groups may place individuals at an increased risk for ACL injury.54 Furthermore, elite female handball and soccer athletes may be at a higher risk if electromyography muscular pre-activity of their lateral hamstrings are decreased relative to the lateral quadriceps.55 Kramer, Denegar, Buckley, and Hertel revealed that decreased iliotibial band flexibility is related to a history of ACL injury,45 and may be related to altered lower extremity movement placing an individual at risk.
Physiologic Factors
A higher than average weight (RR = 1.9)12 or BMI (BMI > 19.9 kb/m2, RR = 2.0; OR = 2.4)12,56 have been reported to place individuals at a higher risk for injury. Furthermore, individuals post menarche (after the onset of menses; OR = 6.68)56 or present in the pre-ovulatory menstrual phase (OR = 2.59 to 3.22) are at increased risk.21,57-59 Sex has been identified as a risk factor, though with conflicting evidence.24,28 Fernandez-Jaen et al.28 revealed, ACL tears (mechanism unreported) occur more frequently in males (OR = 2.217; at least 18 years old; adjusted for age), while Beynnon et al.24 found, females are at a greater risk for first-time non-contact ACL injury (RR = 2.1; adjusting for sport and level of play). Finally, individuals who are younger than 14 years are at an increased risk for injury to their ACL.56
Biomechanical Factors
Individuals who present with the following biomechanical characteristics have been demonstrated to be at altered risk for ACL injury. Knee valgus on landing results in increased ground reaction forces,60 placing females at an increased risk of injury.61,62 Furthermore, Quatman et al. reported that relative to normal landing,61 various combinations of tibial movement (e.g. anterior translation + abduction, anterior translation + external rotation, etc.) resulted in an increased strain on the ACL, with combined abduction and anterior tibial translation showing the greatest tension on the ACL (4.6 times normal).61 Moreover, Tainaka et al.63 demonstrated that individuals with an increased amount of hip internal and external rotation during active range of motion relative to body weight are less likely to sustain injury compared to others(ER OR = 0.23; IR OR = 0.18).63
Genetic Factors
Seven studies investigated a potential genetic predisposition for ACL injury. Five identified that the presence of variants of collagen genes (e.g. COL1A1, COL12A1) in both sexes increase the likelihood of injury to the ACL (OR = 0.8 to 6.6).64-68 One study demonstrated that matrix metalloproteinase genes, which play an important role in tissue remodeling, may have an association with injury.69 Finally, one reported the presence or absence of polymorphisms of proteoglycan genes may predispose individuals for ACL injury (OR = 0.33 to 9.231).70
Other Factors
The following did not fit within other categories, and were reported as risk factors in the female sex. Individuals with previous ACL injury are at a higher likelihood for injury in the same knee (OR = 9.08),71 and individuals with family history of ACL injury (immediate family) are at an increased likelihood of injury (OR = 3.57).56,72 When examining female youth soccer players, there was a higher prevalence of ACL injuries in their non-dominant leg.56 Furthermore, female recreational skiers were demonstrated to be at an increased risk of injuring their non-dominant leg compared to their dominant (OR = 2.0).73
DISCUSSION
This systematic review presents a wide view of potential risk factors for ACL injury, which are both intrinsic and extrinsic in nature. The majority of the extrinsic factors identified are related to the effect weather conditions have on participants during specific sport participation or the conditions of the playing surface, which have been reported in prior reviews.15 Findings presented in this review demonstrate that both sexes may be affected by eroding conditions due to the weather and other external factors. Weather conditions related to an increase in odds of injury for women were those during recreational skiing (icy conditions and during snowfall),21 while the weather conditions for men were related to dry conditions on the pitch for Australian Football.19,20 These findings are presented by sex due to the lack of studies examining these conditions across sexes. Regarding the results of this review, the conditions of ski slopes and the rainfall for field-based participation should be considered.19-21
While there is an abundance of literature identifying intrinsic risk factors, unfortunately the majority of studies included in this review surrounded non-modifiable anatomic factors. Eleven studies reported a decreased intercondylar notch width or notch width index,12,25-33,47 and 11 others identified an increased lateral or posterior tibial plateau slope as a risk factor.30,32,34-41,43 Alentorn-Geli et al.15 reported both factors, and although they are non-modifiable, suggested that injury risk may be mitigated through the implementation of neuromuscular preventative training programs. Within anatomic risk factors, the studies reviewed have presented conflicting evidence regarding how changes in the morphometric characteristics of the bony ridge (increases/decreases in size) within the intercondylar notch affect an individual's risk of sustaining ACL injury. Future inquiry is necessary to determine whether the characteristics of this ridge are consequential.
The majority of the neuromuscular and biomechanical risk factors are presented as modifiable. Those that stand out in this review are impairments of core stability,50,51 increased knee valgus, and increased knee abduction moment and angle on landing.60-62 These risk factors may be addressed through neuromuscular preventative training programs.6,15 Decreased resistance to fatigue was a risk factor found only in males. Neuromuscular (e.g. EMG muscular pre-activity) and biomechanical (e.g. increased knee valgus on landing) factors were found predominantly in females. Decreases in strength and range of motion were risk factors present in both sexes. Myer et al. discuss that hamstring strength and hamstring to quadriceps ratio remain relatively unchanged as females mature, which may increase the likelihood of developing neuromuscular imbalances, thus potentially increasing females risk of sustaining ACL injury.53
Some physiologic factors seem to be on the non-modifiable end of the spectrum, such as the pre-ovulatory phase of the menstrual cycle,21,57,58 and the onset of menarche.56 These are viewed as non-modifiable as the individual may not have control over if or when they happen. The final risk factor that showed a high prevalence in the literature review is the potential for a genetic predisposition. There were six separate studies that demonstrated that variants of multiple collagen genes may play a role in the development of future ACL injury in both sexes.64-69 Similar to physiologic factors, an individual does not have control over their genetic makeup. However, the individual may take themselves out of participation in order to circumvent the potentially negative affect of some of these factors
Along with national sports governing bodies (i.e. NCAA, National Federation of State High School Association [NFHS]), colleges/universities and high schools play a crucial role in contributing to safety during sport participation by governing their affiliated teams and through the development of their sports venues. When adjusted for socioeconomic, health, and lifestyle variables, adolescents who participate in organized sport activities at any level more than four times per week are at higher odds of injury (female, male; Hazard Ratio = 8.5, 4.0).23 This places sport governing bodies in a key role for implementation of preventative strategies focusing on the amount of time per week individuals participate. Managing participation by maintaining adequate recovery time may be a strategy for the reduction of this risk factor, as neuromuscular fatigue may lead to a negative change in mechanics (e.g. increased valgus collapse) during landing tasks.74,75 On the development and maintenance of sporting venues, the type of grass used on fields has been shown to play a role in risk of ACL injury, specifically for men with Bermuda grass increasing their risk.20 Furthermore, for those institutions which house ski teams, the maintenance of the slopes may play a role for their conditions.21 Future research regarding eroding weather conditions and playing surface type should focus on the effects applicable to both sexes in order for more informed decisions to be made by sport governing bodies (i.e. NCAA, NFHS) and universities or high schools for decisions on cancellation of sport activities based on weather and for the development and refurbishing of sporting venues.
Limitations to this systematic review include that this report did not include a synthesis of previous systematic review findings, though attempts to encompass risk for both sexes were made. High risk of bias for included studies is a limitation, however, Table 2 provides clarification as to where the bias in each study may come from. Another limitation includes the search of only two databases for articles. Future directions for research regarding ACL injury include a clarification of conflicting evidence of risk factors and identification of specific methods for alteration of known factors.
CONCLUSION
This systematic review attempts to describe documented risk factors for ACL injury for both sexes to further preventative efforts. While there were a few male specific risk factors, and a number found in both sexes, most of the risk factors identified were present for females. The information presented herein reaffirms that injury to the ACL likely results from a plethora of underlying risk factors. While some of the factors presented in this review may be modified, there are many which an individual may not be able to control or modify. The majority of extrinsic risk factors fall in the non-modifiable category. The nature of sport itself will continue to put those who choose to participate at some level of risk to injury. It may prove beneficial to attempt to change those factors with potential for modification (i.e. field type) as those may provide a widespread reduction of exposure. Further research on modifiable factors may provide insight for the development and advancement of injury prevention programs with the aim to decrease the incidence of injury.
References
- 1.Physical Activity Council. Participation Report. 2015; http://physicalactivitycouncil.com/PDFs/current.pdf. Accessed February, 2017.
- 2.Myer GD Faigenbaum AD Ford KR Best TM Bergeron MF Hewett TE. When to initiate integrative neuromuscular training to reduce sports-related injuries and enhance health in youth? Curr Sports Med Rep. 2011;10(3):155-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Comstock RD Currie DW Pierpoint LA. Summary report national high school injury surveillance study: 2013-2014 School year. Center for Injury Research & Policy;2014.
- 4.DeHaven KE Lintner DM. Athletic injuries: comparison by age, sport, and gender. Am J Sports Med. 1986;14(3):218-224. [DOI] [PubMed] [Google Scholar]
- 5.Dragoo JL Castillo TN Braun HJ Ridley BA Kennedy AC Golish SR. Prospective correlation between serum relaxin concentration and anterior cruciate ligament tears among elite collegiate female athletes. Am J Sports Med. 2011;39(10):2175-2180. [DOI] [PubMed] [Google Scholar]
- 6.Griffin LY Agel J Albohm MJ, et al. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8(3):141-150. [DOI] [PubMed] [Google Scholar]
- 7.Wetters N Weber AE Wuerz TH Schub DL Mandelbaum BR. Mechanism of Injury and Risk Factors for Anterior Cruciate Ligament Injury. Oper Tech Sports Med. 2015. [Google Scholar]
- 8.Dragoo JL Braun HJ Durham JL Chen MR Harris AH. Incidence and risk factors for injuries to the anterior cruciate ligament in national collegiate athletic association football data from the 2004-2005 through 2008-2009 national collegiate athletic association injury surveillance system. Am J Sports Med. 2012;40(5):990-995. [DOI] [PubMed] [Google Scholar]
- 9.Agel J Klossner D. Epidemiologic review of collegiate ACL injury rates across 14 sports: National collegiate athletic association injury surveillance system data 2004-05 through 2011–12. Br J Sports Med. 2014;48(7):560-560. [Google Scholar]
- 10.Lubowitz JH Appleby D. Cost-effectiveness analysis of the most common orthopaedic surgery procedures: knee arthroscopy and knee anterior cruciate ligament reconstruction. Arthroscopy. 2011;27(10):1317-1322. [DOI] [PubMed] [Google Scholar]
- 11.Mather RC Koenig L Kocher MS, et al. Societal and economic impact of anterior cruciate ligament tears. J Bone Joint Surg Am. 2013;95(19):1751-1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Uhorchak JM Scoville CR Williams GN Arciero RA Pierre PS Taylor DC. Risk factors associated with noncontact injury of the anterior cruciate ligament a prospective four-year evaluation of 859 west point cadets. Am J Sports Med. 2003;31(6):831-842. [DOI] [PubMed] [Google Scholar]
- 13.Voskanian N. ACL Injury prevention in female athletes: review of the literature and practical considerations in implementing an ACL prevention program. Curr Rev Musculoskelet Med. 2013;6(2):158-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mandelbaum BR Silvers HJ Watanabe DS, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes 2-year follow-up. Am J Sports Med. 2005;33(7):1003-1010. [DOI] [PubMed] [Google Scholar]
- 15.Alentorn-Geli E, Mendiguchía J Samuelsson K, et al. Prevention of anterior cruciate ligament injuries in sports⊠Part I: Systematic review of risk factors in male athletes. Knee Surg Sports Traumatol Arthrosc. 2014;22(1):3-15. [DOI] [PubMed] [Google Scholar]
- 16.Hewett TE Myer GD Ford KR. Anterior cruciate ligament injuries in female athletes part 1, mechanisms and risk factors. Am J Sports Med. 2006;34(2):299-311. [DOI] [PubMed] [Google Scholar]
- 17.Moher D Liberati A Tetzlaff J Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264-269. [DOI] [PubMed] [Google Scholar]
- 18.Burns PB Rohrich RJ Chung KC. The levels of evidence and their role in evidence-based medicine. Plast Reconstr Surg. 2011;128(1):305-310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Orchard J Seward H McGivern J Hood S. Rainfall, evaporation and the risk of non-contact anterior cruciate ligament injury in the Australian Football League. Med J Aust. 1999;170(7):304-306. [DOI] [PubMed] [Google Scholar]
- 20.Orchard JW Chivers I Aldous D Bennell K Seward H. Rye grass is associated with fewer non-contact anterior cruciate ligament injuries than bermuda grass. Br J Sports Med. 2005;39(10):704-709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ruedl G Ploner P Linortner I, et al. Interaction of potential intrinsic and extrinsic risk factors in ACL injured recreational female skiers. Int J Sports Med. 2011;32(8):618-622. [DOI] [PubMed] [Google Scholar]
- 22.Pope RP. Rubber matting on an obstacle course causes anterior cruciate ligament ruptures and its removal eliminates them. Military medicine. 2002;167(4):355. [PubMed] [Google Scholar]
- 23.Parkkari J Pasanen K Mattila VM Kannus P Rimpela A. The risk for a cruciate ligament injury of the knee in adolescents and young adults: a population-based cohort study of 46 500 people with a 9 year follow-up. Br J Sports Med. 2008;42(6):422-426. [DOI] [PubMed] [Google Scholar]
- 24.Beynnon BD Vacek PM Newell MK, et al. The Effects of Level of Competition, Sport, and Sex on the Incidence of First-Time Noncontact Anterior Cruciate Ligament Injury. Am J Sports Med. 2014;42(8):1806-1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Souryal TO Freeman TR. Intercondylar notch size and anterior cruciate ligament injuries in athletes A prospective study. Am J Sports Med. 1993;21(4):535-539. [DOI] [PubMed] [Google Scholar]
- 26.LaPrade RF Burnett QM. Femoral Intercondylar Notch Stenosis and Correlation to Anterior Cruciate Ligament Injuries A Prospective Study. Am J Sports Med. 1994;22(2):198-203. [DOI] [PubMed] [Google Scholar]
- 27.Xiao WF Yang T Cui Y, et al. Risk factors for noncontact anterior cruciate ligament injury: Analysis of parameters in proximal tibia using anteroposterior radiography. J Int Med Res. 2016;44(1):157-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fernandez-Jaen T Lopez-Alcorocho JM Rodriguez-Inigo E Castellan F Hernandez JC Guillen-Garcia P. The Importance of the Intercondylar Notch in Anterior Cruciate Ligament Tears. Orthop J Sports Med. 2015;3(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Everhart JS Flanigan DC Simon RA Chaudhari AM. Association of noncontact anterior cruciate ligament injury with presence and thickness of a bony ridge on the anteromedial aspect of the femoral intercondylar notch. Am J Sports Med. 2010;38(8):1667-1673. [DOI] [PubMed] [Google Scholar]
- 30.Sturnick DR Vacek PM DeSarno MJ, et al. Combined anatomic factors predicting risk of anterior cruciate ligament injury for males and females. Am J Sports Med. 2015;43(4):839-847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lund-Hanssen H Gannon J Engebretsen L Holen KJ Anda S Vatten L. Intercondylar notch width and the risk for anterior cruciate ligament rupture: a case-control study in 46 female handball players. Acta Orthop Scand. 1994;65(5):529-532. [DOI] [PubMed] [Google Scholar]
- 32.Simon RA Everhart JS Nagaraja HN Chaudhari AM. A case-control study of anterior cruciate ligament volume, tibial plateau slopes and intercondylar notch dimensions in ACL-injured knees. J Biomech. 2010;43(9):1702-1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shaw KA Dunoski B Mardis N Pacicca D. Knee morphometric risk factors for acute anterior cruciate ligament injury in skeletally immature patients. J Child Orthop. 2015;9(2):161-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bisson LJ Gurske-DePerio J. Axial and sagittal knee geometry as a risk factor for noncontact anterior cruciate ligament tear: a case-control study. Arthroscopy. 2010;26(7):901-906. [DOI] [PubMed] [Google Scholar]
- 35.Beynnon BD Vacek PM Sturnick DR, et al. Geometric profile of the tibial plateau cartilage surface is associated with the risk of non-contact anterior cruciate ligament injury. J Orthop Res. 2014;32(1):61-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sturnick DR Argentieri EC Vacek PM, et al. A decreased volume of the medial tibial spine is associated with an increased risk of suffering an anterior cruciate ligament injury for males but not females. J Orthop Res. 2014;32(11):1451-1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sturnick DR Van Gorder R Vacek PM, et al. Tibial articular cartilage and meniscus geometries combine to influence female risk of anterior cruciate ligament injury. J Orthop Res. 2014;32(11):1487-1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zeng C Yang T Wu S, et al. Is posterior tibial slope associated with noncontact anterior cruciate ligament injury? Knee Surg Sports Traumatol Arthrosc. 2016;24(3):830-837. [DOI] [PubMed] [Google Scholar]
- 39.Terauchi M Hatayama K Yanagisawa S Saito K Takagishi K. Sagittal alignment of the knee and its relationship to noncontact anterior cruciate ligament injuries. Am J Sports Med. 2011;39(5):1090-1094. [DOI] [PubMed] [Google Scholar]
- 40.Todd MS Lalliss S Garcia E DeBerardino TM Cameron KL. The relationship between posterior tibial slope and anterior cruciate ligament injuries. Am J Sports Med. 2010;38(1):63-67. [DOI] [PubMed] [Google Scholar]
- 41.Dare DM Fabricant PD McCarthy MM, et al. Increased Lateral Tibial Slope Is a Risk Factor for Pediatric Anterior Cruciate Ligament Injury: An MRI-Based Case-Control Study of 152 Patients. Am J Sports Med. 2015;43(7):1632-1639. [DOI] [PubMed] [Google Scholar]
- 42.Beynnon BD Hall JS Sturnick DR, et al. Increased slope of the lateral tibial plateau subchondral bone is associated with greater risk of noncontact ACL injury in females but not in males: a prospective cohort study with a nested, matched case-control analysis. Am J Sports Med. 2014;42(5):1039-1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vyas S van Eck CF Vyas N Fu FH Otsuka NY. Increased medial tibial slope in teenage pediatric population with open physes and anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. 2011;19(3):372-377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Saper MG Popovich JM Jr. Fajardo R Hess S Pascotto JL Shingles M. The Relationship Between Tibial Tubercle-Trochlear Groove Distance and Noncontact Anterior Cruciate Ligament Injuries in Adolescents and Young Adults. Arthroscopy. 2016;32(1):63-68. [DOI] [PubMed] [Google Scholar]
- 45.Kramer L Denegar C Buckley W Hertel J. Factors associated with anterior cruciate ligament injury: history in female athletes. J Sports Med Phys Fitness. 2007;47(4):446. [PubMed] [Google Scholar]
- 46.Stijak L Bumbasirevic M Kadija M Stankovic G Herzog R Filipovic B. Morphometric parameters as risk factors for anterior cruciate ligament injuries: A MRI case-control study. Vojnosanit Pregl. 2014;71(3):271-276. [DOI] [PubMed] [Google Scholar]
- 47.Whitney DC Sturnick DR Vacek PM, et al. Relationship Between the Risk of Suffering a First-Time Noncontact ACL Injury and Geometry of the Femoral Notch and ACL: A Prospective Cohort Study With a Nested Case-Control Analysis. Am J Sports Med. 2014;42(8):1796-1805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chaudhari AM Zelman EA Flanigan DC Kaeding CC Nagaraja HN. Anterior cruciate ligament-injured subjects have smaller anterior cruciate ligaments than matched controls: a magnetic resonance imaging study. Am J Sports Med. 2009;37(7):1282-1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Price MJ Tuca M Cordasco FA Green DW. Nonmodifiable risk factors for anterior cruciate ligament injury. Curr Opin Pediatr. 2017;29(1):55-64. [DOI] [PubMed] [Google Scholar]
- 50.Raschner C Platzer H-P Patterson C Werner I Huber R Hildebrandt C. The relationship between ACL injuries and physical fitness in young competitive ski racers: a 10-year longitudinal study. Br J Sports Med. 2011;45:310-311. [DOI] [PubMed] [Google Scholar]
- 51.Zazulak BT Hewett TE Reeves NP Goldberg B Cholewicki J. Deficits in neuromuscular control of the trunk predict knee injury risk: a prospective biomechanical-epidemiologic study. Am J Sports Med. 2007;35(7):1123-1130. [DOI] [PubMed] [Google Scholar]
- 52.Khayambashi K Ghoddosi N Straub RK Powers CM. Hip Muscle Strength Predicts Noncontact Anterior Cruciate Ligament Injury in Male and Female Athletes: A Prospective Study. Am J Sports Med. 2016;44(2):355-361. [DOI] [PubMed] [Google Scholar]
- 53.Myer GD Ford KR Foss KDB Liu C Nick TG Hewett TE. The relationship of hamstrings and quadriceps strength to anterior cruciate ligament injury in female athletes. Clin J Sport Med. 2009;19(1):3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Alentorn-Geli E Alvarez-Diaz P Ramon S, et al. Assessment of neuromuscular risk factors for anterior cruciate ligament injury through tensiomyography in male soccer players. Knee Surg Sports Traumatol Arthrosc. 2015;23(9):2508-2513. [DOI] [PubMed] [Google Scholar]
- 55.Zebis MK Andersen LL Bencke J Kjaer M Aagaard P. Identification of athletes at future risk of anterior cruciate ligament ruptures by neuromuscular screening. Am J Sports Med. 2009;37(10):1967-1973. [DOI] [PubMed] [Google Scholar]
- 56.Hagglund M Walden M. Risk factors for acute knee injury in female youth football. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):737-746. [DOI] [PubMed] [Google Scholar]
- 57.Beynnon BD Johnson RJ Braun S, et al. The relationship between menstrual cycle phase and anterior cruciate ligament injury: a case-control study of recreational alpine skiers. Am J Sports Med. 2006;34(5):757-764. [DOI] [PubMed] [Google Scholar]
- 58.Lefevre N Bohu Y Klouche S Lecocq J Herman S. Anterior cruciate ligament tear during the menstrual cycle in female recreational skiers. Orthop Traumatol Surg Res. 2013;99(5):571-575. [DOI] [PubMed] [Google Scholar]
- 59.Ruedl G Ploner P Linortner I, et al. Are oral contraceptive use and menstrual cycle phase related to anterior cruciate ligament injury risk in female recreational skiers? Knee Surg Sports Traumatol Arthrosc. 2009;17(9):1065-1069. [DOI] [PubMed] [Google Scholar]
- 60.Hewett TE Myer GD Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492-501. [DOI] [PubMed] [Google Scholar]
- 61.Quatman CE Kiapour A Myer GD, et al. Cartilage pressure distributions provide a footprint to define female anterior cruciate ligament injury mechanisms. Am J Sports Med. 2011;39(8):1706-1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Myer GD Ford KR Di Stasi SL Foss KDB Micheli LJ Hewett TE. High knee abduction moments are common risk factors for patellofemoral pain (PFP) and anterior cruciate ligament (ACL) injury in girls: Is PFP itself a predictor for subsequent ACL injury? Br J Sports Med. 2015;49(2):118-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tainaka K Takizawa T Kobayashi H Umimura M. Limited hip rotation and non-contact anterior cruciate ligament injury: a case-control study. Knee. 2014;21(1):86-90. [DOI] [PubMed] [Google Scholar]
- 64.Khoschnau S Melhus H Jacobson A, et al. Type I collagen alpha1 Sp1 polymorphism and the risk of cruciate ligament ruptures or shoulder dislocations. Am J Sports Med. 2008;36(12):2432-2436. [DOI] [PubMed] [Google Scholar]
- 65.Posthumus M September AV O'Cuinneagain D van der Merwe W Schwellnus MP Collins M. The COL5A1 gene is associated with increased risk of anterior cruciate ligament ruptures in female participants. Am J Sports Med. 2009;37(11):2234-2240. [DOI] [PubMed] [Google Scholar]
- 66.Posthumus M September AV Keegan M, et al. Genetic risk factors for anterior cruciate ligament ruptures: COL1A1 gene variant. Br J Sports Med. 2009;43(5):352-356. [DOI] [PubMed] [Google Scholar]
- 67.Posthumus M September AV O'Cuinneagain D van der Merwe W Schwellnus MP Collins M. The association between the COL12A1 gene and anterior cruciate ligament ruptures. Br J Sports Med. 2010;44(16):1160-1165. [DOI] [PubMed] [Google Scholar]
- 68.O'Connell K Knight H Ficek K, et al. Interactions between collagen gene variants and risk of anterior cruciate ligament rupture. Eur J Sport Sci. 2015;15(4):341-350. [DOI] [PubMed] [Google Scholar]
- 69.Posthumus M Collins M van der Merwe L, et al. Matrix metalloproteinase genes on chromosome 11q22 and the risk of anterior cruciate ligament (ACL) rupture. Scand J Med Sci Sports. 2012;22(4):523-533. [DOI] [PubMed] [Google Scholar]
- 70.Mannion S Mtintsilana A Posthumus M, et al. Genes encoding proteoglycans are associated with the risk of anterior cruciate ligament ruptures. Br J Sports Med. 2014;48(22):1640-1646. [DOI] [PubMed] [Google Scholar]
- 71.Nilstad A Andersen TE Bahr R Holme I Steffen K. Risk factors for lower extremity injuries in elite female soccer players. Am J Sports Med. 2014;42(4):940-948. [DOI] [PubMed] [Google Scholar]
- 72.Flynn RK. The Familial Predisposition Toward Tearing the Anterior Cruciate Ligament: A Case Control Study. Am J Sports Med. 2005;33(1):23-28. [DOI] [PubMed] [Google Scholar]
- 73.Ruedl G Webhofer M Helle K, et al. Leg dominance is a risk factor for noncontact anterior cruciate ligament injuries in female recreational skiers. Am J Sports Med. 2012;40(6):1269-1273. [DOI] [PubMed] [Google Scholar]
- 74.Kernozek TW Torry MR Iwasaki M. Gender differences in lower extremity landing mechanics caused by neuromuscular fatigue. Am J Sports Med. 2008;36(3):554-565. [DOI] [PubMed] [Google Scholar]
- 75.Renstrom P Ljungqvist A Arendt E, et al. Non-contact ACL injuries in female athletes: an International Olympic Committee current concepts statement. Br J Sports Med. 2008;42(6):394-412. [DOI] [PMC free article] [PubMed] [Google Scholar]