Abstract
Background and purpose:
Elbow pain is common in young gymnasts and is frequently encountered by physical therapists working in direct access outpatient clinics. Most elbow pain is benign; however, non-specific symptoms can mask serious medical pathologies, as is the case with osteochondritis dissecans (OCD). OCD is a joint condition in which bone underneath the cartilage of a joint dies due to lack of blood flow. Risk factor analysis, palpable joint tenderness and swelling, joint locking, and a history of high intensity repetitive activities may inform the clinical reasoning; however, the diagnosis of OCD is best made using magnetic resonance imaging (MRI). The purpose of this case report is to describe the main components of the history and physical examination that led to OCD differential diagnosis.
Case description:
A 12-year-old female gymnast presented to an outpatient physical therapy clinic with right elbow pain following a compressive trauma. The decision was made to refer the patient for diagnostic imaging evaluation due to localized joint swelling and point tenderness over the radial head, elbow pain with compressive loading, the presence of demographic risk factors, and a recent worsening in her symptoms after a second trauma. MRI subsequently revealed OCD associated with external humeral condyle bone marrow edema. The patient underwent surgical repair.
Outcomes:
The follow-up MRI at five months post-surgically reported a “excellent graft integration”. A post-operative progressive load management program was initiated, with full return to sport achieved at 10 months after surgery.
Discussion:
This case report highlights the central role of primary care clinicians, such as physical therapists, in identifying patients with suspected pathologic conditions that may need referral for imaging, medical assessment, or surgical intervention. Physical therapists working in direct access environments should be aware of subtle signs/symptoms and specific risk factors that may be indicative of serious pathologies.
Level of evidence:
Level 4
Keywords: Adolescent gymnast, Differential diagnosis, Direct access, Elbow pain, osteochondritis dissecans, Physical therapy
BACKGROUND AND PURPOSE
Elbow pain is a common morbidity among adolescent athletes such as throwers and gymnasts.
The incidence of elbow pain may be as high as 45% in baseball players between the ages of 13 and 14.1 Generally, elbow pain during adolescence has a good prognosis; however, pain can be caused by serious conditions, as osteochondritis dissecans (OCD), requiring specialist care. It is important that physical therapists working in a direct access setting be able to identify those patients who may present with OCD.
The term OCD was used for the first time in 1888 by Koing.2 OCD refers to an acquired lesion of the subchondral bone associated with potential involvement of the overlying cartilage. OCD lesions are most common in the knee, followed by the ankle and elbow,3 with various degrees of fragmentation and sclerosis.2 In OCD lesions of the elbow, the capitellum of the humerus is typically affected. Notably, the incidence of this pathoanatomical lesion appears to be increasing rapidly.4,5 OCD lesions of the elbow can also be found in the radial head, olecranon, and trochlea.
OCD of the elbow is most common in adolescent athletes engaged in upper extremity weight-bearing and repetitive overhead or elbow extension activities—i.e. baseball, tennis, volleyball, weight lifting and gymnastics.6,7 Kida et al., found a prevalence of 3.4% of capitellar OCD lesions in 2,433 adolescent baseball players between 12 and 18 years old. Moreover, it was found that players who started competition at younger ages and played for a longer period showed an increased risk of developing capitellar OCD lesions.8
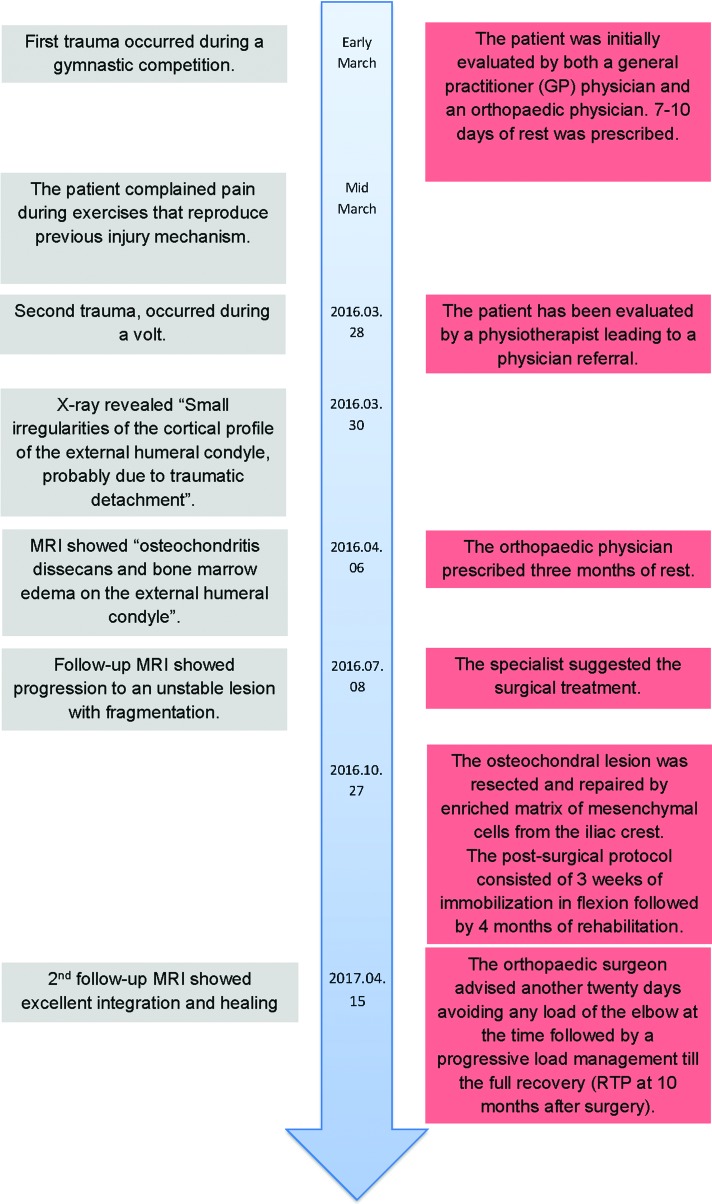
Interestingly, this condition may be asymptomatic.8 Patients with OCD are usually in their second decade of life, from 11 to 23 years old. Males are more commonly affected than females and dominant elbow capitellum is mostly typically affected.9 However, up to 20% of the patients may develop a bilateral condition.9 The etiology of this disorder is still unclear, but repetitive trauma, vascular, inflammatory, and genetic factors seem to play a role.10 In studies of identical twins, a correlation between OCD lesions and repetitive joint loading sport activities was identified.10 Furthermore, repetitive overhead throwing and loading activities generate considerable compressive forces on the radio-capitellar joint.6,11,12,13 The repetitive forces and trauma exerted on immature articular cartilage of the elbow seem to play a primary role on the etiopathogenesis.14,15 Anatomically the radio-capitellar joint is also susceptible to OCD due to the poor blood supply to the capitellum, characterized by a focal avascular zone (Figure 1), that seems to put individuals at risk for OCD lesions in this articulation.
Figure 1.
Focal avascular zone of the Radial Capitellum.
Typically, the clinical picture in adolescent male athletes includes: elbow pain, radiocapitellar joint tenderness, and swelling over the lateral aspect of the elbow.16 Physical examination findings in the early stage of OCD are non-specific, but early diagnosis is important to prevent the expansion of the lesion and the possible degeneration of the joint, especially in adolescents. Individuals that continue to play sports despite elbow pain tend to develop higher grade osteochondral lesions in the longer term.17
Rest and nonsteroidal anti-inflammatory drugs (NSAIDs) reduce the symptoms in the early stages of OCD; however, since acute ligament or muscular sprains/strains will also respond to this intervention, it can lead to a delay in making the correct diagnosis. Generally, patients with capitellar OCD present with a progressive worsening of the activity-related pain and stiffness.6,17,12 In the presence of loose bodies within the joint, loss of active elbow extension (i.e. 15–30 °) range of motion and intermittent catching and locking of the elbow tend to occur.18,6,12 Patients with radiocapitellar OCD may also present with articular crepitus, especially with pronation and supination movements; active pronation and supination with the elbow in extension also tends to reproduce familiar pain at the radio-capitellar joint.18,6,12 In a study of 69 adolescents with elbow OCD, Mihara et al. found that the most frequent symptoms are: (1) discomfort or soreness in the elbow during or after throwing (98%), (2) followed by decreased performance (58%), (3) local tenderness (43%), and (4) swelling (18%).19 None of the 69 patients in this study experienced locking of the elbow joint.19
Diagnostic imaging for elbow OCD typically begins with anterior-posterior and lateral plain film radiographs. Sixty-six percent of the patients with known capitellar OCD show pathoanatomical lesions on imaging.20 Therefore, additional investigation with other diagnostic imaging is usually needed with suspected OCD. Magnetic resonance imaging (MRI) is the gold standard in detecting and evaluating OCD lesions and is able to allow identification of early-stage lesions when plain film radiographs are negative.6,12,22 Furthermore, MRI is helpful in determining the acuity of the condition due to its capacity to detect subchondral edema.21,23,24 CT scans are highly sensitive and may be warranted for the detection of suspected loose bodies within the joint. Various classifications based on radiography, MRI, or arthroscopy have been used to describe OCD lesions. Other types of classifications divide lesions into “early-stage” or “advanced-stage” and into “stable” or “unstable”. Stable lesions are characterized by an immature capitellum with an open growth plate and flattening or radiolucency of the subchondral bone in a patient with normal elbow motion.25,26 Unstable lesions have at least one of the following findings: a capitellum with a closed growth plate, fragmentation or at least 20 degrees of elbow motion restriction.25,26 Generally, stable lesions may be reversible and can heal completely with conservative management (i.e. rest, splinting or bracing for immobilization), while unstable lesions typically require surgical management.25,15,23,19,27,28
Mihara et al.19 proposed guidelines for the management of elbow OCD. Generally, Non-operative treatment and repetitive stress cessation is the management of choice. Surgery is recommended for: (1) closed growth plate early-stage lesions; (2) if new bone formation is not observed on radiography within three to six months of conservative management or when the lesion progresses; (3) advanced-stage lesions. Discontinuing heavy elbow exercise and carrying heavy loads (i.e. conservative therapy) for 6 months has been identified as an important positive prognostic factor in the conservative management of OCD.
Patients who were compliant with the conservative therapy for stable lesions had an 84.2% healing rate, while those who had similar lesions but were non-compliant with conservative therapy only experienced a 22.7% healing rate.29
Elbow pain is very common in young athletes and physical therapists must be able to recognize the clinical picture of those patients in need of imaging, and surgical management. Thus, early diagnosis may prevent the development of higher grade of osteochondral lesions and joint degeneration in the longer term. Therefore, the purpose of this case report is to describe the main components of the history and physical examination that led to OCD differential diagnosis.
CASE DESCRIPTION
Patient History and Systems Review
A 12-year-old female gymnast presented to the clinic complaining a one-month history of right elbow pain, especially with upper extremity loading activities commonly performed during training. The subject describes an initial mechanism of injury producing sharp elbow pain when she landed on her right hand with the elbow extended during an acrobatics maneuver. The subject rated her initial pain as an 8 out of 10 on a Numeric Rating Pain Scale (NPRS) (0, no pain; 10, maximal pain) and stated that her elbow gave out as a result of the pain.30 The subject was initially evaluated by both a general practitioner (GP) physician and an orthopaedic physician and 7-10 days of rest was prescribed in the absence of serious pathology.
After one week, the subject was pain free with ADL's and returned to gymnastic activities although she continued to have pain (NPRS 5/10) with compressive loading of the elbow in extension.
The pain intensity was 5/10 but would increase to 7/10 during the workout when repeatedly performing any load-bearing activities on the upper extremity. However, the pain intensity quickly reduced a few hours after each training session and was progressively improving. After 2 weeks, a second episode of stabbing pain occurred during the landing phase of a spin jump on the affected hand. One week later, as the pain became disabling and the subject sought care from her physical therapist. Notably, the patient didn't stop gymnastics training and her parents did not permit her to take nonsteroidal anti-inflammatory drugs (NSAIDs) or any other pain medications. The patient denied any significant past or current medical problems. She and her family were concerned about the symptoms progressing and having to stop training in her sport as she had been training four to five times per week since she was five years old.
Clinical Impression #1
The patient's history revealed two sport-related elbow traumas and significant risk factors (i.e. high intensity upper extremity weightbearing activities and patient age) that led the physical therapist to suspect a pathologic condition that may have needed referral. Thus, the main objective of physical examination was to exclude any red flags and examine the structural integrity of the elbow joint.
Examination
Physical examination revealed visually and palpatory swelling over the lateral aspect of the right elbow with full flexion/extension active and passive range of motion (ROM) measures bilaterally. Passive pronation/supination, with extended elbow were also normal. Humeral-radial and humeral-ulnar elbow compression was not painful. Palpation revealed tenderness over the postero-lateral aspect of the radial head. There were no side differences in flexion/extension and pronation/supination manual force accepted during strength testing; however, local discomfort was reported during resisted wrist extension. Elbow Valgus and Varus stress tests were negative. Patient's primary pain complaint was reproduced by the injury motion: elbow hyperextension in a weight bearing or loaded position (i.e. body weight on the hand leaning onto the treatment table). In this position, external over pressure on the radiocapitellar joint by the clinician reproduced the subject's chief complaint.
Additionally, the tuning fork test was performed in order to evaluate the bony integrity. The vibrating tuning fork was placed directly and closely to the suspected fracture site (i.e. the radial head and lateral epicondyle) but was negative. Despite the estimated sensitivity ranging from 75% to 100% negative tests are not sufficient to rule out fractures because this test is not sufficiently reliable or accurate in order to rule in or out fractures and should have only limited use in clinical practice.31
Clinical Impression #2
Because of the increased reactivity to compressive load to the joint, the delay of the natural tissue healing, the injury mechanism, and the presence of demographic risk factors in the patient's history being consistent with an OCD presentation, it seemed prudent to consider imaging as part of the subject's evaluation. A decision to contact the referring orthopaedic surgeon to discuss the need for additional diagnostic imaging was made.
Diagnostic Imaging
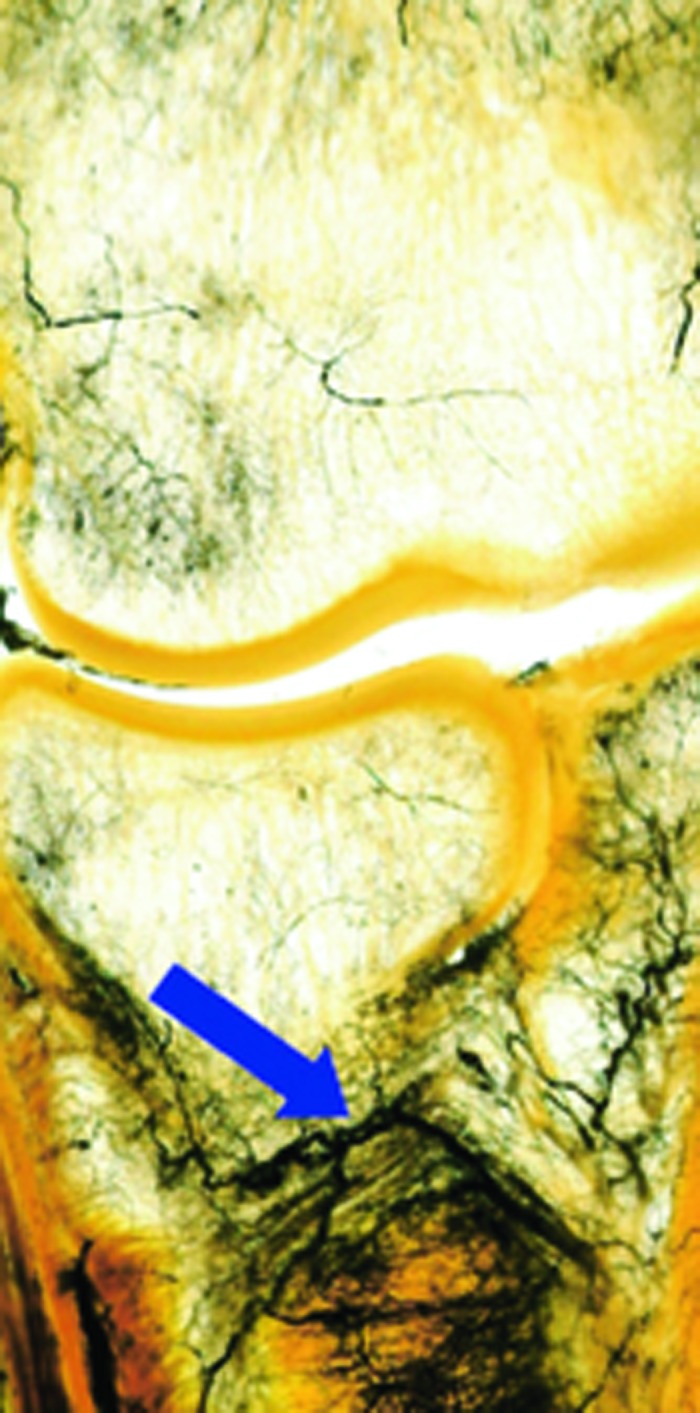
The initial plain film radiography report identified “Small irregularities of the cortical profile of the external humeral condyle, secondary to a minor traumatic detachment” (Figure 2). Based on the radiography findings, the orthopaedic surgeon prescribed an MRI imaging to further evaluate the severity of the lesion. The MRI identified an 11 mm osteochondritis dissecans associated with bone marrow edema on the external humeral condyle. Discontinuity of bone cortical was noted also. However, the extremity of the lesion appeared homogeneous. Two cystic areas, one anterior (2.5mm) and one medial (1.5mm), were identified. The cartilage surface seemed regular. Thus, the lesion was considered stable” (Figures 3a and 3b). Based on the MRI results, the decision of a conservative treatment, which included three months of complete rest from loading sports activities, were prescribed by the orthopaedic surgeon.25 After this time of rest (i.e. three months after the first MRI) a second MRI revealed a progression to an unstable lesion with fragmentation (Figures 4a and 4b).
Figure 2.
Right elbow X-ray revealed a “small irregularities of the cortical profile of the external humeral condyle”.
Figure 3a and 3b.

Protonic Density MRI. The MRI showed an osteochondritis dissecans on the lateral epicondyle associated with a bony marrow edema, indicated by red arrows.
Figure 4a and 4b.

Pre-Surgery MRI. The MRI showed a sclerotic region of the subcondral bony profile, indicated by red arrows.
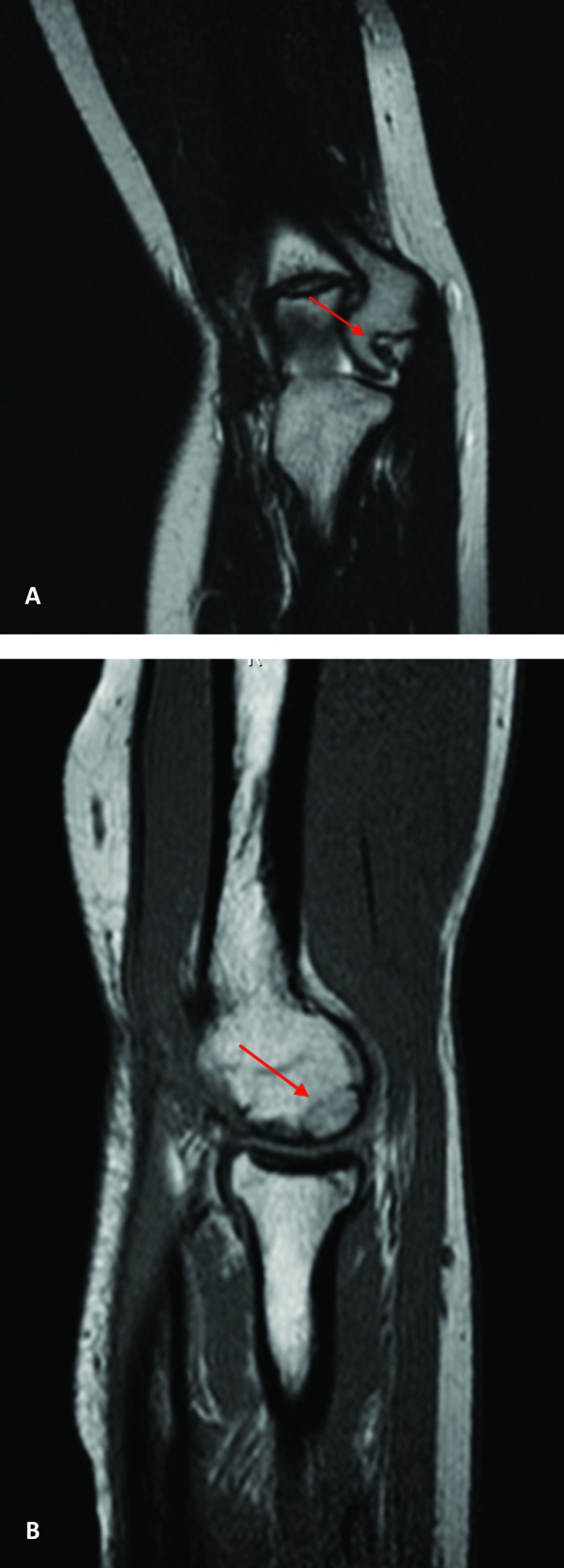
For a more detailed description of the timeline from injury to diagnosis to management, see the timeline in Figure 5
Figure 5.
Timeline of case progression.
INTERVENTION
Due to the presence of an unstable fragment and the absence of new bone genesis, resection of the osteochondral lesion and repair with enriched mesenchymal cell matrix was performed. The osteochondral lesion was resected and repaired using enriched matrix of mesenchymal cells from the iliac crest. The post-surgical protocol consisted of three weeks of immobilization in 90-degree flexion followed by four months of non-loading rehabilitation (Table 1).
Table 1.
Post-Surgical Protocol
| PHASE | OBJECTIVES | STRATEGIES | EXAMPLES |
|---|---|---|---|
| Phase 1 3 weeks - 5 months | Protecting phase | Avoiding any loading of the elbow | |
| Pain management | Pain education, self-management strategies, grade 1-2 mobilization, controlled physiological passive mobilization and soft tissue treatment | ||
| Range of motion | Grade 3-4 mobilization, passive physiological mobilization into the restriction and Mobilization with Movement. Active Mobilization | ||
| Muscular activation | Isometric and concentric istonic exercises. | ||
| Neuromuscular control | External focus exercises | Elbow AROM keeping a ball balanced on the palm or basketball dribbling with a soft sponge ball | |
| General strength and conditioning | Aerobic training, core stability and lower limb exercises | Biking, Crunch, Bridging, free weight Squatting, etc. | |
| Phase 2 5 - 10 months | Progression of general strength and conditioning | Aerobic training, core stability, legs resistance training and reintroduction upper body exercises with progressive load | Running, superman, plyometric jumping, weight free and elastic resistance on upper extremity exercise (i.e. biceps curl, elbow extension, shoulder press, etc.), etc. |
| Muscular strength and endurance | Push and pull exercise with elastic resistance or bodyweights (see the next progression) and grip exercises | Elastic resistance chop, diagonal Elastic resistance superman, wall push-up, etc. | |
| Joint load capacity | Maintenance of position for 60” at different ROM | weight bearing load on upper extremity on stable surfaces, pulling, knee push-up (progression of position: push up, v push up, hand stand, reaching in push-up position), etc. | |
| Stability | Weight bearing load on one upper extremity | One arm plank, side plank, push up on unstable surfaces (balls, TRX, rings), handstand | |
| Sport Specific Rehabilitation | Dynamic uncontrolled exercise | Rings exercises (pull up, dips), handstand walking, Front walkover, back walkover, etc. | |
| Return to sport | Sport specific exercises: | Front handspring, back handspring, etc. |
OUTCOMES
The follow-up MRI at five months post-surgically reported a “excellent graft integration” (Figure 6a, 6b). Thus, the orthopaedic surgeon advised another twenty days avoiding any loading of the elbow, to be followed by a progressive load management rehabilitation program until full recovery and a return to sport was achieved (Table 1). A final follow-up MRI was performed five months after the last PT visit.
Figure 6.
(a) After surgery MRI. T1 Coronal view shows an excellent bone graft integration. (b) After surgery MRI. T2 Sagittal view shows the resolution of the lesion with an excellent bone graft integration.
DISCUSSION
Elbow pain is a common complaint in sport. Physical therapists should be able to recognize serious pathologies outside their scope of practice requiring additional evaluation. This case report highlights the central role of primary care clinicians, such as physical therapists, in identifying patients with suspected pathologic conditions that may need referral for imaging, medical assessment or surgical intervention. Risk factors are well known from the current literature for those patients with elbow OCD. Adolescent athletes that exercise in repetitive overhead or upper extremity weight-bearing activities (e.g., baseball, tennis, volleyball, weight lifting and gymnastics) are specifically at risk.4,6,7 Like the subject described in this case repot that started training at 6 years-old, the risk of developing OCD lesions increases in those individuals that begin gymnastic training and competitions at a young age.8 Missing OCD diagnosis in younger patients could lead to an increased risk for the development of higher grade of osteochondral lesions and joint degeneration making it similar to the process of avascular necrosis in the longer term.4
The following clinical features of elbow OCD have been described in the literature:
Inflammatory-like symptoms after sports activities or load;4
Progressive worsening of pain and stiffness related to load (98% of cases);6,12,17
Decreased sport performance (58% of cases);19
Tenderness at the radiocapitellar joint (43% of cases);19
Local swelling (18% of cases);19
Intermittent catching and locking of the elbow joint;32
Crepitus, especially during pronation supination movements;6,12,18
Local pain during active pronation and supination in an elbow extension position;6,12,18
Ulnar collateral insufficiency and radiocapitellar rotatory instability.4
Risk factors and physical examination findings must be carefully assessed and weighed in order to consider possible diagnoses. This case report describes the clinical features (i.e. a history of trauma and the related injury mechanism; an increased reactivity to compressive load to the joint; the delay in symptom reduction; and the appropriate demographic Risk Factors) and the clinical reasoning that should prompt any clinician in a direct access setting to be suspicious of medical pathology in young sport population. That is to consider the many risk factors (i.e. sport loading activities, a history of long time sports activity, etc.), the behaviour and progression of symptoms especially related to the load.
This case fits with the typical challenges associated with a such complex disorder. Therefore, provoking patient's symptoms using functional testing should be considered standard practice when basic tests and measures are unremarkable.
Moreover, this case report describes the natural history and the post-surgical management of OCD of the elbow in a female gymnast. That is, early identification and optimal treatment were critical to optimize lesion healing.6 Early stage attempts at conservative treatment (i.e. resting phase in respect of the repair process) followed by a long-term post-operative program were essential in order to achieve a successful outcome.4,6,7,29 Specifically, in this case the subject had a five-month period of load avoidance in order to protect the graft. After graft integration was documented by the follow-up MRI the subject then underwent a progressive load management program with the goal of restoring the coordination skills, strength, and load capacity necessary for gymnastics participation. Accordingly, a general athletic fitness and conditioning program was introduced as soon as possible during rehabilitation. Finally, preparatory and sport-specific exercises were performed until the progressive return to sport, 10 months after surgery.
CONCLUSIONS
To the best of authors’ knowledge this is the first documented case of capitellar OCD recognized by a physical therapist in a direct access setting, resulting in operative management of the condition. The subject achieved full return to sport post-operatively (state time frame). Physical therapists are capable of screening patients in need of medical referral for further examination or investigation of conditions.33-46,47
REFERENCES
- 1.Werner SL Murray TA Hawkins RJ Gill TJ. Relationship between throwing mechanics and elbow valgus in professional baseball pitchers. J Shoulder Elbow Surg. 2002; 11(2):151-5. [DOI] [PubMed] [Google Scholar]
- 2.Edmonds EW Polousky J. A review of knowledge in osteochondritis dissecans: 123 years of minimal evolution from Konig to the ROCK study group. Clin Orthop Relat Res. 2013;471(4):1118–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bruns J. Osteochondrosis dissecans. Orthopade 1997; 26: 573-584 [DOI] [PubMed] [Google Scholar]
- 4.Nissen CW. Osteochondritis dissecans of the elbow. Clin Sports Med. 2014;33(2):251–65. [DOI] [PubMed] [Google Scholar]
- 5.Jones KJ et al. Arthroscopic management of osteochondritis dissecans of the capitellum: mid-term results in adolescent athletes. J Pediatr Orthop. 2010;30(1):8–13. [DOI] [PubMed] [Google Scholar]
- 6.Baker 3rd CL Romeo AA Baker CL. Osteochondritis dissecans of the capitellum. Am J Sports Med. 2010;38(9):1917–28. [DOI] [PubMed] [Google Scholar]
- 7.Mihata T et al. Biomechanical characteristics of osteochondral defects of the humeral capitellum. Am J Sports Med. 2013;41(8): 1909–14. [DOI] [PubMed] [Google Scholar]
- 8.Kida Y Morihara T Kotoura Y et al. Prevalence and clinical characteristics of osteochondritis dissecans of the humeral capitellum among adolescent baseball players. Am J Sports Med. 2014; 42: 1963-1971. [DOI] [PubMed] [Google Scholar]
- 9.Baratz M Yi SJ. Osteochondritis dissecans of the elbow. In: Eygendaal D, editor. The elbow. The treatment of basic elbow pathology. Nieuwegein: Arko Sports Media. 2009: 139-148 [Google Scholar]
- 10.Harada M Takahara M Sasaki J et al. Using sonography for the early detection of elbow injuries among young baseball players Am J Roentgenol. 2006; 187: 1436-1441 [DOI] [PubMed] [Google Scholar]
- 11.Uchida S et al. Arthroscopic fragment fixation using hydroxyapatite/poly-L-lactate acid thread pins for treating elbow osteochondritis dissecans. Am J Sports Med. 2015;43(5):1057–65. [DOI] [PubMed] [Google Scholar]
- 12.Greiwe RM Saifi C Ahmad CS. Pediatric sports elbow injuries. Clin Sports Med. 2010;29(4):677–703. [DOI] [PubMed] [Google Scholar]
- 13.Kosaka M et al. Outcomes and failure factors in surgical treatment for osteochondritis dissecans of the capitellum. J Pediatr Orthop. 2013;33(7):719–24. [DOI] [PubMed] [Google Scholar]
- 14.Douglas G Rang M. The role of trauma in the pathogenesis of the osteochondroses. Clin Orthop Relat Res. 1981;158: 28-32. [PubMed] [Google Scholar]
- 15.Takahara M Ogino T Takagi M et al. Natural progression of osteochondritis dissecans of the humeral capitellum: initial observations. Radiology. 2000; 216: 207-212. [DOI] [PubMed] [Google Scholar]
- 16.Takahara M Shundo M Kondo M et al. Early detection of osteochondritis dissecans of the capitellum in young baseball players. Report of three cases. J Bone Joint Surg Am. 1998; 80: 892-897. [DOI] [PubMed] [Google Scholar]
- 17.Kida Y et al. Prevalence and clinical characteristics of osteochondritis dissecans of the humeral capitellum among adolescent baseball players. Am J Sports Med. 2014;42(8):1963–71. [DOI] [PubMed] [Google Scholar]
- 18.Ahmad CS Vitale MA El Attrache NS. Elbow arthroscopy: capitellar osteochondritis dissecans and radiocapitellar plica. Instr Course Lect. 2011;60:181–90. [PubMed] [Google Scholar]
- 19.Mihara K Tsutsui H Nishinaka N Yamaguchi K. Nonoperative treatment for osteochondritis dissecans of the capitellum. Am J Sports Med. 2009; 37: 298-304. [DOI] [PubMed] [Google Scholar]
- 20.Kijowski R De Smet AA. Radiography of the elbow for evaluation of patients with osteochondritis dissecans of the capitellum. Skeletal Radiol. 2005;34(5):266–71. [DOI] [PubMed] [Google Scholar]
- 21.Takenaga T Goto H Nozaki M et al. Ultrasound imaging of the humeral capitellum: a cadaveric study. J Orthop Sci 2014;19:907-912. [DOI] [PubMed] [Google Scholar]
- 22.Zbojniewicz AM Laor T. Imaging of osteochondritis dissecans. Clin Sports Med. 2014;33(2):221–50. [DOI] [PubMed] [Google Scholar]
- 23.Bauer M Jonsson K Josefsson PO, Lindén B. Osteochondritis dissecans of the elbow. A long-term follow-up study. Clin Orthop Relat Res. 1992; 284: 156-160. [PubMed] [Google Scholar]
- 24.Dewan AK Chhabra AB Khanna AJ et al. MRI of the elbow: techniques and spectrum of disease: AAOS exhibit selection. J Bone Joint Surg Am. 2013; 95: e99 1-13. [DOI] [PubMed] [Google Scholar]
- 25.Takahara M Mura N Sasaki J et al. Classification, treatment, and outcome of osteochondritis dissecans of the humeral capitellum. J Bone Joint Surg Am. 2007; 89:1205-1214. [DOI] [PubMed] [Google Scholar]
- 26.Satake H Takahara M Harada M Maruyama M. Preoperative imaging criteria for unstable osteochondritis dissecans of the capitellum. Clin Orthop Relat Res. 2013;471:1137-1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bradley JP Petrie RS. Osteochondritis dissecans of the humeral capitellum. Diagnosis and treatment. Clin Sports Med. 2001; 20: 565-590. [DOI] [PubMed] [Google Scholar]
- 28.Takahara M Ogino T Fukushima S et al. Nonoperative treatment of osteochondritis dissecans of the humeral capitellum. Am J Sports Med. 1999; 27: 728-732. [DOI] [PubMed] [Google Scholar]
- 29.Matsuura T et al. Conservative treatment for osteochondrosis of the humeral capitellum. Am J Sports Med. 2008;36(5):868–72. [DOI] [PubMed] [Google Scholar]
- 30.Young IA Cleland JA Michener LA Brown C. Reliability #construct |validity, and responsiveness of the neck disability index, patient-specific functional scale, and numeric pain rating scale in patients with cervical radiculopathy. Am J Phys Med Rehabil. 2010;89(10):831-9. [DOI] [PubMed] [Google Scholar]
- 31.Mugunthan K Doust J Kurz B et al. Is there sufficient evidence for tuning fork tests in diagnosing fracturesϿ. A systematic review. BMJ Open. 2014;4:e005238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ryan W Churchill Julianne Munoz Christopher S Ahmad. Osteochondritis dissecans of the elbow. Curr Rev Musculoskelet Med. 2016;9:232–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mourad F Giovannico G Maselli F et al. Basilar impression presenting as intermittent mechanical neck pain: a rare case report. BMC Musculoskelet Disord. 2016;11:7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.De Hertogh W Vaes P Versijpt J Diagnostic work-up of an elderly patient with unilateral head and neck pain. A case report. Man Ther.. 2013;18(6):598-601. [DOI] [PubMed] [Google Scholar]
- 35.Plass LM McGee TG Elliott JM. Identification of metastatic lesions in a patient with low back pain following a motor vehicle collision. J Orthop Sports PhysTher. 2016. ;46(2):124. [DOI] [PubMed] [Google Scholar]
- 36.Hawkins AP1 Sum JC Kirages D et al. Pelvic osteomyelitis presenting as groin and medial thigh pain: a resident's case problem. J Orthop Sports Phys Ther. 2015;45(4):306-15. [DOI] [PubMed] [Google Scholar]
- 37.Finucane L. Metastatic disease masquerading as mechanical low back pain; atypical symptoms which may raise suspicion. Man Ther. 2013. ;18(6):624-7. [DOI] [PubMed] [Google Scholar]
- 38.De Hertogh W Vaes P Versijpt J. Diagnostic work-up of an elderly patient with unilateral head and neck pain. A case report. Man Ther. 2013;18(6):598-601. [DOI] [PubMed] [Google Scholar]
- 39.Larkin-Thier SM1 Livdans-Forret AB Harvey PJ. Headache caused by an intracranial aneurysm in a 32-year-old woman. J Manipulative Physiol Ther. 2007. ;30(2):140-3. [DOI] [PubMed] [Google Scholar]
- 40.Maselli F Pennella D Cataldi F et al. Nonspecific low back pain (LBP) can occult a serious pathology: Case report of multiple sclerosis (MS) in a young patient. Acta Medica Int. 2016;3(1):202-206. [Google Scholar]
- 41.Jessie J Mathers. Differential diagnosis of a patient referred to physical therapy with neck pain: a case study of a patient with an atypical presentation of angina. J Man Manip Ther. 2012; 20(4): 214–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mechelli F Preboski Z Boissonnault W. Differential diagnosis of a patient referred to physical therapy with low back pain: Abdominal aortic aneurysm. J Orthop Sports Phys Ther. 2008;38(9):551–557. [DOI] [PubMed] [Google Scholar]
- 43.Rodeghero JR Denninger TR Ross MD. Abdominal pain in physical therapy practice: 3 patient cases. J Orthop Sports Phys Ther. 2013;43(2):44–53. [DOI] [PubMed] [Google Scholar]
- 44.Jordan CL Rhon DI. Differential diagnosis and management of ankylosing spondylitis masked as adhesive capsulitis: A resident's case problem. J Orthop Sports Phys Ther, 2012;42(10): 842–852. [DOI] [PubMed] [Google Scholar]
- 45.Mason JS Crowell MS Goss DL. Fracture of the Scaphoid During a Bench-Press Exercise. J Orthop Sports Phys Ther. 2015;45(8):642. [DOI] [PubMed] [Google Scholar]
- 46.Ojha HA Snyder RS Davenport TE. Direct access compared with referred physical therapy episodes of care: a systematic review. Phys Ther. 2014;94(1): 14–30. [DOI] [PubMed] [Google Scholar]
- 47.Pendergast J Kliethermes SA Freburger JK Duffy PA. A comparison of health care use for physician-referred and self-referred episodes of outpatient physical therapy. Health Serv Res. 2012;47(2):633–54. [DOI] [PMC free article] [PubMed] [Google Scholar]