Abstract
Background
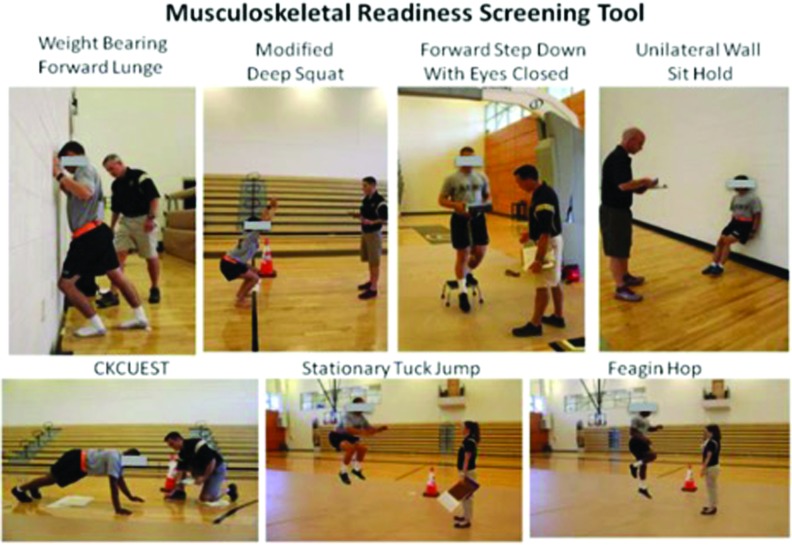
The Musculoskeletal Readiness Screening Tool (MRST) was developed in an effort to consistently predict injury among military personnel. Current injury prediction tools have not consistently predicted injury in this population. The MRST is comprised of the weight bearing forward lunge, modified deep squat, closed kinetic chain upper extremity stability test (CKCUEST), forward step down with eyes closed, stationary tuck jump, unilateral wall sit hold, and subjective, individual perceived level of risk for injury. The Feagin hop and self-reported history of injury were also included in this study protocol. The Feagin hop was a functional test used consistently by the orthopedic department located at the testing site as well as used in a recent study aimed at defining a return to duty screen; self-reported history of injury has been identified as a potential predictor of injury.
Purpose
To examine whether MRST scores, as a composite as individual components, were predictive of a United States Military Academy Preparatory School (USMAPS) student athlete sustaining a future musculoskeletal injury.
Study Design
Prospective Cohort Study
Methods
MRST scores were collected for 141 student athletes (mean age 18.63 ± 1.31) at USMAPS. The injury surveillance period was nine months. Students participated in regularly occurring military specific training and various sports. Mean scores were compared between injured and uninjured groups; binary logistic regression model was also completed.
Results
Seventy students sustained an injury. The top activities resulting in injury included football (36%) and basketball (11%) with injuries predominantly located in the lower extremity including the knee (24%), hip (15%), and ankle (14%). Composite MRST scores were not statistically different between injured (12.58 ± 2.16) and uninjured (13 ± 2.27) groups. There was an association between those with a personal concern for future injury and actual injury (p = .04). There was an association between those reporting a prior injury in the preceding 12 months and those incurring an injury at USMAPS (p = .04).
Conclusion
The MRST composite scores were not predictive of injury in this population. Previous injury and personal concern for injury were significant injury predictors.
Level of Evidence
2a
Keywords: Fear of injury, injury prediction, military, previous injury
INTRODUCTION
Musculoskeletal injuries pose the greatest threat to military readiness during both peacetime and combat operations, especially with the U.S. military drawdown of recent years.1-3 Many of the musculoskeletal injuries are sustained as a direct result of participation in sports and physical training.1 Injuries observed in military service are consistent with those incurred by professional athletes and the subsequent demands put on the military healthcare system are tremendous. In the active component of the U.S. Armed Forces, there were 3.6 million injury related encounters in 2014 alone.4
Physical training is conducted regularly across the military population. For females, physical training represented the most common cause of musculoskeletal injuries.2,5 For males, physical training was closely followed by basketball, football, and softball as the most commonly reported cause of such injuries.2 Prevention of these sports and physical training injuries is a top priority for leaders in the Department of Defense.1
Currently, there is literature aimed at identifying physical and mental (actual and perceived) factors that may predict future injury. For example, prior injury, impaired strength and neuromuscular control are associated with increased risk for second injury after anterior cruciate ligament restriction in athletes.6 However, no existing standard physical performance exam can consistently predict future injury for various athletes and occupations. As a result, sports health professionals and military clinicians treating previously injured athletes are left to use time-based protocols and expert opinion to guide their decision making process.7
While individual physical performance measures have been positively associated with injury prediction, evidence also exists that a combination of functional tests, such as the FMS, may predict future injury.8-11 However, the isolated use of the FMS to screen for injury risk is not recommended because of the low predictive value and misclassification of injury risk.12
Combining physical performance tests with at least moderate predictive validity for musculoskeletal injury with a basic military task analysis, a team of military physical therapists developed a return to duty screening tool consisting of six specific functional movements and one subjective question called the Musculoskeletal Readiness Screening Tool (MRST).13 The authors of one study found that the MRST showed potential as a tool for identifying service members at risk for injury.13 The original idea behind this injury prediction tool came from an author who designed a return to duty screen with good inter-rater reliability.14 The purpose of this study was to examine whether MRST scores, as a composite as individual components, were predictive of a United States Military Academy Preparatory School (USMAPS) student athlete sustaining a future musculoskeletal injury. Investigators hypothesized that subjects with a lower MRST composite score would have a greater likelihood of sustaining a musculoskeletal injury.
METHODS
Study design and subjects
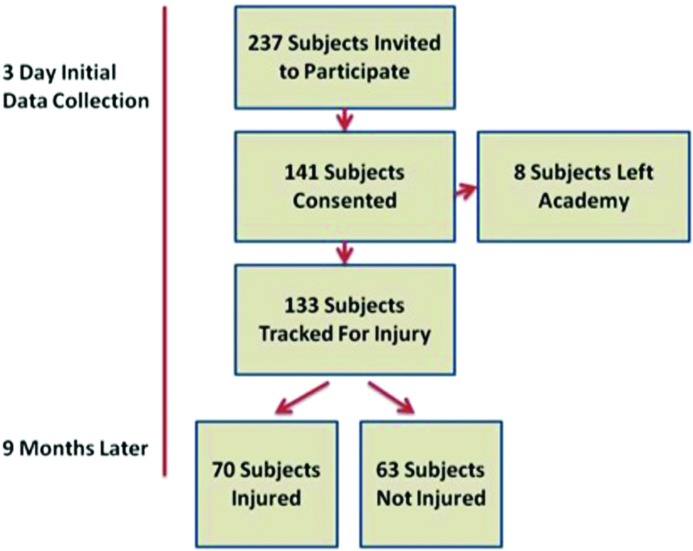
This was a prospective cohort study approved by the Institutional Review Board at Keller Army Community Hospital. Two hundred thirty-seven student athletes were briefed during the first week of attendance regarding the study, including procedures, benefits, and risks. One hundred forty-one participants volunteered (mean age 18.63 years ± 1.31). Enrollment and data collection occurred over the course of three days. Participants provided written informed consent and Health Insurance Portability and Accountability Act authorization, permitting the use of protected health information for research. After volunteering, participants proceeded directly to the health and injury history questionnaire and completed the MRST. Similar to other studies investigating injury prediction, injury was defined as an event that resulted in (1) physical impact to the body during the nine-month academic school year;15 (2) the injury required the subject to seek medical care from an athletic trainer, physician, or physical therapist; and (3) the injury resulted in modification of activity documented for at least 24 hours. Injury data were collected over the course of the nine-month academic school year. (Figure 1)
Figure 1.
Subject flowchart.
Two days prior to initial data collection, all investigators completed two hours of preparatory training. For each day of data collection, the research team set up nine stations; one designated for check-in, seven stations designated for physical performance measures, and the last for check-out. A study that included some of the physical measures of the MRST found good inter-rater reliability and moderate test-retest reliability among their testers with minimal experience.14 The same co-investigator administered each station for three days of data collection while the primary investigator monitored each station for correct performance and subject questions. The investigators were all licensed physical therapists. Focus was placed on the investigators practicing their individual stations for a four-hour training session two days prior to testing subjects.
Musculoskeletal Readiness Screening Tool
The MRST is a screening tool composed of six functional movements and a question regarding perceived risk of future injury. (Figure 2) For the purposes of this study, an additional physical performance measure and one question regarding the subject's prior musculoskeletal injury history were also collected. The Feagin hop was a functional test used consistently by the orthopedic department located at the testing site as well as used in a recent study aimed at defining a return to duty screen; self-reported history of injury has been identified as a potential predictor of injury.
Figure 2.
Components of the Musculoskeletal Readiness Screening Tool (MRST).
CKCUEST = Closed Kinetic Chain Upper Extremity Stability Test.
Tests were scored on a 0-2 ordinal scale. A score of 2 indicated the subject was able to perform the movement according to prescribed criteria and without pain. A score of 1 indicated that only part of the movement was complete and the subject performed the movement without pain. A score of 0 indicated that the subject had pain with the movement or had a bilateral deficiency on the weight-bearing lunge forward lunge. The individual prior injury component was scored on a 0-1 ordinal scale. A score of 1 indicated no prior injury whereas a score of 0 indicated prior injury. For personal concern of future injury, a score of 2 indicated no concern, a score of 1 indicated mild to moderate concern, and a score of 0 indicated significant concern for injury. The total score ranges from a minimum of 0 points to a maximum of 17 points (2 points per physical test, 2 points possible for no personal concern for injury, and 1 point for no prior injury).
Weight Bearing Forward Lunge
The weight bearing forward lunge test was performed with shoes off. Participants assumed a shoulder-width staggered stance position with two fingers touching the wall, as a balance aid only, and the tip of the forward great toe 12cm from the wall. The subject lunged forward while attempting to keep the front heel on the ground. This was repeated for the contralateral limb. The participant received 2 points if each of the patellae contacted the wall and the great toe was positioned 12cm or greater away from the wall. One point was awarded for unilateral achievement, and 0 points if the test was painful or the subject was unable to touch the wall bilaterally. Measurement of weight bearing dorsiflexion has been found to be reliable for novice and expert testers.9 In previous studies, the ankle dorsiflexion lunge was a reliable predictor of injury.9
Modified Deep Squat
The modified deep squat was initiated with the participant standing barefoot and the shoulders abducted 180 degrees and elbows extended to 90 degrees. With the toes facing directly forward, the subject attempted to squat low enough for the thighs to break parallel with the floor. Two points were received for an upper torso that remained parallel with the tibia or vertical, arms in line with the torso, femur below horizontal, and the knees aligned over the feet. Failure to meet any of the criteria listed resulted in one point, and 0 points if the test was painful. The deep squat has been validated as part of the Functional Movement Screen.10,15
Closed Kinetic Chain Upper Extremity Stability Test (CKCUEST)
The CKCUEST required the subject to assume a push-up position with the shoes on. Males started in the push-up position and females began in the kneeling push-up position. With the back slightly inclined in relation to the floor and the hands 36 inches apart, the subject leaned over to touch one hand on the other and then returned the hand to the starting position. Tape marked the starting position for each hand and a folded towel was placed under the knees for comfort of female subjects only. This procedure was repeated in a rapid alternating fashion and 2 points were awarded for 20 repetitions, 1 point for less than 20 repetitions, and 0 points awarded if the test was painful regardless of the number of repetitions completed. The CKCUEST has a high test-retest reliability and inter-rater reliability is excellent.16,17 This test is significantly correlated with both left and right side injuries. It has a sensitivity of 0.83, a specificity of 0.79, and odds ratio of 18.75 in determining a shoulder injury using a score of 21 touches.18
Forward Step Down
The forward step down with eyes closed began with the shod subject standing on a standard 8-inch step with the feet approximately shoulder width apart. The subject held two hardcover textbooks weighing approximately 6.8 kilograms at navel level with elbows flexed to 90 degrees and eyes closed. The textbooks were not permitted to make contact with the subject anywhere other than the hands. The subject stepped down with one leg at a time while the investigator stood in front of the subject for safety. Two points were awarded if the subject kept the eyes closed and there was no deviation of the lower extremities in the frontal plane. One point was awarded if the eyes opened, a loud foot landing determined subjectively by tester, or any frontal plane deviation was noted. Finally, 0 points were awarded if the test was painful.
Stationary Tuck Jump
The stationary tuck jump involved the subject standing with feet shoulder width apart, arms at the side in an athletic crouched position. The subject initiated a jump with arms extended behind the subject and while swinging the arms forward the subject jumped vertically, pulled the knees up as high as possible and then attempted to land softly in the same position. This was repeated quickly three times such that each jump occurred immediately upon landing from the preceding jump. If the subject could perform three jumps with thighs at least oriented 45 degrees in the sagittal plane about a coronal axis, landing in approximately the same position with a soft landing 2 points were awarded. One point was awarded if the subject did not meet the criteria, and 0 points awarded if the test was painful. The tuck jump assessment has been shown to be an easily performed test to identify high risk landing mechanics.19,20 It also has good intra-tester and interrater reliability in it's typical performance over 10 seconds.21
Unilateral Wall Sit Hold
The unilateral wall sit hold required the subject to stand with body weight evenly distributed, feet shoulder width apart, and shoes on. The back was pressed against the wall with the hips and knees flexed to create an angle between the wall and thigh at 45 degrees. The arms hung vertically and then the subject lifted one foot such that it was 1-2 inches off the floor. The investigator started the stopwatch and then stopped at 30 seconds or when the athlete could not sustain the test position. One minute of rest was followed by testing of the contralateral limb. Two points were awarded for maintaining the test position for 30 seconds bilaterally. Only 1 point was awarded for holding less than 30 seconds on either extremity and 0 points awarded if the test was painful. The unilateral wall sit hold is a significant predictor of injury for NCAA football.22
Feagin Hop
The Feagin hop test involved the subject standing directly on a line with the non-test lower extremity held in slight knee flexion with the shoes on. The subject performed a maximum effort vertical hop. This was performed twice on each leg. Two points were awarded for landing in the same position with a soft landing and no frontal plane deviation bilateral. Only 1 point was awarded if the subject did not meet all criteria above and 0 points awarded if the test was painful.14 The Feagin hop test was included in a military return-to-duty screen and found to have moderate to good interrater reliability.14
Questionnaire
Participants completed a questionnaire to assess their history of previous injury and other descriptive information. The first question asked, “Have you experienced a prior injury that limited your participation in athletics or daily activity for more than seven days within the last 12 months?” Response categories were “yes” or “no”. One point was awarded for the answer no and 0 points awarded for answering yes. The follow-up questions asked, “If you answered yes for question #1, please identify the following from your prior injury by circling the words that best fit your injury.” “Was the injury on your left or right?” “The injured body part was the head, arm, leg, back, or chest/torso?” “The injury occurred during contact or non-contact sport?” Next, the subject's personal concern for injury was asked with this question ensuring the participant circled only one answer: “How would you describe your personal concern for sustaining a musculoskeletal injury within the next nine months?” Responses included, “no concern for injury, mild to moderate concern for injury, or significant concern for Injury.” Two points were awarded for no concern for injury. One point was awarded for mild to moderate concern for injury and 0 points awarded for significant concern for injury. Age in years, height in inches, weight in pounds, and gender were also collected. Finally, the following demographic data were also collected ensuring participants circled one answer: “Arab, Asian/Pacific Islander, Black, Caucasian/White, Hispanic, Multiracial, and Other.”
Documentation
All health-related records were stored in three primary locations including the paper-based local athletic training record, and two automated medical documentation systems: the Cadet Illness and Injury Tracking System and the Armed Forces Health Longitudinal Technology Application. All medical encounters were reviewed initially by the principal investigator. In a separate meeting, two USMAPS certified athletic trainers and principal investigator collected all injury documentation occurring from August 2014 through May 2015. Similar to the study by Garrison et al. investigating injury prediction,23 injury was defined as an event that resulted in physical impact to the body during the academic school year, the injury required the subject to seek medical care from an athletic trainer, physician, or physical therapist, and the injury resulted in modification of activity for a minimum of 24 hours. The following details regarding each injury occurrence were recorded: contact or non-contact mechanism, traumatic or atraumatic, exact anatomic location(s), diagnosis, activity or sport mechanism of injury, and finally the number of lost duty days.
Statistical Methods
Mean MRST scores were compared between injured and uninjured groups with an independent t-test. With nine predictors, investigators sought a minimum of 15 subjects per predictive test or 135 subjects to conservatively ensure adequate power. All MRST composite scores were evaluated to see if any score would be associated with the greatest degree of both sensitivity and specificity. Several elements of the data were analyzed including total MRST score, history of past injury, and a personal concern of injury. Odds ratios, sensitivity, specificity, and likelihood ratios were calculated for each of these conditions. To determine if the MRST could predict future injury, logistic regression models were performed. Predictor variables were determined by analyzing individual component scores on the MRST, the composite MRST score, past history of injury, and personal concern for injury. The Pearson's Chi-Square test was used to determine the impact prior injury and personal concern for injury had on future injury. Data analysis was performed using the PEDro Confidence Interval Calculator and the R Core Team 2015 v 3.1.1. (R Foundation; Vienna, Austria).
RESULTS
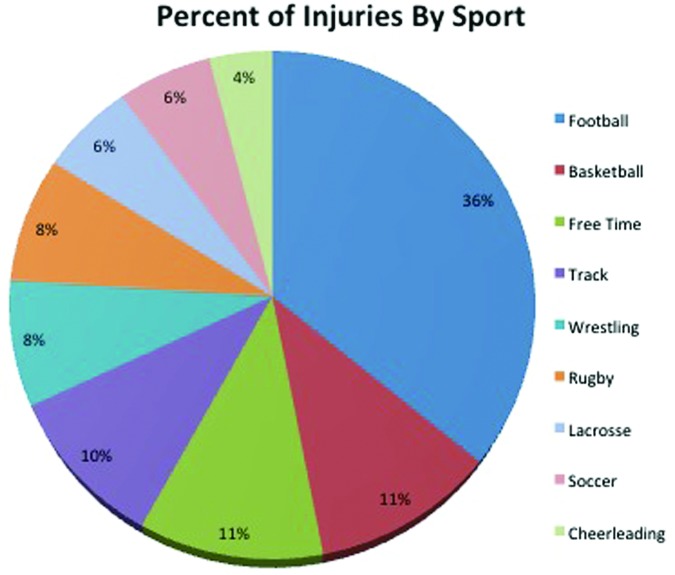
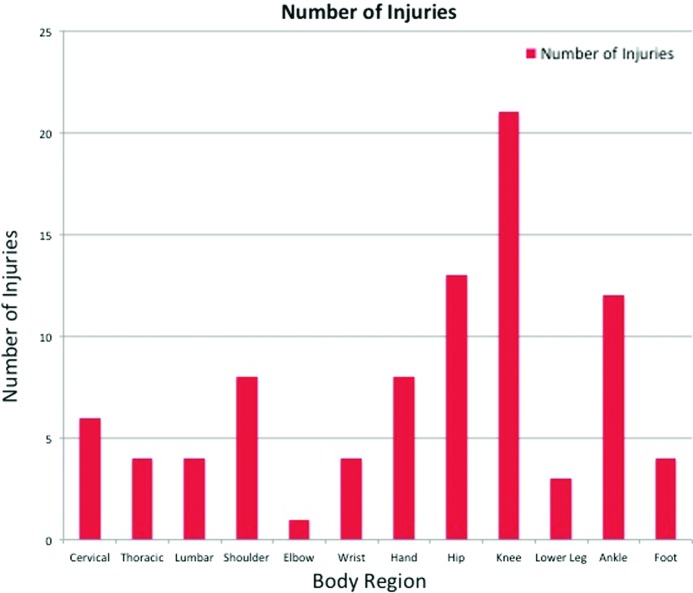
One hundred thirty-three participants (133/141 = 94%) were included in the final data analysis. Eight participants were lost to follow-up because they left the academy for personal reasons. Mean age was 18.63 years (±1.31), mass 81.04 kg (±16.98), and height 177.46 cm (±10.21). One hundred ten (83%) of the subjects were male. Forty-one percent of the subjects were self-reported Caucasian/white, 38% black, and 12% multiracial. 53% of participants sustained an injury and 47% did not sustain an injury during the nine-month 2014-2015 academic school year. The top four activities resulting in injury were: football (36%), basketball (11%), free time (11%), and track (10%). (Figure 3) Injuries predominantly occurred at the knee (24%), hip (15%), and ankle (14%). (Figure 4)
Figure 3.
Injuries by sport.
Figure 4.
Injuries by body region.
The mean MRST composite score for the injured group was 12.58 (±2.16) and for the uninjured group was 13(±2.27). Comparing these means with an independent t-test resulted in no statistically significant difference between the two groups (p = .78) No statistically significant difference was observed between composite MRST scores for those that incurred an overuse injury at 12.54 to those uninjured or incurred an acute injury at 12.64 (p = .85).
The impact of prior injury and personal concern for injury had on future injury was also investigated. Using the Pearson's Chi-Square Test there was a significant association between those reporting a prior injury and those incurring a future injury (p = .04). (Table 1) There was also a significant association between those with a personal concern for future injury and those actually incurring a future injury (p = .04). (Table 2)
Table 1.
Association Between Self-Reported Prior Injury and Nine-Month Injury Follow-Up.
| Uninjured | Injured | |
|---|---|---|
| Prior Injury | 11 | 23 |
| No Prior Injury | 52 | 47 |
p = 0.04. Odds Ratio: 2.3; 95% CI (1.02,5.25)
Table 2.
Association Between Self-Reported Concern For Injury and Nine-Month Injury Follow-Up.
| Uninjured | Injured | |
|---|---|---|
| Concern | 23 | 38 |
| No Concern | 40 | 32 |
p = 0.04. Odds Ratio: 2.1; 95% CI (1.03, 4.14)
Sensitivity, specificity, and likelihood ratios were calculated based on individual MRST components. Of note, the two tests with the greatest sensitivity were the dorsiflexion lunge and squat at 0.62 and 0.85, respectively. The two tests with the greatest specificity were the wall sit hold and CKCUEST at 0.83 and 0.70 respectively. (Table 3)
Table 3.
Association between Individual Physical Measures on MRST and Injury.
| Sensitivity | Specificity | Positive Likelihood Ratio | Negative Likelihood Ratio | Odds Ratio (Confidence Interval) | |
|---|---|---|---|---|---|
| Weight Bearing Forward Lunge | 0.62 | 0.44 | 1.11 | 0.86 | 1.29 (0.65,2.59) |
| Modified Deep Squat | 0.85 | 0.23 | 1.10 | 0.66 | 1.65 (0.68, 3.96) |
| Stationary Tuck Jump | 0.39 | 0.60 | 0.98 | 1.01 | 0.97 (0.48, 1.97) |
| CKCUEST | 0.09 | 0.70 | 0.33 | 1.28 | 0.25 (0.09, 0.66) |
| Forward Step Down | 0.19 | 0.67 | 0.59 | 1.19 | 0.49 (0.22, 1.09) |
| Feagin Hop | 0.58 | 0.45 | 1.06 | 0.92 | 1.14 (0.57, 2.28) |
| Unilateral Wall Sit Hold | 0.22 | 0.83 | 1.37 | 0.92 | 1.48 (0.61, 3.56) |
MRST = Musculoskeletal Readiness Screening Tool, CKCUEST = Closed kinetic Chain Upper Extremity Stability Test
Odds ratios compared the predictive power of the MRST composite scores and prior injury. No MRST composite score was identified as a useful cutoff score for predicting future injury. The composite score that represented the best combination of sensitivity and specificity was 12 with an odds ratio of 1.33 (0.67, 2.64).
DISCUSSION
Results indicated that MRST scores were not predictive of injury in USMAPS student athletes. A previous history of injury was predictive of future injury. A USMAPS student athlete that reported a previous injury had an 83% chance of sustaining an injury. These results are consistent with the results of multiple studies demonstrating that a history of previous injury is the strongest individual predictor of future injury.24-27 The odds ratio of 2.31 for prior injury demonstrates that a student athlete with a history of a prior injury in the previous 12 months has more than two times greater chance of injury than a student athlete without a prior injury.
In this student population, 53% of injuries resulted from sports and physical training, which is consistent with multiple military studies. Musculoskeletal injuries represented the leading cause of medical care visits across the military.3 Physical training and sports are the main cause of non-battle injuries, 56% a direct result of physical training.3 Basketball, football, and softball were the most common sports associated with injury in recent studies examining Air Force and Army sports and physical training injuries. The results of this study are similar, with football, basketball, and free time ranking as the most common activities associated with injury at 36%, 11%, and 11%, respectively. Also similar to Lauder and colleagues,2 the top injuries directly involved the lower extremity with the knee being the most common site of injury.
In this current population, fear of injury was an injury predictor. Previous investigators have observed that psychological factors and the fear of re-injury influence return to play and injury risk.28-30 There appears to be a strong positive correlation of injury occurrence with athletes undergoing greater degrees of stress, whereas athletes with increased optimism toward their activity were less likely to sustain an injury.30 Self-confidence and psychological influences affect sport injury risk.31,32
Although the MRST did not predict injury in this population, it may be useful in predicting injury outside of a student athlete population. Various units in the military participate in more diverse physical activity, such as military training events, without the daily sport activity frequently encountered in a preparatory school. Evaluating the predictive abilities of the MRST in specific military units will help determine its utility in the military.
This study has some limitations that should be taken into consideration. First, exposure to sports was not controlled. Understanding the exposure to training and the participants' prior fitness levels may help account for the amount of risk the subjects were exposed to and allow for a more accurate comparison of exposure to other studies. This sample consisted of 60% football players which may have affected the injury rate. This was a fairly homogeneous sample and may not be representative of other young, collegiate athletes or the military in general. Finally, there is a lack of reliability data on the Feagin Hop as opposed to the other physical measures identified in this study. This does not mean that the Feagin Hop shouldn't be used; rather, research should be performed to examine it's as an evidence-based test.
The results of this study may provide valuable information to clinicians. It is clear that a prior history of injury and concern for injury continue to be a strong risk factor for injury. Although the MRST did not predict injury, this study provided information on the incidence of injury, sports most commonly associated with injury, and the incidence of injury according to body location in this select population. More research is needed to determine if the MRST should be used with other military personnel or student athletes. This study adds to the descriptive epidemiological research demonstrating lower extremity injuries and sports such as football and basketball account for the most injuries.
CONCLUSIONS
This study contributes to the current research investigating functional movement and screening tools used to predict future injury and suggests injury prediction is likely multi-factorial and may not come down to purely physical or psychological factors alone. Given that the only factors directly associated with injury in this study were reported previous injury and fear of injury, clinicians should continue to query athletes regarding their injury history. Future research should focus on evaluating the reliability, predictive and convergent validity of the MRST, or another screening tool, if it is to potentially be considered a viable option for injury prevention within the military.
References
- 1.Cameron KL Owens BD. The burden and management of sports-related musculoskeletal injuries and conditions within the US military. Clin Sports Med. 2014;33(4):573-589. [DOI] [PubMed] [Google Scholar]
- 2.Lauder TD Baker SP Smith GS Lincoln AE. Sports and physical training injury hospitalizations in the army. Am J Prev Med. 2000;18(3 Suppl):118-128. [DOI] [PubMed] [Google Scholar]
- 3.Nindl BC Williams TJ Deuster PA Butler NL Jones BH. Strategies for optimizing military physical readiness and preventing musculoskeletal injuries in the 21st century. US Army Med Dep J. December 2013:5-23. [PubMed] [Google Scholar]
- 4.Brundage J. Absolute and Relative Morbidity Burdens Attributable to Various Illnesses and Injuries, U.S. Armed Forces, 2014. Med Surveill Mon Rep. 2014;22(4):5-10. [PubMed] [Google Scholar]
- 5.Roy TC Songer T Ye F, et al. Physical training risk factors for musculoskeletal injury in female soldiers. Mil Med. 2014;179(12):1432-1438. [DOI] [PubMed] [Google Scholar]
- 6.Myer GD Martin L Ford KR, et al. No association of time from surgery with functional deficits in athletes after anterior cruciate ligament reconstruction: evidence for objective return-to-sport criteria. Am J Sports Med. 2012;40(10):2256-2263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haines S Baker T Donaldson M. Development of a physical performance assessment checklist for athletes who sustained a lower extremity injury in preparation for return to sport: a delphi study. Int J Sports Phys Ther. 2013;8(1):44-53. [PMC free article] [PubMed] [Google Scholar]
- 8.Chorba RS Chorba DJ Bouillon LE Overmyer CA Landis JA. Use of a functional movement screening tool to determine injury risk in female collegiate athletes. North Am J Sports Phys Ther. 2010;5(2):47-54. [PMC free article] [PubMed] [Google Scholar]
- 9.Clanton TO Matheny LM Jarvis HC Jeronimus AB. Return to play in athletes following ankle injuries. Sports Health. 2012;4(6):471-474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lisman P O'Connor FG Deuster PA Knapik JJ. Functional movement screen and aerobic fitness predict injuries in military training. Med Sci Sports Exerc. 2013;45(4):636-643. [DOI] [PubMed] [Google Scholar]
- 11.Garrison M Westrick R Johnson MR Benenson J. Association between the functional movement screen and injury development in college athletes. Int J Sports Phys Ther. 2015;10(1):21-28. [PMC free article] [PubMed] [Google Scholar]
- 12.Bushman TT Grier TL Canham-Chervak M Anderson MK North WJ Jones BH. The Functional Movement Screen and Injury Risk: Association and Predictive Value in Active Men. Am J Sports Med. 2016;44(2):297-304. [DOI] [PubMed] [Google Scholar]
- 13.Hearn D Rhon D Goss D Thelen M. Evaluation of a Novel Field Expedient Musculoskeletal Readiness Screening Tool in an Army Basic Training Population. Mil Med. 2017;182(7):e1862-e1868. [DOI] [PubMed] [Google Scholar]
- 14.Thelen MD Koppenhaver SL Hoppes CW Shutt C Musen J-L Williams MK. Reliability of a Novel Return to Duty Screening Tool for Military Clinicians. US Army Med Dep J. December 2015:14-23. [PubMed] [Google Scholar]
- 15.Kiesel K Plisky PJ Voight ML. Can Serious Injury in Professional Football be Predicted by a Preseason Functional Movement Screen? North Am J Sports Phys Ther. 2007;2(3):147-158. [PMC free article] [PubMed] [Google Scholar]
- 16.Roush JR Kitamura J Waits MC. Reference Values for the Closed Kinetic Chain Upper Extremity Stability Test (CKCUEST) for Collegiate Baseball Players. North Am J Sports Phys Ther NAJSPT. 2007;2(3):159-163. [PMC free article] [PubMed] [Google Scholar]
- 17.Tarara DT Hegedus EJ Taylor JB. Real-time test-retest and interrater reliability of select physical performance measures in physically active college-aged students. Int J Sports Phys Ther. 2014;9(7):874-887. [PMC free article] [PubMed] [Google Scholar]
- 18.Pontillo M Spinelli BA Sennett BJ. Prediction of in-season shoulder injury from preseason testing in division I collegiate football players. Sports Health. 2014;6(6):497-503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Myer GD Brent JL Ford KR Hewett TE. Real-time assessment and neuromuscular training feedback techniques to prevent ACL injury in female athletes. Strength Cond J. 2011;33(3):21-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Myer GD Ford KR Hewett TE. Tuck Jump Assessment for Reducing Anterior Cruciate Ligament Injury Risk. Athl Ther Today J Sports Health Care Prof. 2008;13(5):39-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Herrington L Myer GD Munro A. Intra and inter-tester reliability of the tuck jump assessment. Phys Ther Sport. 2013;14(3):152-155. [DOI] [PubMed] [Google Scholar]
- 22.Wilkerson GB Colston MA. A Refined Prediction Model for Core and Lower Extremity Sprains and Strains Among Collegiate Football Players. J Athl Train. 2015;50(6):643-650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Garrison M Westrick R Johnson MR Benenson J. Association between the functional movement screen and injury development in college athletes. Int J Sports Phys Ther. 2015;10(1):21-28. [PMC free article] [PubMed] [Google Scholar]
- 24.Hoch MC Staton GS McKeon PO. Dorsiflexion range of motion significantly influences dynamic balance. J Sci Med Sport Sports Med Aust. 2011;14(1):90-92. [DOI] [PubMed] [Google Scholar]
- 25.Hootman JM Macera CA Ainsworth BE Martin M Addy CL Blair SN. Predictors of lower extremity injury among recreationally active adults. Clin J Sport Med. 2002;12(2):99-106. [DOI] [PubMed] [Google Scholar]
- 26.Konor MM Morton S Eckerson JM Grindstaff TL. Reliability of three measures of ankle dorsiflexion range of motion. Int J Sports Phys Ther. 2012;7(3):279-287. [PMC free article] [PubMed] [Google Scholar]
- 27.Warren M Smith CA Chimera NJ. Association of the Functional Movement Screen with injuries in division I athletes. J Sport Rehabil. 2015;24(2):163-170. [DOI] [PubMed] [Google Scholar]
- 28.Ardern CL Taylor NF Feller JA Whitehead TS Webster KE. Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2013;41(7):1549-1558. [DOI] [PubMed] [Google Scholar]
- 29.Taylor J. Predicting athletic performance with self-confidence and somatic and cognitive anxiety as a function of motor and physiological requirements in six sports. J Pers. 1987;55(1):139-153. [DOI] [PubMed] [Google Scholar]
- 30.Wadey R Evans L Hanton S Neil R. Effect of dispositional optimism before and after injury. Med Sci Sports Exerc. 2013;45(2):387-394. [DOI] [PubMed] [Google Scholar]
- 31.Taylor J. Predicting athletic performance with self-confidence and somatic and cognitive anxiety as a function of motor and physiological requirements in six sports. J Pers. 1987;55(1):139-153. [DOI] [PubMed] [Google Scholar]
- 32.Wiese-Bjornstal DM. Psychology and socioculture affect injury risk, response, and recovery in high-intensity athletes: a consensus statement. Scand J Med Sci Sports. 2010;20 Suppl 2:103-111. [DOI] [PubMed] [Google Scholar]