Abstract
Background
There are inconsistencies in the reported rates of second anterior cruciate ligament (ACL) injuries per limb, patients' sex and graft types after primary ACL reconstruction (ACLR). There are also inconsistencies regarding the influence of these factors on the occurrence of second ACL injury after primary ACLR.
Purpose
To determine the rate of second ACL injury, to either the ipsilateral graft or contralateral healthy ACL, as influenced by sex, age, and graft types and to determine the influence of sex, age, and graft types on the occurrence of second ACL injury after primary ACLR.
Study design
Systematic review and meta-analysis
Methods
A computerized search of MEDLINE, CINAHL, and SPORTDiscus was conducted using combinations of these terms: ACL, ACLR, re-injury, re-rupture, revisions, contralateral tear, ipsilateral graft tear, and second injury. Articles were required to report the number or percentage of sex, graft type, ipsilateral graft and contralateral ACL injuries after ACLR. Rates of second ACL injuries and pooled dichotomous data were calculated using random-effect proportion meta-analysis.
Results
The pooled rate of second ACL injuries (ipsilateral graft and contralateral ACL) was 6.11%. A slightly higher rate of ipsilateral graft injuries (3.29%) than contralateral ACL injuries (2.82%) (OR: 1.09 [95%CI: 0.89, 1.34] was reported. Ipsilateral graft injuries occurred earlier (median: 20 months) than contralateral ACL injuries (median: 36.3 months). Men had lower rate of second ACL injuries (5.67%) than women (6.84%) (OR: 0.92 [95%CI: 0.70, 1.20]). Significantly higher rate of ipsilateral graft injuries (3.40%) occurred in men compared to contralateral ACL injuries (2.26%) (OR: 1.53 [95CI%: 1.33, 1.77]), while women had significantly higher rate of contralateral ACL injuries (3.75%) compared to ipsilateral graft injuries (3.09%) (OR: 0.73 [95%CI: 0.55, 0.96]). The rate of second ACL (ipsilateral graft and contralateral ACL) injuries was higher in patients with hamstring tendon (HT) autograft (5.83%) than bone-patella tendon-bone autograft (BPTB) (5.10%) (p = 0.04) and allografts (3.12%) (p<0.0001). The rate of ipsilateral graft injuries was significantly higher than contralateral ACL injuries in all graft types (p<0.001).
Conclusion
Injuries to the ipsilateral graft are more common than contralateral ACL, with ipsilateral graft injuries occurring nearly 16 months earlier after ACLR. More women sustain second ACL injuries compared to men, with men incurring more injuries to the ipsilateral graft and women to the contralateral ACL. Furthermore, second ACL injuries are more common in patients with HT autograft, BPTB autograft, and then allograft; with ipsilateral graft injuries higher than contralateral ACL injuries regardless of graft types.
Levels of Evidence
2a
Keywords: Autograft injury, contralateral ACL injury, ipsilateral graft injury, second ACL injury, women re-injury
INTRODUCTION
Early anterior cruciate ligament reconstruction (ACLR) is the standard of care for managing young athletes after initial ACL rupture, as it restores mechanical knee stability, function, and preserves the joint integrity.1-4 In the United States alone, up to 175,000 reconstructive surgeries are performed annually.5 After ACLR, resuming preinjury level of activity without incurring a second anterior cruciate ligament (ACL) injury is considered a successful outcome.6 Unfortunately, second ACL injuries continue to occur even after successful reconstructive surgery and rehabilitation, with the reported rates of second ACL injuries varying between 3% and 30%.7-14 High variability in the reported rates of second ACL injury may be related to inclusion of data from patients with different ages, sex, graft types, activity levels, and different follow-up timeframes after surgery.
Incurring an injury to the ipsilateral graft or contralateral ACL after primary ACLR is devastating for both the patient and medical care providers. This has triggered attention of researchers to focus their investigations on identifying potential risk factors that may account for the occurrence of second ACL injuries. Multiple factors have been reported to be associated with incurring an ipsilateral graft injury. Some patient-related factors include being younger in age15-17 and having family history of ACL injury.18,19 Surgical-related factors included a vertical graft orientation,7,8,18 small graft size and post-operative knee laxity,16,20-22 and using the hamstring graft.23 Other factors associated with ipsilateral graft injury include the same mechanism of injury as that at the time of initial ACL injury11 and patients' physical activities after reconstructive surgery: such as early return to high-demand physical activities11 and pivoting activities.18,24
After ACLR, the rate of injury for contralateral ACL is comparable to that of ipsilateral graft.25,26 A recent systemic review and meta-analysis, investigated the risk of second ACL injury in young athletes after ACLR, found that the rates of ipsilateral graft and contralateral ACL injuries to be 7% and 8%, respectively.25 Bourke et al, however, reported a higher injury rate to the ipsilateral graft (17%) compared to the contralateral ACL (9.7%).22 Additionally, Reid et al reported that the rate of ipsilateral graft injury was 9% compared to only 2% in the contralateral ACL.27 Risk factors that may account for the contralateral ACL injury include the same risk factors that caused the primary ACL injury28 such as altered lower extremity biomechanics, and the presence of functional deficits after ACLR.9,29-34
The influence of patients' sex as a risk factor on second ACL injury is still controversial, as it has been reported that men tend to have a high risk of reinjury8,17,18,22 while women have higher revision rates.24,35 Women demonstrate a higher risk of sustaining a primary ACL rupture36,37 and second ACL injury to the contralateral limb after ACLR compared to men.17,24,38 Authors of several cohort studies have indicated that men tend to demonstrate an equal to higher risk of incurring an ipsilateral graft injury compared to the contralateral intact ACL after ACLR.17,26,35,39 Paterno et al24 reported that, after ACLR, women were four times more likely to sustain an ipsilateral graft injury and six times more likely to acquire a contralateral ACL injury compared to men.24 Recent systemic reviews have reported that there were no differences between men and women incurring an ipsilateral graft injury.40,41 Thus, a systemic review and meta-analysis study could be useful to further investigate the incidence rates of ipsilateral graft and contralateral ACL injuries between sexes.
Second ACL injury has been reported to be associated with various graft types. There is a consensus that allografts have a lower survival rate compared to autografts.23,42,43 However, there is inconsistency in the reported findings for autografts. Tylor et al44 found similar injury rates between patellar tendon (PT) and hamstring tendon (HT) autografts. Whereas Mohtadi et al45 found no differences in re-rupture rates between PT and HT autografts. Other authors have reported a higher rate of ipsilateral graft injury in the HT compared to the PT autograft.46-48 While graft type is a potential risk factor for graft failure, it has yet to be determined the extent of influence that each type of tissue has on graft failure or injury to the contralateral ACL after ACLR. The importance of determining the failure tendency of the harvested tissue may help the decision-making of which graft type to use during the reconstructive surgery.
Whether the second ACL injury occurs in the ipsilateral graft or contralateral intact ACL, it is an outcome of growing concern with substantial consequences. Although there is currently a significant amount of evidence indicating an increased likelihood of incurring a second ACL injury after primary ACLR, a lack of evidence continues to exist in determining which demographic factors and graft types contribute most to the increased number of second ACL injuries. Conducting a comprehensive data analysis of published studies may help provide an accurate review of ipsilateral graft and contralateral ACL injury rates per patients' age, sex, and graft type. Moreover, it could clarify the influence of these factors on the occurrence of second ACL injuries after primary ACLR. Therefore, the purposes of this systemic review and meta-analysis were (1) to determine the rate of second ACL injury, to either the ipsilateral graft or contralateral healthy ACL, as influenced by sex, age, and graft types and (2) to determine the influence of sex, age, and graft types on the occurrence of second ACL injury after primary ACLR.
MATERIALS AND METHODS
Literature Search
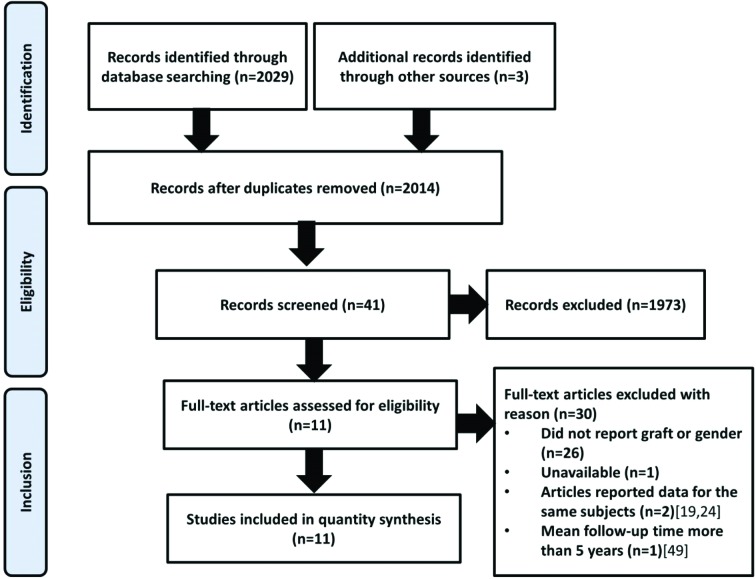
A computerized search was performed for articles on second ACL injury, either to the ipsilateral or contralateral ACL, in patients after primary ACLR. The databases of MEDLINE, CINAHL, and SPORTDiscus were searched for full text articles published in English using combinations and variations of the following terms: ACL, ACLR, re-injury, re-rupture, revisions, contralateral tear, ipsilateral graft tear, and second injury. Authors conducted a broad search in order to capture the majority of articles that reported second ACL injury. The original search revealed 2,029 articles that fit the searched terms. After deleting the duplicated articles, the titles and the abstracts of all identified articles were reviewed for relevance. The search was augmented by cross-checking citations and references of the relevant published articles. In addition to the computerized search, three articles were identified through a hand search of relevant published articles.19,26,49 The search was completed in September 2016 with a total of 41 articles left to be thoroughly read for inclusion criteria. Thirty articles were excluded from this analysis (26 articles did not report graft type or sex, one article was not available in full text, one article included data at a mean follow-up time of 20 years,50 and two articles reported data from the same patients19,24). If articles that reported data for the same patients, the articles that were published earlier were excluded. This resulted in articles by Paterno et al (2014)38 and Webster and Feller(2016)26 being utilized, while Paterno et al (2012)24 and Webster et al (2014)19 were excluded.
Study selection
After all available abstracts were thoroughly examined; the full-text articles were evaluated for inclusion criteria. All articles included in this systematic review and meta-analysis were written in English language and reported the number or percentage of ipsilateral graft and/or contralateral ACL injuries within five years from ACLR. Exclusion criteria included: articles that did not meet any of the previously stated requirements, written in non-English language, had a mean follow-up of more than five years, conference proceedings abstracts, narrative reviews, or clinical commentaries. One article reported follow up of second injury at 2, 5, 10 and 15 years after ACLR, but only data from the 2 and 5 years were included in the analysis of the current analysis.18 While conducting the systematic review and meta-analysis, authors identified articles' eligibility and inclusion based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Figure 1).
Figure 1.
Assessment of Studies' Quality
The methodological quality of the included articles was assessed and rated by two reviewers independently using the Modified Downs and Black checklist (Table 1). This tool is a checklist including 13 items of “yes (Y)” or “no (N)” questions used to assess: 1) the potential sources of bias in non-randomized or cohort studies, 2) the quality of a study, and 3) suggests use of a study in a public health context.51 The questions are designed to test the studies' quality, external validity, study bias, confounding and selection bias, and the power of the study. Any discrepancies in selection process, methodological quality assessment, and data extraction was resolved by discussion or if needed, a third reviewer. A larger total number indicates more satisfied items and thus, articles at less risk of bias.
Table 1.
Modified Downs and Black for Study Quality Checklist
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bak et al (1999)53 | Y | Y | Y | N | Y | Y | N | Y | Y | Y | Y | Y | N | 10 |
| Salmon et al (2005)11 | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | N | 11 |
| Wright et al (2006)57 | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | N/A | N | N | 9 |
| Shelbourne et al (2009)17 | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | N/A | N | N | 9 |
| Bourke et al (2012)18 | Y | N | Y | N | Y | Y | Y | Y | Y | Y | N | N | N | 8 |
| Paterno et al (2014)38 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N/A | N | N | 10 |
| Heijne et al (2015)58 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N/A | N | N | 10 |
| Kaeding et al (2015)52 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | 12 |
| Maletis et al (2015)39 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N/A | N | N | 10 |
| Kyritsis et al (2016)49 | Y | Y | Y | N | N | Y | Y | N/A | N | Y | Y | Y | N | 8 |
| Webster and Feller et al (2016)26 | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | N | 11 |
Mean study quality was a 9.82 out of a total of 13 points
Data Extraction/Analysis/Synthesis
Sample size at baseline and follow-up time were recorded for each article. The number of men and women, patients' age, number of each graft and the reported patients' demographics were also recorded. The primary variables that were extracted include the number or percentage of ipsilateral graft injuries, number of contralateral ACL injuries, and the time of second injury per sex, graft types, and patients' age. However, age at injury was unable to be further researched as only two articles grouped their participants based on their ages.17,26 Age ranges for these articles were overlapping thus making it difficult to determine incidence rate of second injury by age. There was inconsistency among articles regarding the reported data; therefore, the corresponding authors of the included articles were contacted to provide information about number of men, women, and harvested grafts. Additionally, corresponding authors were also asked to provide information regarding the number of ipsilateral graft and contralateral ACL injuries per sex and graft types. Responses with data were received from five authors,17,19,26,49,55 while another author indicated that the archived data was no longer accessible.52
STATISTICAL METHODS
The counts of injuries per limb side, sex, age, and graft type were extracted from each article. The pooled rate of second injury to both the ipsilateral graft and contralateral ACL was calculated by the total number of injured patients to the total number of patients. To determine the pooled rate of second injury in men and women, the pooled number of injured patients of one sex was compared to the total number of patients of that sex. Rates were then calculated for each injured limb side. The pooled rate of second injury for each graft type was calculated by the pooled number of second injury per graft type to the total number of patients who had the same graft type; again, the rates of second ACL injuries were calculated per limb side. Two independent proportions analysis was used to determine the significant differences in second ACL injuries between limb sides (ipsilateral graft and contralateral ACL), sexes, and graft types.
Frequency counts were used for each article that reported demographic information (sex, age, height, and weight), graft type, and timing of second injury. Pooled dichotomous data for the outcomes of interest were analyzed using random effect proportion meta-analysis (weighted effect size for each article, odds ratio, relative risk, and 95% CIs) using StatsDirect Statistical Software (V.3.1.1, Altrincham, UK). The random effects model was used in this meta-analysis to account for the heterogeneity of the included articles.56 Publication bias to the results of this meta-analysis was assessed by Funnel plots,57 with Harbord-Egger regression test used as a bias indicator and to assess asymmetry of funnel plots.58
RESULTS
Demographic
From the 11 included articles, the pooled number of patients was 24,352, of whom 23,579 patients completed the follow-up (Pooled mean±SD: 45.7 ± 19.38 months; ranges 12-60 months) and were included in this analysis. The pooled mean percentage of men included in the articles [56.15 ± 18.76% (n = 14,720)] was significantly higher than that of women [36.54 ± 17.54% (n = 8,859)] (p = 0.02) (Table. 2), with one article having only men participants.49 The pooled mean age for participants was 23.96 + 4.42 years. From the available data, 7,769 (33.04%) of the patients had BPTB autograft, 7,788 (33%) had HT autograft, 7,921 (33.69%) had allograft, and 34 (0.145%) had an iliotibial band autograft.52 (Table. 2)
Table 2.
Demographic and graft types data from the included studies
| Study | Age (year) | # of patients (women/men) | BPTB | HT | Allograft | Iliotibial band |
|---|---|---|---|---|---|---|
| Bak et al (1999)53 | Median:22(16-39) | 40 (28/12) | NR | NR | NR | 34 |
| Salmon et al (2005) 11 | Median: 28 (range: 14-62) | 672 (383/289) | 248 | 364 | NR | NR |
| Wright et al (2006)57 | 24(11-54) | 235 (125/110) | 102 | 115 | 17 | NR |
| Shelbourne et al (2009)17 | Mean: 21.6 ± 3.6 | 1415 (863/552) | 1415 | NR | NR | NR |
| Bourke et al (2012)18 | Mean: 29 (range:13-62) | 673 (432/241) | 314 | 359 | NR | NR |
| Paterno et al (2014)38 | 17.1 ± 3.1 | 78 (19/59) | 39 | 33 | 6 | NR |
| Heijne et al (2015)58 | 29 ± 7/30 ± 9 | 68 (36/32) | 34 | 34 | NR | NR |
| Kaeding et al (2015)52 | Mean: 27 ± 11 | 2488 (1365/1123) | 1131 | 891 | 466 | NR |
| Maletis et al (2015)39 | Median: 27.2(18.7-37.7) | 17436 (11111/6325) | 4436 | 5568 | 7432 | NR |
| Kyritsis et al (2016)49 | 21 ± 4; 22 ± 5 | 158 (158/0) | 50 | 108 | NR | NR |
| Webster and Feller et al (2016)26 | 17.2 (11-19) | 316 (200/116) | NR | 316 | NR | NR |
BPTB = Bone patellar tendon bone autograft ; HT = hamstring tendon autograft; NR = not reported
Second Injuries by Limb Side
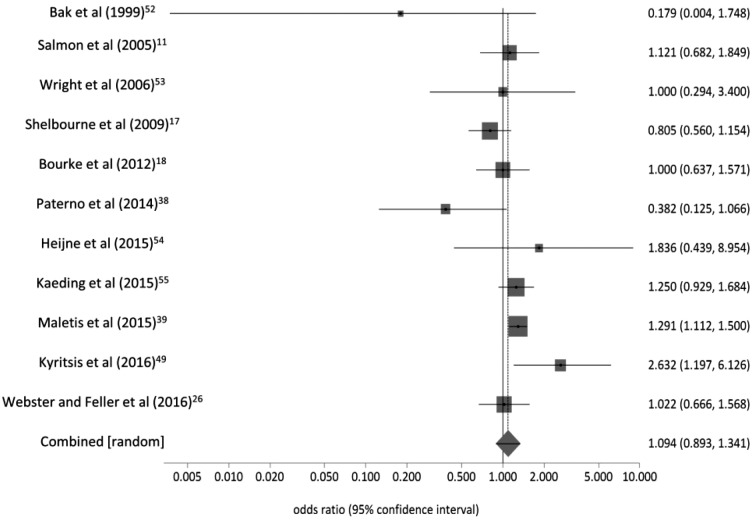
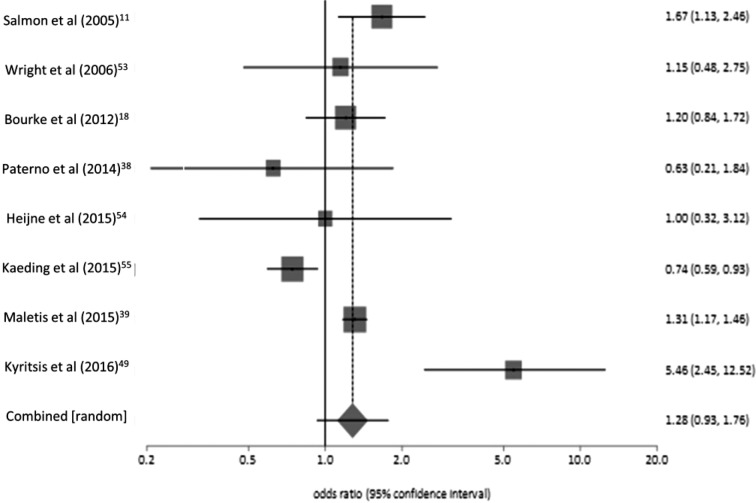
The pooled rate of second ACL injuries (ipsilateral graft and contralateral ACL injuries) was 6.11% (n = 1,441). The pooled rate of ipsilateral graft injuries of 3.29% (n = 775) was significantly higher than contralateral ACL injuries of 2.82% (n = 666) (p = 0.004), with a non-significant pooled odds ratio of 1.09 (95% CI:0.89, 1.34; p = 0.38; I2 = 51.5% [95% CI:0%, 74%]; Harbord-Egger = -0.95[(92.5% CI:-2.40, 0.51] p = 0.22) (Figure 2). Of those who had a second ACL injury, 53.8% (775/1,441) of the injuries occurred to the ipsilateral graft and 46.22% (666/1,441) to the contralateral ACL. The pooled relative risk of sustaining an ipsilateral graft injury compared to a contralateral ACL injury was 1.09 ((95% CI: 0.09, 1.32) (p = 0.38); I2 = 51.5% [95%CI: 0%, 74%]; Harbord-Egger = -1.00 [92.5% CI:-2.52, 0.51] p = 0.22). Three articles reported that a total of 17 patients sustained a second injury in both limbs after ACL.11,26,39 Five articles reported the time of ipsilateral graft injury,11,17,26,38,59 with the pooled mean time of ipsilateral graft injuries being 25.56 months (Median:20 months; range:7-60 months). The time of contralateral ACL injury was reported in six articles,11,17,26,38,49,59 with the pooled mean time of contralateral ACL injuries being 47.3 months (Median: 36.3 months; range: 16-84 months).
Figure 2.
Pooled odds ratio of ipsilateral graft and contralateral ACL injuries after ACLR regardless of the sex and graft types (Odd ratio, 95% CI, [Random effects]).
Second Injury by Sex
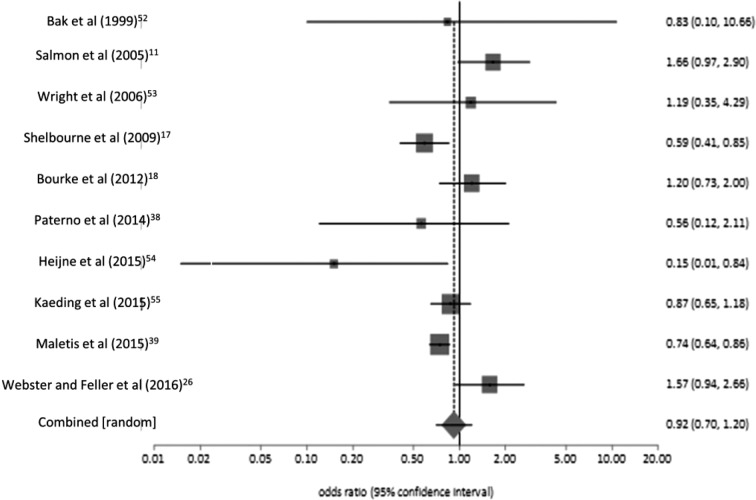
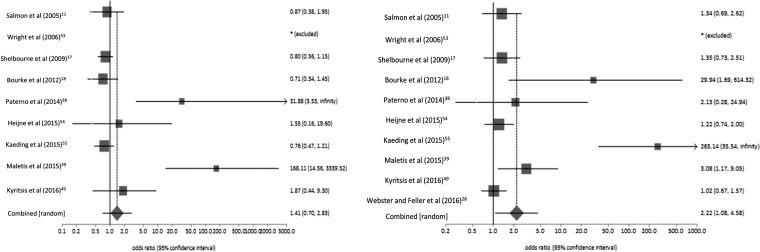
A total of 14,720 men and 8,859 women participants were included in the analysis of this study, with one article included only men participants.49 The pooled rate of second ACL injuries in men 5.67% (n = 835) was significantly lower than in women 6.84% (n = 606) (p = 0.0003), with the pooled odds ratio of second ACL injury in men and women of 0.92 (95CI%: 0.70, 1.20; p = 0.57; I2 = 66.5% [95% CI:19.3%, 81.2%]; Harbord-Egger = 0.53 [92.5% CI:-1.43, 2.50, p = 0.59]) (Figure 3). Of those who had an injury, 57.95% (835/1,441) of injuries occurred in men and 42.05% (606/1,441) in women. The pooled relative risk of second ACL injury in men compared to women was 0.92 (95% CI: 0.73, 1.7, p = 0.49; I2 = 67.7% [95% CI:23.5%, 81.8%]; Harbord-Egger = 0.45 (92.5% CI:-1.75, 2.65) p = 0.69)
Figure 3.
Pooled odds ratio of second ACL injuries between men and women after ACLR regardless of the limb side and graft types (Odd ratio, 95% CI, [Random effects]).
Men had a significantly higher pooled rate of ipsilateral graft injuries 3.40% (n = 501) than that of the contralateral ACL injuries 2.26% (n = 334) (p<0.00001), with pooled odds ratio of ipsilateral graft and contralateral ACL injuries of 1.53 (95 CI%:1.33, 1.77; p = 0.0001; I2 = 0% [95% CI:0% to 51.2%]; Harbord-Egger = -0.38 [92.5% CI:-1.29. 0.53] p = 0.42) (Figure 4 A). Of the injured men, 60.0% of the injuries occurred in the ipsilateral graft and 40.0% in the contralateral ACL. The pooled relative risk for men to sustain an ipsilateral graft injury compared to a contralateral ACL injury was 1.49 (95% CI: 1.30, 1.71, p<0.0001; I2 = 0% [95% CI: 0%, 51.2%]; Harbord-Egger = -0.43 [92.5% CI: -1.39, 0.52, p = 0.39])
Figure 4.
Pooled odds ratio of ipsilateral graft and contralateral ACL injuries in men (Left) and women (Right) after ACLR regardless of the graft types (Odd ratio, 95% CI, [Random effects]).
One article49 did not include women participants and another study52 reported no second ipsilateral graft injury in women. Women had a significantly higher rate of contralateral ACL injuries 3.75% (n = 332) than ipsilateral graft injuries 3.09% (n = 274) (p = 0.016), with pooled odds ratio of ipsilateral graft and contralateral ACL injuries of 0.73 (95% CI:0.55-0.96; p = 0.02; I2 = 40.4% [95% CI:0%. 71.1%]; Harbord-Egger = -1.37 [92.5% CI:-2.77, 0.03), p = 0.08]) (Figure 4 B). Of injured women, 54.79% of the injuries occurred in the contralateral ACL and 45.21% in the ipsilateral graft. The pooled relative risk for women to sustain a contralateral ACL injury compared to an ipsilateral graft injury was 1.34 (95% CI: 1.04, 1.72, p = 0.024; I2 = 37.9% [95% CI:0%, 70.1%]; Harbord-Egger = 1.38 [92.5% CI:-0.083, 2.84, p = 0.09])
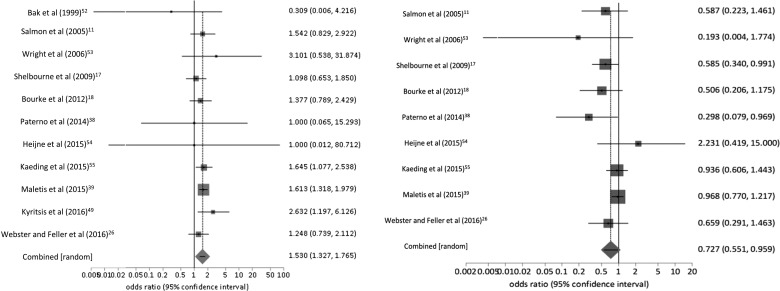
Second injuries by Graft Type
The pooled rate of second ACL injuries in patients with HT autograft of 5.83% (n = 454) was significantly higher than in those with BPTB autograft of 5.10% (n = 396 (p = 0.04) and with allograft of 3.12% (n = 247) (p<0.0001). Additionally, the pooled rate of second ACL injuries in patients with BPTB autograft was significantly higher than those with an allograft (p<0.0001). The pooled odds ratio of second ACL injuries in HT and BPTB autografts, regardless of the sex, was 1.28 (95% CI:0.93, 1.76; p = 0.058, I2 = 0% [95% CI: 0%. 58.5%]); Harbord-Egger = -0.27 [92.5% CI:-0.91, 0.37, p = 0.39]) (Figure 5). The pooled relative risk of patients with HT autograft to sustain a second ACL injury compared to patients with BPTB autograft was 1.16 (95% CI:0.99, 1.35, p = 0.06); I2 = 0% [95% CI:0%, 58.5%]; Harbord-Egger = -0.40 [92.5% CI:-1.20, 0.39, p = 0.31])
Figure 5.
Pooled odds ratio of second ACL injuries between HT and BPTB autografts after primary ACLR regardless of limb and sex (Odd ratio, 95% CI) [Random effects]).
One of the articles reported that six ipsilateral graft injuries occurred in patients who had an autograft; however, the type of the harvested tissue was not specified.53 Two articles did not use HT autograft,17,52 and three articles did not use BPTB autograft.26,52 The number of ipsilateral graft injuries in patients who had an allograft was reported in four articles (pooled number = 240),38,39,53,55 and one article reported the second injury in the contralateral ACL (n = 7);55 therefore, determining the pooled odds ratio of ipsilateral and contralateral of allografts was not possible.
The pooled rate of ipsilateral graft injuries in patients with BPTB autograft was significantly higher (2.96%) than that of the contralateral ACL injuries (2.14%) (p = 0.001) (Table 3), with pooled odds ratio of injuring ipsilateral graft and contralateral ACL injuries of 1.41 (95% CI: 0.70, 2.83; p = 0.34; I2 = 82.1% [95% CI: 62.3%, 89.2%], Harbord-Egger = 1.09 [92.5% CI:-5.26, 7.45, p = 0.72]) (Figure 6 A). The pooled relative risk of sustaining an ipsilateral graft injury compared to a contralateral ACL injury in patient with BPTB autograft was 1.35 (95% CI: 0.70, 2.61, (p = 0.37; I2 = 81.9% [95% CI: 61.7%, 89.1%]; Harbord-Egger = 1.25 [92.5% CI:-5.37, 7.87, p = 0.70])
Table 3.
Number of Ipsilateral graft and contralateral ACL injuries per graft types
| Total number of graft used | Ipsilateral graft injury | Contralateral ACL injury | Total injury | |
|---|---|---|---|---|
| BPTB autografts | 7769 | 230 (58.08%) | 166 (41.92%) | 396 (5.10%) |
| HT autografts | 7788 | 314 (69.16%) | 140 (30.84%) | 454 (5.83%) |
| Allografts | 7921 | 240 (97.17%) | 7 (2.83%) | 247 (3.12%) |
| Iliotibial band | 34 | Not reported | Not reported | Not reported |
BPTB = bone patellar tendon bone; HT = hamstring tendon
Figure 6.
Pooled odds ratio of second ACL injuries in patients with BPTB (Left) and HS (Right) autografts after primary ACLR (Odd ratio, 95% CI) [Random effects]).
The pooled odds ratio of injuring the ipsilateral graft and contralateral ACL injuries in patients with HS autograft was 2.22 (95% CI: 1.08, 4.58; p = 0.031; I2 = 85% [95% CI: 70.6%, 90.7%]; Harbord-Egger = -0.78 [92.5% CI:-7.48, 5.91, p = 0.81]) (Figure 6 B). The pooled relative risk of sustaining an ipsilateral graft injury compared to a contralateral ACL injury in patient with HT autograft was 2.06 (95% CI: 10.04, 4.07, (p = 0.038); I2 = 85.9% [95% CI = 73%, 91.1%]; Harbord-Egger = -0.07 [92.5% CI:-7.23, 7.10, p = 0.98])
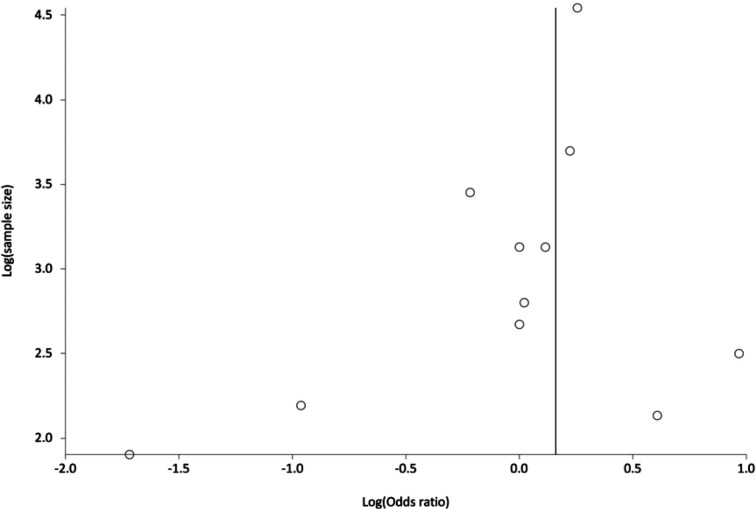
Publication Bias
The results of Harbord-Egger's regression tests ranged between -1.37 and 1.09 (p>0.08) for the odd ratios and between -1.0 and 1.38 (p>0.09), indicating no publication bias (Figure 7).
Figure 7.
Funnel plot for publication bias assessment by Log (Odds ratio).
DISCUSSION
The purpose of this systemic review and meta-analysis study was to determine the rate of ipsilateral graft and contralateral ACL injuries per patients' sex and graft types, and to explore the influence of these factors on the occurrence of second ACL injury after primary ACLR. The results of this study indicate that the overall rate of ipsilateral graft injuries was higher than the contralateral ACL injuries, regardless of sex and graft types. Ipsilateral graft injuries on average occurred earlier than the contralateral ACL injuries after primary ACLR. Additionally, the rate of second ACL injuries was higher in women compared to men. With regard to sex, men had a higher rate of ipsilateral graft injuries (3.40%) compared to contralateral ACL injuries (2.26%), while women had a higher rate of contralateral ACL injuries (3.75%) compared to ipsilateral graft injury (3.09). In all graft types, ipsilateral graft injuries were higher than contralateral ACL injuries. Both ipsilateral graft and contralateral ACL injuries were more common in patients with HT autograft followed by those with BPTB autograft, and then allografts.
While the results of this study indicate that more men had second ACL injuries, women had a higher rate of second ACL injuries and were more likely to sustain an injury to their contralateral ACL when compared to men. The trend regarding women being more likely to sustain a second ACL injury to the contralateral ACL in this study is similar to what has previously been reported in several studies.17,24,35,38,39 High rates of contralateral ACL injuries in women may have resulted from adapting a protective strategy to compensate for the reconstructed limb due to the lack of confidence and fear of sustaining further injury to the reconstructed knee.60-62 As a response, women may have tended to rely mainly on their contralateral (uninjured) limb during participation in daily living and physical activities. This, in turn, may have placed an excessive load on the uninjured contralateral ACL, that over time may cause an overuse and fatigue leading to complete rupture.62 Further, women may have continued to exhibit unresolved neuromuscular and biomechanical deficits that may contribute to injuring the contralateral ACL.9,28-34
Overall, men were more likely to sustain an injury to their ipsilateral graft compared to women and the results of this study provide evidence that men are at a higher risk to injure their ipsilateral graft than the contralateral ACL. The findings of the current study support the findings of previous studies that found a high ipsilateral graft injury in men compared to women.26,39 Unfortunately, the results of the current systematic review and meta-analysis do not explain why men demonstrate a higher risk for sustaining an injury to the ipsilateral graft. These injuries may be due to the number of men who return to participate in high-demand physical activities after ACLR as compared to women. Authors in previous studies have reported that younger men are more likely to return to their preinjury level of sports, which include mainly cutting and pivoting activities.13,63 Therefore, men returning to sport activities may, as a consequence, expose the newly harvested graft to an excessive mechanical load thus resulting in ipsilateral graft failure.
The results of the current study agree that ipsilateral graft injury occurred earlier post-operatively than the contralateral ACL injury, similar to what has been previously reported in other studies.11,17,18,26,38,49,59,64 Paterno and colleagues38 reported that 50% of the athletes with second ACL injuries sustained their injury during the first 72 sport exposures. After ACLR, the graft tissues undergo remodeling processes during the first year, which may affect the mechanical properties of the harvested graft tissue. Although, functional deficits may have been resolved prior to returning to high-demand physical activities, exposing the harvested graft (which continues to mature over time) to high loading may lead to graft failure. Recently, Nageli and Hewett recommended delaying return to sport activities for up to two years in order to preserve the graft tissue.65
Sustaining a second ACL injury, either to the ipsilateral graft or contralateral ACL, is devastating for both the injured patient and health care providers. While it is unclear why the second injury occurred, early return to high-level sport activities may put patient more at risk.13,25,63,66 Early ( ≤ 9 months after ACLR) return to sport and participation in high demand physical activities without fully resolving the patients' functional deficits may contribute to second ACL injury.29,67,68 Several authors have reported that young athletes ( ≤ 25 years)25 who return to sports are at risk for sustaining a second ACL injury.11,15,17,19,25,64,69 Other factors that may also contribute to a second ACL injury include, but are not restricted to, the risk factors that caused the primary ACL injury,9,70 inadequate rehabilitation after ACLR, returning to participate in physical activities without being rehabilitated to meet the demand of the activities,34,71-76 or clearing patients to return to their activities without using robust objective criteria that are sensitive to determine the patients' physical deficits.29,67,77-79
In this analysis, only four out of 11 articles reported using an allograft for reconstructive surgery. Patients who had an allograft sustained more injuries to the ipsilateral graft than to the contralateral ACL. This finding is consistent with what has been reported in the literature. However, computing the odds ratio for patients who had an allograft (between ipsilateral and contralateral limbs) was not possible due to the small number of studies that reported use of an allograft, of which only one reported a contralateral ACL injury. Fewer studies reporting the use of an allograft might be due to the fact that the current standard for graft option is an autograft instead of an allograft.80-82
Second ACL injuries, after primary ACLR, were more common in patients with hamstring tendon autograft followed by BPTB autograft, and then allograft. Furthermore, patients who had hamstring tendon autograft, BPTB autograft, or allograft demonstrated higher ipsilateral graft injury compared to the contralateral ACL injury. Patients with HT autograft were more likely to sustain an ipsilateral graft injury compared to contralateral ACL injury, with an odds ratio of 2.22 for patients with HS autograft injuring their ipsilateral graft compared to the contralateral ACL. The results of this study support the findings of previous studies that report HT autograft patients sustain more second ACL injury compared to BPTB autograft patients.23,47,48 The studies included in this meta-analysis did not report the ipsilateral graft injury per sex. Therefore, stratifying second ACL injuries between sexes per graft types was not possible.
Although this systematic review and meta-analysis studied only the influence of patients' sex and graft types on ipsilateral graft and contralateral ACL injuries, other studies have indicated an influence of BMI, race, graft size, family history, age, abnormal joint biomechanics, and return to activity levels on second ACL injury.7-9,11,13,18,19,23-26,42-44,63,83 Bourke et al. noted a correlation between family history of ACL ruptures and second injury to the ipsilateral limb.59 As reported by Maletis et al,39 higher BMI could contribute to decreased risk for second ACL injuries, potentially due to the fact that patients of higher BMI do not return to sport or high level activities. Maletis et al39 also noted that patients of African-American descent had a lower risk of second injury; however, the researchers were unable to determine the reasons for this observation. Many of the risk factors appraised in the articles are non-modifiable factors including sex, race, and family history. Other risk factors are modifiable at the time of the surgical procedure, during the post-surgical rehabilitation, or during the decision-making process to clear patients for return to preinjury activity levels. Bourke et al.59 indicated that a higher risk of contralateral injury might be due to an overall lack of a central protective mechanism after primary ACL injury. Bourke et al59 noted that there might be high “cost” to the body when harvesting the BPTB compared to the HT which, in return, produces greater neuromuscular control deficits. Kaeding et al55 attributed the increased risk of ipsilateral second injury with use of HT autografts to the decreased graft diameter compared to BPTB autografts. Similarly, Shelbourne et al17 reported that anatomical differences between men and women continue to play a role in sustaining a second injury. After ACL reconstruction, the graft is typically larger than the native ACL in women; therefore, a potential risk of injury to the contralateral limb is present since it is comparatively “smaller” and unable to sustain the same amount of tensile forces as the reconstructed ligament. However, the opposite may be true in men, thus placing them at an increased risk of second injury to the ipsilateral limb.
Articles were appraised using a modified checklist to assess the potential sources of bias and the quality of a study. All articles were scored at eight or higher out of a total possible score of 13, suggesting that all included articles were of acceptable to high quality. Additionally, a random effects model was performed to account for heterogeneity or variability explained by the difference between included studies.56 This allowed the authors to account for any unexplained heterogeneity between studies and provide an estimate of the odds ratio for each outcome variable.
Limitations
The articles included in this meta-analysis reported findings from data collected within the first five years after ACLR. Thereby, one limitation of this meta-analysis is that the rates of second ACL injuries per limb side, sex, and graft type are not time-specific as second ACL injury may have occurred at any time within the five years after surgery. This, in turn, may limit the generalizability of this study's findings to a specific follow-up time after ACLR. Another limitation of this meta-analysis was related to the inconsistency in the reported data and findings across articles regarding the patients' age, number of men and women, and time of follow-ups. This may cause a publication bias that led to underestimating the rate of second ACL injuries. In this meta-analysis, however, publication bias does not appear to be an issue as Harbord-Egger test was not significant for any of the measures at a confidence interval of 92.5%. The articles included in the meta-analysis did not consistently report the second ACL injury per limb side, sex, graft type, and the mechanism of injury for the primary ACL injury which prevented advanced statistical analysis to account for or discern the influence of multiple factors simultaneously. An additional limitation was associated with the reporting of mechanism of injury for the second ACL injury, only two articles reported the contact mechanism of injury for the second ACL injuries (Salmon 200511 [ipsilateral graft injury:17; contralateral ACL:10]; Webster 201419 [ipsilateral graft injury:16; contralateral ACL injury:15] and only three articles reported the non-contact mechanism of injury for the second ACL injury (Salmon 200511 [graft injury:22; contralateral ACL:25]; Webster 201419 [graft injury:10; contralateral ACL injury:26]; and Paterno 38 [23 injuries, but did not specify for graft and contralateral ACL injuries]. Further, this study is limited as to whether the patients of the included articles did or did not return to their preinjury sport participation, because it was not reported. Further studies may consider investigating the impact of returning to the preinjury sport activities on the incidence of second ACL injury. A final limitation was related to the lack of a uniform method used to confirm a second ACL injury.
CONCLUSIONS
The results of this systematic review and meta-analysis indicate that ipsilateral graft injury occurs more frequent than a contralateral ACL injury after primary ACLR, regardless of the sex and graft type, with ipsilateral graft injuries occurring earlier (post-operatively) than contralateral injuries. Second ACL injury of both ipsilateral graft and contralateral ACL are more common among women compared to men. Men are more likely to sustain an injury to ipsilateral graft while women are more likely to sustain an injury to the contralateral ACL. Patients with HT autograft demonstrate a higher rate of sustaining a second ACL injury to either limb, followed by patients with BPTB autograft, and allograft respectively. Regardless of graft type, ipsilateral graft injuries are more common than contralateral injuries.
REFERENCES
- 1.Marx RG Jones EC Angel M Wickiewicz TL Warren RF. Beliefs and attitudes of members of the american academy of anterior cruciate ligament Injury. Arthroscopy. 2003;19(7):762-770. [DOI] [PubMed] [Google Scholar]
- 2.Beynnon BD Johnson RJ Abate JA, et al. Treatment of anterior cruciate ligament injuries, part I. Am J Sports Med. 2005;33(10):1579-1602. [DOI] [PubMed] [Google Scholar]
- 3.Myklebust G Bahr R. Return to play guidelines after anterior cruciate ligament surgery. Br J Sports Med. 2005;39(3):127-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roos EM Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spindler KP Wright RW. Anterior cruciate ligament tear. N Engl J Med. 2008;359(20):2135-2142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lynch AD Logerstedt DS Grindem H, et al. Consensus criteria for defining “successful outcome” after ACL injury and reconstruction: a Delaware-Oslo ACL cohort investigation. Br J Sports Med. 2013;49(5):335-342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hui C Salmon LJ Kok A Maeno S Linklater J Pinczewski LA. Fifteen-year outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft for “isolated” anterior cruciate ligament tear. Am J Sports Med. 2011;39(1):89-98. [DOI] [PubMed] [Google Scholar]
- 8.Leys T Salmon L Waller A Linklater J Pinczewski L. Clinical results and risk factors for reinjury 15 years after anterior cruciate ligament reconstruction: a prospective study of hamstring and patellar tendon grafts. Am J Sports Med. 2012;40(3):595-605. [DOI] [PubMed] [Google Scholar]
- 9.Paterno M V. Schmitt LC Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968-1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shelbourne KD Muthukaruppan Y. Subjective results of nonoperatively treated, acute, isolated posterior cruciate ligament injuries. Arthroscopy. 2005;21(4):457-461. [DOI] [PubMed] [Google Scholar]
- 11.Salmon L Russell V Musgrove T Pinczewski L Refshauge K. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthrosc - J Arthrosc Relat Surg. 2005;21(8):948-957. [DOI] [PubMed] [Google Scholar]
- 12.Wright RW Magnussen RA Dunn WR Spindler KP. Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction: a systematic review. J Bone Joint Surg Am. 2011;93(12):1159-1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ardern CL Taylor NF Feller JA, et al. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48(21):1543-1552. [DOI] [PubMed] [Google Scholar]
- 14.Kamath G V Murphy T Creighton RA Viradia N Taft TN Spang JT. Anterior cruciate ligament injury, return to play, and reinjury in the elite collegiate athlete: Analysis of an NCAA division I cohort. Am J Sports Med. 2014;42(7):1638-1643. [DOI] [PubMed] [Google Scholar]
- 15.Lind M Menhert F Pedersen AB. Incidence and outcome after revision anterior cruciate ligament reconstruction: results from the Danish registry for knee ligament reconstructions. Am J Sports Med. 2012;40(7):1551-1557. [DOI] [PubMed] [Google Scholar]
- 16.Magnussen RA Lawrence JTR West RL Toth AP Taylor DC Garrett WE. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthrosc - J Arthrosc Relat Surg. 2012;28(4):526-531. [DOI] [PubMed] [Google Scholar]
- 17.Shelbourne KD Gray T Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37(2):246-251. [DOI] [PubMed] [Google Scholar]
- 18.Bourke HE Salmon LJ Waller A Patterson V Pinczewski L a. Survival of the anterior cruciate ligament graft and the contralateral ACL at a minimum of 15 years. Am J Sports Med. 2012;40(9):1985-1992. [DOI] [PubMed] [Google Scholar]
- 19.Webster KE Feller JA Leigh WB, et al. Younger Patients Are at Increased Risk for Graft Rupture and Contralateral Injury After Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2014;42(3):641-647. [DOI] [PubMed] [Google Scholar]
- 20.Park SSY Oh H Park SSY Lee JH Lee SH Yoon KH. Factors predicting hamstring tendon autograft diameters and resulting failure rates after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21(5):1111-1118. [DOI] [PubMed] [Google Scholar]
- 21.Pinczewski LA Lyman J Salmon LJ Russell VJ Roe J Linklater J. A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sport Med. 2007;35(4):564-574. [DOI] [PubMed] [Google Scholar]
- 22.Bourke HE Gordon DJ Salmon LJ Waller a Linklater J Pinczewski LA. The outcome at 15 years of endoscopic anterior cruciate ligament reconstruction using hamstring tendon autograft for “isolated” anterior cruciate ligament rupture. J Bone Joint Surg Br. 2012;94(5):630-637. [DOI] [PubMed] [Google Scholar]
- 23.Maletis GB Inacio MCS Desmond JL Funahashi TT. Reconstruction of the anterior cruciate ligament: Association of graft choice with increased risk of early revision. Bone Jt J. 2013;95 B(5):623-628. [DOI] [PubMed] [Google Scholar]
- 24.Paterno M V. Rauh MJ Schmitt LC Ford KR Hewett TE. Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med. 2012;22(2):116-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wiggins AJ Grandhi RK Schneider DK Stanfield D Webster KE Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44(7):Published online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Webster KE Feller JA. Exploring the High Reinjury Rate in Younger Patients Undergoing Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2016. [DOI] [PubMed] [Google Scholar]
- 27.Reid D Leigh W Wilkins S Willis R Twaddle B Walsh S. A 10-year Retrospective Review of Functional Outcomes of Adolescent Anterior Cruciate Ligament Reconstruction. J Pediatr Orthop. 2015;37(2):133-137. [DOI] [PubMed] [Google Scholar]
- 28.Hewett TE Myer GD Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492-501 The American journal of sports medicine. [DOI] [PubMed] [Google Scholar]
- 29.Nawasreh Z Logerstedt D Cummer K Axe MJ Risberg MA Snyder-Mackler L. Do Patients failing return-to-activity criteria at 6 months after anterior cruciate ligament reconstruction continue demonstrating deficits at 2 years?? Am J Sports Med. 2016;45(5):1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Paterno M V Ford KR Myer GD Heyl R Hewett TE. Limb asymmetries in landing and jumping 2 years following anterior cruciate ligament reconstruction. Clin J Sport Med. 2007;17(4):258-262. [DOI] [PubMed] [Google Scholar]
- 31.Schmitt LC, Paterno M V. Hewett TE. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sport Phys Ther. 2012;42(9):750-759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Di Stasi S Hartigan EH Snyder-Mackler L. Sex-specific gait adaptations prior to and up to 6 months after anterior cruciate ligament reconstruction. J Orthop Sport Phys Ther. 2015;45(3):207-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Roewer BD, Di Stasi SL Snyder-Mackler L. Quadriceps strength and weight acceptance strategies continue to improve two years after anterior cruciate ligament reconstruction. J Biomech. 2011;44(10):1948-1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hartigan EH Axe MJ Snyder-Mackler L. Time line for noncopers to pass return-to-sports criteria after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2010;40(3):141-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ahlden M Samuelsson K Sernert N Forssblad M Karlsson J Kartus J. The Swedish national anterior cruciate ligament register: A report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med. 2012;40(10):2230-2235. [DOI] [PubMed] [Google Scholar]
- 36.Hewett TE Myer GD Ford KR. Anterior cruciate ligament injuries in female athletes: Part 1, mechanisms and risk factors. Am J Sports Med. 2006;34(2):299-311. [DOI] [PubMed] [Google Scholar]
- 37.Renstrom P Ljungqvist A Arendt E, et al. Non-contact ACL injuries in female athletes: an International Olympic Committee current concepts statement. Br J Sports Med. 2008;41(4):20-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Paterno M V. Rauh MJ Schmitt LC Ford KR Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42(7):1567-1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Maletis GB Inacio MCS Funahashi TT. Risk factors associated with revision and contralateral anterior cruciate ligament reconstructions in the kaiser permanente ACLR registry. Am J Sports Med. 2015;43(3):641-647. [DOI] [PubMed] [Google Scholar]
- 40.Tan SHS Lau BPH Khin LW Lingaraj K. The importance of patient sex in the outcomes of anterior cruciate ligament reconstructions. Am J Sports Med. 2016;44(1):242-254. [DOI] [PubMed] [Google Scholar]
- 41.Ryan J Magnussen R a Cox CL Hurbanek JG Flanigan DC Kaeding CC. ACL reconstruction: do outcomes differ by sexϿ. A systematic review. J Bone Joint Surg Am. 2014;96(6):507-512. [DOI] [PubMed] [Google Scholar]
- 42.Mascarenhas R Erickson BJ Sayegh ET, et al. Is there a higher failure rate of allografts compared with autografts in anterior cruciate ligament reconstruction: A systematic review of overlapping meta-analyses. Arthrosc - J Arthrosc Relat Surg. 2015;31(2):364-372. [DOI] [PubMed] [Google Scholar]
- 43.Engelman GH Carry PM Hitt KG Polousky JD Vidal AF. Comparison of allograft versus autograft anterior cruciate ligament reconstruction graft survival in an active adolescent cohort. Am J Sports Med. 2014;42(10):2311-2318. [DOI] [PubMed] [Google Scholar]
- 44.Taylor DC DeBerardino TM Nelson BJ, et al. Patellar tendon versus hamstring tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2009;37(10):1946-1957. [DOI] [PubMed] [Google Scholar]
- 45.Mohtadi NG Chan DS Dainty KN Whelan DB. Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane database Syst Rev. 2011;(9):CD005960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Freedman KB D'Amato MJ Nedeff DD, et al. Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med. 2003;31(1):2-11. [DOI] [PubMed] [Google Scholar]
- 47.Persson A Fjeldsgaard K Gjertsen J-E, et al. Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction. Am J Sports Med. 2013;42(2):285-291. [DOI] [PubMed] [Google Scholar]
- 48.Reinhardt KR Hetsroni I Marx RG. Graft selection for anterior cruciate ligament reconstruction: a level I systematic review comparing failure rates and functional outcomes. Orthop Clin North Am. 2010;41(2):249-262. [DOI] [PubMed] [Google Scholar]
- 49.Kyritsis P Bahr R Landreau P Miladi R Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50(15):bjsports-2015-095908. [DOI] [PubMed] [Google Scholar]
- 50.Thompson SM Salmon LJ Waller A Linklater J Roe JP Pinczewski LA. Twenty-year outcome of a longitudinal prospective evaluation of isolated endoscopic anterior cruciate ligament reconstruction with patellar tendon or hamstring autograft. Am J Sports Med. 2016;44(12):3083-3094. [DOI] [PubMed] [Google Scholar]
- 51.Downs SH Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377-384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bak K Jorgensen U Ekstrand J Scavenius M. Results of reconstruction of acute ruptures of the anterior cruciate ligament with an iliotibial band autograft. Knee Surg Sports Traumatol Arthrosc. 1999;7(2):111-117. [DOI] [PubMed] [Google Scholar]
- 53.Wright RW Dunn WR Amendola A, et al. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: A prospective MOON cohort study. Am J Sports Med. 2007;35(7):1131-1134. [DOI] [PubMed] [Google Scholar]
- 54.Heijne A Hagstromer M Werner S. A two- and five-year follow-up of clinical outcome after ACL reconstruction using BPTB or hamstring tendon grafts: a prospective intervention outcome study. Knee Surg Sports Traumatol Arthrosc. 2015;23(3):799-807. [DOI] [PubMed] [Google Scholar]
- 55.Kaeding CC, Pedroza a. D Reinke EK, et al. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: Prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015:1583-1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Thorlund K Imberger G Johnston BC, et al. Evolution of heterogeneity (I2) estimates and their 95% confidence intervals in large meta-analyses. PLoS One. 2012;7(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sterne JAC Egger M. Funnel plots for detecting bias in meta-analysis: Guidelines on choice of axis. J Clin Epidemiol. 2001;54(10):1046-1055. [DOI] [PubMed] [Google Scholar]
- 58.Harbord RM Egger M Sterne JAC. A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Stat Med. 2006;25(20):3443-3457. [DOI] [PubMed] [Google Scholar]
- 59.Bourke HE Salmon LJ Waller A Patterson V Pinczewski LA. Survival of the anterior cruciate ligament graft and the contralateral ACL at a minimum of 15 years. Am J Sports Med. 2012;40(9):1985-1992. [DOI] [PubMed] [Google Scholar]
- 60.Ardern CL Webster KE Taylor NF Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45(7):596-606. [DOI] [PubMed] [Google Scholar]
- 61.Chmielewski TL Jones D Day T Tillman SM Lentz T a George SZ. The association of pain and fear of movement/reinjury with function during anterior cruciate ligament reconstruction rehabilitation. J Orthop Sports Phys Ther. 2008;38(12):746-753. [DOI] [PubMed] [Google Scholar]
- 62.Andriacchi TP Mündermann A Smith RL Alexander EJ Dyrby CO Koo S. A framework for the in vivo pathomechanics of osteoarthritis at the knee. Ann Biomed Eng. 2004;32(3):447-457. [DOI] [PubMed] [Google Scholar]
- 63.Ardern CL Webster KE Taylor NF Feller JA. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery: two-thirds of patients have not returned by 12 months after surgery. Am J Sports Med. 2011;39(3):538-543. [DOI] [PubMed] [Google Scholar]
- 64.Borchers JR Pedroza A Kaeding C. Activity level and graft type as risk factors for anterior cruciate ligament graft failure: A case-control study. Am J Sports Med. 2009;37(12):2362-2367. [DOI] [PubMed] [Google Scholar]
- 65.Nagelli C V. Hewett TE. Should return to sport be delayed until 2 years after anterior cruciate ligament reconstruction? Biological and functional considerations. Sport Med. 2017;47(2):221-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Webster K Feller J Richmond A. Anterior cruciate ligament reconstruction: Incidence and risk factors for graft failure and contralateral rupture. J Sci Med Sport. 2012;15:127-187. [Google Scholar]
- 67.Nawasreh Z Logerstedt D Cummer K Axe M Risberg MA Snyder-Mackler L. Functional performance 6 months after ACL reconstruction can predict return to participation in the same preinjury activity level 12 and 24 months after surgery. Br J Sports Med. 2018;52(6):375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Grindem H Snyder-Mackler L Moksnes H Engebretsen L Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50(13):804-808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Barrett AM Craft J a Replogle WH Hydrick JM Barrett GR. Anterior cruciate ligament graft failure: a comparison of graft type based on age and Tegner activity level. Am J Sports Med. 2011;39(10):2194-2198. [DOI] [PubMed] [Google Scholar]
- 70.Di Stasi S Myer GD Hewett TE. Neuromuscular training to target deficits associated with second anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2013;43(11):777-792, A1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.de Jong SN van Caspel DR van Haeff MJ Saris DBF. Functional assessment and muscle strength before and after reconstruction of chronic anterior cruciate ligament lesions. Arthroscopy. 2007;23(1):21-28, 28.e1-3. [DOI] [PubMed] [Google Scholar]
- 72.Keays SL Bullock-Saxton J Keays AC Newcombe P. Muscle strength and function before and after anterior cruciate ligament reconstruction using semitendonosus and gracilis. Knee. 2001;8(3):229-234. [DOI] [PubMed] [Google Scholar]
- 73.White K Logerstedt D Snyder-Mackler L. Gait asymmetries persist 1 year after anterior cruciate ligament reconstruction. Orthop J Sport Med. 2013;1(2):3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Di Stasi SL Logerstedt D Gardinier ES Snyder-Mackler L. Gait patterns differ between ACL-reconstructed athletes who pass return-to-sport criteria and those who fail. Am J Sports Med. 2013;41(6):1310-1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Logerstedt D Lynch A Axe MJ Snyder-Mackler L. Symmetry restoration and functional recovery before and after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21(4):859-868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Palmieri-Smith RM Thomas AC. A neuromuscular mechanism of posttraumatic osteoarthritis associated with ACL injury. Exerc Sport Sci Rev. 2009;37(3):147-153. [DOI] [PubMed] [Google Scholar]
- 77.Barber-Westin SD Noyes FR. Objective criteria for return to athletics after anterior cruciate ligament reconstruction and subsequent reinjury rates: A systematic review. Phys Sportsmed. 2011;39(3):100-110. [DOI] [PubMed] [Google Scholar]
- 78.Barber-Westin SD Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27(12):1697-1705. [DOI] [PubMed] [Google Scholar]
- 79.Ardern CL Taylor NF Feller JA Webster KE. Return-to-sport outcomes at 2 to 7 years after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2012;40(1):41-48. [DOI] [PubMed] [Google Scholar]
- 80.Marder RA Raskind JR Carroll M. Prospective evaluation of arthroscopically assisted anterior cruciate ligament reconstruction. Patellar tendon versus semitendinosus and gracilis tendons. Am J Sports Med. 1991;19(5):478-484. [DOI] [PubMed] [Google Scholar]
- 81.Corry ISISIS Webb JMJMJM Clingeleffer AJAJAJ, Pinczewski L a LALA. Arthroscopic reconstruction of the anterior cruciate ligament. A comparison of patellar tendon autograft and four-strand hamstring tendon autograft. Am J Sports Med. 1999;27(3):444-454. [DOI] [PubMed] [Google Scholar]
- 82.Aglietti P Buzzi R Zaccherotti G De Biase P. Patellar tendon versus doubled semitendinosus and gracilis tendons for anterior cruciate ligament reconstruction. Am J Sports Med. 1994;22(2):211-217; discussion 217-218. [DOI] [PubMed] [Google Scholar]
- 83.Yabroudi MA Björnsson H Lynch AD, et al. Predictors of revision surgery after primary anterior cruciate ligament reconstruction. Orthop J Sport Med. 2016;4(9):2325967116666039. [DOI] [PMC free article] [PubMed] [Google Scholar]