Abstract
Pyogenic granuloma is a ‘reactive lesion’ in the oral cavity caused due to hormonal imbalance or poor oral hygiene. There are different methods to excise this lesion but most successful is treatment with lasers. Currently, there are different lasers available commercially and are used by clinicians to excise this lesion. In this case report, a 20-year-old female patient reported to the department with a complaint of overgrowth of gingiva on lower canine. It was excised by using neodymium-doped yttrium aluminium garnet laser and the patient was asked for regular follow-up after 1 week and 6 months. The excised lesion was sent to pathology where the lesion was confirmed to be pyogenic granuloma. The patient reported no pain, no blood loss during or postsurgery. Laser is a useful technique for excisional surgeries; it is safe, effective and reduces time of treatment as well as time of healing.
Keywords: dentistry and oral medicine, mouth
Background
Poncet and Dor,1 two French surgeons, originally explained pyogenic granuloma and termed it as botryomycosis hominis.1 Although in 1844, Hullihen2 described about this lesion, he did not termed it. In 1903, Crocker3 coined the term granuloma pyogenicum. But in the literature, some researchers mentioned the name of Hartzell4 4 who coined the term pyogenic granuloma. Pyogenic granuloma is not a correct definition as it is not a true granuloma and it does not contains pus. It is a benign, mucocutaneous lesion commonly evolves on tongue, gum, lips5 and some extraoral sites like face, nose, eyelids, neck,6 etc. As pyogenic granuloma is non-neoplastic in nature, excisional treatment is the better option. Excision can be done by using laser because the cutting is clean and almost no blood loss and also be painless. The lasers that can be used for the excision treatment are neodymium-doped yttrium aluminium garnet (Nd:YAG) laser, diode lasers, erbium-doped YAG (Er:YAG) laser, flash lamp pulsed dye laser.7 In this case report, Nd:YAG laser is used to excise the lesion without any blood loss.
Case presentation
A 20-year-old female patient reported to the outpatient department of conservative dentistry and endodontics, King George’s Medical University, with a complaint of growth of gingiva in the lower canine gingival region (figure 1) since 4 months and was increasing in size. The lesion was firm, soft and similar to the colour of gingiva. The lesion was measured around 1.0×0.8 cm. She also complained of bleeding in lesion while brushing. It was a painless lesion but was growing, which raised an alarm for the patient. There was no relevant medical history of the patient.
Figure 1.

Preoperative view of the lesion.
Investigations
Extraoral evaluation: nothing anomalous found.
Intraoral evaluation: an odd distinct gingival growth was observed on the mandibular canine region of about 1.0×0.8 cm in size. The shape of overgrown gingiva was oval and colour was reddish pink. The surface was slick. This lesion covered almost whole canine. It was painless. The oral hygiene of the patient was moderate.
Palpation: the intraoral evaluation related to size, shape, site and number was confirmed.
Treatment
After oral prophylaxis, the excision biopsy was done by using Nd:YAG laser manufactured by Fotona lasers, with the following specifications: length of the fibre 320 µm, power 2 W and frequency 20 Hz. The fibre was in contact mode with the lesion. Anaesthetic spray was sprayed on the lesion to reduce pain while excision. It took around 5 min to completely excise the lesion. Nd:YAG laser provided clean cutting of the lesion (figures 2 and 3) and maintained haemostasis. The excised lesion was sent to the pathology for further histopathological examination (figure 4). The patient was not prescribed with any analgesics or anti-inflammatory drugs. She was discharged after explaining all the postoperative precautions.
Figure 2.

Excision of the lesion by using Nd:YAG laser.
Figure 3.

Postoperative view just after the removal of lesion.
Figure 4.

Excised lesion.
Outcome and follow-up
The follow-up was done after 1 week and 6 months (figure 5).
Figure 5.

Follow-up after 6 months.
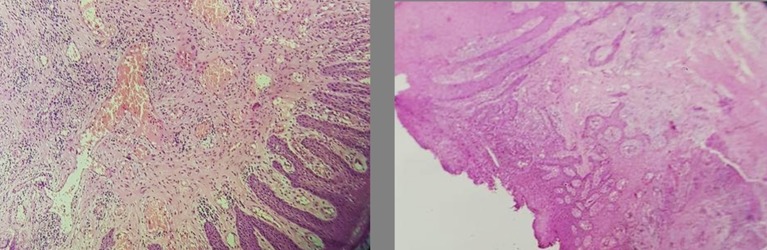
Histopathological analysis confirmed the lesion as pyogenic granuloma. The microscopic view of the granuloma showed a hyperplastic stratified squamous epithelium which showed papilomatosis and acanthosis and was partially exposed in one area (figure 6). The underlying subepithelial stroma showed congested blood vessels, capillary proliferation and lymphoplasmacytic infiltrate. Malignancy was not observed.
Figure 6.
Histopathological view of the pyogenic granuloma.
Discussion
Originally, it was thought that pyogenic granuloma was caused by pyogenic organisms.8 But now it is believed that it has no relation with infection. More often, women are affected by pyogenic granuloma due to hormonal changes in their body or while during pregnancy, but it is also common in young adults and children.9 Although pyogenic granuloma may be clinically observed approximately at any age, but it is mostly occurs at the ages between 8 years10 and 75 years.11
Basically, pyogenic granuloma is classified as:
Non-lobular capillary haemangioma (pedunculated form)—77%.
Lobular Capillary Haemangioma (sessile form)—66%.
They both show different histological features.
There are different methods that have been used to treat pyogenic granuloma like excisional biopsy, liquid nitrogen spray,12 flash lamp pumped pulsed dye laser,13 corticosteroids,14 injection of absolute alcohol,15 use of sclerosing agent like monoethanolamine oleate,16 carbon dioxide laser,17 Nd:YAG laser,5 Er:YAG laser,18 etc.
Lasers are a better option for treating pyogenic granuloma because there is a lower risk of bleeding while excision and a mild pain that is bearable. Out of all the lasers, Nd:YAG lasers are mostly chosen for excision because they have better coagulation characteristics. Lasers show no adverse effects on patients. The treatment time is very less and the healing process is fast compared with the surgical excision of pyogenic granuloma. Lasers are the successful treatment modality for pyogenic granuloma.
Fekrazard et al18 performed a laser surgery for treating a pyogenic granuloma of a 24-year-old female patient. The lesion was present on the buccal and palatal side of 5 six maxillary teeth. They used Er:YAG laser with 3 W, 10 Hz, 300 mJ and contact mode technique. The patient had no pain after the surgery and was regularly kept on follow-up for the period of 9 months. They concluded that the result was positive; it is a safe and effective technique for lesion excision.
Another case reported by Al-Mohaya19 was of a 51-year-old patient having a long history of diabetes type II and had a complaint of pyogenic granuloma covering the buccal region. It was treated by using diode laser of 940 nm in length and in contact mode. After the treatment, the patient had no pain and the healing process was fast, it was a suture-less procedure and improves homeostasis. Another case reported by Rakesh et al,20 also used diode laser to treat pyogenic granuloma of a 12-year-old patient having complaint of pyogenic granuloma in the right buccal mucosa near the angle of the mouth. The specifications of diode laser in this case were 350 μm fibre and in contact mode. The excision was successful and healing process was swift.
Kocaman et al5 used Nd:YAG laser to treat pyogenic granuloma of 14-year-old female patient having complaint of overgrown gingiva on the buccal site of her mandibular teeth (premolar). The specifications of Nd:YAG laser for the treatment were 4 W, 100mJ and 40 Hz. The excision was complete within few minutes and the excised area was healed within a month.
Another study of Truschnegg et al17 reported a case of 67-year-old male patient having a lesion around two implants in the lower jaw. The pyogenic granuloma was removed by using carbon doxide laser. The treatment process was successful without any adverse effects. After the excision, the patient was called for a follow-up and no medications were given. Healing was fast.
Another case report reported by Verma in 201421 involved a 12-year-old female patient who had a complaint of a huge lesion over growth from lower right canine to first molar. The lesion was excised by surgery, and postsurgery, the patient was advised with medications from the medicine department. The excised lesion was sent for histopathological examination.
Learning points.
Lasers are useful in treating pyogenic granuloma because while excision there is bloodless field, rapid healing and no stitches were required.
It is a painless procedure.
It reduces postoperative infection and that is why the patient does not require any medications (analgesics or antibiotics) for rapid healing or relief in pain.
This method requires less time compared with other surgical technique.
Footnotes
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Poncet A, Dor L. De La botryomycose humaine: Identite’ de nature de tumeurs d’apparance papillomateuse chez l’homme avec la botryomycose ou champignon de castration du cheval. Lyon Med 1897;86:213. [Google Scholar]
- 2.Hullihen SP. Case of aneurism by anastomosis of the superior maxillae. Am J Dent Sci 1844;4:160–2. [PMC free article] [PubMed] [Google Scholar]
- 3.Crocker HR. Diseases of skin. Philadelphia: P Blakiston’s Son & Co, 1903;2:1081. [Google Scholar]
- 4.Hartzell MB. Granuloma pyogenicum (Botryomycosis of French authors). J Cutan Dis 1904;22:520–5. [Google Scholar]
- 5.Kocaman G, Beldüz N, Erdogan C, et al. The use of surgical Nd:YAG laser in an oral pyogenic granuloma: a case report. J Cosmetic Laser Ther 2014;16:197–200. 10.3109/14764172.2014.910078 [DOI] [PubMed] [Google Scholar]
- 6.Koo MG, Lee SH, Han SE. Pyogenic granuloma: a retrospective analysis of cases treated over a 10-year. Arch Craniofac Surg 2017;18:16–20. 10.7181/acfs.2017.18.1.16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rai S, Kaur M, Bhatnagar P. Laser: a powerful tool for treatment of pyogenic granuloma. J Cutan Aesthet Surg 2011;4:144–7. 10.4103/0974-2077.85044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kamal R, Dahiya P, Puri A. Oral pyogenic granuloma: various concepts of etiopathogenesis. J Oral Maxillofac Pathol 2012;16:79–82. 10.4103/0973-029X.92978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nthumba PM. Giant pyogenic granuloma of the thigh: a case report. J Med Case Rep 2008;2:95 10.1186/1752-1947-2-95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nirmala S, Vallepu R, Babu M, Dasarraju RK. Pyogenic granuloma in an 8 year old boy – a rare case report. J Pediat Neonat Care 2016;4:00135 10.15406/jpnc.2016.04.00135 [DOI] [Google Scholar]
- 11.Shaikh S, Singh G, Singh A, et al. Pyogenic granuloma of unusual size with alveolar resorption in a 75-year-old patient. Natl J Maxillofac Surg 2012;3:75–9. 10.4103/0975-5950.102170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ishida CE, Ramos-e-Silva M, Ram M. Cryosurgery in oral lesions. Int J Dermatol 1998;37:283–5. 10.1046/j.1365-4362.1998.00426.x [DOI] [PubMed] [Google Scholar]
- 13.Tay YK, Weston WL, Morelli JG. Treatment of pyogenic granuloma in children with the flashlamp-pumped pulsed dye laser. Pediatrics 1997;99:368–70. 10.1542/peds.99.3.368 [DOI] [PubMed] [Google Scholar]
- 14.Parisi E, Glick PH, Glick M. Recurrent intraoral pyogenic granuloma with satellitosis treated with corticosteroids. Oral Dis 2006;12:70–2. 10.1111/j.1601-0825.2005.01158.x [DOI] [PubMed] [Google Scholar]
- 15.Ichimiya M, Yoshikawa Y, Hamamoto Y, et al. Successful treatment of pyogenic granuloma with injection of absolute ethanol. J Dermatol 2004;31:342–4. 10.1111/j.1346-8138.2004.tb00682.x [DOI] [PubMed] [Google Scholar]
- 16.Matsumoto K, Nakanishi H, Seike T, et al. Treatment of pyogenic granuloma with a sclerosing agent. Dermatol Surg 2001;27:521–3. [DOI] [PubMed] [Google Scholar]
- 17.Truschnegg A, Acham S, Kqiku L, et al. CO2 laser excision of a pyogenic granuloma associated with dental implants: a case report and review of the literature. Photomed Laser Surg 2016;34:425–31. 10.1089/pho.2016.4089 [DOI] [PubMed] [Google Scholar]
- 18.Fekrazad R, Nokhbatolfoghahaei H, Khoei F, et al. Pyogenic granuloma: surgical treatment with Er:YAG laser. J Lasers Med Sci 2014;5:199–5. [PMC free article] [PubMed] [Google Scholar]
- 19.Al-Mohaya MA, Al-Malik AM. Excision of oral pyogenic granuloma in a diabetic patient with 940nm diode laser. Saudi Med J 2016;37:1395–400. 10.15537/smj.2016.12.15941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rakesh N, Majumdar K, Devi YBK, et al. Pyogenic granuloma of buccal mucosa: a rare case report. JBR Journal of Interdisciplinary Medicine and Dental Science 2014;2:144 10.4172/2376-032X.1000144 [DOI] [Google Scholar]
- 21.Verma UP. Pyogenic granuloma of 12 years old female child. Int J Curr Re 2014;6:5798–9. [Google Scholar]