Abstract
An 81-year-old woman was admitted under the acute medical team with a significant acute kidney injury secondary to presumed gastroenteritis, following a 5-day history of diarrhoea and vomiting. She continued to deteriorate despite resuscitative efforts. Subsequently, a non-contrast CT scan revealed likely small bowel obstruction second to a Richter’s hernia in the inguinal canal. At diagnostic laparoscopy, both small bowel and appendix were identified to be incarcerated within the right femoral canal. The patient recovered uneventfully and was safely discharged several days following a laparoscopic appendicectomy and right femoral hernia repair.
Keywords: general surgery, gastrointestinal surgery, pathology
Background
The femoral canal, found below the inguinal ligament, is the recognised location of femoral hernias. Due to its narrow and minimally expansile nature, it leads to a high risk of incarceration and strangulation. A de Garengeot hernia describes the finding of an appendix within the femoral canal and occurs in <1% of all femoral hernia cases.1 In contrast, a Richter’s hernia, occurring in approximately 10% of all strangulated hernias, occurs when only part of the circumference of the intestine’s antimesenteric border protrudes and incarcerates through a defect in the abdominal wall.2 Here, we present a rare case of Richter’s and de Garengeot hernia found simultaneously within the same defect, leading to incarceration and small bowel obstruction. The combination presents a significant diagnostic challenge, which requires a thorough clinical work-up and prompt management. The absence of treatment guidelines also presents some difficulty in managing these patients and requires responsible clinicians to be aware of the various treatment options.
Case presentation
A 81-year-old Caucasian woman presented to A&E due to severe nausea, vomiting and an inability to keep food down for 5 days. This was associated with diarrhoea for the first 2 days, reduced to only passing minimal flatus over the subsequent 3 days. The patient denied any other symptoms including a negative systemic screen. She had no significant medical, surgical or drug history, lived alone and was completely independent.
Her initial observations were heart rate 75 bpm, blood pressure 175/80 mm Hg, respiratory rate 16, saturation 96% on 2 L via nasal cannulae and temperature 37.0°C. She was clinically dry and had mild epigastric tenderness. Rectal examination was unremarkable. There was a significant derangement of her renal function, with urea 25.3 mmol/L and creatinine 176 μmol/L. Other initial blood tests, including inflammatory markers and lactate measurements, were unremarkable. She was initially accepted by the acute medical team and treated with intravenous fluids for presumed severe dehydration secondary to gastroenteritis, leading to an acute kidney injury.
Investigations
Progressive abdominal distension occurred with no improvement of the patient’s clinical state. A plain abdominal film (figure 1) was ordered revealing evidence of small bowel obstruction, followed by a non-contrast CT scan, which suggested the cause was an incarcerated right inguinal hernia (figures 2 and 3). Further clinical review by the general surgeons did not reveal a palpable right inguinal hernia, but rather a fullness in the right femoral canal on standing, suggestive of a femoral hernia. A diagnostic laparoscopy was therefore performed, which demonstrated an incarcerated femoral hernia containing the antimesenteric border of a loop of jejunum (Richter’s hernia) as well as the tip of her appendix (de Garengeot hernia) (figure 4).
Figure 1.

Abdominal film showing small bowel dilatation.
Figure 2.

Abdominal coronal CT image showing the presence of a femoral hernia. Within the sac, a loop of small bowel (purple arrow) and appendix tip (orange arrow) was identified.
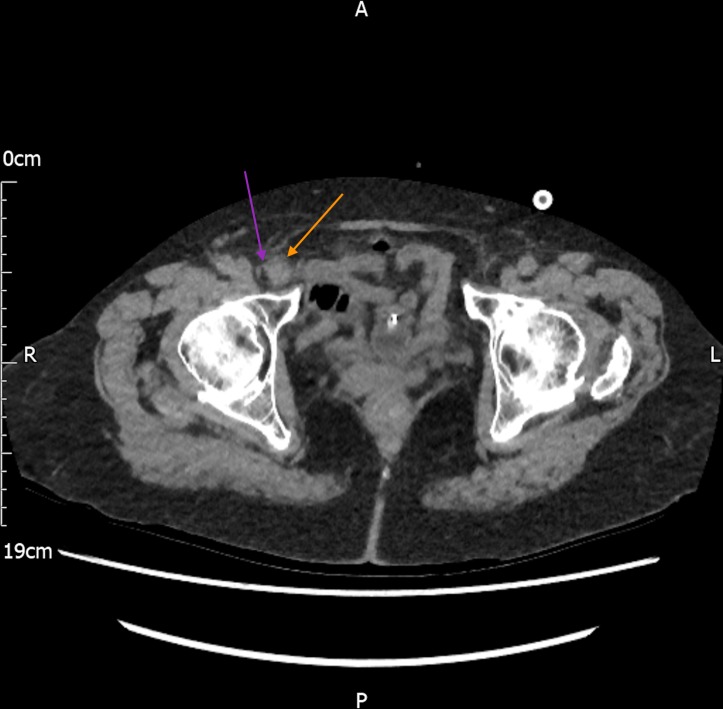
Figure 3.
Abdominal axial CT image showing the presence of a femoral hernia. Within the sac, a loop of small bowel (purple arrow) and appendix tip (orange arrow) was identified.
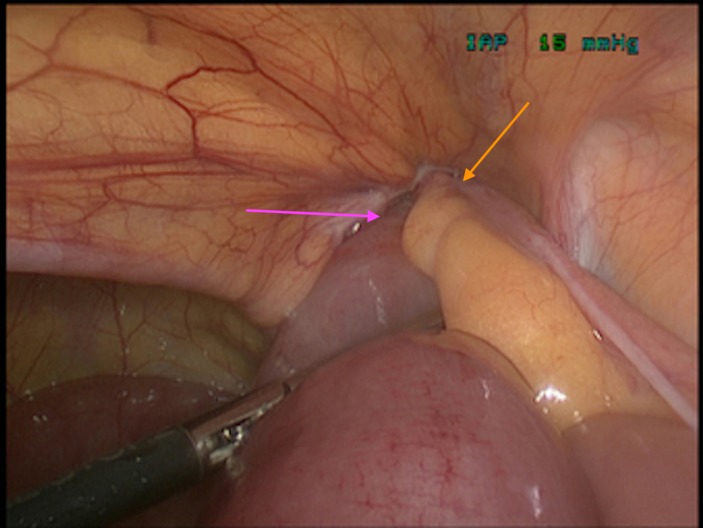
Figure 4.
Intraoperative pictures showing the presence of an incarcerated appendix (orange arrow) and antimesenteric border of jejunum within the femoral canal (purple arrow).
Treatment
A diagnostic laparoscopy was performed under general anaesthesia. An infraumbilical 10 mm port was placed using the open Hasson technique and a pneumoperitoneum achieved with 12 mm Hg of CO2. The distal appendix and a knuckle of jejunum was found within a right femoral hernia. Two further 5 mm ports were inserted under direct vision in the left iliac fossa and right lumbar region.
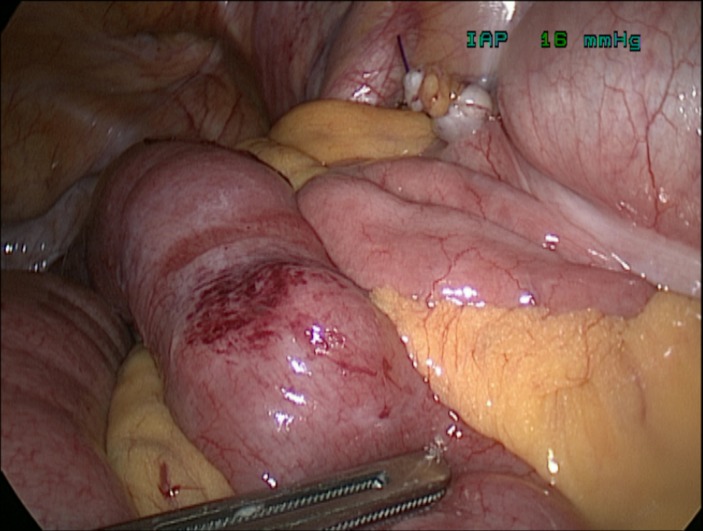
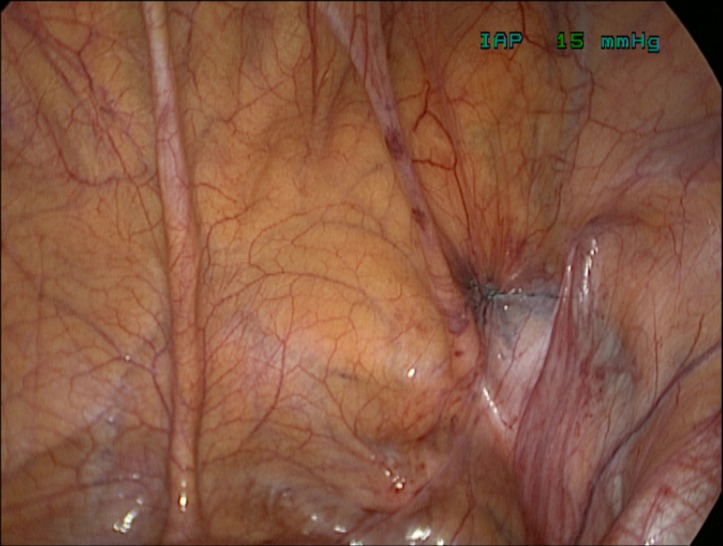
The hernia contents were reduced into the peritoneal cavity and inspected. The distal appendix was strangulated and the area of involved small bowel was bruised (figures 5 and 6). Decision was made to proceed with an appendicectomy and a right femoral hernia repair. The mesoappendix was dissected from the appendix using monopolar diathermy, secured using three Polydioxanone (PDS) endoloops and separated from its base. The small bowel was re-inspected and found to be viable, therefore no bowel resection was performed (figure 7). The defect overlying the femoral canal was closed laparoscopically with 2–0 Ethibond without mesh (figure 8).
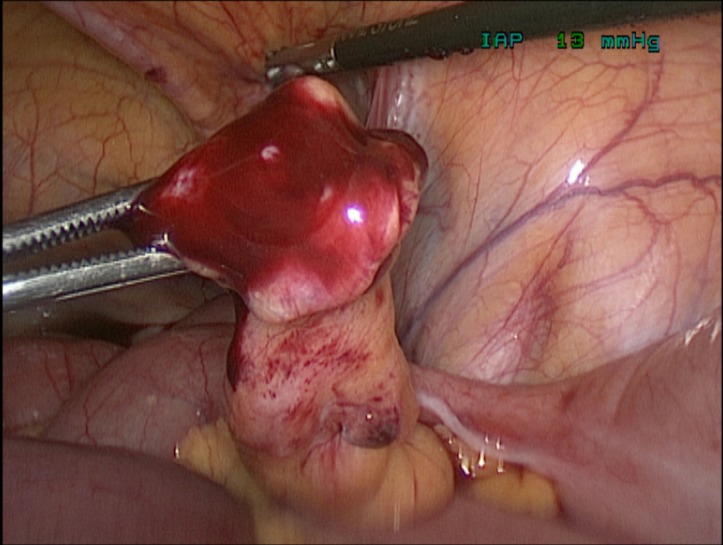
Figure 5.
Intraoperative images showing the reduced damaged appendix tip.
Figure 6.
Intraoperative images showing the reduced damaged antimesenteric border of jejunum.
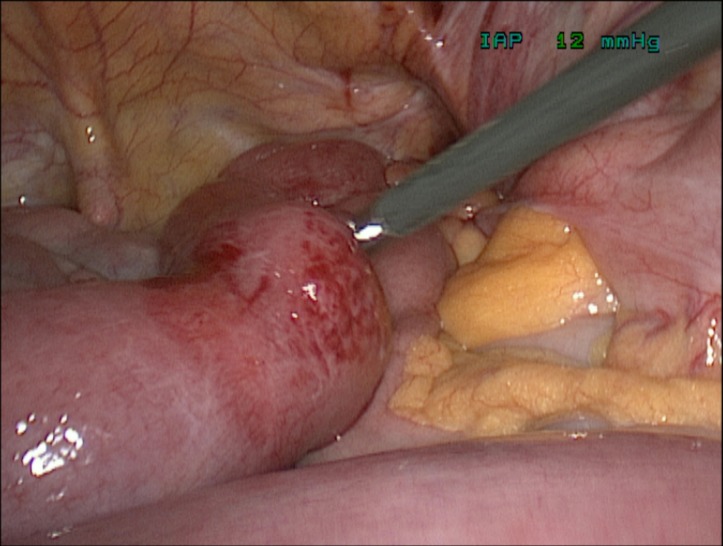
Figure 7.
Intraoperative pictures showing the appendix stump and viable jejunal loop.
Figure 8.
Intraoperative image showing the closed femoral defect.
Outcome and follow-up
Following the procedure, she was managed in HDU and was subsequently discharged from the ward on day 9. She developed no postoperative complications during her inpatient stay. Histology results revealed a non-necrotic non-dysplastic fibrotic appendix. No outpatient follow-up was required and the patient was discharged back to the care of their general practitioner.
Discussion
Femoral hernias account for approximately 4% of all groin hernias and may contain any intra-abdominal structure that is relatively mobile.3 These hernias may contain different structures, including the small or large bowel, appendix or a Meckel’s Diverticulum. Very rarely, these hernias may contain both a De Garengeot’s and Richter’s hernias.
De Garengeot’s hernias, defined by the presence of appendix inside a femoral hernia sac, are extremely rare and account for 0.9% of femoral hernias.1 De Garengeot’s hernias remain a diagnostic challenge, presenting with vague abdominal symptoms while lacking the typical clinical signs of acute appendicitis.4 Although preoperative CT scanning may be helpful in establishing the diagnosis, most cases are diagnosed intraoperatively.1 The established management of these hernias typically consists of emergency surgery with either an open or laparoscopic approach, influenced by the clinical picture. In situations where clinically there is suspicion of a femoral hernia containing a perforated appendicitis, one may consider an open approach to reduce the risk of spillage into the peritoneal cavity.4 Similarly, a laparoscopic approach may be considered in bilateral femoral hernias depending on available expertise.
Richter’s hernias, defined by the protrusion or strangulation of part of the circumference of the intestine’s antimesenteric border, are more prevalent and occur in approximately 10% of femoral hernias.2 These hernias usually contain the distal ileum and have a tendency to progress rapidly to gangrene and perforation.2 Less than two-thirds of the bowel wall is often involved, leading to a patent gut lumen and no clinical indication of bowel obstruction.2 This often leads to late diagnosis and significant bowel necrosis.5 Once diagnosis is achieved, treatment is often via a preperitoneal approach or laparotomy if significant complications are suspected.2
From our knowledge, there has only been one previous reported case of a combined De Garengeot’s and Richter’s hernia in the literature.6 The authors describe the clinical difficulty in achieving a diagnosis and suggest options for management, namely via an open approach.6
In our case, diagnosis was achieved via a thorough clinical history, examination and imaging by the surgical team. However, diagnosis was delayed initially, due to the vague presenting symptoms and failure to perform a full abdominal examination, including the hernial orifices. Interestingly, retrospective studies have revealed as many as 40% of acutely obstructed hernias are missed due to incomplete groin examination.7 CT imaging helped to identify the presence of an obstructed hernia in our case, but did not identify the presence of the appendix within the hernia sac. In the literature, only approximately 50% of these cases are diagnosed by CT imaging and therefore present a significant diagnostic challenge.3
A definitive diagnosis was only achieved after diagnostic laparoscopy, which may be considered in similar cases of diagnostic uncertainty. We opted for a laparoscopic rather than an open approach, performing an appendicectomy and femoral hernia repair for definitive treatment. A laparoscopic approach in these cases may help to reduce postoperative complications such as paralytic ileus, overall length of hospital stay and overall financial burden.8 An open approach, however, may be required if significant complications arise, such as bowel necrosis, gangrene or perforation. Decision was taken to close the femoral defect laparoscopically without mesh (figure 8), due to the potential complication of mesh infection in the presence of a damaged appendix tip (figure 5).
Learning points.
Clinical examination, including a full hernial orifices examination, is essential in the diagnosis of incarcerated hernias and ensuring timely management.
Combined Richter’s and De Garengeot’s hernia is possible, best diagnosed with CT imaging and may be treated with simultaneous hernia repair and appendicectomy.
Combined Richter’s and De Garengeot’s hernias may be treated laparoscopically, reducing postoperative complications such as ileus that are more common in an open approach.
Footnotes
Contributors: TB-UD: responsible for the conception of this case report; took the intraoperative pictures and decided on which ones to use. PS and MK: responsible for the design of the case report using the provided template, and also collected the data. PS and TB-UD: responsible for interpreting all images used. All authors contributed towards the planning and conduct of this case report and were responsible for the reporting of this case.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Garcia-Amador C, De la Plaza R, Arteaga V, et al. Garengeot’s hernia: two case reports with CT diagnosis and literature review. Open Med 2016;11:354–60. 10.1515/med-2016-0065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bay-Nielsen M, Kehlet H, Strand L, et al. Quality assessment of 26,304 herniorrhaphies in Denmark: a prospective nationwide study. Lancet 2001;358:1124–8. 10.1016/S0140-6736(01)06251-1 [DOI] [PubMed] [Google Scholar]
- 3. Skandalakis PN, Zoras O, Skandalakis JE, et al. Richter hernia: surgical anatomy and technique of repair. Am Surg 2006;72:180–4. [PubMed] [Google Scholar]
- 4. Kalles V, Mekras A, Mekras D, et al. De Garengeot’s hernia: a comprehensive review. Hernia 2013;17:177–82. 10.1007/s10029-012-0993-3 [DOI] [PubMed] [Google Scholar]
- 5. Steinke W, Zellweger R. Richter’s hernia and sir frederick treves: an original clinical experience, review, and historical overview. Ann Surg 2000;232:710–8. 10.1097/00000658-200011000-00014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Le HD, Odom SR, Hsu A, et al. A combined Richter’s and de Garengeot’s hernia. Int J Surg Case Rep 2014;5:662–4. 10.1016/j.ijscr.2014.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Whalen HR, Kidd GA, O’Dwyer PJ, et al. Femoral hernias. BMJ 2011;343:d7668 10.1136/bmj.d7668 [DOI] [PubMed] [Google Scholar]
- 8. McCormack K, Scott N. Laparoscopic techniques versus open techniques for repair of a hernia in the groin. Cochrane Library 2003. [DOI] [PMC free article] [PubMed] [Google Scholar]