Abstract
Background
Lung cancer ranks as the leading cause of cancer-related deaths worldwide and we performed this meta-analysis to investigate eligible studies and determine the prognostic effect of Ki-67.
Methods
In total, 108 studies in 95 articles with 14,732 patients were found to be eligible, of which 96 studies reported on overall survival (OS) and 19 studies reported on disease-free survival (DFS) with relation to Ki-67 expression in lung cancer patients.
Results
The pooled hazard ratio (HR) indicated that a high Ki-67 level could be a valuable prognostic factor for lung cancer (HR = 1.122 for OS, P < 0.001 and HR = 1.894 for DFS, P < 0.001). Subsequently, the results revealed that a high Ki-67 level was significantly associated with clinical parameters of lung cancer including age (odd ratio, OR = 1.246 for older patients, P = 0.018), gender (OR = 1.874 for males, P < 0.001) and smoking status (OR = 3.087 for smokers, P < 0.001). Additionally, significant positive correlations were found between Ki-67 overexpression and poorer differentiation (OR = 1.993, P = 0.003), larger tumor size (OR = 1.436, P = 0.003), and higher pathologic stages (OR = 1.867 for III-IV, P < 0.001). Furthermore, high expression of Ki-67 was found to be a valuable predictive factor for lymph node metastasis positive (OR = 1.653, P < 0.001) and advanced TNM stages (OR = 1.497 for stage III-IV, P = 0.024). Finally, no publication bias was detected in any of the analyses.
Conclusions
This study highlights that the high expression of Ki-67 is clinically relevant in terms of the prognostic and clinicopathological characteristics for lung cancer. Nevertheless, more prospective well-designed studies are warranted to validate these findings.
Electronic supplementary material
The online version of this article (10.1186/s12931-018-0843-7) contains supplementary material, which is available to authorized users.
Keywords: Ki-67, Lung cancer, Meta-analysis, Prognosis, Clinicopathological characteristics
Background
Lung cancer is the most frequent diagnosed malignant neoplasms, and it was the first cause of cancer death in 2016 globally [1]. In the United States, lung cancer accounted for 27% of all cancer deaths in 2016. Non-small cell lung cancer (NSCLC), accounting for over 80% of all lung cancers, is the major cause of death worldwide [2]. Although the treatment of NSCLC patients includes surgery, radiotherapy and chemotherapy, the progress in lung cancer treatment is still slow, for which the 5-year relative survival is currently 18%. Diagnosis at an advanced stage is the major reason for this low survival rate [3]. Several prognostic factors were well characterized in lung cancer including sex, age, loss of weight, TNM stage, LDH, neutrophilia, haemoglobin as well as serum calcium [4]. Importantly, The IASLC Lung Cancer Staging Project in 2015 also carried out the 8th edition of the anatomic classification of lung cancer, which redefined the tumor-size cut-points in TNM stage for the lung cancer patients. The prognostic value of reclassification of tumor size were confirmed in 70,967 non–small-cell lung cancer patients from 1999 to 2010 [5]. To improve the survival of lung cancer patients, the choice of targeted treatments is increasingly being based on oncogenic drivers including ALK rearrangements, KRAS and epidermal growth factor receptor (EGFR) mutations [6, 7]. Additionally, BRAF mutations represent promising new therapeutic targets for lung cancer [8]. Likewise, several driver biomarkers also shed new light on the target treatment for lung cancer patients such as Her2 [9], NUT [10], DDR2 [11], FGFR1 [12], and PTEN [13]. Furthermore, several new molecular targets been highlighted in lung cancer, including ROS1 fusions [14], NTRK1 fusions [15] and exon 14 skipping mutations [16]. Recently, the checkpoint inhibitors targeting programmed death protein 1 (PD-1) have shown for durable clinical responses in NSCLC patients with advanced stage [17]. The immunomodulatory monoclonal antibodies against cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4) also present the promising results for the treatment of advanced -stages lung cancer patients. However, due to the complex molecular mechanism of lung cancer, the identification of biomarkers in a large proportion of lung cancer patients is still required for a deeper understanding of the underlying epigenetic heterogeneity, and this will benefit the discovery of targeted therapies against lung cancer.
Ki-67, encoded by the MKI67 gene, is expressed throughout the cell cycle in proliferating but absent in in quiescent (G0) cells [18]. Ki-67 appears in the middle or late G1 stage, and then its expression increases through the S and G2 stage until it reaches a peak during the M stage [19]. The high expression of Ki-67 may contribute to aggressive and infiltrative growth of lung squamous carcinoma (SQC), cervical SQC and laryngeal SQC [20–22]. In addition, overexpression of Ki-67 has been positively associated with lymph node metastasis in gastric carcinoma and breast cancer [23, 24]. Ki-67 expression has been reported to be associated with a poor outcome in many malignancies including prostate, bladder and breast cancer [25–29].
Although two meta-analyses have previously reported that Ki-67 could be a possible indicator of short-term survival in lung cancer patients [30, 31], studies on a larger number of lung cancer patients and more reliable evidence are still needed to confirm the prognostic and clinicopathological role of Ki-67 for patients with lung cancer. Thus, our investigation aimed to evaluate the prognostic value and clinicopathological significance of Ki-67 in lung cancer patients via the review of previously published articles.
Results
Study selection and characteristics
As shown in Fig. 1, two investigators read the full text and considered 108 studies in 95 articles [18, 25, 32–124] consisting of 14,732 patients as applicable. The baseline characteristics of the included articles are indicated in Table 1. Ninety-six studies included data regarding OS, and nineteen studies included data regarding DFS. The number of cohorts of each study ranged from 32 to 778. In terms of the study region, 62 studies were from Asia, 30 were from Europe, and 15 were from America. In total, 104 studies consisted of 14,596 NSCLC patients: of these, 28 studies reported on ADC patients, and 10 studies reported on SQC patients. All the studies detected Ki-67 reactivity using IHC.
Fig. 1.
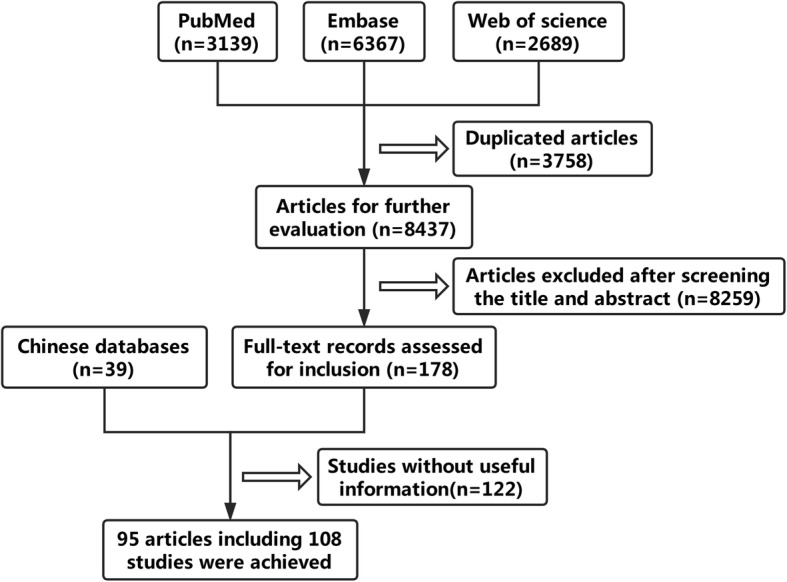
Flow chart of study selection process
Table 1.
Characteristics of studies included into the meta-analysis
| Study(author/year) | Region | Tumor stage | Histological type | Patients | Sample size | Cutoff value | Sample type | Assay | NOS score | Extract method | Survival |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Scagliotti 1993 [91] | Italy | I-IIIA | NSCLC | 111 | Large | 25% | Tumor tissue | IHC | 7 | Survival curve | OS |
| Pence 1993 [120] | USA | I-IV | NSCLC | 61 | Small | 4% | Tumor tissue | IHC | 7 | Survival curve | OS |
| Fontanini 1996 [46] | Italy | NA | NSCLC | 70 | Small | 30% | Tumor tissue | IHC | 7 | Survival curve | OS |
| Bohm 1996 [37] | Germany | NA | SCLC | 32 | Small | 27% | Tumor tissue | IHC | 7 | Original data | OS |
| Harpole 1996 [50] | USA | I | NSCLC | 275 | Large | 7% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Pujoll 1996 [88] | France | I-IV | LC | 97 | Small | NA | Tumor tissue | IHC | 7 | Survival curve | OS |
| Mehdi 1999 [119] | USA | I-IV | NSCLC | 203 | Large | 25% | Tumor tissue | IHC | 9 | Multivariate | OS and DFS |
| Demarchi 1999 [41] | Brazil | I-III | ADC | 64 | Small | 22% | Tumor tissue | IHC | 7 | Original data | OS |
| Dingemans 1999 [42] | Netherland | I-III | SCLC | 93 | Small | 30% | Tumor tissue | IHC | 7 | Survival curve | OS |
| Wang 1999 [99] | China | NA | NSCLC | 85 | Small | 30% | Tumor tissue | IHC | 7 | Survival curve | OS |
| Shiba 2000 [92] | Japan | I-III | NSCLC | 95 | Small | 20% | Tumor tissue | IHC | 7 | Univariate | OS |
| Hommura 2000 [54] | Japan | I-II | SQC | 91 | Small | 30% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Hommura 2000 [54] | Japan | I-II | NSCLC | 124 | Large | 30% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Nguyen 2000 [80] | Czech Republic | I-IV | NSCLC | 89 | Small | 30% | Tumor tissue | IHC | 7 | Survival curve | OS |
| Puglisi 2001 [87] | Italy | I-III | NSCLC | 81 | Small | 30% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Hayashi 2001 [52] | Japan | I-IV | NSCLC | 98 | Small | 13% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Pelosi 2001 [84] | Italy | I | SQC | 119 | Large | NA | Tumor tissue | IHC | 9 | Multivariate | OS and DFS |
| Ramnath 2001 [121] | USA | I-IV | NSCLC | 160 | Large | 24% | Tumor tissue | IHC | 7 | Univariate | OS |
| Ramnath 2001 [121] | USA | I-IV | NSCLC | 41 | Small | 50% | Tumor tissue | IHC | 7 | Univariate | OS |
| Wang 2001 [101] | China | I-IV | LC | 166 | Large | 18% | Tumor tissue | IHC | 7 | Survival curve | OS |
| Mojtahedzadeh 2002 [78] | Japan | I-III | ADC | 141 | Large | 10% | Tumor tissue | IHC | 8 | Multivariate | OS |
| Minami 2002 [76] | Japan | I | ADC | 47 | Small | 20% | Tumor tissue | IHC | 8 | Multivariate | OS |
| Takahashi 2002 [94] | Japan | I-IV | NSCLC | 62 | Small | 25% | Tumor tissue | IHC | 9 | Multivariate | DFS |
| Wakabayashi 2003 [97] | Japan | I-IV | NSCLC | 140 | Large | 13% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Pelosi 2003 [85] | UK | I | ADC | 96 | Small | NA | Tumor tissue | IHC | 9 | Multivariate | OS |
| Haga 2003 [49] | Japan | I | ADC | 58 | Small | 10% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Hashimoto 2003 [51] | Japan | I-III | ADC | 122 | Large | 20% | Tumor tissue | IHC | 8 | Multivariate | OS |
| Poleri 2003 [86] | Argentina | I | NSCLC | 50 | Small | 67% | Tumor tissue | IHC | 7 | Survival curve | DFS |
| Matheus 2004 [75] | Brazil | I-III | ADC | 33 | Small | 22% | Tumor tissue | IHC | 7 | Original data | OS |
| Niemiec 2004 [81] | Poland | I-III | SQC | 78 | Small | 28% | Tumor tissue | IHC | 7 | Survival curve | OS |
| Ahn 2004 [33] | Korea | II-IIIA | NSCLC | 65 | Small | 15% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Huang 2005 [55] | Japan | I | NSCLC | 97 | Small | 25% | Tumor tissue | IHC | 8 | Multivariate | OS |
| Gasinska 2005 [48] | Poland | I-III | SQC | 81 | Small | 39% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Wang 2005 [100] | China | I-III | NSCLC | 51 | Small | 5% | Tumor tissue | IHC | 7 | Survival curve | OS |
| Dong 2005 [43] | Japan | I-IV | ADC | 131 | Large | 18% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Niemiec 2005 [81] | Poland | I-III | SQC | 78 | Large | 28% | Tumor tissue | IHC | 7 | Survival curve | OS |
| Huang 2005 [55] | Japan | II-III | NSCLC | 76 | Small | 25% | Tumor tissue | IHC | 8 | Multivariate | OS |
| Tsubochi 2006 [64] | Japan | I-III | NSCLC | 219 | Large | 20% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Yang 2006 [110] | USA | I-III | NSCLC | 128 | Large | 25% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Nozawa 2006 [82] | Japan | IV | ADC | 35 | Small | 40% | Tumor tissue | IHC | 7 | Survival curve | OS |
| Maddau 2006 [118] | Italy | II-III | NSCLC | 88 | Large | 25% | Tumor tissue | IHC | 7 | Univariate | OS |
| Maddau 2006 [118] | Italy | I | NSCLC | 92 | Large | 25% | Tumor tissue | IHC | 7 | Univariate | OS |
| Inoue 2007 [58] | Japan | I-III | ADC | 97 | Small | 5% | Tumor tissue | IHC | 9 | Multivariate | DFS |
| Mohamed 2007 [77] | Japan | I-IV | NSCLC | 61 | Small | 20% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Zhou 2007 [116] | China | I-II | NSCLC | 70 | Small | NA | Tumor tissue | IHC | 6 | Multivariate | OS |
| Morero 2007 [79] | Argentina | III | NSCLC | 32 | Small | 66% | Tumor tissue | IHC | 7 | Survival curve | OS |
| Yoo 2007 [112] | Korea | I-III | NSCLC | 219 | Large | 30% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Fujioka 2008 [47] | Japan | I | ADC | 73 | Small | 14% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Imai 2008 [57] | Japan | I | NSCLC | 248 | Large | 25% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Woo 2008 [103] | Japan | Ia | ADC | 131 | Large | 10% | Tumor tissue | IHC | 8 | Univariate | DFS |
| Woo 2008 [103] | Japan | Ib | ADC | 59 | Small | 10% | Tumor tissue | IHC | 8 | Univariate | DFS |
| Saad 2008 [89] | USA | I-III | NSCLC | 54 | Small | 30% | Tumor tissue | IHC | 7 | Survival curve | OS |
| Kaira 2008 [124] | Japan | I-III | NSCLC | 321 | Large | 25% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Ikeda 2008 [56] | Japan | I-III | NSCLC | 200 | Large | 5% | Tumor tissue | IHC | 7 | Univariate | OS and DFS |
| Anami 2009 [34] | Japan | I-IV | ADC | 139 | Large | 10% | Tumor tissue | IHC | 8 | Multivariate | OS |
| Yuan 2009 [113] | China | I-III | NSCLC | 140 | Large | 25% | Tumor tissue | IHC | 8 | Multivariate | OS |
| Kaira 2009 [62] | Japan | 1 | ADC | 139 | Large | 20% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Erler 2010 [44] | USA | NA | SCLC | 68 | Small | 50% | Tumor tissue | IHC | 7 | Survival curve | OS |
| Filipits 2011 [45] | Austria | I-III | NSCLC | 778 | Large | NA | Tumor tissue | IHC | 9 | Multivariate | OS and DFS |
| Werynska 2011 [102] | Poland | I-IV | NSCLC | 145 | Large | 25% | Tumor tissue | IHC | 7 | Univariate | OS |
| Yamashita 2011 [109] | Japan | I | NSCLC | 44 | Small | 5% | Tumor tissue | IHC | 8 | Multivariate | DFS |
| Wu 2011 [106] | China | I-IV | NSCLC | 160 | Large | 10% | Tumor tissue | IHC | 8 | Multivariate | OS |
| Oka 2011 [83] | Japan | I-III | ADC | 183 | Large | 20% | Tumor tissue | IHC | 9 | Multivariate | DFS |
| Sterlacci 2011 [122] | Austria | I-IV | NSCLC | 386 | Large | 3% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Werynska 2011 [102] | Poland | NA | NSCLC | 145 | Large | 25% | Tumor tissue | IHC | 7 | Univariate | OS |
| Liu 2012 [71] | China | I-IV | NSCLC | 494 | Large | 50% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Wang 2012 [98] | China | NA | SCLC | 42 | Small | 10% | Tumor tissue | IHC | 7 | Survival curve | OS |
| Liu 2012 [71] | China | I-IV | ADC | 97 | Small | 10% | Tumor tissue | IHC | 7 | Survival curve | OS |
| Wu 2012 [105] | China | I-IV | ADC | 309 | Large | 50% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Salvi 2012 [90] | Italy | I-III | NSCLC | 81 | Small | 15% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Yang 2012 [111] | China | I-III | NSCLC | 68 | Small | 38% | Tumor tissue | IHC | 7 | Survival curve | OS |
| Wu 2013 [104] | China | I-IV | NSCLC | 192 | Large | 10% | Tumor tissue | IHC | 9 | Multivariate | OS and DFS |
| Maki 2013 [74] | Japan | I | ADC | 105 | Large | 15% | Tumor tissue | IHC | 9 | Multivariate | DFS |
| Lei 2013 [69] | China | I-IV | NSCLC | 279 | Large | 30% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Berghoff 2013 [36] | Austria | I-IV | NSCLC | 230 | Large | 40% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Ji 2013 [61] | China | I-III | NSCLC | 67 | Small | 5% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Kobyakov 2013 [68] | USA | I-III | SQC | 118 | Large | 30% | Tumor tissue | IHC | 7 | Survival curve | OS |
| Zu 2013 [117] | China | I-III | ADC | 96 | Small | 25% | Tumor tissue | IHC | 7 | Survival curve | OS |
| Liu 2013 [70] | China | I-III | NSCLC | 105 | Large | 50% | Tumor tissue | IHC | 8 | Multivariate | OS |
| Hokka 2013 [53] | Japan | I-IV | ADC | 125 | Large | NA | Tumor tissue | IHC | 9 | Multivariate | OS |
| Xue 2013 [73] | China | I-III | NSCLC | 83 | Small | 50% | Tumor tissue | IHC | 8 | Multivariate | OS |
| Zhong 2014 [115] | China | I-IV | NSCLC | 270 | Large | 50% | Tumor tissue | IHC | 8 | Multivariate | OS |
| Ahn 2014 [32] | Korea | I-III | NSCLC | 108 | Large | 40% | Tumor tissue | IHC | 9 | Multivariate | DFS |
| Shimizu 2014 [93] | Japan | I-III | SQC | 32 | Small | 10% | Tumor tissue | IHC | 8 | Multivariate | DFS |
| Shimizu 2014 [93] | Japan | I-III | ADC | 52 | Small | 10% | Tumor tissue | IHC | 8 | Multivariate | DFS |
| Kim 2014 [136] | Korea | I-IV | ADC | 122 | Large | 10% | Tumor tissue | IHC | 7 | Univariate | OS |
| Tsoukalas 2014 [95] | Greece | I-IV | NSCLC | 112 | Large | NA | Tumor tissue | IHC | 9 | Multivariate | OS |
| Kawatsu 2014 [63] | Japan | I-IV | NSCLC | 183 | Large | 10% | Tumor tissue | IHC | 8 | Multivariate | OS |
| Corzani 2014 [39] | Italy | III | NSCLC | 50 | Small | 50% | Tumor tissue | IHC | 8 | Multivariate | OS |
| Warth 2014 [18] | Germany | I-IV | ADC | 482 | Large | 25% | Tumor tissue | IHC | 7 | Univariate | OS and DFS |
| Warth 2014 [18] | Germany | I-IV | SQC | 233 | Large | 50% | Tumor tissue | IHC | 8 | Multivariate | OS |
| Tabata 2014 [25] | Japan | I-IV | NSCLC | 74 | Small | 10% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Xu 2014 [108] | China | I-IV | ADC | 80 | Small | 5% | Tumor tissue | IHC | 7 | Survival curve | OS |
| Liu 2014 [70] | China | I-IV | NSCLC | 96 | Small | 30% | Tumor tissue | IHC | 7 | Survival curve | OS |
| Ji 2014 [60] | China | I-III | NSCLC | 83 | Small | NA | Tumor tissue | IHC | 8 | Multivariate | OS |
| Shimizu 2014 [93] | Japan | I-IV | SQC | 32 | Large | 10%% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Shimizu 2014 [93] | Japan | I-IV | ADC | 52 | Large | 10%% | Tumor tissue | IHC | 9 | Multivariate | OS |
| Kobierzycki 2014 [67] | Poland | I-IV | NSCLC | 218 | Large | 25% | Tumor tissue | IHC | 6 | Univariate | OS |
| Xu 2014 [107] | China | I-III | NSCLC | 114 | Large | 50% | Tumor tissue | IHC | 7 | Univariate | OS |
| Zhang 2015 [114] | China | I-IV | ADC | 616 | Large | NA | Tumor tissue | IHC | 8 | Multivariate | OS |
| Gobbo 2015 [40] | Italy | NA | NSCLC | 383 | Large | 20% | Tissue microarray | IHC | 7 | Univariate | OS |
| Stewart 2015 [123] | USA | II-IIIA | NSCLC | 230 | Large | NA | Tumor tissue | IHC | 7 | Univariate | DFS |
| Vigouroux 2015 [96] | France | I-IV | NSCLC | 190 | Large | 40% | Tumor tissue | IHC | 7 | Survival curve | OS |
| Jethon 2015 [59] | Poland | I-IV | SQC | 89 | Small | 25% | Tumor tissue | IHC | 7 | Univariate | OS |
| Jethon 2015 [59] | Poland | I-IV | ADC | 98 | Small | 25% | Tumor tissue | IHC | 7 | Univariate | OS |
| Apostolova 2016 [35] | Germany | I-IV | NSCLC | 83 | Small | 75% | Tumor tissue | IHC | 8 | Multivariate | OS |
| Cardona 2016 [38] | USA | NA | NSCLC | 144 | Large | 30% | Tumor tissue | IHC | 7 | Original data | OS |
Prognostic value of Ki-67 for survival outcome in lung cancer patients
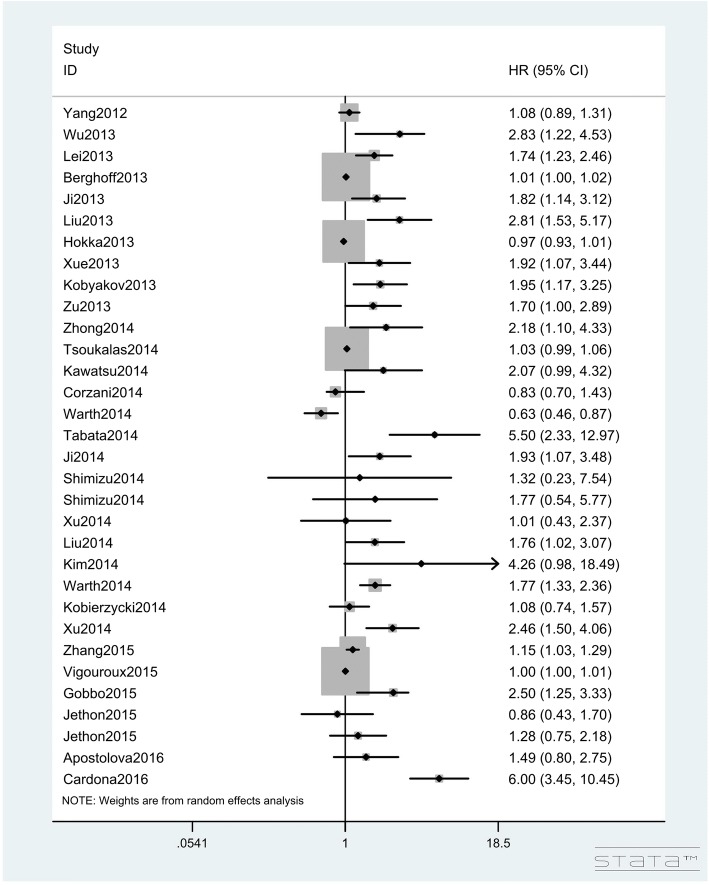
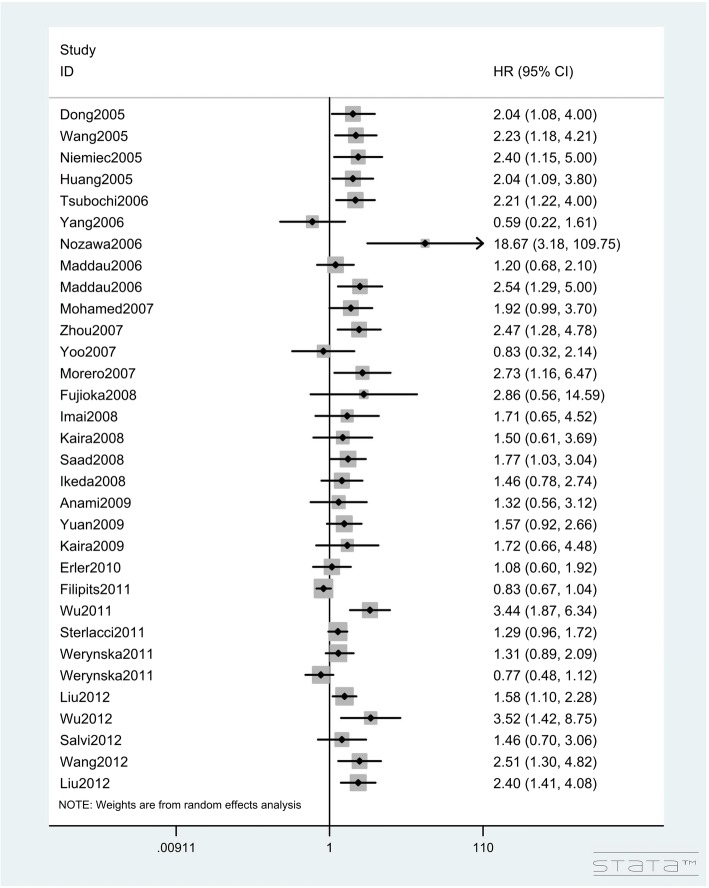
In total, 95 studies with 13,678 lung cancer patients investigated the impact of Ki-67 expression on OS (Table 2). The pooled HR of the total population for OS was 1.122 (95%CIs: 1.089–1.156, Z = 7.56, P < 0.001; I2 = 78.20%, P < 0.001, Figs. 2, 3 and 4), showing that a high Ki-67 level indicates worse outcome for lung cancer patients. Furthermore, the correlation of high Ki-67 expression with DFS in 3127 lung cancer patients was then analyzed (Table 3). For the total study population, worse DFS (HR = 1.894, 95%CIs: 1.456–2.463, Z = 4.76, P < 0.001, Fig. 5) was observed among patients with high expression of Ki-67, while the heterogeneity using the random effects model was obvious (I2 = 78.30%, P < 0.001). To investigate the source of heterogeneity, subgroup analyses of publication year, region, histological type, sample size, cut-off value of Ki-67 and estimated method for HR determination were performed. From the subgroup analysis of OS, no heterogeneity was found in the small cell lung cancer (SCLC) group (I2 = 22.30%, P = 0.277). Next, a reduction in heterogeneity was observed after performing subgroup analysis of DFS according to the study region, especially in the studies from America (I2 = 8.40%, P = 0.351) and Asia (I2 = 25.60%, P = 0.179). As indicated in the subgroup of cutoff value, there was a low degree of heterogeneity in both Ki-67 low expression (I2 = 25.30%, P = 0.196) and high expression groups (I2 = 19.40%, P = 0.287). Furthermore, we also performed meta-regression analysis to explore the original of the heterogeneity in the studies. Consistent with the subgroup analysis, the results revealed that the regions and cut-off values might be the potential bias for the heterogeneity (P = 0.017 and P = 0.022, respectively). Altogether, we concluded that the different regions and inconsistent cut-off values might have contributed to the heterogeneity in the results of analyses for DFS. The regression also revealed that the heterogeneity originated from regions and inconsistent cut-off values (Table 4).
Table 2.
Summarized HRs of overall and subgroup analyses for OS
| Stratified analysis | Study(N) | HR | z | P | Heterogeneity | ||
|---|---|---|---|---|---|---|---|
| I2 | P | Estimated method | |||||
| OS | 95 | 1.122(1.089–1.156) | 7.56 | < 0.001 | 78.20% | < 0.001 | Random-effect |
| Subgroup analysis | |||||||
| Publication year | |||||||
| Early year(~ 2007) | 44 | 1.307(1.212–1.408) | 7.01 | < 0.001 | 72.50% | < 0.001 | Random-effect |
| Later year(2007~ 2016) | 51 | 1.101(1.063–1.142) | 5.28 | < 0.001 | 81.20% | < 0.001 | Random-effect |
| Region | |||||||
| Europe | 30 | 1.021(1.001–1.042) | 2.05 | 0.041 | 71.30% | < 0.001 | Random-effect |
| America | 13 | 1.671(1.266–2.205) | 3.63 | < 0.001 | 66.60% | < 0.001 | Random-effect |
| Asia | 52 | 1.821(1.623–2.043) | 10.21 | < 0.001 | 78.20% | < 0.001 | Random-effect |
| Histological type | |||||||
| SCLC | 4 | 1.023(1.004–1.042) | 3.28 | 0.001 | 22.30% | 0.277 | Fixed-effect |
| NSCLC | 89 | 1.113(1.081–1.147) | 7.11 | < 0.001 | 78.70% | < 0.001 | Random-effect |
| ADC | 22 | 1.219(1.113–1.336) | 4.26 | < 0.001 | 76.20% | < 0.001 | Random-effect |
| SQC | 9 | 1.115(0.806–1.542) | 0.66 | 0.512 | 74.40% | < 0.001 | Random-effect |
| Sample size | |||||||
| < 100 | 45 | 1.486(1.340–1.649) | 7.71 | < 0.001 | 73.10% | < 0.001 | Random-effect |
| > 100 | 50 | 1.083(1.049–1.119) | 4.90 | < 0.001 | 81.50% | < 0.001 | Random-effect |
| Cutoff value | |||||||
| L(< 20%) | 34 | 1.962(1.622–2.373) | 6.95 | < 0.001 | 74.50% | < 0.001 | Random-effect |
| H(≥20%) | 52 | 1.144(1.094–1.197) | 5.91 | < 0.001 | 78.90% | < 0.001 | Random-effect |
| Estimated method | |||||||
| Original data | 4 | 2.043(0.868–4.808) | 1.64 | 0.102 | 83.90% | < 0.001 | Random-effect |
| Survival curve | 23 | 1.629(1.368–1.940) | 5.47 | < 0.001 | 76.30% | < 0.001 | Random-effect |
| HR(univariate) | 16 | 1.511(1.236–1.847) | 4.02 | < 0.001 | 56.10% | 0.004 | Random-effect |
| HR(multivariate) | 53 | 1.108(1.063–1.155) | 4.87 | < 0.001 | 75.30% | < 0.001 | Random-effect |
Fig. 2.
Hazard ratios and 95% CIs of studies included in meta-analysis of OS
Fig. 3.
Hazard ratios and 95% CIs of studies included in meta-analysis of OS
Fig. 4.
Hazard ratios and 95% CIs of studies included in meta-analysis of OS
Table 3.
Summarized HRs of overall and subgroup analyses for DFS
| Stratified analysis | Study(N) | HR | Z | P | Heterogeneity | ||
|---|---|---|---|---|---|---|---|
| I2 | P | Estimated method | |||||
| DFS | 21 | 1.894(1.456–2.463) | 4.76 | < 0.001 | 78.30% | < 0.001 | Random-effect |
| Subgroup analysis for DFS | |||||||
| Publication year | |||||||
| Early year(~ 2007) | 6 | 1.428(0.992–2.055) | 1.92 | 0.055 | 62.10% | 0.022 | Random-effect |
| Later year(2007~ 2016) | 15 | 2.237(1.54–3.249) | 4.23 | < 0.001 | 72.00% | < 0.001 | Random-effect |
| Region | |||||||
| Europe | 3 | 1.023(1.005–1.041) | 2.51 | 0.012 | 53.40% | 0.117 | Fixed-effect |
| America | 4 | 1.559(1.155–2.105) | 2.9 | 0.004 | 8.40% | 0.351 | Fixed-effect |
| Asia | 14 | 2.673(2.096–3.409) | 7.92 | < 0.001 | 25.60% | 0.179 | Fixed-effect |
| Histological type | |||||||
| SCLC | |||||||
| NSCLC | 21 | 1.894(1.456–2.463) | 4.76 | < 0.001 | 78.30% | < 0.001 | Random-effect |
| ADC | 9 | 3.186(1.797–5.650) | 3.96 | < 0.001 | 62.10% | 0.007 | Random-effect |
| SQC | 2 | 1.022(1.004–1.04) | 2.42 | 0.015 | 0.00% | 0.774 | Random-effect |
| Sample size | |||||||
| < 100 | 7 | 2.455(1.392–4.330) | 3.10 | < 0.001 | 20.30% | 0.28 | Fixed-effect |
| > 100 | 14 | 1.770(1.340–2.338) | 4.02 | < 0.001 | 82.80% | < 0.001 | Random-effect |
| Cutoff value | |||||||
| L(< 20%) | 12 | 2.783(2.141–3.619) | 7.64 | < 0.001 | 25.30% | 0.196 | Fixed-effect |
| H(≥20%) | 6 | 1.514(1.243–1.844) | 4.12 | < 0.001 | 19.40% | 0.287 | Fixed-effect |
| Estimated method | |||||||
| Survival curve | 2 | 1.595(1.053–2.416) | 2.21 | 0.027 | 52.60% | 0.146 | Fixed-effect |
| HR(univariate) | 6 | 2.126(1.156–3.909) | 2.43 | 0.015 | 67.40% | 0.009 | Random-effect |
| HR(multivariate) | 13 | 1.892(1.328–2.698 | 3.53 | < 0.001 | 79.90% | < 0.001 | Random-effect |
Fig. 5.
Hazard ratios and 95% CIs of studies included in meta-analysis of DFS
Table 4.
Meta-regression for the OS and DFS analysis
| Variables | HR | Standard Error | t | P > |t| | Lower limit | Upper limit |
|---|---|---|---|---|---|---|
| OS | ||||||
| Year | 0.999 | 0.104 | −0.010 | 0.991 | 0.811 | 1.230 |
| Region | 0.835 | 0.061 | −2.450 | 0.017 | 0.722 | 0.967 |
| Cancer type | 0.954 | 0.045 | −0.990 | 0.326 | 0.868 | 1.049 |
| Sample size | 1.108 | 0.122 | 0.930 | 0.353 | 0.890 | 1.380 |
| Cutoff value | 0.777 | 0.084 | −2.330 | 0.022 | 0.626 | 0.964 |
| Statistical method | 1.045 | 0.044 | 1.050 | 0.295 | 0.961 | 1.137 |
| DFS | ||||||
| Year | 2.011 | 1.525 | 0.920 | 0.377 | 0.379 | 10.678 |
| Region | 0.591 | 0.289 | −1.070 | 0.306 | 0.201 | 1.736 |
| Cancer type | 1.125 | 0.401 | 0.330 | 0.747 | 0.513 | 2.467 |
| Sample size | 0.793 | 0.348 | −0.530 | 0.607 | 0.302 | 2.081 |
| Cutoff value | 0.767 | 0.363 | −0.560 | 0.587 | 0.271 | 2.172 |
| Statistical method | 0.994 | 0.221 | −0.030 | 0.979 | 0.609 | 1.622 |
The correlation of Ki-67 expression and clinicopathological features in lung cancer patients
An association of Ki-67 expression with age in 2506 lung cancer patients was identified using the fixed effects model in 19 studies, and higher Ki-67 expression was found to be more common in older patients (OR = 1.246, 95%CIs: 1.039–1.494; Z = 2.37, P = 0.018, I2 = 0.00%, P = 0.967, Table 5 and Additional file 1: Figure S1). Subsequently, the results revealed significant differences in Ki-67 level between male and female (OR = 1.874, 95%CIs: 1.385–2.535; Z = 4.07, P < 0.001, I2 = 69.70%, P < 0.0001, Additional file 1: Figure S1B). Meta-analysis of 15 studies including 2152 lung cancer patients revealed a positive association between high Ki-67 level and smoking history (OR = 3.087, 95%CIs: 2.504–3.806, Z = 10.56, P < 0.001; I2 = 39.40%, P = 0.064, Additional file 1: Figure S1C). According to the histological type, a pooled OR of 0.397 (95%CIs: 0.236–0.667) indicated that Ki-67 expression was significantly higher in ADC compared with that in SQC (Z = 3.49, P < 0.001; I2 = 81.20%, P < 0.001, Additional file 2: Figure S2A). Next, tumor differentiation was considered. The results from 11 studies enrolling 1731 lung cancer patients showed that an elevated Ki-67 level was associated with poor differentiation, with a pooled OR of 1.993 (95%CIs:1.262–3.146, Z = 2.96, P = 0.003; I2 = 66.30%, P = 0.001, Additional file 2: Figure S2B). A total of 13 studies with 1851 individuals were analyzed in this meta-analysis, and the results showed that a higher Ki-67 level was positively associated with the pathologic stage III/IV with a low degree of heterogeneity (OR = 1.867, 95%CIs: 1.498–2.327, Z = 5.56, P < 0.001; I2 = 23.1%, P = 0.210, Additional file 2: Figure S2C). A trend toward positive correlation was found between a high Ki-67 level and larger tumor size in 12 studies based on 1707 lung cancer patients, with a pooled OR of 1.436 (95%CIs:1.127~ 1.290,, Z = 2.93, P = 0.003; I2 = 0.00%, P = 0.876, Additional file 3: Figure S3A). Twenty-three studies comprising 2994 cases were used for meta-analysis of Ki-67 expression and lymph node metastasis, and the pooled OR indicated that a high Ki-67 level was significantly correlated with lymph node metastasis positive (OR = 1.653, 95%CIs: 1.285–2.127, Z = 3.91, P < 0.0001; I2 = 46.70%, P = 0.008, Additional file 3: Figure S3B). The association of Ki-67 expression and TNM stage was then incorporated into the meta-analysis. Eight studies with 736 patients showed a trend for correlation between Ki-67 overexpression and advanced TNM stages, with a pooled OR of 1.50 (95%CIs:1.053~ 2.126, Z = 2.25, P = 0.024; I2 = 36.90%, P = 0.134, Additional file 3: Figure S3C). In the meta-analysis, no association between Ki-67 and tumor stage was observed in lung cancer patients (OR = 1.287, 95%CIs:0.882–1.877, Z = 1.31, P = 0.191; I2 = 55.30%, P = 0.013). Additionally, analysis of four selected studies using the random effects model did not reveal any significance for the association between Ki-67 expression and metastasis (OR = 2.609, 95%CIs: 0.667–10.204, Z = 1.38, P = 0.168) or invasion (OR = 0.993, 95%CIs: 0.511–1.930, Z = 0.02, P = 0.984; I2 = 14.20%, P = 0.312).
Table 5.
Main results for meta-analysis between Ki-67 and clinicopathological features in lung cancer
| Clinicopathological features | Study(n) | Pooled OR(95%CIs) | z | P | Heterogeneity | Publication bias | ||
|---|---|---|---|---|---|---|---|---|
| I2 | P | Estimated method | P | |||||
| Age | 19 | 1.246(1.039–1.494) | 2.37 | 0.018 | 0.00% | 0.967 | Fixed-effect | 0.234 |
| Gender | 26 | 1.874(1.385–2.535) | 4.07 | < 0.001 | 69.70% | 0.000 | Random-effect | 1.000 |
| Histological type | 16 | 0.397(0.236–0.667) | 3.49 | < 0.001 | 81.20% | 0.000 | Random-effect | 0.324 |
| Differentiation | 11 | 1.993(1.262–3.146) | 2.96 | 0.003 | 66.30% | 0.001 | Random-effect | 0.893 |
| Pathologic stage | 13 | 1.867(1.498–2.327) | 5.56 | < 0.001 | 23.10% | 0.210 | Fixed-effect | 1.000 |
| Tumor size | 12 | 1.436(1.127–1.29) | 2.93 | 0.003 | 0.00% | 0.876 | Fixed-effect | 0.276 |
| Tumor stage | 11 | 1.287(0.882–1.877) | 1.31 | 0.191 | 55.30% | 0.013 | Random-effect | 0.086 |
| Metastasis | 4 | 2.609(0.667–10.204) | 1.38 | 0.168 | 64.50% | 0.038 | Random-effect | 0.428 |
| Lymph node | 23 | 1.653(1.285–2.127) | 3.91 | < 0.001 | 46.70% | 0.008 | Random-effect | 0.876 |
| TNM stage | 8 | 1.497(1.053–2.126) | 2.25 | 0.024 | 36.90% | 0.134 | Fixed-effect | 0.187 |
| Invasion | 3 | 0.993(0.511–1.930) | 0.02 | 0.984 | 14.20% | 0.312 | Fixed-effect | 0.308 |
| Smoking | 15 | 3.087(2.504–3.8060) | 10.56 | < 0.001 | 39.40% | 0.064 | Fixed-effect | 0.711 |
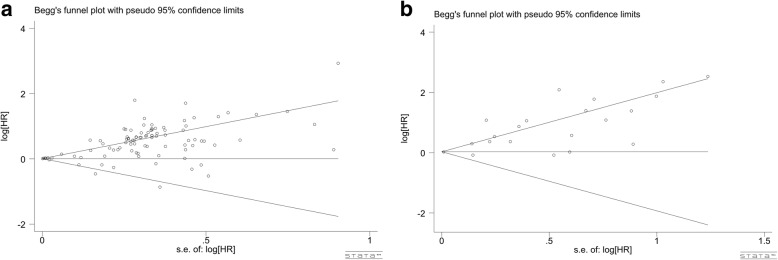
Publication bias
To identify potential publication bias, Begg’s test and funnel plots were used. No publication bias was found in the analysis for OS (p = 0.444, Fig. 6a) and DFS (P = 0.246, Fig. 6b). Moreover, there was no publication bias among any of the analyses used to correlate Ki-67 expression and clinicopathological characteristics (all P > 0.05, Table 5, Additional file 4: Figure S4, Additional file 5: Figure S5, Additional file 6: Figure S6 and Additional file 7: Figure S7).
Fig. 6.
Funnel plots for publication bias of OS and DFS meta-analysis
Discussion
As previously mentioned, there are two meta-analyses showing that high expression of Ki-67 predicts worse prognosis in lung cancer patients [30] and early-stage NSCLCs [31]. Nevertheless, there is no consensus regarding the clinicopathological significance of Ki-67 in lung cancer patients. Martin et al. performed a meta-analysis on 37 studies to evaluate the prognostic value of Ki-67 in 3983 lung cancer patients in 2004 [30]. Lacking sufficient information for other subtypes of lung cancer and Asian patients, the results from the abovementioned meta-analysis were not convincing. Our meta-analysis includes 108 studies with 14,831 lung cancer patients comprising NSCLC and SCLC cases and thus provides more reliable evidence. Additionally, we also restricted the number of patients in each study to greater than 30 to exclude low-quality studies. To strengthen the evidence, we estimated not only OS data but also DFS to determine the prognostic role of Ki-67 in lung cancer patients. Moreover, multivariate analyses of OS and DFS were performed, and the HR of OS was 1.108(95%CIs: 1.063–1.155), and that for DFS was 1.892(95%CIs: 1.328–2.698), indicating that Ki-67 is an independent prognostic marker for lung cancer. Compared to the previous meta-analysis, our meta-analysis included results on all subtypes of lung cancer and represented broader ethnicity; in addition, subgroups were classified according to region, cut-off value, number of patients and histological type. With the inclusion of high-quality studies and a larger number of patients, the results derived from our study are more convincing.
Ki-67 is present in the active phases of the cell cycle (G1, S, and G2), as well as during mitosis, but it is not expressed in the G0 phase. Thus, it has become an excellent operational marker for the estimation of the proportion of proliferative cells in a given cell population [125]. Our study demonstrated that Ki-67 expression was lower in ADC compared with that in SQC, suggesting it is a useful biomarker for distinguishing ADC from SQC. Consisted with our result, Ki-67 was also revealed to be higher in ADC than in SQC in the same stage, duo to the different tumor biology of histological subtypes in NSCLC [49, 64]. The high-grade Ki-67 was proved to be significantly correlated with a more aggressive tumor infiltration patterns in lung SQC, Indicating the strong association between tumor invasiveness and cell proliferation [20]. It has been reported in the literature that inverted papillomas with high levels of Ki-67 also include squamous cell carcinomas. Regarding the SCLC, Vasudha Murlidhar et al. recently carried out a result that Ki-67 could contribute to the early detection of metastasis in circulating lung cancer cells. Ki-67 was also demonstrated as a potential diagnostic factor for histopathological definition of SCLC [126]. Contrary to our study, previous study revealed that maternal cigarette smoking could dramatically decrease the expression of Ki-67 in cytotrophoblasts [127]. Interestingly, further study also found that Ki-67 was lower expressed in smokers and smokers with COPD compared to the non-smokers. The authors hypothesized that the permanent cellular damage might play a crucial role in the destruction of bronchiolar tissue [128]. Nevertheless, the mechanisms that govern how Ki-67 expression contribute to the tumorigenesis and progression of lung cancer remain to be unveiled.
The authors suspected that Ki-67 might affect cyclin-dependent kinase1 (CDK1), leading to the entry of inverted papilloma cells into the active phase of cell cycle(G1)and resulting in malignant transformation [129]. Interestingly, our study found that Ki-67 expression in male patients was significantly higher comparing with that in female patients. Previous reports have suggested that testosterone can promote the growth of cancer cells that express androgen receptors, which negatively regulates the Ki-67 level in lung cancer patients [130, 131]. Many previous studies have also revealed that Ki-67 is significantly associated with histopathologic parameters in other tumor because of the correlation between proliferation and those parameters [132–134]. It was found that p53 regulated the p53- and Sp1-dependent pathways, leading to the inhibition of Ki-67 promoter [135, 136]. A recent study confirmed that there was a correlation between the specific Ki-67 splice variants and the progression through the cell cycle in cancer cells. Ki-67 might be involved in a putative extranuclear elimination pathway transported to the Golgi apparatus [137]. Based on these results, we concluded that Ki-67 serves as a valuable indicator for the aggressiveness and prognosis of lung cancer.
Heterogeneity was significant in this meta-analysis. To eliminate the heterogeneity, subgroup analyses according to region, cut-off value, number of patients and histological type were carried out using random effects models. As a result, we revealed that the source of heterogeneity originated from the publication region and the cutoff value by the meta-regression analysis. Our meta-analysis was limited to publications in English or Chinese; nevertheless, the researchers typically tend to publish studies with negative results in local journals and in the native language of the study region. In addition, although detailed exclusion criteria were established to avoid duplication, our meta-analysis was not able to avoid the same patient cohorts in different publications. Other methodological factors might also affect heterogeneity, such as the antibody and cut-off value used in the study. Although anti-MIB-1 antibody is the most frequently used antibody in studies, most of the included studies stratified high and low levels of Ki-67 using a median value varying from 3 to 75%, which might have influenced the results. Several studies used the Ki-67 cut-off less than 10% to assess the prognostic impact of Ki-67 after surgical resection with curative intent in early-stages lung cancer patients. Most of the included studies used the median value of Ki-67 index as cutoff value, which could divide the patient into equally the group but did not reflect the clinical relevant use. A cut-off value of Ki-67 maximizing the hazard ratio across the groups could be used for the clinical management for the diagnosis and prognosis of lung cancers. More importantly, Multiple clinical laboratories have reported the Ki-67 cutoff values between 10 and 14% could be recommended as the gold standard identify the high risk of the survival outcome in cancers [138–141]. Additionally, microarrays were used in several studies, for which the sensitivity of assessment of Ki-67 expression is generally poor. Another possibility of bias may be related to the method of extrapolating the HR; the HR extracted from survival curves was less reliable than direct analysis of variance. Additionally, the subgroup analysis for different stages because most of the included studies recruited the lung cancer patients within three or more tumor stages. Thus, we could not classify the patients into the early stages and advanced stages for the subgroup analysis.
Conclusion
In conclusion, our meta-analysis demonstrated that high expression of Ki-67 is associated with worse prognosis and disease progression in lung cancer patients. Ki-67 can be an independent biological marker for predicting the prognosis of lung cancer patients. Subsequent studies are required to investigate the prognoses and clinical characteristics of lung cancer patients to confirm our findings.
Materials and methods
Literature search and selection
The databases that we searched included PubMed, Web of Science, EMBASE, and Chinese datasets (WanFang, China National Knowledge Infrastructure and Chinese VIP) until June 1, 2017. The key words identifying the articles were as follows: (Ki-67 OR Ki67 OR MIB-1 OR “proliferative index” OR “proliferative activity” OR “mitotic index” OR “labeling index” OR “mitotic count” OR “proliferative marker” OR “mitotic figure” OR “mitotic activity”) AND (Cancer OR carcinoma OR adenocarcinoma OR tumour OR tumor OR malignanc* OR neoplas*) AND (Lung OR pulmonary OR respiratory OR respiration OR aspiration OR bronchi OR bronchioles OR alveoli OR pneumocytes OR “air way”).
Selection criteria
Publications were included if they met the following inclusion criteria: (1) the patients enrolled had been diagnosed with lung cancer; (2) the results for the study included the correlation between Ki-67 and overall survival (OS) or disease-free survival (DFS); (3) the samples used in the studies were human lung tissue, serum or sputum but not animals or cell lines; (4) the techniques used to measure the expression level of Ki-67 in cancer tissue or tumors of the patients were immunohistochemistry (IHC), PCR/RT-PCR, ELISA or western blotting; (5) the study provided hazard ratios (HRs) and their 95% confidence intervals (CIs) or sufficient information for estimating these parameters; (6) the article was fully written in English or Chinese; and (7) the sample size was larger than 30. Studies were excluded if they met the following exclusion criteria:(1) if they included animal experiments or cell lines or were pre-clinical studies, meta-analyses, reviews, comments, conference abstracts, letters or case reports; (2) articles in languages other than English or Chinese; and (3) studies did not include the key information for survival analyses such as HRs and 95%CIs. To avoid data duplication, when the same patient cohort was reported in different publications or the same article was found in different journals, only the most recent and complete publication was included.
Data extraction and quality assessment
All the articles were independently reviewed and selected by two investigators. Discrepancies were resolved by discussion and arbitrated by a third investigator. The following information was extracted from each publication: first author’s name, year of publication year, pathology type, tumor stage, number of patients, sample type, cut-off value of Ki-67, determination assay, method to extract HR and survival type. Additionally, we also obtained the clinicopathological characteristics of the lung cancer patients in the included studies including age (old/young), gender (male/female), histological type (adenocarcinoma/squamous carcinoma, ADC/SQC), smoking status (smoker/non-smoker), differentiation (poor/well or moderate), pathologic stage (III-IV/I-II), tumor size (large/small), tumor stage (T3–4/T1-T2), metastasis (yes/no), lymph node (N1-Nx/N0), TNM stage (T3–4/T1-T2) and invasion (yes/no). Especially, the tumor stage was used to describe the size and extent of tumor. And the TNM stage were used to define the progression of cancer based on the size and extension tumor, lymphatic involvement and metastasis status. Based on the Newcastle Ottawa Scale (NOS) criteria [142], studies with NOS scores higher than 6 are considered high-quality studies, whereas those with NOS scores less than 5 are defined as low-quality studies. This study was strictly performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [143] and the PRISMA checklist were also provided in the Additional file 8.
Statistical methods
HR and 95%CIs were used to measure the relationship between Ki-67 expression and prognosis of lung cancer patients. The most accurate determination was made when the study directly provided the HRs and 95%CIs. The multivariate HRs were calculated by using the Cox proportional hazards model, which could independently predict the survival outcome for the lung cancer patients. We preferentially chose the multivariate values when the study provided both univariate and multivariate HRs. If the above data were not available, we used the Engauge Digitizer version 4.1 to extract the survival rates from KM curves and estimated the HR according the method as Tierneyet al. described [144, 145]. Moreover, we calculated the HR from the original survival data that the study provided using SPSS. An observed HR > 1 indicated worse prognosis for the lung cancer patients with high expression of Ki-67, if the 95%CIs for the overall HR was not 1, we considered the prognostic effect of Ki-67 on to be statistically significant. Odds ratio (OR) with 95%CIs were used to analyze the degree of association between Ki-67 level and clinicopathological characteristics. Heterogeneity was determined using the χ2 and inconsistency (I2) tests [146]. I2 > 50% or P < 0.1 indicated substantial heterogeneity among the studies, in which case a random effects model was applied; otherwise, we utilized the fixed effects model. Then, subgroup analysis and meta-regression analysis were used to investigate any source of heterogeneity. Moreover, publication bias was assessed using Begg’s test and funnel plots, and P-values < 0.05 indicated statistically significant publication bias [147].
Additional files
Figure S1. Forest plots for the relationships between Ki-67 expression and clinicopathological features of patients with lung cancer. A. Age B. Gender C. Histological type. (TIF 4444 kb)
Figure S2. Forest plots for the relationships between Ki-67 expression and clinicopathological features of patients with lung cancer. A. Differentiation B. Pathologic stage C. Tumor size. (TIF 3759 kb)
Figure S3. Forest plots for the relationships between Ki-67 expression and clinicopathological features of patients with lung cancer. A. Lymph node B. TNM stage C. Smoking. (TIF 3186 kb)
Figure S4. Funnel plots for publication bias of clinicopathological features meta-analysis (A~C). A. Age B. Gender C. Histological type. (TIF 20061 kb)
Figure S5. Funnel plots for publication bias of clinicopathological features meta-analysis (D~F). A. Differentiation B. Pathologic stage C. Tumor size. (TIF 21452 kb)
Figure S6. Funnel plots for publication bias of clinicopathological features meta-analysis (G~J). A. Tumor stage B. Lymph node C. TNM stage. (TIF 21299 kb)
Figure S7. Funnel plot for publication bias of clinicopathological features meta-analysis (Smoking status). (TIF 7465 kb)
PRISMA 2009 Checklist. (DOC 63 kb)
Acknowledgments
Funding
The current study was supported by the Funds of National Natural Science Foundation of China (NSFC 81360327, NSFC 81560469), Natural Science Foundation of Guangxi, China (2015GXNSFCA139009) and Guangxi Medical University Training Program for Distinguished Young Scholars (2017).
Availability of data and materials
The databases which we collection Literature include PubMed, Web of Science, EMBASE, and Chinese datasets (WanFang, China National Knowledge Infrastructure and Chinese VIP) until June 1, 2017.
Abbreviations
- CDK1
Cyclin-dependent kinase1
- CIs
Confidence intervals
- DFS
Disease-free survival
- EGFR
Epidermal growth factor receptor
- HR
Hazard ratio
- IHC
Immunohistochemistry
- NSCLC
Non-small cell lung cancer
- OR
Odds ratio
- OS
Overall survival
- SCLC
Small cell lung cancer
- SQC
Squamous carcinoma
Authors’ contributions
DMW and GC conceived of the project and designed the study. DMW and WJC wroted the manuscript. RMM and NZ participated in selecting study and extracting data. WJC and DYL take part in Manuscript Revise. GC was in charge of quality control. All authors read and approved the final manuscript.
Not applicable.
Not applicable.
The authors declare that they have no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Dan-ming Wei, Email: danmingwei08@163.com.
Wen-jie Chen, Email: ajchenwenjie@gmail.com.
Rong-mei Meng, Email: 3088601866@qq.com.
Na Zhao, Email: 1803378864@qq.com.
Xiang-yu Zhang, Email: 949195924@qq.com.
Dan-yu Liao, Email: 842060442@qq.com.
Gang Chen, Email: chengang@gxmu.edu.cn.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66(1):7–30. doi: 10.3322/caac.21332. [DOI] [PubMed] [Google Scholar]
- 2.Polanski J, Jankowska-Polanska B, Rosinczuk J, Chabowski M, Szymanska-Chabowska A. Quality of life of patients with lung cancer. Onco Targets Ther. 2016;9:1023–1028. doi: 10.2147/OTT.S100685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.John LD. Self-care strategies used by patients with lung cancer to promote quality of life. Oncol Nurs Forum. 2010;37(3):339–347. doi: 10.1188/10.ONF.339-347. [DOI] [PubMed] [Google Scholar]
- 4.Paesmans M. Prognostic factors in lung cancer. Rev Mal Respir. 2005;22(6 Pt 2):8S76–8S80. [PubMed] [Google Scholar]
- 5.Goldstraw P, Chansky K, Crowley J, Rami-Porta R, Asamura H, Eberhardt WE, Nicholson AG, Groome P, Mitchell A, Bolejack V. The IASLC lung cancer staging project: proposals for revision of the TNM stage groupings in the forthcoming (eighth) edition of the TNM classification for lung cancer. J Thorac Oncol. 2016;11(1):39–51. doi: 10.1016/j.jtho.2015.09.009. [DOI] [PubMed] [Google Scholar]
- 6.Won JK, Keam B, Koh J, Cho HJ, Jeon YK, Kim TM, Lee SH, Lee DS, Kim DW, Chung DH. Concomitant ALK translocation and EGFR mutation in lung cancer: a comparison of direct sequencing and sensitive assays and the impact on responsiveness to tyrosine kinase inhibitor. Ann Oncol. 2015;26(2):348–354. doi: 10.1093/annonc/mdu530. [DOI] [PubMed] [Google Scholar]
- 7.Suda K, Tomizawa K, Mitsudomi T. Biological and clinical significance of KRAS mutations in lung cancer: an oncogenic driver that contrasts with EGFR mutation. Cancer Metastasis Rev. 2010;29(1):49–60. doi: 10.1007/s10555-010-9209-4. [DOI] [PubMed] [Google Scholar]
- 8.Baik CS, Myall NJ, Wakelee HA. Targeting BRAF-mutant non-small cell lung Cancer: from molecular profiling to rationally designed therapy. Oncologist. 2017;22(7):786–96. [DOI] [PMC free article] [PubMed]
- 9.Li BT, Ross DS, Aisner DL, Chaft JE, Hsu M, Kako SL, Kris MG, Varella-Garcia M, Arcila ME. HER2 amplification and HER2 mutation are distinct molecular targets in lung cancers. J Thorac Oncol. 2016;11(3):414–419. doi: 10.1016/j.jtho.2015.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee JT, Lai GY, Liao LM, Subar AF, Bertazzi PA, Pesatori AC, Freedman ND, Landi MT, Lam TK. Nut consumption and lung cancer risk: results from two large observational studies. Cancer Epidemiol Prev Biomarkers. 2017;26:826–36. [DOI] [PMC free article] [PubMed]
- 11.Terai H, Tan L, Beauchamp EM, Hatcher JM, Liu Q, Meyerson M, Gray NS, Hammerman PS. Characterization of DDR2 inhibitors for the treatment of DDR2 mutated nonsmall cell lung cancer. ACS Chem Biol. 2015;10(12):2687–2696. doi: 10.1021/acschembio.5b00655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malchers F, Dietlein F, Schöttle J, Lu X, Nogova L, Albus K, Fernandez-Cuesta L, Heuckmann JM, Gautschi O, Diebold J. Cell-autonomous and non–cell-autonomous mechanisms of transformation by amplified FGFR1 in lung cancer. Cancer Discov. 2014;4(2):246–257. doi: 10.1158/2159-8290.CD-13-0323. [DOI] [PubMed] [Google Scholar]
- 13.Pérez-Ramírez C, Cañadas-Garre M, Molina MÁ, Faus-Dáder MJ, Calleja-Hernández MÁ. PTEN and PI3K/AKT in non-small-cell lung cancer. Pharmacogenomics. 2015;16(16):1843–1862. doi: 10.2217/pgs.15.122. [DOI] [PubMed] [Google Scholar]
- 14.Kohno T, Nakaoku T, Tsuta K, Tsuchihara K, Matsumoto S, Yoh K, Goto K. Beyond ALK-RET, ROS1 and other oncogene fusions in lung cancer. Transl Lung Cancer Res. 2015;4(2):156–164. doi: 10.3978/j.issn.2218-6751.2014.11.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vaishnavi A, Capelletti M, Le AT, Kako S, Butaney M, Ercan D, Mahale S, Davies KD, Aisner DL, Pilling AB, et al. Oncogenic and drug-sensitive NTRK1 rearrangements in lung cancer. Nat Med. 2013;19(11):1469–1472. doi: 10.1038/nm.3352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Awad MM, Oxnard GR, Jackman DM, Savukoski DO, Hall D, Shivdasani P, Heng JC, Dahlberg SE, Janne PA, Verma S, et al. MET exon 14 mutations in non-small-cell lung Cancer are associated with advanced age and stage-dependent MET genomic amplification and c-met overexpression. J Clin Oncol. 2016;34(7):721–730. doi: 10.1200/JCO.2015.63.4600. [DOI] [PubMed] [Google Scholar]
- 17.D'incecco A, Andreozzi M, Ludovini V, Rossi E, Capodanno A, Landi L, Tibaldi C, Minuti G, Salvini J, Coppi E. PD-1 and PD-L1 expression in molecularly selected non-small-cell lung cancer patients. Br J Cancer. 2015;112(1):95. doi: 10.1038/bjc.2014.555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Warth A, Cortis J, Soltermann A, Meister M, Budczies J, Stenzinger A, Goeppert B, Thomas M, Herth FJ, Schirmacher P, et al. Tumour cell proliferation (Ki-67) in non-small cell lung cancer: a critical reappraisal of its prognostic role. Br J Cancer. 2014;111(6):1222–1229. doi: 10.1038/bjc.2014.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Endl E, Gerdes J. Posttranslational modifications of the KI-67 protein coincide with two major checkpoints during mitosis. J Cell Physiol. 2000;182(3):371–380. doi: 10.1002/(SICI)1097-4652(200003)182:3<371::AID-JCP8>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 20.Masuda D, Masuda R, Matsuzaki T, Imamura N, Aruga N, Tanaka M, Inokuchi S, Kijima H, Iwazaki M. Ki-67 labeling index affects tumor infiltration patterns of lung squamous cell carcinoma. Mol Med Rep. 2015;12(5):7303–7309. doi: 10.3892/mmr.2015.4354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yu JQ, Zhou Q, Zheng YF, Bao Y. Expression of vimentin and Ki-67 proteins in cervical squamous cell carcinoma and their relationships with Clinicopathological features. Asian Pac J Cancer Prev. 2015;16(10):4271–4275. doi: 10.7314/APJCP.2015.16.10.4271. [DOI] [PubMed] [Google Scholar]
- 22.Gioacchini FM, Alicandri-Ciufelli M, Magliulo G, Rubini C, Presutti L, Re M. The clinical relevance of Ki-67 expression in laryngeal squamous cell carcinoma. Eur Arch Otorhinolaryngol. 2015;272(7):1569–1576. doi: 10.1007/s00405-014-3117-0. [DOI] [PubMed] [Google Scholar]
- 23.Yin Y, Zeng K, Wu M, Ding Y, Zhao M, Chen Q. The levels of Ki-67 positive are positively associated with lymph node metastasis in invasive ductal breast cancer. Cell Biochem Biophys. 2014;70(2):1145–1151. doi: 10.1007/s12013-014-0034-1. [DOI] [PubMed] [Google Scholar]
- 24.Calik M, Demirci E, Altun E, Calik I, Gundogdu OB, Gursan N, Gundogdu B, Albayrak M. Clinicopathological importance of Ki-67, p27, and p53 expression in gastric cancer. Turk J Med Sci. 2015;45(1):118–128. doi: 10.3906/sag-1311-107. [DOI] [PubMed] [Google Scholar]
- 25.Tabata K, Tanaka T, Hayashi T, Hori T, Nunomura S, Yonezawa S, Fukuoka J. Ki-67 is a strong prognostic marker of non-small cell lung cancer when tissue heterogeneity is considered. BMC Clin Pathol. 2014;14:23. doi: 10.1186/1472-6890-14-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stathopoulos GP, Malamos NA, Markopoulos C, Polychronis A, Armakolas A, Rigatos S, Yannopoulou A, Kaparelou M, Antoniou P. The role of Ki-67 in the proliferation and prognosis of breast cancer molecular classification subtypes. Anti-Cancer Drugs. 2014;25(8):950–957. doi: 10.1097/CAD.0000000000000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Verhoven B, Yan Y, Ritter M, Khor LY, Hammond E, Jones C, Amin M, Bahary JP, Zeitzer K, Pollack A. Ki-67 is an independent predictor of metastasis and cause-specific mortality for prostate cancer patients treated on radiation therapy oncology group (RTOG) 94-08. Int J Radiat Oncol Biol Phys. 2013;86(2):317–323. doi: 10.1016/j.ijrobp.2013.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schmid SC, Zahel T, Haller B, Horn T, Metzger I, Holzapfel K, Seitz AK, Gschwend JE, Retz M, Maurer T. Prognostic value of computed tomography before radical cystectomy in patients with invasive bladder cancer: imaging predicts survival. World J Urol. 2016;34(4):569–576. doi: 10.1007/s00345-015-1654-9. [DOI] [PubMed] [Google Scholar]
- 29.Hasselblom S, Ridell B, Sigurdardottir M, Hansson U, Nilsson-Ehle H, Andersson PO. Low rather than high Ki-67 protein expression is an adverse prognostic factor in diffuse large B-cell lymphoma. Leuk Lymphoma. 2008;49(8):1501–1509. doi: 10.1080/10428190802140055. [DOI] [PubMed] [Google Scholar]
- 30.Martin B, Paesmans M, Mascaux C, Berghmans T, Lothaire P, Meert AP, Lafitte JJ, Sculier JP. Ki-67 expression and patients survival in lung cancer: systematic review of the literature with meta-analysis. Br J Cancer. 2004;91(12):2018–2025. doi: 10.1038/sj.bjc.6602233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wen S, Zhou W, Li CM, Hu J, Hu XM, Chen P, Shao GL, Guo WH. Ki-67 as a prognostic marker in early-stage non-small cell lung cancer in Asian patients: a meta-analysis of published studies involving 32 studies. BMC Cancer. 2015;15:520. doi: 10.1186/s12885-015-1524-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ahn HK, Jung M, Ha S-Y, Lee J-I, Park I, Kim YS, Hong J, Sym SJ, Park J, Shin DB. Clinical significance of Ki-67 and p53 expression in curatively resected non-small cell lung cancer. Tumor Biol. 2014;35(6):5735–5740. doi: 10.1007/s13277-014-1760-0. [DOI] [PubMed] [Google Scholar]
- 33.Ahn J-H, Kim S-W, Hong S-M, Suh C, Kim WK, Lee IC, Lee J-S. Epidermal growth factor receptor (EGFR) expression in operable non-small cell lung carcinoma. J Korean Med Sci. 2004;19(4):529–535. doi: 10.3346/jkms.2004.19.4.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Anami Y, Iijima T, Suzuki K, Yokota J, Minami Y, Kobayashi H, Satomi K, Nakazato Y, Okada M, Noguchi M. Bronchioloalveolar carcinoma (lepidic growth) component is a more useful prognostic factor than lymph node metastasis. J Thorac Oncol. 2009;4(8):951–958. doi: 10.1097/JTO.0b013e3181ad8631. [DOI] [PubMed] [Google Scholar]
- 35.Apostolova I, Ego K, Steffen IG, Buchert R, Wertzel H, Achenbach HJ, Riedel S, Schreiber J, Schultz M, Furth C. The asphericity of the metabolic tumour volume in NSCLC: correlation with histopathology and molecular markers. Eur J Nucl Med Mol Imaging. 2016;43(13):2360–2373. doi: 10.1007/s00259-016-3452-z. [DOI] [PubMed] [Google Scholar]
- 36.Berghoff A, Ilhan-Mutlu A, Wöhrer A, Hackl M, Widhalm G, Hainfellner J, Dieckmann K, Melchardt T, Dome B, Heinzl H. Prognostic significance of Ki67 proliferation index, HIF1 alpha index and microvascular density in patients with non-small cell lung cancer brain metastases. Strahlenther Onkol. 2014;190(7):676–685. doi: 10.1007/s00066-014-0639-8. [DOI] [PubMed] [Google Scholar]
- 37.Boehm J, Koch S, Gais P, Juetting U, Praeuer HW, Hoefler H. Prognosis value of MIB-1 in neuroendocrine tumors of the lung. J Pathol. 1996;178(4):402–409. doi: 10.1002/(SICI)1096-9896(199604)178:4<402::AID-PATH498>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 38.Cardona AF, Rojas L, Wills B, Arrieta O, Carranza H, Vargas C, Otero J, Cuello M, Corrales L, Martín C. Pemetrexed/carboplatin/bevacizumab followed by maintenance pemetrexed/bevacizumab in Hispanic patients with non-squamous non-small cell lung cancer: outcomes according to thymidylate synthase expression. PLoS One. 2016;11(5):e0154293. doi: 10.1371/journal.pone.0154293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Corzani R, Luzzi L, Spina D, Voltolini L, Paladini P, Ghiribelli C, Ghisalberti M, Borrelli R, Meniconi F, Monaci N. The prognostic significance of proliferative indices in surgically resected IIIA-N2 non-small cell lung cancer after induction chemotherapy. J Cardiovasc Surg. 2014;58:763–9. [DOI] [PubMed]
- 40.Del Gobbo A, Pellegrinelli A, Gaudioso G, Castellani M, Zito Marino F, Franco R, Palleschi A, Nosotti M, Bosari S, Vaira V. Analysis of NSCLC tumour heterogeneity, proliferative and 18F-FDG PET indices reveals Ki67 prognostic role in adenocarcinomas. Histopathology. 2016;68(5):746–751. doi: 10.1111/his.12808. [DOI] [PubMed] [Google Scholar]
- 41.Demarchi LMMF, Reis MM, Palomino SAP, Farhat C, Takagaki TY, Beyruti R, Saldiva PHN, Capelozzi VL. Prognostic values of stromal proportion and PCNA, Ki-67, and p53 proteins in patients with resected adenocarcinoma of the lung. Mod Pathol. 2000;13(5):511. doi: 10.1038/modpathol.3880089. [DOI] [PubMed] [Google Scholar]
- 42.Dingemans A-MC, Witlox MA, Stallaert RA, van der Valk P, Postmus PE, Giaccone G. Expression of DNA topoisomerase IIα and topoisomerase IIβ genes predicts survival and response to chemotherapy in patients with small cell lung cancer. Clin Cancer Res. 1999;5(8):2048–2058. [PubMed] [Google Scholar]
- 43.Dong B, Sato M, Sakurada A, Sagawa M, Endo C, Wu S, Yamanaka S, Horii A, Kondo T. Computed tomographic images reflect the biologic behavior of small lung adenocarcinoma: they correlate with cell proliferation, microvascularization, cell adhesion, degradation of extracellular matrix, and K-ras mutation. J Thorac Cardiovasc Surg. 2005;130(3):733–739. doi: 10.1016/j.jtcvs.2005.05.013. [DOI] [PubMed] [Google Scholar]
- 44.Erler BS, Presby MM, Finch M, Hodges A, Horowitz K, Topilow AA, Matulewicz T. CD117, Ki-67, and p53 predict survival in neuroendocrine carcinomas, but not within the subgroup of small cell lung carcinoma. Tumor Biol. 2011;32(1):107–111. doi: 10.1007/s13277-010-0104-y. [DOI] [PubMed] [Google Scholar]
- 45.Filipits M, Pirker R, Dunant A, Lantuejoul S, Schmid K, Huynh A, Haddad V, André F, Stahel R, Pignon J-P. Cell cycle regulators and outcome of adjuvant cisplatin-based chemotherapy in completely resected non–small-cell lung cancer: the international adjuvant lung Cancer trial biologic program. J Clin Oncol. 2007;25(19):2735–2740. doi: 10.1200/JCO.2006.08.2867. [DOI] [PubMed] [Google Scholar]
- 46.Fontanini G, Vignati S, Bigini D, Mussi A, Lucchi M, Chine S, Angeletti CA, Bevilacqua G. Recurrence and death in non-small cell lung carcinomas: a prognostic model using pathological parameters, microvessel count, and gene protein products. Clin Cancer Res. 1996;2(6):1067–1075. [PubMed] [Google Scholar]
- 47.Fujioka S, Shomori K, Nishihara K, Yamaga K, Nosaka K, Araki K, Haruki T, Taniguchi Y, Nakamura H, Ito H. Expression of minichromosome maintenance 7 (MCM7) in small lung adenocarcinomas (pT1): prognostic implication. Lung Cancer. 2009;65(2):223–229. doi: 10.1016/j.lungcan.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 48.Gasinska A, Kolodziejski L, Niemiec J, Dyczek S. Clinical significance of biological differences between cavitated and solid form of squamous cell lung cancer. Lung Cancer. 2005;49(2):171–179. doi: 10.1016/j.lungcan.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 49.Haga Y, Hiroshima K, Iyoda A, Shibuya K, Shimamura F, Iizasa T, Fujisawa T, Ohwada H. Ki-67 expression and prognosis for smokers with resected stage i non–small cell lung cancer. Ann Thorac Surg. 2003;75(6):1727–1732. doi: 10.1016/S0003-4975(03)00119-X. [DOI] [PubMed] [Google Scholar]
- 50.Harpole DH, Richards WG, Herndon JE, Sugarbaker DJ. Angiogenesis and molecular biologic substaging in patients with stage I non—small cell lung cancer. Ann Thorac Surg. 1996;61(5):1470–1476. doi: 10.1016/0003-4975(96)00104-X. [DOI] [PubMed] [Google Scholar]
- 51.Hashimoto K, Araki K, Osaki M, Nakamura H, Tomita K, Shimizu E, Ito H. MCM2 and Ki-67 expression in human lung adenocarcinoma: prognostic implications. Pathobiology. 2004;71(4):193–200. doi: 10.1159/000078673. [DOI] [PubMed] [Google Scholar]
- 52.Hayashi H, Ogawa N, Ishiwa N, Yazawa T, Inayama Y, Ito T, Kitamura H. High cyclin E and low p27/Kip1 expressions are potentially poor prognostic factors in lung adenocarcinoma patients. Lung Cancer. 2001;34(1):59–65. doi: 10.1016/S0169-5002(01)00211-2. [DOI] [PubMed] [Google Scholar]
- 53.Hokka D, Maniwa Y, Tane S, Nishio W, Yoshimura M, Okita Y, Ohbayashi C, Sakai Y, Chen X, Hayashi Y. Psf3 is a prognostic biomarker in lung adenocarcinoma. Lung Cancer. 2013;79(1):77–82. doi: 10.1016/j.lungcan.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 54.Hommura F, Dosaka-Akita H, Mishina T, Nishi M, Kojima T, Hiroumi H, Ogura S, Shimizu M, Katoh H, Kawakami Y. Prognostic significance of p27KIP1 protein and ki-67 growth fraction in non-small cell lung cancers. Clin Cancer Res. 2000;6(10):4073–4081. [PubMed] [Google Scholar]
- 55.Huang C, Liu D, Masuya D, Nakashima T, Kameyama K, Ishikawa S, Ueno M, Haba R, Yokomise H. Clinical application of biological markers for treatments of resectable non-small-cell lung cancers. Br J Cancer. 2005;92(7):1231. doi: 10.1038/sj.bjc.6602481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ikeda Ji OT, Inoue M, Uekita T, Sakai R, Okumura M, Aozasa K, Morii E. Expression of CUB domain containing protein (CDCP1) is correlated with prognosis and survival of patients with adenocarcinoma of lung. Cancer Sci. 2009;100(3):429–433. doi: 10.1111/j.1349-7006.2008.01066.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Imai H, Kaira K, Oriuchi N, Yanagitani N, Sunaga N, Ishizuka T, Kanai Y, Endou H, Nakajima T, Mori M. L-type amino acid transporter 1 expression is a prognostic marker in patients with surgically resected stage I non-small cell lung cancer. Histopathology. 2009;54(7):804–813. doi: 10.1111/j.1365-2559.2009.03300.x. [DOI] [PubMed] [Google Scholar]
- 58.Inoue M, Takakuwa T, Minami M, Shiono H, Utsumi T, Kadota Y, Nasu T, Aozasa K, Okumura M. Clinicopathologic factors influencing postoperative prognosis in patients with small-sized adenocarcinoma of the lung. J Thorac Cardiovasc Surg. 2008;135(4):830–836. doi: 10.1016/j.jtcvs.2007.10.034. [DOI] [PubMed] [Google Scholar]
- 59.Jethon A, Pula B, Olbromski M, Werynska B, Muszczynska-Bernhard B, Witkiewicz W, Dziegiel P, Podhorska-Okolow M. Prognostic significance of SOX18 expression in non-small cell lung cancer. Int J Oncol. 2015;46(1):123–132. doi: 10.3892/ijo.2014.2698. [DOI] [PubMed] [Google Scholar]
- 60.Ji L, Ni T, Shen Y, Xue Q, Liu Y, Chen B, Cui X, Lv L, Yu X, Cui Y. Transformer 2β (Tra2β/SFRS10) positively regulates the progression of NSCLC via promoting cell proliferation. J Mol Histol. 2014;45(5):573–582. doi: 10.1007/s10735-014-9582-3. [DOI] [PubMed] [Google Scholar]
- 61.Ji Y, Zheng M, Ye S, Chen J, Chen Y. PTEN and Ki67 expression is associated with clinicopathologic features of non-small cell lung cancer. J Biomed Res. 2014;28(6):462. doi: 10.7555/JBR.27.20130084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kaira K, Oriuchi N, Imai H, Shimizu K, Yanagitani N, Sunaga N, Hisada T, Ishizuka T, Kanai Y, Nakajima T. Prognostic significance of L-type amino acid transporter 1 (LAT1) and 4F2 heavy chain (CD98) expression in stage I pulmonary adenocarcinoma. Lung Cancer. 2009;66(1):120–126. doi: 10.1016/j.lungcan.2008.12.015. [DOI] [PubMed] [Google Scholar]
- 63.Kawatsu Y, Kitada S, Uramoto H, Zhi L, Takeda T, Kimura T, Horie S, Tanaka F, Sasaguri Y, Izumi H. The combination of strong expression of ZNF143 and high MIB-1 labelling index independently predicts shorter disease-specific survival in lung adenocarcinoma. Br J Cancer. 2014;110:2583. [DOI] [PMC free article] [PubMed]
- 64.Tsubochi H, Sato N, Hiyama M, Kaimori M, Endo S, Sohara Y, Imai T. Combined analysis of cyclooxygenase-2 expression with p53 and Ki-67 in nonsmall cell lung cancer. Ann Thorac Surg. 2006;82(4):1198–1204. doi: 10.1016/j.athoracsur.2006.04.069. [DOI] [PubMed] [Google Scholar]
- 65.Kawatsu Y, Kitada S, Uramoto H, Zhi L, Takeda T, Kimura T, Horie S, Tanaka F, Sasaguri Y, Izumi H, Kohno K, Yamada S. The combination of strong expression of ZNF143 and high MIB-1 labelling index independently predicts shorter disease-specific survival in lung adenocarcinoma. Br J Cancer. 2014;110(10):2583–2592. doi: 10.1038/bjc.2014.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kim C-H, Lee HS, Park J-H, Choi J-H, Jang S-H, Park Y-B, Lee MG, Hyun IG, Kim KI, Kim HS. Prognostic role of p53 and Ki-67 immunohistochemical expression in patients with surgically resected lung adenocarcinoma: a retrospective study. J Thoracic Dis. 2015;7:822. doi: 10.3978/j.issn.2072-1439.2015.05.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kobierzycki C, Pula B, Werynska B, Piotrowska A, Muszczynska-Bernhard B, Dziegiel P, Rakus D. The Lack of evidence for correlation of pyruvate kinase M2 expression with tumor grade in non-small cell lung cancer. Anticancer Res. 2014;34:3811–3817. [PubMed] [Google Scholar]
- 68.Kobyakov DS, Klimachev VV, Avdalyan AM, Bobrov IP, Bychkova EY, Kruglova NM, Lazarev AF, Lushnikova EL, Nepomnyashchikh LM. Argyrophilic Proteins of Nucleolar Organizer Regions and Proliferative Activity of Cells in Squamous Cell Carcinoma of the Lung. Bull Exp Biol Med. 2014;157(5):677–682. doi: 10.1007/s10517-014-2642-6. [DOI] [PubMed] [Google Scholar]
- 69.Lei B, Liu S, Qi W, Zhao Y, Li Y, Lin N, Xu X, Zhi C, Mei J, Yan Z, Wan L, Shen H. PBK/TOPK expression in non-small-cell lung cancer: its correlation and prognostic significance with Ki67 and p53 expression. Histopathology. 2013;2013(63):696–703. doi: 10.1111/his.12215. [DOI] [PubMed] [Google Scholar]
- 70.Liu Q, Lu M, Ouyang F, Liu Y. Expression and prognosis significance of Geminin and Ki-67 protein in non small cell lung cancer. Chinese J Clin Exper Path. 2014;30:279–282. [Google Scholar]
- 71.Liu X, Ma L, Wang K. The expression of NET-1 and Ki-67 in lung cancer tissues. Chin J Gerontol. 2012;23:5297–5298. [Google Scholar]
- 72.Liu Y-Z, Jiang Y-Y, Hao J-J, Lu S-S, Zhang T-T, Shang L, Cao J, Song X, Wang B-S, Cai Y, Zhan Q-M, Wang M-R. Prognostic significance of MCM7 expression in the bronchial brushings of patients with non-small cell lung cancer (NSCLC) Lung Cancer. 2012;77(1):176–182. doi: 10.1016/j.lungcan.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 73.Xue Q, Lv L, Wan C, Chen B, Li M, Ni T, Liu Y, Liu Y, Cong X, Zhou Y, Ni R, Mao G. Expression and clinical role of small glutamine-rich tetratricopeptide repeat (TPR)-containing protein alpha (SGTA) as a novel cell cycle protein in NSCLC. J Cancer Res Clin Oncol. 2013;139(9):1539–1549. doi: 10.1007/s00432-013-1474-5. [DOI] [PubMed] [Google Scholar]
- 74.Maki Y, Soh J, Ichimura K, Shien K, Furukawa M, Muraoka T, Tanaka N, Ueno T, Yamamoto H, Asano H, et al. Impact of GLUT1 and Ki-67 expression on earlystage lung adenocarcinoma diagnosed according to a new international multidisciplinary classification. Oncol Rep. 2013;29:133–140. doi: 10.3892/or.2012.2087. [DOI] [PubMed] [Google Scholar]
- 75.Roberto Storte Matheus, Fabiola Del Carlo Bernardi, Célia Petrossi Gallo, Alecsander Pereira da Silva, Olavo Ribeiro Rodrigues, Marisa Capelozzi, Ademar Lopes, Sandra Fenezelian, Paulo Hilário Nascimento Saldiva, Vera Luiza Capelozzi, (2004) Nuclear markers (star volume, mitotic index, AgNOR and Ki-67) of the primary tumor and its metastasis in non-small cell lung carcinomas. Pathol Res Pract 200 (1):13-23 [DOI] [PubMed]
- 76.Minami K-i, Saito Y, Imamura H, Okamura A. Prognostic significance of p53, Ki-67, VEGF and Glut-1 in resected stage I adenocarcinoma of the lung. Lung Cancer. 2002;38(1):51–57. doi: 10.1016/S0169-5002(02)00108-3. [DOI] [PubMed] [Google Scholar]
- 77.Mohamed S, Yasufuku K, Hiroshima K, Nakajima T, Yoshida S, Suzuki M, Sekine Y, Shibuya K, Iizasa T, Farouk A, Fujisawa T. Prognostic implications of cell cycle-related proteins in primary resectable pathologic N2 nonsmall cell lung cancer. Cancer. 2007;109(12):2506–2514. doi: 10.1002/cncr.22651. [DOI] [PubMed] [Google Scholar]
- 78.Mojtahedzadeh S, Hashimoto S, Nakashima Y, Koga T, Matsuo Y, Yoshino I, Sugio K, Kinukawa N, Sugimachi K, Sueishi K. Clinicopathologic Relevance of Apoptotic and Proliferative Factors in Human Lung Adenocarcinoma: Fas Expression Correlates with the Histologic Subtype, But Not with the Degree of Apoptosis. Pathol Res Pract. 2002;198(10):645–654. doi: 10.1078/0344-0338-00316. [DOI] [PubMed] [Google Scholar]
- 79.Morero JL, Poleri C, Martín C, Van Kooten M, Chacón R, Rosenberg M. Influence of Apoptosis and Cell Cycle Regulator Proteins on Chemotherapy Response and Survival in Stage IIIA/IIIB NSCLC Patients. J Thorac Oncol. 2007;2(4):293–298. doi: 10.1097/01.JTO.0000263711.54073.fa. [DOI] [PubMed] [Google Scholar]
- 80.Nguyen VN, Miřejovský P, Miejovský T, Melínová L, Mandys V. Expression of cyclin D1, Ki-67 and PCNA in non-small cell lung cancer: prognostic significance and comparison with p53 and bcl-2. Acta Histochem. 2000;102(3):323–338. doi: 10.1078/S0065-1281(04)70039-2. [DOI] [PubMed] [Google Scholar]
- 81.Niemiec J, Kolodziejski L, Dyczek S. EGFR LI and Ki-67 LI are independent prognostic parameters influencing survivals of surgically treated squamous cell lung cancer patients. Neoplasma. 2005;52:231–237. [PubMed] [Google Scholar]
- 82.Nozawa N, Hashimoto S, Nakashima Y, Matsuo Y, Koga T, Sugio K, Niho Y, Harada M, Sueishi K. Immunohistochemical α- and β-catenin and E-cadherin expression and their clinicopathological significance in human lung adenocarcinoma. Pathol Res Pract. 2006;202(9):639–650. doi: 10.1016/j.prp.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 83.Oka S, Uramoto H, Shimokawa H, Iwanami T, Tanaka F. The expression of Ki-67, but not proliferating cell nuclear antigen, predicts poor disease free survival in patients with adenocarcinoma of the lung. Anticancer Res. 2011;31:4277–4282. [PubMed] [Google Scholar]
- 84.Pelosi G, Fraggetta F, Pasini F, Maisonneuve P, Sonzogni A, Iannucci A, Terzi A, Bresaola E, Valduga F, Lupo C. Immunoreactivity for thyroid transcription factor-1 in stage I non–small cell carcinomas of the lung. Am J Surg Pathol. 2001;25:363–372. doi: 10.1097/00000478-200103000-00011. [DOI] [PubMed] [Google Scholar]
- 85.Pelosi G, Pastorino U, Pasini F, Maissoneuve P, Fraggetta F, Lannucci A, Sonzogni A, De Manzoni G, Terzi A, Durante E, Bresaola E, Pezzella F, Viale G. Independent prognostic value of fascin immunoreactivity in stage I nonsmall cell lung cancer. Br J Cancer. 2003;88(4):537–547. doi: 10.1038/sj.bjc.6600731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Poleri C, Morero JL, Nieva B, Vaézquez MF, Rodriéguez C, de Titto E, Rosenberg M. Risk of Recurrence in Patients With Surgically Resected Stage I Non-small Cell Lung Carcinomaa. Chest. 2003;123(6):1858–1867. doi: 10.1378/chest.123.6.1858. [DOI] [PubMed] [Google Scholar]
- 87.Puglisi F, Aprile G, Bruckbauer M, Barbone F, Damante G, Guerra S, Beltrami CA, Di Loreto C. Combined analysis of MIB-1 and thyroid transcription factor-1 predicts survival in non-small cell lung carcinomas. Cancer Lett. 2001;162(1):97–103. doi: 10.1016/S0304-3835(00)00625-X. [DOI] [PubMed] [Google Scholar]
- 88.Pujol J-L, Simony J, Jolimoy G, Jaffuel D, Demoly P, Quantin X, Marty-Ané C, Boher J-M, Charpentier R, Michel F-B. Hypodiploidy, Ki-67 growth fraction and prognosis of surgically resected lung cancers. Br J Cancer. 1996;74(6):964–970. doi: 10.1038/bjc.1996.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Saad AG, Yeap BY, Thunnissen FBJM, Pinkus GS, Pinkus JL, Loda M, Sugarbaker DJ, Johnson BE, Chirieac LR. Immunohistochemical markers associated with brain metastases in patients with nonsmall cell lung carcinoma. Cancer. 2008;113(8):2129–2138. doi: 10.1002/cncr.23826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Salvi S, Fontana V, Boccardo S, Merlo DF, Margallo E, Laurent S, Morabito A, Rijavec E, Bello MGD, Mora M, Ratto GB, Grossi F, Truini M, Pistillo MP. Evaluation of CTLA-4 expression and relevance as a novel prognostic factor in patients with non-small cell lung cancer. Cancer Immunol Immunother. 2012;61(9):1463–1472. doi: 10.1007/s00262-012-1211-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Scagliotti GV, Micela M, Gubetta L, Leonardo E, Cappia S, Borasio P, Pozzi E. Prognostic significance of Ki67 labelling in resected non small cell lung cancer. Eur J Cancer. 1993;29(3):363–365. doi: 10.1016/0959-8049(93)90387-U. [DOI] [PubMed] [Google Scholar]
- 92.Shiba M, Kohno H, Kakizawa K, Iizasa T, Otsuji M, Saitoh Y, Hiroshima K, Ohwada H, Fujisawa T. Ki-67 immunostaining and other prognostic factors including tobacco smoking in patients with resected nonsmall cell lung carcinoma. Cancer. 2000;89(7):1457–1465. doi: 10.1002/1097-0142(20001001)89:7<1457::AID-CNCR7>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 93.Shimizu K, Maeda A, Yukawa T, Nojima Y, Saisho S, Okita R, Nakata M. Difference in prognostic values of maximal standardized uptake value on fluorodeoxyglucose-positron emission tomography and cyclooxygenase-2 expression between lung adenocarcinoma and squamous cell carcinoma. World J Surg Oncol. 2014;12(1):343. doi: 10.1186/1477-7819-12-343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Takahashi S, Kamata Y, Tamo W, Koyanagi M, Hatanaka R, Yamada Y, Tsushima T, Takaya S, Fukuda I. Relationship between postoperative recurrence and expression of cyclin E, p27, and Ki-67 in nonsmall cell lung cancer without lymph node metastases. Int J Clin Oncol. 2002;7(6):349–355. doi: 10.1007/s101470200053. [DOI] [PubMed] [Google Scholar]
- 95.Tsoukalas NG, Giaginis C, Alexandrou P, Tolia M, Bournakis E, Papakostidi A, Sfiniadakis I, Kavantzas N, Agapitos E, Patsouris E, Theocharis S. 1650pthe Clinical and Pathological Significance of Cyclooxygenase-2 (cox-2) and Human Antigen Receptor (hur) Expression in Non Small Cell Lung Cancers. Ann Oncol. 2014;25(suppl_4):iv569-iv570.
- 96.Vigouroux C, Casse J-M, Battaglia-Hsu S-F, Brochin L, Luc A, Paris C, Lacomme S, Gueant J-L, Vignaud J-M, Gauchotte G. Methyl(R217)HuR and MCM6 are inversely correlated and are prognostic markers in non small cell lung carcinoma. Lung Cancer. 2015;89(2):189–196. doi: 10.1016/j.lungcan.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 97.Wakabayashi O, Yamazaki K, Oizumi S, Hommura F, Kinoshita I, Ogura S, Dosaka-Akita H, Nishimura M. CD4+ T cells in cancer stroma, not CD8+ T cells in cancer cell nests, are associated with favorable prognosis in human non-small cell lung cancers. Cancer Sci. 2003;94(11):1003–1009. doi: 10.1111/j.1349-7006.2003.tb01392.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wang A, Cai X, Zhou T, Liu J. Correlation between the expression of MMP-2, VEGF, CD1105 and Ki-67 in small cell lung cancer and their prognostic value. Chin Clin Oncol. 2012;17:988–993. [Google Scholar]
- 99.Wang H, Liao S. The correlation of Ki-67 and prognosis of non small cell lung cancer. Chin J Clin Oncol. 1999;26:309–310. [Google Scholar]
- 100.Wang X, Wang H, Tian T, Han X, Xu M. The expression and clinical value of Ki67, bcl-2 and bax in non-small cell lung cancers. Beijing Med J. 2005;26:744–746. [Google Scholar]
- 101.Wang Y, ZHOU Q, Wang D, Zhang S, Niang C, Zhang H. A Study on Relationship between Tumor Cell Proliferation, Apoptosis and Prognosis in Patients with Primary Lung cancer. Can Res Prev Treat. 2001;28:339–341. [Google Scholar]
- 102.Werynska B, Pula B, Muszczynska-Bernhard B, Piotrowska A, Jethon A, Podhorska-Okolow M, Dziegiel P, Jankowska R. Correlation between expression of metallothionein and expression of Ki-67 and MCM-2 proliferation markers in non-small cell lung cancer. Anticancer Res. 2011;31:2833–2839. [PubMed] [Google Scholar]
- 103.Woo T, Okudela K, Yazawa T, Wada N, Ogawa N, Ishiwa N, Tajiri M, Rino Y, Kitamura H, Masuda M. Prognostic value of KRAS mutations and Ki-67 expression in stage I lung adenocarcinomas. Lung Cancer. 2009;65(3):355–362. doi: 10.1016/j.lungcan.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 104.Wu J, Zhou J, Yao L, Lang Y, Liang Y, Chen L, Zhang J, Wang F, Wang Y, He C, Ma J. High expression of M3 muscarinic acetylcholine receptor is a novel biomarker of poor prognostic in patients with non-small cell lung cancer. Tumor Biol. 2013;34(6):3939–3944. doi: 10.1007/s13277-013-0982-x. [DOI] [PubMed] [Google Scholar]
- 105.Wu Q, Qian Y-M, Zhao X-L, Wang S-M, Feng X-J, Chen X-F, Zhang S-H. Expression and prognostic significance of centromere protein A in human lung adenocarcinoma. Lung Cancer. 2012;77(2):407–414. doi: 10.1016/j.lungcan.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 106.Wu S, Cheng Z, Yu L, Song W, Tao Y. Expression of p16 and Ki67 and their correlation with prognosis in nonsmall cell lung cancer. Chinese J Histochem Cytochem. 2011;20:605–609. [Google Scholar]
- 107.Xu M, Yang X, Zhao J, Zhang J, Zhang S, Huang H, Liu Y, Liu J. High expression of Cullin1 indicates poor prognosis for NSCLC patients. Pathol Res Pract. 2014;210(7):397–401. doi: 10.1016/j.prp.2014.01.015. [DOI] [PubMed] [Google Scholar]
- 108.Xu Y, Liu B, Shi Q-L, Huang P-L, Zhou X-J, Ma H-H, Lu Z-F, Bo Y, Eriksson S, He E. Thymidine kinase 1 is a better prognostic marker than Ki-67 for pT1 adenocarcinoma of the lung. Int J Clin Exp Med. 2014;7:2120. [PMC free article] [PubMed] [Google Scholar]
- 109.Yamashita S-i, Moroga T, Tokuishi K, Miyawaki M, Chujo M, Yamamoto S, Kawahara K. Ki-67 Labeling Index Is Associated with Recurrence after Segmentectomy under Video-assisted Thoracoscopic Surgery in Stage I Non-small Cell Lung Cancer. Ann Thorac Cardiovasc Surg. 2011;17(4):341–346. doi: 10.5761/atcs.oa.10.01573. [DOI] [PubMed] [Google Scholar]
- 110.Yang J, Ramnath N, Moysich KB, Asch HL, Swede H, Alrawi SJ, Huberman J, Geradts J, Brooks JSJ, Tan D. Prognostic significance of MCM2, Ki-67 and gelsolin in non-small cell lung cancer. BMC Cancer. 2006;6(1) [DOI] [PMC free article] [PubMed]
- 111.Yang W, Zhang Y, Zheng F, Sun X, Dianbin M, Yu J. Imaging proliferation of 18F-FLT PET/CT correlated with the expression of microvessel density of tumour tissue in nonsmall-cell lung cancer. Eur J Nucl Med Mol Imaging. 2012;39(8):1289–1296. doi: 10.1007/s00259-012-2126-8. [DOI] [PubMed] [Google Scholar]
- 112.Yoo J, Jung JH, Lee MA, Seo KJ, Shim BY, Kim SH, Cho DG, Ahn MI, Kim CH, Cho KD. Immunohistochemical analysis of non-small cell lung cancer: correlation with clinical parameters and prognosis. J Korean Med Sci. 2007;22:318–325. doi: 10.3346/jkms.2007.22.2.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Yuan K, Zheng R. The Correlation between the Expression of H IF-2a and the Proliferation of Tum or and Its Impaction on the Prognosis in Human Non—small Cell lung Cance. Chinese J Clin Medicin. 2009;16:194–197. [Google Scholar]
- 114.Zhang X, Deng C, Qu Y. Clinical Characteristics and Prognostic Factors of 616 Cases of Patients with Lung Adenocarcinoma. J Med Res. 2015:53–6.
- 115.Zhong X, Guan X, Liu W, Zhang L. Aberrant expression of NEK2 and its clinical significance in non-small cell lung cancer. Oncol Lett. 2014;8:1470–1476. doi: 10.3892/ol.2014.2396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Zhou S, Xu Z, Zhang H, Liu Z. Proliferation and apoptosis in stage-I NSCLC and their clinical implications. Chinese J Prac Inter Med. 2007;27:1031–1033. [Google Scholar]
- 117.Zu Y, Wang X, Liu X. Chen y, Li C, Shang X, Xie Y, Zhao H, Wang J: Expression and Clinical Significance of the Thyroid Transcription Factor 1 in Xuanwei Lung Adenocarcinoma. Chinese J Lung Can. 2013;16:131–137. doi: 10.3779/j.issn.1009-3419.2013.03.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Maddau C, Confortini M, Bisanzi S, Janni A, Montinaro F, Paci E, Pontenani G, Rulli P, Salani A, Zappa M, Benvenuti A. Prognostic Significance of p53 and Ki-67 Antigen Expression in Surgically Treated Non–small Cell Lung Cancer: Immunocytochemical Detection With Imprint Cytology. Am J Clin Pathol. 2006;125(3):425–431. doi: 10.1309/DQ2AGXV2P8QT0001. [DOI] [PubMed] [Google Scholar]
- 119.Mehdi SA, Tatum AH, Newman NB, Gamble GP, Etzell JE, Weidner N, Kern JA, Sorscher SM, Kohman LJ, Graziano SL. Prognostic markers in resected stage I and II non small-cell lung cancer: an analysis of 260 patients with 5 year follow-up. Clin Lung Cancer. 1999;1:59–67. doi: 10.3816/CLC.1999.n.004. [DOI] [PubMed] [Google Scholar]
- 120.Pence JC, Kerns B-JM, Dodge RK, Iglehart JD. Prognostic Significance of the Proliferation Index in Surgically Resected Non—Small-Cell Lung Cancer. Arch Surg. 1993;128:1382–1390. doi: 10.1001/archsurg.1993.01420240090017. [DOI] [PubMed] [Google Scholar]
- 121.Ramnath N, Hernandez FJ, Tan D-F, Huberman JA, Natarajan N, Beck AF, Hyland A, Todorov IT, Brooks JS, Bepler G. MCM2 is an independent predictor of survival in patients with non–small-cell lung cancer. J Clin Oncol. 2001;19:4259–4266. doi: 10.1200/JCO.2001.19.22.4259. [DOI] [PubMed] [Google Scholar]
- 122.Sterlacci W, Tzankov A, Veits L, Oberaigner W, Schmid T, Hilbe W, Fiegl M. The prognostic impact of sex on surgically resected non–small cell lung cancer depends on clinicopathologic characteristics. Am J Clin Pathol. 2011;135:611–618. doi: 10.1309/AJCPQF24NYWNMVMG. [DOI] [PubMed] [Google Scholar]
- 123.Stewart DJ, Nunez MI, Behrens C, Liu D, Lin YH, Lee JJ, Roth J, Heymach J, Swisher SG, Hong WK. Membrane Carbonic Anhydrase IX Expression and Relapse Risk in Resected Stage I–II Non–Small-Cell Lung Cancer. J Thorac Oncol. 2014;9:675–684. doi: 10.1097/JTO.0000000000000148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Kaira K, Oriuchi N, Imai H, Shimizu K, Yanagitani N, Sunaga N, Hisada T, Tanaka S, Ishizuka T, Kanai Y. Prognostic significance of L-type amino acid transporter 1 expression in resectable stage I–III nonsmall cell lung cancer. Br J Cancer. 2008;98:742. doi: 10.1038/sj.bjc.6604235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Sobecki M, Mrouj K, Colinge J, Gerbe F, Jay P, Krasinska L, Dulic V, Fisher D. Cell-cycle regulation accounts for variability in Ki-67 expression levels. Cancer Res. 2017;77(10):2722–2734. doi: 10.1158/0008-5472.CAN-16-0707. [DOI] [PubMed] [Google Scholar]
- 126.Murlidhar V, Reddy RM, Fouladdel S, Zhao L, Ishikawa MK, Grabauskiene S, Zhang Z, Lin J, Chang AC, Carrott P. Poor prognosis indicated by venous circulating tumor cell clusters in early-stage lung cancers. Cancer Res. 2017;77:5194–206. [DOI] [PMC free article] [PubMed]
- 127.Genbacev O, McMaster MT, Lazic J, Nedeljkovic S, Cvetkovic M, Joslin R, Fisher SJ. Concordant in situ and in vitro data show that maternal cigarette smoking negatively regulates placental cytotrophoblast passage through the cell cycle☆. Reprod Toxicol. 2000;14(6):495–506. doi: 10.1016/S0890-6238(00)00107-6. [DOI] [PubMed] [Google Scholar]
- 128.Chiappara G, Gjomarkaj M, Sciarrino S, Vitulo P, Pipitone L, Pace E. Altered expression of p21, activated caspase-3, and PCNA in bronchiolar epithelium of smokers with and without chronic obstructive pulmonary disease. Exp Lung Res. 2014;40(7):343–353. doi: 10.3109/01902148.2014.928836. [DOI] [PubMed] [Google Scholar]
- 129.Byeon IJ, Li H, Song H, Gronenborn AM, Tsai MD. Sequential phosphorylation and multisite interactions characterize specific target recognition by the FHA domain of Ki67. Nat Struct Mol Biol. 2005;12(11):987–993. doi: 10.1038/nsmb1008. [DOI] [PubMed] [Google Scholar]
- 130.Mikkonen L, Pihlajamaa P, Sahu B, Zhang FP, Janne OA. Androgen receptor and androgen-dependent gene expression in lung. Mol Cell Endocrinol. 2010;317(1–2):14–24. doi: 10.1016/j.mce.2009.12.022. [DOI] [PubMed] [Google Scholar]
- 131.Stakisaitis D, Mozuraite R, Kavaliauskaite D, Slekiene L, Balnyte I, Juodziukyniene N, Valanciute A. Sex-related differences of urethane and sodium valproate effects on Ki-67 expression in urethane-induced lung tumors of mice. Exp Ther Med. 2017;13(6):2741–2750. doi: 10.3892/etm.2017.4324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Inwald EC, Klinkhammer-Schalke M, Hofstadter F, Zeman F, Koller M, Gerstenhauer M, Ortmann O. Ki-67 is a prognostic parameter in breast cancer patients: results of a large population-based cohort of a cancer registry. Breast Cancer Res Treat. 2013;139(2):539–552. doi: 10.1007/s10549-013-2560-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Fabbri A, Cossa M, Sonzogni A, Papotti M, Righi L, Gatti G, Maisonneuve P, Valeri B, Pastorino U, Pelosi G. Ki-67 labeling index of neuroendocrine tumors of the lung has a high level of correspondence between biopsy samples and surgical specimens when strict counting guidelines are applied. Virchows Arch. 2017;470(2):153–64. [DOI] [PubMed]
- 134.Yalcin SE, Ocal I, Yalcin Y, Selim HS, Caltekin MD, Aydogmus H, Kelekci S. Evaluation of the Ki-67 proliferation index and Urocortin expression in women with ovarian Endometriomas. Eurasian J Med. 2017;49(2):107–112. doi: 10.5152/eurasianjmed.2017.17070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Nakano T, Ohno T, Ishikawa H, Suzuki Y, Takahashi T. Current advancement in radiation therapy for uterine cervical cancer. J Radiat Res. 2010;51(1):1–8. doi: 10.1269/jrr.09132. [DOI] [PubMed] [Google Scholar]
- 136.Kim B, Ys B, Kim SH, Hj J, Hong SW, Yoon SO. Usefulness of Ki-67 (MIB-1) immunostaining in the diagnosis of pulmonary sclerosing hemangiomas. Apmis. 2013;121(2):105–110. doi: 10.1111/j.1600-0463.2012.02945.x. [DOI] [PubMed] [Google Scholar]
- 137.Chierico L, Rizzello L, Guan L, Joseph AS, Lewis A, Battaglia G. The role of the two splice variants and extranuclear pathway on Ki-67 regulation in non-cancer and cancer cells. PLoS One. 2017;12(2):e0171815. doi: 10.1371/journal.pone.0171815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ibrahim T, Farolfi A, Scarpi E, Mercatali L, Medri L, Ricci M, Nanni O, Serra L, Amadori D. Hormonal receptor, human epidermal growth factor receptor-2, and Ki67 discordance between primary breast cancer and paired metastases: clinical impact. Oncology. 2013;84(3):150–157. doi: 10.1159/000345795. [DOI] [PubMed] [Google Scholar]
- 139.Chlebowski RT, Col N, Winer EP, Collyar DE, Cummings SR, Vogel VG, III, Burstein HJ, Eisen A, Lipkus I, Pfister DG. American Society of Clinical Oncology technology assessment of pharmacologic interventions for breast cancer risk reduction including tamoxifen, raloxifene, and aromatase inhibition. J Clin Oncol. 2002;20(15):3328–3343. doi: 10.1200/JCO.2002.06.029. [DOI] [PubMed] [Google Scholar]
- 140.Blancato J, Singh B, Liu A, Liao D, Dickson R. Correlation of amplification and overexpression of the c-myc oncogene in high-grade breast cancer: FISH, in situ hybridisation and immunohistochemical analyses. Br J Cancer. 2004;90(8):1612. doi: 10.1038/sj.bjc.6601703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Jonat W, Arnold N. Is the Ki-67 labelling index ready for clinical use? Ann Oncol. 2011;22:500–2. [DOI] [PubMed]
- 142.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 143.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16. doi: 10.1186/1745-6215-8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med. 1998;17(24):2815–2834. doi: 10.1002/(SICI)1097-0258(19981230)17:24<2815::AID-SIM110>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- 146.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 147.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Forest plots for the relationships between Ki-67 expression and clinicopathological features of patients with lung cancer. A. Age B. Gender C. Histological type. (TIF 4444 kb)
Figure S2. Forest plots for the relationships between Ki-67 expression and clinicopathological features of patients with lung cancer. A. Differentiation B. Pathologic stage C. Tumor size. (TIF 3759 kb)
Figure S3. Forest plots for the relationships between Ki-67 expression and clinicopathological features of patients with lung cancer. A. Lymph node B. TNM stage C. Smoking. (TIF 3186 kb)
Figure S4. Funnel plots for publication bias of clinicopathological features meta-analysis (A~C). A. Age B. Gender C. Histological type. (TIF 20061 kb)
Figure S5. Funnel plots for publication bias of clinicopathological features meta-analysis (D~F). A. Differentiation B. Pathologic stage C. Tumor size. (TIF 21452 kb)
Figure S6. Funnel plots for publication bias of clinicopathological features meta-analysis (G~J). A. Tumor stage B. Lymph node C. TNM stage. (TIF 21299 kb)
Figure S7. Funnel plot for publication bias of clinicopathological features meta-analysis (Smoking status). (TIF 7465 kb)
PRISMA 2009 Checklist. (DOC 63 kb)
Data Availability Statement
The databases which we collection Literature include PubMed, Web of Science, EMBASE, and Chinese datasets (WanFang, China National Knowledge Infrastructure and Chinese VIP) until June 1, 2017.