Abstract
We present three cases of cardiac arrest at different stages of pathology. Acute myocardial infarction and resulting heart failure is emerging as the leading cause of mortality. In the long run, acute episodes and cardiac remodelling can cause considerable damage and result in heart failure. In these cases, individualized homeopathic therapy was instituted along with the conventional medicines and the results were encouraging. The changes in the laboratory diagnostic parameters (single-photon emission computed tomography, electrocardiograph, echocardiography and ejection fraction as the case may be) are demonstrated over time. The key result seen in all three cases was the preservation of general well-being while the haemodynamic states also improved. While the three cases provide evidence of positive outcomes for homeopathic therapy, more extensive studies are required in a hospital setting to establish the real extent to which this therapy may be employed.
Keywords: Cardiovascular, heart failure, homeopathy
Introduction
Cardiovascular disorders (cardiovascular disease (CVD)) in general and acute myocardial infarction (AMI) are responsible for 31% of all deaths globally and are a leading cause of mortality. While it is true that modern therapeutic interventions have reduced this considerably, the challenge remains.1,2 The risk of re-infarction is also great in survivors (8%– 10% have re-infarctions within a year) making it even more important to have care available for emergencies.
The situation is further complicated by the incidence of arrhythmias along with AMI, in which case the person may proceed to heart failure and cardiogenic shock.3 Advanced age, atrial fibrillation (AF) and anterior infarction herald a poor prognosis in the case of AMI with approximately 50% of deaths occurring in the first month after the episode, most within the first 2 h.3,4 The first goal is reperfusion of the myocardium, so primary percutaneous coronary intervention (PCI) is the first line of therapy along with fibrinolytics and other cardiac drugs (except when contraindicated).5
After myocardial infarction (MI), along with local inflammation, inflammatory processes are known to occur in remote parts of the heart6 and in the kidney glomeruli7 indicating the involvement of the entire immune system in an attempt at repair. Despite the diagnosis being the similar, it is seen that the process of inflammation and repair of the tissue after MI do not evoke the same response in everybody. The mechanism of harmful heart remodelling after a MI includes numerous cellular, extracellular and neurohumoral components8 and in most cases, the size of scar formed is proportionate to the severity of heart remodelling, but it has also been demonstrated that size of scar need not translate into severe heart remodelling.9
The evidence is more in favour of the energy state of the person and its bearing on the reparative process. The harmful remodelling under ischaemic conditions is primarily consistent with the lack of energy production. It has been reported that the reduced glucose uptake at the level of the heart cells due to the genetically induced liver X receptor α (LXRα) deficiency leads to a severe damage after MI, which indirectly confirms that during ischaemia the adaptive transfer mechanism of the energy production is activated in the heart, from the fatty acid metabolism to the glucose metabolism which has greater oxidative utilization for synthesis of Adinosine Tri Phosphate (ATP).10 A healthy heart quickly activates this cardio protective mechanism in the condition of ischaemia which reduces the damage.11 This is delayed or absent in a weaker state of the person.
The current therapeutic options, despite the advances, are far from satisfactory. The continued discovery of factors involved in the remodelling of an infarcted heart pose continuous challenges. The latest available therapeutic options include the following: interleukin 10 (IL-10),11 calcium-activated potassium channel (KCa3.1) blocking,12 basic fibroblast growth factor with the transplantation of stem cells from fat tissue13 and regenerative cell therapy14,15 but also berberine therapy,16 lycopene supplementation,17 continuous normobaric hypoxia,18 repeated controlled ischaemia19 and so on.
Classical homeopathy
The premise on which homeopathic therapeutic principles are constructed is that living organism is governed by a bioenergy which preserves health in the best possible manner depending on the circumstances of conception (genetics, epigenetics, etc.). This energy is given the name ‘vital force or the life principle’. When affected by any detrimental force (disease or disturbance), this energy marshals the tools it has at its disposal – the immune system – and combats the influence, always trying to return to normal dynamic state. During this fight, it generates symptoms that are as individualistic as there are people – the better the level of health, the stronger the individualizing symptoms.20–22
The classical homeopathic therapy, as was propounded by Samuel Hahnemann and later adapted to the contemporary health situations by James T Kent and George Vithoulkas,21–23 operates on the paradigm that every human being is born with a certain amount of energy available for his bio-social functions. The higher this energy to begin with, the better the health level.24 As such, the ability to defend itself against disease is also higher in the organism with higher energy level. The pathological stimulus affecting the healthier being, when compared to less healthy one, is warded off easily and homeostasis is re-established.
Classical homeopathic practitioner follows a certain protocol to establish the level of the patient’s health at the beginning of every case taking in order to project the possibilities with the therapy. Whereas the diagnosis helps understand the pathology in question, the real prognosis may be assessed from an understanding of the health level of the person. The better the energy complex, the better the prognosis and better the response to homeopathic therapy.24 The truth of this idea may be seen in this case series as the patients all exhibit a poor prognostic diagnosis but respond well to homeopathic therapy on account of their better health state to begin with. The same approach may not yield such favourable results in a less healthy case.
This case series presents the treatment of MI with homeopathy. It is, to best of the authors’ knowledge, the first of its kind, demonstrating treatment of acute episodes as well as the consequence of MI over time. A long-term follow-up has been provided with laboratory investigations for the purpose of comparison.
Case presentation
Case 1
The patient, a 62-year-old Serbian man with history of MI 17 years before, presented with the diagnosis of status-post MI pars anterioris and PCI left anterior descending (LAD) aa XVII; ischaemic compensatory cardiomyopathy; hypertension and diabetes mellitus type 2 were also present (Table 1).
Table 1.
Case 1 treatment details.
| Date of intervention | Symptoms | Changes in laboratory findings | Remedy | Response | Conventional medicine changes |
|---|---|---|---|---|---|
| 15 Jan 2015 | Panic attacks, tightness in chest; weakness, tachycardia; cold hands and feet; pulse – intermittent; strong acid peptic symptoms; constant catarrh of the posterior nares with post nasal secretion | SPECT (2011): LVEF = 28%, global hypokinetic ventricles, coronary angiogram (2013): LAD stent restenosis less than 50%, stenosis of the middle part less than 50% Hypertension Diabetes mellitus |
Medorrhinum 1M | Energy better the next day Increased nasal secretion Bleeding gums; panic reduced |
B-blockers, statins, ACE inhibitors, ASA, Vit B complex, selenium |
| 10 Mar 2015 | Panic attacks with intense fear of poverty | Bryonia 200C | Mild redness around neck for 1 day Mentally felt relaxed (no panic) Feet got warmer Increased hunger at forenoon |
Stopped all conventional medicines | |
| 25 May 2015 | Anxiety increased at night; discomfort in maxillary sinuses; weakness on ascending stairs | Calcarea carbonica 30C | Tiredness better; blood pressure normal; anxiety reduced, feeling calmer | ||
| 18 Aug 2015 | Severe abdominal distension causing cardiac distress | Sinus rhythm, rate 103/min, LBBB, QS in V2, reduced R inV2–V4, biphasic T wave in D1, inverted in aVL Torponin was not elevated Blood pressure: 150/90 mmHg |
Lycopodium 30C | Two similar episodes in a day; pulse was regular after administration of lycopodium | |
| 14 Oct 2015 | Increased panic attacks at night; tachycardia; blood pressure was normal even during the attack; dry cough | Natrum muriaticum 12C, increasing later to 14C | Panic reduced; cough became productive; Fever of 37.2°C–37.5°C for 2 days; lower respiratory tract infection persisted with profuse yellow expectoration and cough at night (this is excellent response – return of acute inflammatory states); increased acid peptic symptoms at night | B-blockers re introduced | |
| 30 Dec 2015 | Choking sensation with panic attack while lying on the right side at night; tachycardia; mentally very irritable; feet are warmer at night | Lachesis 30C one dose | Feels calm; took cold from exposure with earache and headache; fever for 3 days, highest at 37.6°C followed by fever for a week with temperature going up to 37°C; maxillary sinusitis with sever zygomatic pains; one episode of painful erection at night | ||
| 18 Apr 2016 | Increased bloating of stomach causing cardiac distress; decreased sexual drive; anxiety; energy better; waking at 3 a.m.; increased craving for sweets; emotionally sensitive | Blood sugar: 12.5 mmol/L later went up to 17 (normal 3.5–6.1 mmol/L) | Lycopodium 12C Increased to 14C and eventually 16C |
Abdominal bloating and acid peptic symptoms reduced; pain in left foot only while walking; lipomatous swelling on the back opened and drained on its own; panic attacks reduced in intensity; energy improved; cannot lie on the left side again | |
| 20 Jul 2016 | Sulphurous odour from urine; intense heat from knees to feet in the night; increased bleeding of gums; redness of face in the morning; flashes in the lateral visual field; left knee and heel pain during rest, better by walking | Blood sugar: 12 | Nux vomica 12C | Blood sugar dropped to 9; sexual drive improved; energy improved | |
| 1 Nov 2016 | Constant heat in feet (uncovers them), legs and hands; increased craving for sweets | Blood sugar 11 | Sulphur 12C increased till 16C gradually | Pain in legs and hip reduced; skin eruptions on the scalp; inflammation in an old abscess spot in the lower jaw, reduced on its own; two episodes of cold and fever, temperature of 37.2°C | |
| 31 May 2017 | Echocardiography: LVEDD 6.1 cm (norm 3.5–6.0 cm) LVESD 4.8 cm (norm 2.1–4.0) LVEF 40% Mitral flow – MR in trace Tricuspid flow normal Left atrial normal dimension Mitral flow – diastolic dysfunction of LV (E/A = 0.65); MR in trace LV – enlarged with hypertrophic walls; hypokinesia of septum and anterior wall |
||||
| 12 Jun 2017 | (Cardiologist opinion): SPECT showed significantly improved perfusion in this segment and only apical part of anterior wall and inferior septum are still cold without perfusion, restoration of perfusion in the area of right coronary artery or circumflex artery with persistence of distal LAD occlusion. The characteristics of SPECT in the stress and rest indicate repair of cardiomyocyte function and restoring of cardiac pump function |
SPECT: single-photon emission computed tomography; LVEF: left ventricular ejection fraction; LAD: left anterior descending; ACE: angiotensin-converting enzyme; ASA: acetyl salicylic acid; LVEDD: left ventricular end diastolic dimension; LVESD: left ventricular end systolic dimension; LVEF: left ventricular ejection fraction; MR: mitral regurgitation; LV: left ventricle; LBBB: Left Bundle Branch Block.
The patient presented on 15 January 2015 with a transient, painless ischaemic attack with a feeling of weakness in chest, paleness and cold sweating. He was hospitalized for 5 days in the intensive care unit when a coronary angiography showed restenosis of the anterior descendent artery in the stent area and the middle part of the same artery. Past medical history: He had MI 17 years ago. Posterior Coronary Artery (PCA) re-vascularization was performed with the installation of stent in the proximal part of the LAD. Diabetes mellitus and hypertension were diagnosed in 2002. He had been on B-blockers, statins, angiotensin-converting enzyme (ACE) inhibitors, acetyl salicylic acid (ASA), vitamin B complex, selenium; and not on any anti-hyperglycaemic drugs. In addition, he had gonorrhoea at 21 years – treated with antibiotics; recurrent throat infections since childhood; tonsillectomy at 26 years of age.
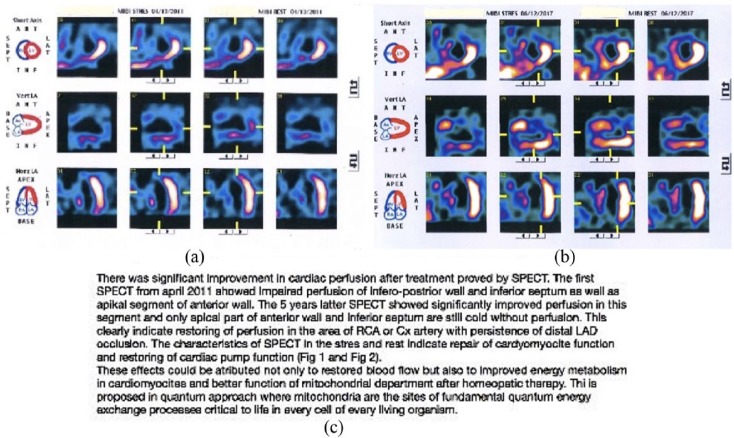
Laboratory investigations: myocardial perfusion single-photon emission computed tomography (SPECT) 13 April 2011 (Figure 1(a)). Report of radiologist: pharmacological dipyridamole stress test combined with treadmill exercise low-level 50WmDipy EX: in the beginning, BP 120/80 mmHg; beats per minute (BPM) 70, at peak exertion BPM 115. Enlarged left ventricle with large anterior wall perfusion defect and septum perfusion defect. Echocardiography (25 September 2015); left ventricular end diastolic dimension (LVEDD): 64 mm (norm till 56 mm); left ventricular end systolic dimension (LVESD): 52 mm (norm till 40 mm); left ventricular ejection fraction (LVEF): 38% (norm >60%); end systole (ES): 18% (norm 28.44%); mitral flow – E wave = 0.7; A wave 0.8; mitral regurgitation (MR): 1–2+; tricuspid flow – tricuspid regurgitation (TR) 1+; left atrial dilation; mitral valve incompetent with moderate MR with central flow; left ventricular dilation, remodelling with akinesia of anterior wall, and akinesia of part of the septum; moderately reduced ventricle function; diastolic dysfunction with increased values of left ventricular end diastolic pressure (LVEDP).
Figure 1.
Case 1: changes in myocardial perfusion before and after homeopathic therapy with cardiologist’s opinion (via email): (a) 4 December 2011, (b) 6 December 2017 and (c) cardiologist’s opinion.
Homeopathic intervention: homeopathic therapy was started on 15 January 2015. The remedies were selected based on the principles of classical homeopathy. The case details along with the follow-ups are given in Table 1.
Laboratory investigations at the end of homeopathic treatment: myocardial perfusion SPECT 12 June 2017 (Figure 1(b)): report of radiologist: pharmacological dipyridamole stress test combined with treadmill exercise low-level 50WmDipy EX: in the beginning, BP 120/80 mmHg; BPM 70, on peak exercise BPM 120. Enlarged left ventricle with perfusion defect in the following areas: apical, apical anterior, anterior wall and apical half of septal area. No signs of progress of pathological state.
Echocardiography (31 May 2017): LVEDD 6.1 cm (norm 3.5–6.0 cm); LVESD 4.8 cm (norm 2.1–4.0); LVEF 40%; mitral flow – MR in trace; tricuspid flow normal; left atrial normal dimension; mitral flow – diastolic dysfunction of left ventricle (LV) (E/A = 0.65); MR in trace; LV – enlarged with hypertrophic walls; hypokinesia of septum and anterior wall, LVEF 40%.
Case 2
The patient, a 92 year-old Serbian woman, presented on 22 June 2015 with an acute episode of MI and was hospitalized. There was associated AF with rapid ventricular response, preventing stabilization of her general condition (Table 2).
Table 2.
Case 2 treatment details.
| Date of intervention | Symptoms | Changes in laboratory findings | Remedy | Response | Conventional medicine changes |
|---|---|---|---|---|---|
| 25 Jun 2015 | Acute myocardial infarction 3 days ago; fear of being approached; atrial fibrillation; refused food | 12 lead ECG shows ST segment elevation (orange), in I, aVL and V1–V5 with reciprocal changes (blue) in the inferior leads; anterior wall infarction; increased cardio-specific enzymes; cardiac therapy started – but no stability in 2 days; atrial fibrillation with rapid ventricular response | Arnica 30C | Few minutes after arnica, the monitor showed sinus rhythm; subjectively she is better; no fear when approached; patient was stable the next 2 days (remedy not repeated) | Is on B-blockers, ACE inhibitors, amiodarone intravenous once on 22 Jun 2015 for atrial fibrillation, Cardiopirin Lasix |
| 26 Jun 2015 | Stable condition; sinus rhythm | ECG showed sinus rhythm, a large akinetic area in the front wall, the septum and apex; physician expects an aneurysm | Stable; released from ICU | Amiodarone intravenous once, Lasix tapered down and stopped | |
| 28 Jun 2015 | Atrial fibrillation since previous day | ECG showed atrial fibrillation | Arnica 30C | 5 min after Arnica sinus rhythm appeared; released from hospital next day | Amiodaron, Lasix tapered down |
| 10 Nov 2015 | Repeat of MI; fear on anyone approaching her; but is better generally than during previous attack | No atrial fibrillation during the attack; echocardiography showed: LVEF 15% | Arnica 200C immediately after appearance of symptoms – even before hospitalization | Stabilized; no fear when approached | In the hospital: B-blocker, ACE inhibitor, clopidogrel, enoxaparin, diuretic, isosorbide mononitrate, eventually tapered and stopped |
| 10 Apr 2017 | Generally patient has been well except for an episode of urinary tract infection in 2016 | Echocardiography: remodelling of the left ventricle (LV) with apical aneurysms and akinesia of a part of the septum and a part of the anterior wall. Reduced global systolic function of LV; diastolic dysfunction… Thrombus is not present in apical aneurisms ECG: sinus rhythm |
Stable state | Since June 2016: B-blocker Cardiopirin |
ECG: electrocardiograph; ACE: angiotensin-converting enzyme; ICU: intensive care unit; MI: myocardial infarction; LVEF: left ventricular ejection fraction.
Past medical history: tuberculosis (1951), malaria (1960), total hysterectomy (1980) and traffic accident causing brain concussion (1982). Laboratory investigations and follow-up: electrocardiograph (ECG; 23 June 2015) (Figure 2(a)) showed ST segment elevation, in I, aVL and V1–V5 with reciprocal changes in the inferior leads; anterior wall infarction. AF with rapid ventricular response. The patient was given intravenous amiodarone (anti-arrhythmic).
Figure 2.
Case 2: changes in rhythm and ECG before and after homeopathic therapy: (a) 23 June 2015, (b) 26 June 2015 and (c) 10 April 2017.
Homeopathic intervention: on 25 June 2017, homeopathic therapy was given in the form of a few sips of water dose of Arnica montana 30C. A few minutes later, the cardiac monitor showed a sinus rhythm, confirmed by the ECG on 26 June 2017(Figure 2(b)).
She was moved from the intensive care unit to a hospital room at this point, and homeopathy was not repeated. On 27 June 2015, she went into AF with rapid ventricular response again and was re-admitted to the intensive care unit.
On repetition of Arnica 30C (on 28 June 2015), however, the sinus rhythm appeared within a few minutes, and she was discharged from the hospital the next day. She stabilized and stayed well for six more months after being discharged from the hospital, evidenced by the stability in ECG. On 10 November 2015, she had another MI attack. However, this time there was no AF, and she was stable with immediate administration of Arnica 200C, despite the LVEF being only 15%. She stayed in the intensive care unit for a day. Holter ECG showed a sinus rhythm.
After the last episode, she has stayed well hitherto, and the last investigation performed was on 10 April 2017. The echocardiography (Figure 2(c)) shows a stable cardiac state, despite remodelling of myocardium and reduced left ventricular function. She is not on any anti-arrhythmic drugs.
Case 3
A 68-year-old Indian man with a history of coronary artery disease underwent percutaneous transluminal coronary angioplasty (PTCA) for LAD in 2001, underwent coronary artery bypass grafting in 2009 (Table 3). On 26 November 2016, he started complaining of severe breathlessness and collapsed around 3.30 a.m. at home and was transported to hospital immediately.
Table 3.
Case 3 treatment details.
| Date of intervention | Symptoms | Changes in laboratory findings | Remedy | Response | Conventional medicine changes |
|---|---|---|---|---|---|
| 29 Dec 2016 | Tiredness, easy fatigue, breathlessness with slight effort | Acute ventricular failure; severe LV dysfunction; EF: 16% High-blood pressure |
Calc phos 200C | Fatigue decreased, appetite better, sleep better, put on half a kilo in 2 weeks; BP stable | Deplatt, Ecosprin, Biotor, Starace, Cardivas, Dytor, Aldactone, Glycomet SR, Pantocid, Vibact, Alprax, Levoflex |
| 07 Feb 2017 | Stable general condition | EF: 42.3% | Nil | Deplatt, Ecosprin, Biotor, Cardace, Cardivas, Dytor, Aldactone, Glycomet SR | |
| 12 Mar 2017 | Stable general condition | EF: 33% | Calc phos 200C | Generally well | |
| 18 May 2017 | Stable general condition | EF: 32% | Calc phos 1M | Generally well | Deplatt, Ecosprin, Biotor, Cardace, Cardivas |
| 25 Jun 2017 | Stable general condition | EF: 41% | Nil | Generally well | |
| 02 Aug 2017 | Stable general condition | EF: 54% | Nil | Generally well | Stopped Biotor, Cardivas and ?Glycomet |
| 13 Oct 2017 | Stable general condition | EF: 64.98% Dilated left atrium; concentric left ventricular hypertrophy; good left ventricle; no regional wall motional abnormalities; sclerotic aortic valve; mild mitral regurgitation; diastolic dysfunction grade 2 |
Nil | Generally well. Is able to travel internationally. Walks briskly carrying his luggage without any sign of breathlessness or fatigue | Stopped Deplatt and Ecosprin |
| 12 Apr 2018 | Patient is leading normal routine | EF: 64.68% Dilated left atrium; mild concentric left ventricular hypertrophy; mild regional wall motion abnormalities in inferoseptal and inferior segments with preserved thickness; fair LV systolic function; Grade 1 diastolic dysfunction; normal valves morphology; mild mitral regurgitation; trivial tricuspid regurgitation |
Nil | Generally maintaining stable state | No changes |
LV: left ventricle.
The patient also had hypertension and diabetes mellitus. Laboratory investigations: echocardiography (27 November 2016) (Figure 3(a)): dilated left atrium; dilated left ventricle; severe hypokinesia of entire septum, apex and anterior wall; mild to moderate MR; sclerosed aortic valve; mild tricuspid regurgitation; ejection fraction 24%. Echocardiography was repeated on 27 December 2016 (Figure 3(b)) and found the same findings as above, but the ejection fraction had reduced to 16%.
Figure 3.
Case 3: changes in the cardiac status and ejection fraction before and after homeopathic therapy: (a) 27 November 2016, (b) 27 December 2016, (c) 7 February 2017, (d) 13 October 2017 and (e) 12 April 2018.
Homeopathic intervention: homeopathic therapy was begun on 29 December 2016; one dose of Calcarea phosphorica 200C was given with evidence of improvement in the ejection fraction (Figure 3(c)). The details of the follow-up are given in Table 3.
Most recent laboratory investigation (12 April 2018) (Figure 3(e)): dilated left atrium; mild concentric left ventricular hypertrophy; mild regional wall motion abnormalities in inferoseptal and inferior segments with preserved thickness; fair LV systolic function; grade 1 diastolic dysfunction; normal valves morphology; mild MR; trivial tricuspid regurgitation; ejection fraction 64.68%. The patient is well till date and is carrying on with his daily life with vigour.
Discussion
Although not usually applied in emergency cases and severe pathologies, homeopathy has previously helped repair severe conditions.25 This case series indicates that we may investigate further the possibilities of homeopathy in such cases. The immune system is always trying to achieve balance, and in situations, as described here, there are patients whose energy complex is good enough that the stimulation from homeopathic remedy is employed to the benefit of the patient. However, this outcome is not expected to be the rule. Homeopathy bases its prescription on the symptoms that the individual organism generates as a response to pathology and this response is the only guide that exists for the homeopath.20 Considering the idea of vital force/life principle as explained earlier, the existence of individualistic symptoms presupposes a certain amount of energy present to be applied for the process of cure in the person. If this is not the case, which is quite common in a potentially terminal situation, then there is not much that homeopathy can do. However, when individual symptoms do exist, the recovery is impressive if the rules of homeopathy are followed.
In the first case, attention must be paid to the fact that although the primary target of the treatment was cardiac pathology, the treatment was inclusive of all his other complaints such as panic attacks and indigestion. The remedies were given in a specific sequence according to the most dominant and indicative symptoms of the moment. At all times, attention was paid to make sure that the patient was moving towards a better level of health.24 The opinion of the cardiologist (Figure 1(c)) states that the perfusion of the myocardium had considerably improved, as evidenced by the SPECT reports. The opinion is that such an improvement is not just representative of improved blood flow but that of improved cardiomyocyte metabolism – an essential factor for a healthy heart.26
The parameters for improvement and good response to treatment in homeopathic therapy are measured by the body’s ability to defend itself with an efficient acute inflammation when required. The idea is that as the defence mechanism becomes weaker, the organism loses the ability to put up an efficient acute inflammation and enters a low-grade chronic inflammation eventually triggering the chronic disease that the patient is predisposed to genetically.27,28 The reverse of this occurs during homeopathic therapy and patient begins to have acute inflammatory states as the chronic complaints reduce.29 In this case, as the cardiac status improved, the patient began suffering more in his gastrointestinal tract and as that improved, there appeared suppuration in the lipomas that had stayed as such for many years. This is interpreted with the background of hierarchy of organs systems and pathologies. The reduction in the deeper problem is followed by concentration of the disease/suffering on the lower system and is of a more superficial pathology (Gastro Intestinal Tract (GIT) and skin; acute inflammation).22 Without the support of homeopathic therapy, such a reversal of state has not been recorded. If such results are to be achieved with homeopathy, exact observation and prescription at every change of health status is essential and is a potential limitation in the absence of expertise.
The second case is of AMI with AF and rapid ventricular response in an aged woman with anterior infarction (Figure 2), heralding a bad prognosis.3,4 Nevertheless, in this case, a clear picture of a homeopathic remedy was apparent during the acute attack, which depicted a good prognosis and a very efficient immune system. The dramatic response to a few sips of Arnica shows that the vitality of the organism was preserved. In such cases, homeopathy may be employed for the benefit of the patient with impressive results.24 We see that during her second episode of MI, when Arnica was administered right in the beginning, she was stable and did not have any associated AF. The ejection fraction was still low but she did not have any associated complaints and is able to go about her daily life without any difficulty.
The third case is also an example of a very healthy constitution according to levels of health theory.22 Here, despite such poor functioning of the heart, the symptoms indicating homeopathic remedy were very clear. In addition, the response to single dose of the remedy was dramatic. Within a year, the ejection fraction of the heart increased from 16% to 65% (Figure 3) and has been maintained within normal limits since then. The functioning of the left ventricle was also restored along with the valves returning to near normal, as is evident from the reports. The diastolic dysfunction that was grade 2 has over time reduced to grade 1.
In these cases, the advantage was that of adherence to therapy. Non adherence could become a limitation in severe pathologies if patient is not informed regarding the various responses that may occur during the course of treatment. Certain developments such as return of old complaints and aggravation of peripheral symptoms (which are a part and requisite of homeopathic therapy) must be anticipated before hand and the patient informed duly.21,22,24
Further studies are required to establish the exact possibilities of homeopathic therapy in severe cardiac pathology. These studies must be carried out in hospital setting and strictly adhere to the rules of classical homeopathy to avoid indelible errors. This case series suggests that homeopathy may be investigated for use in cardiac events, both during the acute attack and for its consequences, when scientifically applied, based on its laws.
Conclusion
The three cases in this series provide evidence of positive outcomes for homeopathic therapy. Case-controlled studies can further establish the exact role-played by homeopathic therapy in such severe cardiac conditions. Here, there is a selection bias as the patients were all kin of homeopathic therapists and this may be overcome by conducting a large randomized grouping in the said controlled study.
There are some observations made commonly in classical homeopathic practice such as return of acute inflammatory states while at the same time there is betterment of the chronic complaint that are yet to be borne out by proper experimental evidence despite existence of vast clinical support to this. This series is a starting point on which evidence we may design further studies.
Acknowledgments
The authors acknowledge the help of the patients in consenting to publish their case details. L.T.: data collection; initial draft of manuscript. B.D. and O.M.: data collection. B.J.P.: homeopathic physician – data collection; initial draft of manuscript. S.M.: final editing of manuscript. G.V.: guide and final approval of the paper.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethical approval: Our institution does not require ethical approval for reporting individual cases or case series.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
Informed consent: Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
ORCID iD: Seema Mahesh  https://orcid.org/0000-0002-4765-5595
https://orcid.org/0000-0002-4765-5595
References
- 1. Yeh RW, Sidney S, Chandra M, et al. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med 2010; 362(23): 2155–2165. [DOI] [PubMed] [Google Scholar]
- 2. World Health Organization. Prevention of recurrences of myocardial infarction and stroke study, http://www.who.int/cardiovascular_diseases/en/ (25 October 2017)
- 3. Van de Werf F, Bax J, Betriu A, et al. Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the task force on the management of ST-segment elevation acute myocardial infarction of the European society of cardiology. Eur Heart J 2008; 29(23): 2909–2945. [DOI] [PubMed] [Google Scholar]
- 4. Michniewicz E, Mlodawska E, Lopatowska P, et al. Patients with atrial fibrillation and coronary artery disease – double trouble. Adv Med Sci 2017; 63(1): 30–35. [DOI] [PubMed] [Google Scholar]
- 5. Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet 2003; 361(9351): 13–20. [DOI] [PubMed] [Google Scholar]
- 6. Biesbroek PS, Amier RP, Teunissen PFA, et al. Changes in remote myocardial tissue after acute myocardial infarction and its relation to cardiac remodeling: a CMR T1 mapping study. PLoS ONE 2017; 12(6): e0180115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ruparelia N, Digby JE, Jefferson A, et al. Myocardial infarction causes inflammation and leukocyte recruitment at remote sites in the myocardium and in the renal glomerulus. Inflamm Res 2013; 62(5): 515–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bhatt AS, Ambrosy AP, Velazquez EJ. Adverse remodeling and reverse remodeling after myocardial infarction. Curr Cardiol Rep 2017; 19(8): 71. [DOI] [PubMed] [Google Scholar]
- 9. Westman PC, Lipinski MJ, Luger D, et al. Inflammation as a driver of adverse left ventricular remodeling after acute myocardial infarction. J Am Coll Cardiol 2016; 67(17): 2050–2060. [DOI] [PubMed] [Google Scholar]
- 10. Ji Q, Zhao Y, Yuan A, et al. Deficiency of liver-X-receptor-a reduces glucose uptake and worsens post-myocardial infarction remodeling. Biochem Bioph Res Co 2017; 488: 489–495. [DOI] [PubMed] [Google Scholar]
- 11. Estep JD, Aguilar D. Diabetes and heart failure in the post-myocardial infarction patient. Curr Heart Fail Rep 2006; 3(4): 164–169. [DOI] [PubMed] [Google Scholar]
- 12. Jung M, Ma Y, Iyer RP, et al. IL-10 improves cardiac remodeling after myocardial infarction by stimulating M2 macrophage polarization and fibroblast activation. Basic Res Cardiol 2017; 112(3): 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ju CH, Wang XP, Gao CY, et al. Blockade of KCa3.1 attenuates left ventricular remodeling after experimental myocardial infarction. Cell Physiol Biochem 2015; 36(4): 1305–1315. [DOI] [PubMed] [Google Scholar]
- 14. Ebelt H, Jungblut M, Zhang Y, et al. Cellular cardiomyoplasty: improvement of left ventricular function correlates with the release of cardioactive cytokines. Stem Cells 2006; 25(1): 236–244. [DOI] [PubMed] [Google Scholar]
- 15. Xiong Q, Ye L, Zhang P, et al. Functional consequences of human induced pluripotent stem cell therapy: myocardial ATP turnover rate in the in vivo swine heart with postinfarction remodeling. Circulation 2013; 127(9): 997–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zhang YJ, Yang SH, Li MH, et al. Berberine attenuates adverse left ventricular remodeling and cardiac dysfunction after acute myocardial infarction in rats: role of autophagy. Clin Exp Pharmacol Physiol 2014; 41(12): 995–1002. [DOI] [PubMed] [Google Scholar]
- 17. Pereira BLB, Reis PP, Severino FE, et al. Tomato (Lycopersicon esculentum) or lycopene supplementation attenuates ventricular remodeling after myocardial infarction through different mechanistic pathways. J Nutr Biochem 2017; 46: 117–124. [DOI] [PubMed] [Google Scholar]
- 18. Hrdlicka J, Neckar J, Papousek F, et al. Beneficial effect of continuous normobaric hypoxia on ventricular dilatation in rats with post-infarction heart failure. Physiol Res 2016; 65(5): 867–870. [DOI] [PubMed] [Google Scholar]
- 19. Yamaguchi T, Izumi Y, Nakamura Y, et al. Repeated remote ischemic conditioning attenuates left ventricular remodeling via exosome-mediated intercellular communication on chronic heart failure after myocardial infarction. Int J Cardiol 2015; 178: 239–246. [DOI] [PubMed] [Google Scholar]
- 20. Hahnemann S. Organon of medicine. 6th ed. New Delhi, India: B.Jain Publishers, 1994. [Google Scholar]
- 21. Kent J. Lectures on homoeopathic philosophy. New Delhi: B.Jain Publishers, 2002. [Google Scholar]
- 22. Vithoulkas G, Tiller W. The science of homeopathy. 7th ed. Athens: International Academy of Classical Homeopathy, 2014. [Google Scholar]
- 23. Hahnemann S. Organon der rationellen Heilkunde. 1st ed Dresden: In Der Arnoldischen Buchh, 1810. [Google Scholar]
- 24. Vithoulkas G. Levels of health. Athens: International Academy of Classical Homeopathy, 2017. [Google Scholar]
- 25. Mahesh S, Mallappa M, Vithoulkas G. Gangrene: five case studies of gangrene, preventing amputation through homoeopathic therapy. Indian J Res Homoeopath 2015; 9(2): 114. [Google Scholar]
- 26. Woodcock E, Matkovich S. Cardiomyocytes structure, function and associated pathologies. Int J Biochem Cell Biol 2005; 37(9): 1746–1751. [DOI] [PubMed] [Google Scholar]
- 27. George V, Carlino S. The ‘continuum’ of a unified theory of diseases. Med Sci Monit 2010; 16(2): 15. [PubMed] [Google Scholar]
- 28. Kivellos S, Mahesh S, Vithoulkas G. Assessing human health-correlation of autoimmune diseases with chemically suppressed acute infections of patient’s past medical history. J Autoimmune Dis Rheumatol 2017; 5: 31–38. [Google Scholar]
- 29. Kivellos S, Skifti S, Vithoulkas G. EHMTI-0396 Reappearance of high fever on migraine patients, after individualized homeopathic treatment, is a valuable prognostic factor. J Headache Pain 2014; 15(suppl 1): M7. [Google Scholar]