Abstract
Background:
Acetabular cartilage lesions are a common abnormality found in patients undergoing hip arthroscopic surgery and may cause pain and functional limitations. Several strategies have been developed to treat chondral defects, with no overwhelming success. Recently, BST-CarGel has gained interest as a scaffolding material that can be injected into the microfracture site to stabilize the clot and facilitate cartilage repair.
Purpose:
To perform a retrospective analysis of prospectively collected data to evaluate the safety profile and short-term clinical and radiographic outcomes of patients treated arthroscopically with BST-CarGel for acetabular chondral defects in conjunction with microfracture.
Study Design:
Case series; Level of evidence, 4.
Methods:
A retrospective chart review was performed on all patients who underwent hip arthroscopic surgery by the senior surgeon to identify those who had BST-CarGel applied to their hip from November 2014 to July 2016, and basic demographic information for those patients was obtained. Operative reports and patient charts were reviewed to assess intraoperative and postoperative complications as well as to obtain the details of surgery, including lesion size and treatment method of the labrum (repair vs reconstruction). All patients filled out self-reported questionnaires, including the international Hip Outcome Tool (iHOT), Hip Outcome Score–Activities of Daily Living (HOS-ADL), and Hip Outcome Score–Sports Profile (HOS-SP) at the time of consultation and at 1 year postoperatively, and results were used to assess the clinical outcomes of surgery.
Results:
Thirty-seven patients (37 hips) with a mean age of 36.19 years at the time of the index procedure were evaluated. There were 30 male patients, and 20 procedures were performed on the right hip. The minimum follow-up was 1 year, with a mean follow-up of 12.72 months. There were no major adverse events of deep vein thrombosis, blood vessel or nerve damage, hemarthrosis, arthralgia, or device-related adverse events. Two patients (5.4%) were readmitted because of pain, probably resulting from an inflammatory reaction to BST-CarGel. At 1 year postoperatively, there were statistically significant improvements in the iHOT (40.4 to 59.1; P < .001), HOS-ADL (60.6 to 71.4; P = .02), and HOS-SP (36.9 to 51.6; P = .01) scores. When the patients were subdivided based on the chondral defect size, the iHOT score improved for all chondral defect sizes, and the HOS-SP score improved in patients with medium (2-4 cm2) and very large (>6 cm2) chondral defects. In addition, the iHOT score improved whether the patients had their labrum repaired or reconstructed (P < .001 and P = .02, respectively).
Conclusion:
The arthroscopic treatment of chondral acetabular defects with BST-CarGel demonstrates a satisfactory safety profile, with statistically significant improvement in patient-reported clinical outcome scores, even for those with very large chondral defect sizes.
Keywords: arthroscopic surgery, hip, acetabulum, cartilage, clinical outcome, chondral defect
Osteoarthritis of the hip is a disabling condition, which leads to large burdens on patients and society.14 The cause of osteoarthritis is thought to be multifactorial, with genetic, biomechanical, structural, and morphological factors as main contributors.11 Because of the avascular nature of cartilage, a chondral lesion often does not spontaneously heal, and this has been theorized to result in early osteoarthritis.17 Numerous treatments have been proposed for this challenging condition. Microfracture is a standard treatment for small chondral defects, with good results and low complication rates.7,8,19 This procedure results in the attraction of undifferentiated stem cells to chondral defects. These cells are stabilized by a bone marrow clot and differentiate into stable fibrocartilaginous tissue.3 Its indications and efficacy are well established for chondral lesions in the knee.8,19
Success with this technique in treating chondral damage in the knee has led to the application of the same technique in the hip joint with good results. Philippon and colleagues16 assessed 9 patients with full-thickness chondral defects who underwent microfracture via hip arthroscopic surgery. Eight patients had 95% to 100% coverage of the chondral defect as seen during revision second-look arthroscopic surgery of the hip.16 In addition, the study by Karthikeyan and colleagues7 showed that 19 of 20 patients had an average fill of 96% when chondral defects were treated with microfracture. McDonald and colleagues12 showed that professional hockey players who underwent microfracture for Outerbridge grade 4 chondral lesions were able to return to competitive games without a statistically significant decrease in performance when compared with the matched control cohort.
In our clinical practice, we combine microfracture with an injectable chitosan-based medical device as there is evidence of increased cell recruitment, transient vascularization, and subchondral bone remodeling in drilled cartilage defects using chitosan–glycerol phosphate/blood implants.1,4 BST-CarGel (Piramal Life Sciences) is an injectable chitosan-based medical device that is designed to be used in conjunction with the bone marrow stimulation technique. It is composed of the buffer β-glycerophosphate and chitosan, which is in a liquid state at room temperature. It is mixed with the patient’s untreated whole blood and delivered to a surgically prepared cartilage lesion in which microfracture has already been performed. The BST-CarGel and blood mixture then solidifies in the cartilage defect, forming a 3-dimensional scaffold for the repair process by stabilizing the clot in the cartilage lesion via adhesion and inhibition of clot retraction. The resulting gel implant facilitates the body’s own healing response, potentially by enhancing the residency of wound-healing factors found in the blood along with bone marrow–derived cells.1,4,5 The safety and efficacy of BST-CarGel in treating chondral lesions of the femoral condyles have been shown in a randomized controlled trial by Stanish et al.18 However, clinical research on other joints including the hip is limited.
The primary purpose of this study was to assess the safety profile of the hip in patients who underwent arthroscopic microfracture in conjunction with BST-CarGel through a retrospective chart review. The secondary objective was to conduct a retrospective analysis of prospectively collected early clinical outcome data on patients who underwent arthroscopic microfracture in conjunction with BST-CarGel for femoral head chondral defects. The international Hip Outcome Tool (iHOT) and the Hip Outcome Score (HOS) were used for clinical outcome analysis.
Methods
Ethics approval was obtained from the Nova Scotia Health Authority Research Ethics Board. The first application of BST-CarGel for hip lesions at our institution was in November 2014. Therefore, the case log of the senior surgeon (I.H.W.) was reviewed to identify patients who had BST-CarGel applied to their hip from November 2014 to July 2016, which was about a year before the date of the chart review to allow for up to 1 year of clinical follow-up.
All patients who underwent hip arthroscopic surgery by the senior surgeon, after providing informed consent, filled out a self-reported questionnaire, which included the iHOT and HOS, at their preoperative and 1-year postoperative follow-up visits. The HOS was further divided into the Activities of Daily Living (HOS-ADL) and Sports Profile (HOS-SP) subsections. All patients underwent magnetic resonance arthrography of their affected hip as a usual preoperative protocol to better characterize the chondral defect and also to identify other hip abnormalities.
The approved use of BST-CarGel at our institution is for a chondral defect larger than 2 cm2. Therefore, if the magnetic resonance arthrogram is consistent with a chondral defect larger than 2 cm2, BST-CarGel is ordered in advance before surgery. If the intraoperative measurement of the chondral defect is less than 2 cm2, then only the bone marrow stimulation procedure via microfracture is performed, without BST-CarGel augmentation. Occasionally, the intraoperative measurement of the chondral defect size is found to be larger than preoperatively anticipated, in which BST-CarGel could not have been ordered in advance. In these cases, the patients are given an option to return to the operating room for revision hip arthroscopic surgery with microfracture and BST-CarGel application.
Surgical Technique
The senior surgeon followed a similar surgical technique to that reported by Tey et al.21 In short, hip arthroscopic surgery was performed with the patient placed in a lateral position on the traction table. The standard anterolateral portal was used as a viewing portal, while the distal midanterior portal was used as a working portal. A curette and motorized shaver were used to remove delaminated cartilage. Once a stable and well-defined margin of healthy cartilage was seen, the calcified layer was removed to expose the subchondral bone. Microfracture was performed using a 60° arthroscopic awl with a depth of 2 to 3 mm and length of 5 mm until the entire defect was covered. Acetabuloplasty was performed to treat the labral lesion, and suture anchors (2.3-mm Osteoraptor; Smith & Nephew) were used to refix the labrum if the labrum was repairable (Figure 1). The labrum was reconstructed using a gracilis allograft and only when found irreparable.9 Once traction was released, cam lesions were addressed by horizontal capsulotomy or T-capsulotomy (if required) mainly through a distal-lateral portal.
Figure 1.
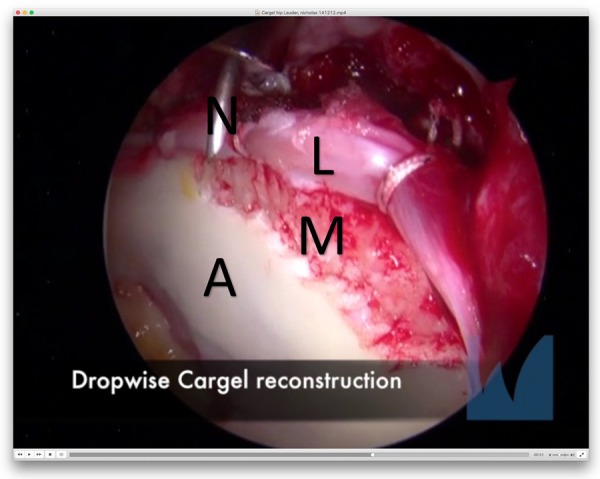
Labral repair before CarGel insertion. A, acetabulum; L, labral repair; M, microfracture; N, needle.
BST-CarGel was prepared according to the manufacturer’s instructions with 4.5 mL of autologous venous blood. Traction was reapplied, and neural strips were used to dry the joint. A large bent spinal needle was used to deliver the BST-CarGel mixture to treat the defect. The implant was left in place for 10 minutes, and then traction was released (Figure 2 and Supplemental Video). After placement of the implant, no fluid was reinfused into the hip joint.
Figure 2.
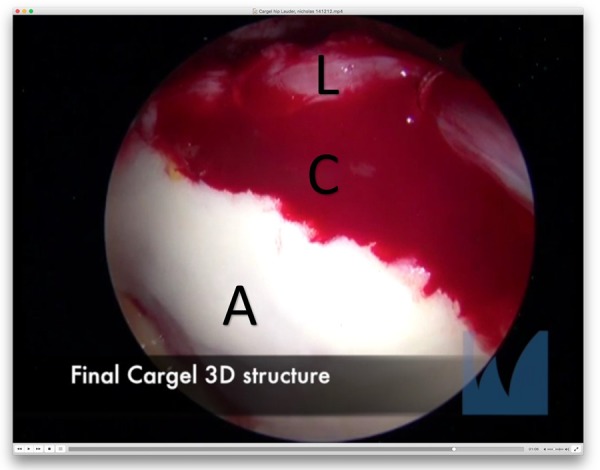
Labral repair after CarGel insertion (final view). 3D, 3-dimensional; A, acetabulum; C, CarGel; L, labral repair.
Postoperative Rehabilitation Protocol
Patients were instructed to practice weightbearing according to the following schedule: 20% weightbearing for 7 weeks, continuing to optimize the gait pattern with crutches; 50% weightbearing at week 8; 75% weightbearing at week 9; and full weightbearing at week 10.
Range of motion was maintained according to the following schedule:
0-2 weeks: hip flexion to 90° and side-lying hip extension.
>2-6 weeks: passive range of motion with flexion (full as tolerated), extension (minimum 15° is crucial), internal rotation, gentle external rotation, circumduction, and abduction.
>6-12 weeks: restoration of full hip joint mobility (all movements; combined movements of flexion, adduction, and internal rotation; and flexion, abduction, and external rotation), distraction techniques with a belt (mobilization with movement) as required, soft tissue release/massage therapy to antagonistic muscle(s), fascial release, scar adhesion, and mobilization of the lumbar spine and pelvis if needed.
>12 weeks: continuation of previous stretching exercises as needed.
Statistical Analysis
A chart review was performed on all the included patients. Basic demographic information such as sex, age at the time of surgery, and body mass index was obtained. In addition, any adverse events were recorded from the follow-up clinic visits and emergency department visits postoperatively. Operative reports were reviewed to obtain the lesion size based on the intraoperative measurement and whether the labral tear was repaired or reconstructed. These intraoperative variables were used to stratify the study population to allow subgroup analysis. All statistical analyses were performed with SPSS Statistics version 24 (IBM), and a paired t test was used to compare the preoperative and postoperative patient-reported clinical outcome scores. A P value of <.05 was used to determine statistical significance.
Results
There were 37 hips (37 patients) that involved the application of BST-CarGel. The mean age of the patients was 36.19 ± 8.19 years, and the mean body mass index was 27.11 ± 3.93 kg/m2. Thirty procedures (81.1%) were performed on male patients, and 20 procedures (54.1%) were performed on the right hip (Table 1).
TABLE 1.
Demographic Characteristics of Patientsa
| Sex, n (%) | |
| Male | 30 (81.1) |
| Female | 7 (18.9) |
| Side, n (%) | |
| Right | 20 (54.1) |
| Left | 17 (45.9) |
| Labral repair, n (%) | 22 (59.5) |
| Labral reconstruction, n (%) | 15 (40.5) |
| Cam lesion, n (%) | 17 (45.9) |
| Age at surgery, y | 36.19 ± 8.19 |
| Body mass index, kg/m2 | 27.11 ± 3.93 |
| Duration of follow-up, mo | 12.72 ± 7.25 |
aValues are presented as mean ± SD unless otherwise indicated.
No major adverse events of deep vein thrombosis, blood vessel or nerve damage, hemarthrosis, arthralgia, or device-related adverse events were reported. Two (5.4%) patients underwent repeat surgery because of significant pain within 2 days of their procedure. Combined with significantly elevated inflammatory markers (C-reactive protein >200 mg/L), both patients were taken to the operating room for urgent irrigation and debridement. However, neither the intraoperative findings nor cultures were consistent with an infection, and antibiotics were discontinued for both patients after the final culture came back negative. Their postoperative courses were unremarkable afterward.
There was a statistically significant improvement in all patient-reported outcome scores at 1 year postoperatively compared with the preoperative values. The preoperative iHOT score improved significantly at the 1-year postoperative time point (P < .001). The HOS-ADL and HOS-SP scores also improved significantly (P = .02 and P < .01, respectively) (Table 2).
TABLE 2.
Clinical Outcome Scores Measured Preoperatively and Postoperativelya
| Outcome Measure | Preoperative | Postoperative | Differenceb | P |
|---|---|---|---|---|
| iHOT | 40.4 ± 19.7 | 59.1 ± 26.1 | 18.7 ± 4.7 | <.001 |
| HOS-ADL | 60.6 ± 19.4 | 71.4 ± 22.9 | 10.8 ± 3.2 | .02 |
| HOS-SP | 36.9 ± 24.9 | 51.6 ± 31.0 | 14.7 ± 4.1 | .01 |
aValues are presented as mean ± SD unless otherwise indicated. HOS-ADL, Hip Outcome Score–Activities of Daily Living; HOS-SP, Hip Outcome Score–Sports Profile; iHOT, international Hip Outcome Tool.
bValues are presented as mean ± standard error.
The mean chondral defect size based on the intraoperative measurement was 5.8 ± 2.6 cm2. The study population was divided into 3 subgroups based on the chondral defect size: medium (2-4 cm2), large (4-6 cm2), and very large (>6 cm2). The iHOT score showed a statistically significant improvement in all 3 subgroups. The HOS-SP score also showed a statistically significant improvement in the groups with medium and very large chondral defects (Tables 3 -5).
TABLE 3.
Preoperative and Postoperative Clinical Outcome Scores in Patients With Medium Chondral Defects (2-4 cm2)a
| Outcome Measure | Preoperative | Postoperative | Differenceb | P |
|---|---|---|---|---|
| iHOT | 40.6 ± 16.2 | 65.2 ± 25.3 | 24.6 ± 6.4 | <.001 |
| HOS-ADL | 65.7 ± 20.9 | 77.2 ± 21.1 | 11.4 ± 6.1 | .04 |
| HOS-SP | 38.6 ± 29.2 | 60.3 ± 35.5 | 21.7 ± 9.7 | .02 |
aValues are presented as mean ± SD unless otherwise indicated. HOS-ADL, Hip Outcome Score–Activities of Daily Living; HOS-SP, Hip Outcome Score–Sports Profile; iHOT, international Hip Outcome Tool.
bValues are presented as mean ± standard error.
TABLE 4.
Preoperative and Postoperative Clinical Outcome Scores in Patients With Large Chondral Defects (4-6 cm2)a
| Outcome Measure | Preoperative | Postoperative | Differenceb | P |
|---|---|---|---|---|
| iHOT | 45.1 ± 23.2 | 60.3 ± 28.3 | 15.2 ± 7.6 | .03 |
| HOS-ADL | 67.2 ± 21.8 | 75.5 ± 19.1 | 8.3 ± 6.7 | .13 |
| HOS-SP | 44.0 ± 26.0 | 45.5 ± 34.3 | 1.5 ± 6.7 | .41 |
aValues are presented as mean ± SD unless otherwise indicated. HOS-ADL, Hip Outcome Score–Activities of Daily Living; HOS-SP, Hip Outcome Score–Sports Profile; iHOT, international Hip Outcome Tool.
bValues are presented as mean ± standard error.
TABLE 5.
Preoperative and Postoperative Clinical Outcome Scores in Patients With Very Large Chondral Defects (>6 cm2)a
| Outcome Measure | Preoperative | Postoperative | Differenceb | P |
|---|---|---|---|---|
| iHOT | 36.9 ± 20.6 | 51.6 ± 26.5 | 14.7 ± 8.7 | .05 |
| HOS-ADL | 51.8 ± 11.5 | 58.1 ± 25.4 | 6.3 ± 8.2 | .23 |
| HOS-SP | 26.6 ± 17.1 | 43.9 ± 25.7 | 17.3 ± 8.9 | .04 |
aValues are presented as mean ± SD unless otherwise indicated. HOS-ADL, Hip Outcome Score–Activities of Daily Living; HOS-SP, Hip Outcome Score–Sports Profile; iHOT, international Hip Outcome Tool.
bValues are presented as mean ± standard error.
The study population was also divided and compared based on the method of surgical management of the labral lesion, which was either repaired or reconstructed based on the viability of the torn labrum. The outcome scores were generally lower in the reconstruction group, but statistically significant improvements in some clinical outcome scores were observed in both groups. The iHOT score showed a statistically significant improvement in both the repair and reconstruction groups (P < .001 and P = .02, respectively). In addition, the repair group showed a statistically significant increase in the HOS-ADL score (P = .05), and the reconstruction group showed an increase in the HOS-SP score (P = .008). The findings are summarized in Tables 6 and 7.
TABLE 6.
Preoperative and Postoperative Clinical Outcome Scores in Patients Who Underwent Labral Repaira
| Outcome Measure | Preoperative | Postoperative | Differenceb | P |
|---|---|---|---|---|
| iHOT | 46.6 ± 20.1 | 68.0 ± 27.3 | 21.4 ± 5.5 | <.001 |
| HOS-ADL | 71.5 ± 19.4 | 82.0 ± 17.3 | 10.6 ± 5.9 | .05 |
| HOS-SP | 45.8 ± 30.0 | 52.1 ± 37.0 | 6.3 ± 7.0 | .19 |
aValues are presented as mean ± SD unless otherwise indicated. HOS-ADL, Hip Outcome Score–Activities of Daily Living; HOS-SP, Hip Outcome Score–Sports Profile; iHOT, international Hip Outcome Tool.
bValues are presented as mean ± standard error.
TABLE 7.
Preoperative and Postoperative Clinical Outcome Scores in Patients Who Underwent Labral Reconstructiona
| Outcome Measure | Preoperative | Postoperative | Differenceb | P |
|---|---|---|---|---|
| iHOT | 31.2 ± 14.4 | 47.4 ± 22.0 | 16.2 ± 7.4 | .02 |
| HOS-ADL | 49.3 ± 9.4 | 55.8 ± 21.3 | 6.5 ± 6.4 | .16 |
| HOS-SP | 26.5 ± 14.9 | 45.3 ± 24.0 | 18.8 ± 6.8 | .008 |
aValues are presented as mean ± SD unless otherwise indicated. HOS-ADL, Hip Outcome Score–Activities of Daily Living; HOS-SP, Hip Outcome Score–Sports Profile; iHOT, international Hip Outcome Tool.
bValues are presented as mean ± standard error.
Discussion
Our study examined the safety profile as well as short-term clinical outcomes of BST-CarGel in treating chondral lesions of the hip joint. There were 2 (5.4%) patients who underwent irrigation and debridement with a presumed diagnosis of an infection. Both patients presented with significant hip pain within 2 days of surgery, with C-reactive protein levels above 200 mg/L. However, both patients were later found to be noninfected with a negative intraoperative culture and were successfully treated with appropriate analgesics without the use of long-term antibiotics. This was believed to be caused by an exaggerated inflammatory response to BST-CarGel.18 These events led to changes in the postoperative regimen at our institution, including overnight admission, strict use of a cooling device, and around-the-clock use of multimodal oral analgesics during the early postoperative period. There were no more unplanned admissions after these changes in the postoperative regimen.
There was no incidence of deep vein thrombosis, blood vessel or nerve damage, or hemarthrosis in our study. A literature review suggests a variability in complication rates, ranging from 0% to 97%, after cartilage repair in the knee.13,18 Stanish et al18 reported that 97% of the patients who received BST-CarGel treatment of the femoral condyle developed complications of mild to moderate intensity during the postoperative period, including arthralgia (68%), procedural pain (32%), nausea (17%), unanticipated device-related adverse events (12%), and anticipated device-related adverse events (10%). Severe adverse effects, including procedure-related and device-related events, were found in 12% of patients, and 1 patient developed pulmonary embolism, deep vein thrombosis, and pleurisy.18 A systematic analysis conducted by Mithoefer et al13 involving 28 studies and 5276 participants who underwent microfracture for knee cartilage repair reported complication rates of 0% to 13%, including procedure-related complications. Our results showed a better safety profile in treating hip cartilage defects with BST-CarGel than was seen in the knee. The safety profile of BST-CarGel in our series is similar to that seen for isolated microfracture of the knee.
We demonstrated that there is a statistically significant improvement in iHOT, HOS-ADL, and HOS-SP scores at short-term follow-up (1 year). The minimal clinically important differences for iHOT, HOS-ADL, and HOS-SP scores are 6, 9, and 6 points, respectively. Therefore, the improvement of all 3 scores observed in our study is not only statistically but also clinically significant, with mean increases of 18.7, 10.8, and 14.7 for the iHOT, HOS-ADL, and HOS-SP, respectively. These promising clinical outcomes in our study are also supported by other studies using BST-CarGel for the treatment of knee and hip chondral lesions.2,3,10,18 Tahoun et al20 reported a significant increase in the HOS-ADL score by 23 points (P < .001) and the HOS-SP score by 40 points (P < .001) for 13 patients who received BST-CarGel treatment for chondral lesions. Stanish et al18 also reported a significant improvement in the Western Ontario and McMaster Universities Osteoarthritis Index score in 41 patients who underwent BST-CarGel with microfracture for knee chondral defects.
Moreover, we observed a significant improvement in patient-reported outcome scores irrespective of the chondral defect size (see Tables 3-5). Even the patients with a very large lesion size (>6 cm2) showed significant improvements in the iHOT (P = .05) and HOS-SP (P = .04) scores. The treatment of large chondral lesions (4-6 cm2) has been a challenging task, as reported in several previous studies.6,19,22 Both studies by Jannelli and Fontana6 and Yen and Kocher22 suggested microfracture as a suitable treatment option only for small chondral defects of less than 2 cm2. The study by Steadman et al19 reported better efficacy of microfracture when treating small chondral lesions of less than 4 cm2 compared with lesion sizes greater than 4 cm2. This trend is also shown in the study by Fontana and de Girolamo,2 in which 77 patients underwent microfracture for femoroacetabular impingement–induced chondral lesions. Unsatisfactory results of microfracture for large chondral lesions have led to trials with more invasive and resource-intensive procedures, including mosaicplasty and autologous membrane–induced chondrogenesis.2,6 Our study suggests BST-CarGel as a potentially effective tool in treating large chondral defects in the hip.
There was both a statistically and a clinically significant improvement in iHOT (16.2; P = .02) and HOS-SP (18.8; P = .008) scores for the patients who underwent labral reconstruction. The reconstruction group in our study represents patients with more chronic problems and a worse clinical status, as shown by the lower mean preoperative clinical outcome scores. Philippon et al15 reported that the outcomes of patients who underwent labral debridement or reconstruction were inferior to those of patients who underwent labral repair. However, our results demonstrate that microfracture in conjunction with BST-CarGel is effective for patients with chronic chondral defects and worse preoperative clinical outcome scores.
The main limitation of this study is the lack of a control group (no group with only microfracture or no treatment of the chondral lesion), so the added benefit of BST-CarGel over microfracture and femoroacetabular impingement treatment alone is still unclear. In addition, the safety profile was examined via a retrospective chart review, which likely underestimated the postoperative complications. The follow-up duration was relatively short at 1 year, and therefore, the long-term effects of BST-CarGel for the treatment of chondral defects in the hip joint are still unknown. A well-designed randomized controlled trial comparing BST-CarGel and other conventional treatments with a long-term follow-up is the next step to demonstrate any advantage of BST-CarGel over isolated microfracture.
In conclusion, our study showed a satisfactory safety profile for the use of BST-CarGel in treating patients with hip chondral defects, irrespective of the defect size, at 1-year short-term follow-up. Early clinical outcomes in this difficult patient population (young patients with large chondral defects) are promising. Longer follow-ups and randomized clinical trials are needed to adequately evaluate the role of this technique.
Supplementary Material
Acknowledgment
The authors acknowledge the help of Swagata Ghosh in conducting statistical analyses and overall formatting, Ryland Murphy for data collection and management, and Jalisa den Hartog for coordinating research and work with the research ethics board.
Footnotes
A Video Supplement for this article is available at http://journals.sagepub.com/doi/suppl/10.1177/2325967118789871.
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
Ethical approval for this study was obtained from the Nova Scotia Health Authority Research Ethics Board.
References
- 1. Chevrier A, Hoemann CD, Sun J, Buschmann MD. Chitosan–glycerol phosphate/blood implants increase cell recruitment, transient vascularization and subchondral bone remodeling in drilled cartilage defects. Osteoarthritis Cartilage. 2007;15(3):316–327. [DOI] [PubMed] [Google Scholar]
- 2. Fontana A, de Girolamo L. Sustained five-year benefit of autologous matrix-induced chondrogenesis for femoral acetabular impingement-induced chondral lesions compared with microfracture treatment. Bone Joint J. 2015;97-B(5):628–635. [DOI] [PubMed] [Google Scholar]
- 3. Harris JD, Siston RA, Brophy RH, Lattermann C, Carey JL, Flanigan DC. Failures, re-operations, and complications after autologous chondrocyte implantation: a systematic review. Osteoarthritis Cartilage. 2011;19(7):779–791. [DOI] [PubMed] [Google Scholar]
- 4. Hoemann CD, Hurtig M, Rossomacha E, et al. Chitosan-glycerol phosphate/blood implants improve hyaline cartilage repair in ovine microfracture defects. J Bone Joint Surg Am. 2005;87(12):2671–2686. [DOI] [PubMed] [Google Scholar]
- 5. Hoemann CD, Sun J, McKee MD, et al. Chitosan-glycerol phosphate/blood implants elicit hyaline cartilage repair integrated with porous subchondral bone in microdrilled rabbit defects. Osteoarthritis Cartilage. 2007;15(1):78–89. [DOI] [PubMed] [Google Scholar]
- 6. Jannelli E, Fontana A. Arthroscopic treatment of chondral defects in the hip: AMIC, MACI, microfragmented adipose tissue transplantation (MATT) and other options. SICOT J. 2017;3:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Karthikeyan S, Roberts S, Griffin D. Microfracture for acetabular chondral defects in patients with femoroacetabular impingement: results at second-look arthroscopic surgery. Am J Sports Med. 2012;40(12):2725–2730. [DOI] [PubMed] [Google Scholar]
- 8. Knutsen G, Engebretsen L, Ludvigsen TC, et al. Autologous chondrocyte implantation compared with microfracture in the knee: a randomized trial. J Bone Joint Surg Am. 2004;86-A(3):455–464. [DOI] [PubMed] [Google Scholar]
- 9. MacInnis LE, Al Hussain A, Coady C, Wong IH. Labral gracilis tendon allograft reconstruction and cartilage regeneration scaffold for an uncontained acetabular cartilage defect of the hip. Arthrosc Tech. 2017;6(3):e613–e619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Marquez-Lara A, Mannava S, Howse EA, Stone AV, Stubbs AJ. Arthroscopic management of hip chondral defects: a systematic review of the literature. Arthroscopy. 2016;32(7):1435–1443. [DOI] [PubMed] [Google Scholar]
- 11. McCarthy JC, Noble PC, Schuck MR, Wright J, Lee J. The watershed labral lesion: its relationship to early arthritis of the hip. J Arthroplasty. 2001;16(8 suppl 1):81–87. [DOI] [PubMed] [Google Scholar]
- 12. McDonald JE, Herzog MM, Philippon MJ. Performance outcomes in professional hockey players following arthroscopic treatment of FAI and microfracture of the hip. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):915–919. [DOI] [PubMed] [Google Scholar]
- 13. Mithoefer K, McAdams T, Williams RJ, Kreuz PC, Mandelbaum BR. Clinical efficacy of the microfracture technique for articular cartilage repair in the knee: an evidence-based systematic analysis. Am J Sports Med. 2009;37(10):2053–2063. [DOI] [PubMed] [Google Scholar]
- 14. Nho SJ, Kymes SM, Callaghan JJ, Felson DT. The burden of hip osteoarthritis in the United States: epidemiologic and economic considerations. J Am Acad Orthop Surg. 2013;21(suppl 1):S1–S6. [DOI] [PubMed] [Google Scholar]
- 15. Philippon MJ, Briggs KK, Yen Y-M, Kuppersmith DA. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg Br. 2009;91(1):16–23. [DOI] [PubMed] [Google Scholar]
- 16. Philippon MJ, Schenker ML, Briggs KK, Maxwell RB. Can microfracture produce repair tissue in acetabular chondral defects? Arthroscopy. 2008;24(1):46–50. [DOI] [PubMed] [Google Scholar]
- 17. Schinhan M, Gruber M, Vavken P, et al. Critical-size defect induces unicompartmental osteoarthritis in a stable ovine knee. J Orthop Res. 2012;30(2):214–220. [DOI] [PubMed] [Google Scholar]
- 18. Stanish WD, McCormack R, Forriol F, et al. Novel scaffold-based BST-CarGel treatment results in superior cartilage repair compared with microfracture in a randomized controlled trial. J Bone Joint Surg Am. 2013;95(18):1640–1650. [DOI] [PubMed] [Google Scholar]
- 19. Steadman JR, Briggs KK, Rodrigo JJ, Kocher MS, Gill TJ, Rodkey WG. Outcomes of microfracture for traumatic chondral defects of the knee: average 11-year follow-up. Arthroscopy. 2003;19(5):477–484. [DOI] [PubMed] [Google Scholar]
- 20. Tahoun M, Shehata TA, Ormazabal I, Mas J, Sanz J, Tey Pons M. Results of arthroscopic treatment of chondral delamination in femoroacetabular impingement with bone marrow stimulation and BST-CarGel®. SICOT J. 2017;3:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tey M, Mas J, Pelfort X, Monllau JC. Arthroscopic treatment of hip chondral defects with bone marrow stimulation and BST-CarGel. Arthrosc Tech. 2015;4(1):e29–e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yen Y-M, Kocher MS. Chondral lesions of the hip. Sports Med Arthrosc. 2010;18(2):83–89. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


