Abstract
Background:
Ulnar collateral ligament (UCL) injury of the elbow is a common and debilitating problem seen frequently among elite baseball pitchers. Ultrasound is a useful diagnostic tool in evaluating UCL injuries.
Hypothesis:
Evaluation with stress ultrasound of the elbow to measure the morphology of the UCL and the ulnohumeral joint space gapping is indicative of higher risk of UCL injury among professional baseball pitchers.
Study Design:
Cohort study; Level of evidence, 2.
Methods:
Ultrasound imaging was used to assess the medial joint laxity of the elbow of 70 asymptomatic professional baseball pitchers during spring training. Medial joint laxity and UCL morphology were assessed with OsiriX imaging software under 2 conditions—gravity valgus load and 5.5 lb of valgus load per a handheld dynamometer—with the shoulder in the maximal cocking position and the elbow in 90° of flexion. Two trials of resting position, elbow gapping, and UCL thickness were collected, measured, and averaged for data analysis. Intra- and interrater reliabilities were established and maintained, with intraclass correlation coefficients in the acceptable range for all measures (0.84-0.99). One-way analysis of variance was used to compare dominant variables between those pitchers who sustained a subsequent UCL injury and those who did not. A receiver operating curve was used to identify pitchers who, based on elbow gapping measures (by cut score), were at high risk versus low risk for UCL injury.
Results:
Players who went on to injure the UCL (n = 7) displayed a significantly wider opening under 5.5 lb of applied stress (6.5 ± 1.2 vs 5.3 ± 1.2 mm, P = .01) when compared with pitchers without UCL injury history (n = 63); they also presented a trend toward wider dominant arm resting joint opening (4.9 ± 1.2 vs 4.0 ± 1.1 mm, P = .07). Professional pitchers with valgus stress ulnohumeral joint gapping ≥5.6 mm (area underneath the curve, 0.77; P = .02) of the dominant arm were at a 6-times greater risk of sustaining a UCL tear requiring reconstruction within a season.
Conclusion:
Our data suggest that ultrasound evaluation of UCL morphology may be indicative of pitchers who are at risk of sustaining UCL injury and that it may improve player assessment.
Keywords: UCL, morphology, injury risk, ultrasound, baseball
Pitchers are known to exert large valgus force across the elbow. The primary soft tissue stabilizer to valgus stress across the elbow is the ulnar collateral ligament (UCL), specifically the anterior band.1,2 Previous studies showed that the highest valgus torque moment occurs during the late cocking phase of throwing, where the elbow is close to 90° of flexion.13,20 As such, there is interest in evaluating the UCL in the anatomic position in which it is maximally stressed during the pitching motion. The current diagnosis of UCL injury relies on history and physical examination, as well as static imaging modalities.
Traditionally, imaging workup for possible UCL injury includes plain radiographs, stress radiographs, and magnetic resonance imaging (MRI).2,6,9,21 MRI has become the imaging modality of choice for the evaluation of the high-level pitcher. It provides excellent visualization of the UCL; however, it may be less effective for partial-thickness tears.4,14,16,23 Magnetic resonance arthrography has been proposed as a more precise and accurate modality, but it comes with the downside of expense, inconvenience, and the potential for false-positive results.10,16,19,23 An additional shortcoming with all the aforementioned imaging modalities is that they are static examinations and do not provide a dynamic assessment of ligament laxity and injury.8
Stress ultrasound has gained momentum in the evaluation of UCL injuries with assessment of joint space gapping under stress.17–19,22 Cadaveric studies have shown the ability of dynamic ultrasound to evaluate the UCL effectively, with reproducible results.19 Studies evaluating diagnostic effectiveness in populations of Major League Baseball pitchers have demonstrated it to be a low-cost, efficient, and noninvasive modality for UCL evaluation.19,22 Previous studies have also indicated morphologic changes with stress ultrasound, such as increased joint gapping, hypoechoic foci, and calcifications, in the elite pitching population.19,22 Other studies attempting to determine the future risk of UCL injury in the elite pitching population have failed to demonstrate a significant link between UCL gapping and subsequent risk of injury to the UCL.8,19 The purpose of this study was to utilize stress ultrasound of the elbow in a professional pitching population to measure the morphology of the UCL and the ulnohumeral joint space gapping to determine if it can serve as a risk factor for future UCL injury.
Methods
Study Population
Seventy asymptomatic professional pitchers during spring training of a Major League Baseball organization were included in this study. All pitchers were asymptomatic and participating fully in spring training activities at the time of assessment. No pitcher had any current shoulder or elbow pain complaints, nor was there a history of elbow surgery or documented UCL injury. Any pitcher that was released prior to the beginning of the regular season was excluded from the final cohort. Demographics were recorded, including age, hand dominance, and injury history.
Assessment
All pitchers underwent dynamic ultrasound of their dominant and nondominant arms. Patients were imaged lying in the supine position with 90° of shoulder abduction, with a towel roll between the upper arm and the examination table. The distal humerus was held as a fulcrum by the examiner placing the stress while another examiner controlled the ultrasound transducer. A handheld dynamometer was placed at the ulnar styloid on all participants (Figure 1). Two separate trials were recorded on each extremity within each test participant.
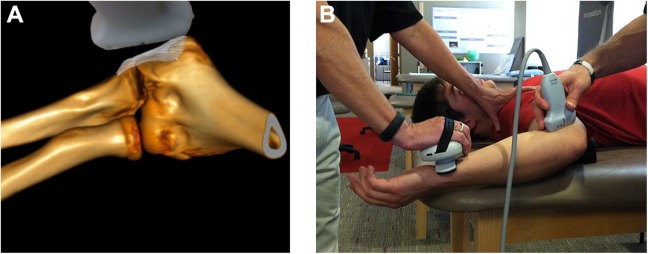
Figure 1.
Medial ulnohumeral joint distance and ulnar collateral ligament thickness imaging. (A) Graphic displaying the ultrasound placement to obtain the medial ulnohumeral joint distance and ulnar collateral ligament thickness. (B) The shoulder is positioned within the coronal plane with a towel roll placed under the distal humerus while the moving valgus stress is applied via a handheld dynamometer at a standard load of 2.5 kg (5.5 lb).
Ulnohumeral joint opening distance and UCL thickness were measured with ultrasonography using a 5-MHz linear array transducer with standard transducer gel to capture images of the dominant throwing elbows. The elbow was assessed statically at 90° of flexion and within the moving valgus stress test arc, where maximal joint distance was observed on the real-time ultrasound image under 2 loading conditions: (1) valgus gravity stress recorded as resting joint opening and (2) 2.5 kg (5.5 lb) of valgus load with a handheld dynamometer with digital readout recorded as stressed joint opening (microFET-2; Hoggan Scientific LLC).
With sagittal ultrasound images, ulnohumeral joint distances and UCL thickness were measured in both stressed conditions. Ulnohumeral joint distance measures were defined by a straight-line method between the peaks of the humeral trochlea and ulnar coronoid process at the joint line. UCL thickness was measured from the peak of the humeral trochlea to the most superficial border of the UCL with a straight-line method (Figure 2). All measurements were documented by 2 blinded sports medicine fellowship–trained physicians (B.K.M., M.J.K.) with the OsiriX platform (Pixmeo SARL) on identical computing devices. Intrarater reliability was established by calculating intraclass correlation coefficients and standard error of the measure for each testing parameter (Table 1). Univariate analyses of variance were used to compare the ulnohumeral joint opening and UCL thickness between noninjured and UCL-injured athletes. Receiver operating characteristic (ROC) curves were used to determine the utility of the moving valgus stress test in discriminating between athletes who were at high and low risk for the development of UCL injury in the subsequent season. A χ2 analysis was performed to calculate odds ratios with confidence intervals for all significant ROC curve analyses.
Figure 2.
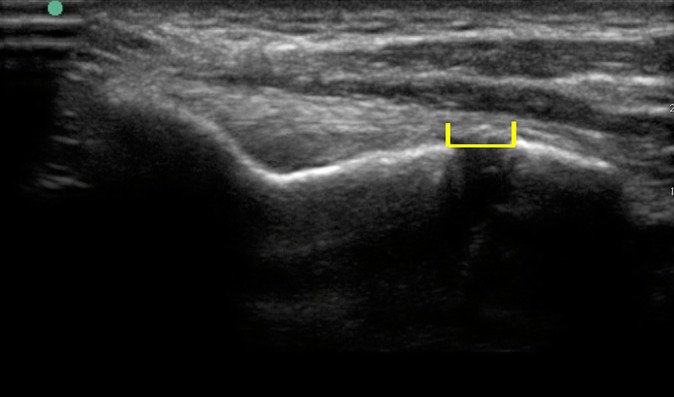
Landmarks for measurement of resting and stressed joint space opening are the superior portion (crest) of the humeral and ulnar joint lines. Measurement from the humeral side of the joint. Each set of participant images began by measuring the resting image twice prior to measuring the stressed image (also twice).
TABLE 1.
Demographics of Pitchers by Injury Statusa
| Entire Cohort | Subsequent UCL injury | P Value | ||
|---|---|---|---|---|
| Yes | No | |||
| Pitchers, n | 70 | 7 | 63 | |
| Age, y | 23.3 ± 2.3 | 21.7 ± 1.5 | 23.4 ± 2.3 | .06 |
| Height, cm | 181.0 ± 29.8 | 171.0 ± 42.9 | 182.2 ± 28.3 | .35 |
| Weight, kg | 89.8 ± 8.2 | 92.0 ± 8.8 | 89.6 ± 8.1 | .45 |
| Dominant arm: right, % | 83 | 100 | 80 | .23 |
| Starting pitcher, % | 45 | 43 | 45 | .92 |
| Games pitched | 26 ± 13 | 14 ± 13 | 28 ± 13 | .009 |
| Innings pitched | 60 ± 41 | 14 ± 14 | 65 ± 40 | .003 |
aValues are presented as mean ± SD unless indicated otherwise. UCL, ulnar collateral ligament.
All statistical analyses were conducted with SPSS Statistics (v 22.0; IBM). Statistical significance was set a priori at P = .05 for all statistical comparisons and for the ROC curve analysis of a minimum area under the curve (AUC) >0.70.
Results
The demographic information for the 70 assessed professional pitchers is listed in Table 1. The mean ± SD age of the cohort was 23 ± 2.3 years. Most pitchers were right-handed (58 right, 12 left). A similar number of starters and relievers were included in the cohort. Seven players (10%) sustained a UCL injury, with a mean time loss of 113 days (range, 45-183 days). All pitchers sustaining a UCL injury within the season were initially treated nonoperatively with rest and rehabilitation, but none were able to return to play. All pitchers diagnosed with a UCL tear opted for surgical treatment on the dominant throwing elbow by the end of the season, after failing initial conservative treatment.
Ultrasound was found to be a reliable and reproducible measure of UCL thickness and gapping (intraclass correlation coefficients, 0.84-0.99). Minimum detectable differences were as follows: thickness, 0.44 mm; gravity gappings, 0.47 mm; and stress gapping, 0.3 mm. This minimum detectable difference was approximately one-third of the measured differences in this study, confirming that our technique was reproducibly measurable. For the entire cohort, the dominant arm demonstrated an increase in UCL thickness (3.4 ± 0.72 mm) as well as an increase in UCL gapping at both gravity (4.1 ± 1.3 mm) and stress (5.5 ± 1.2 mm) gapping.
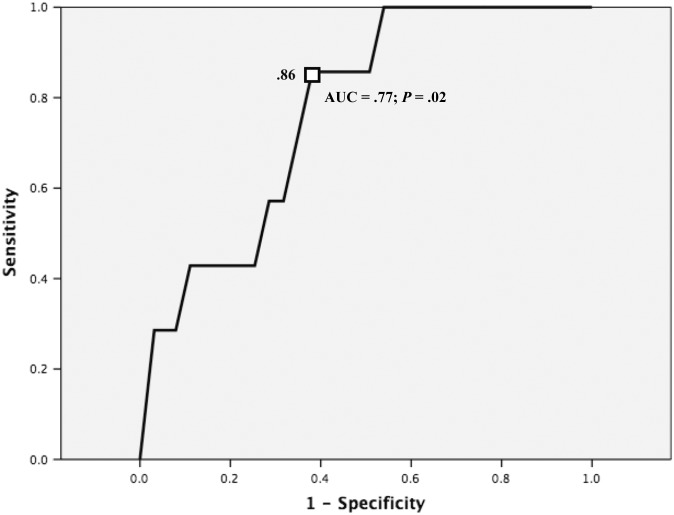
Differences in gapping of the dominant and nondominant arms between those who sustained a UCL injury and those who remained healthy are included in Table 2. No differences in gapping or morphology of the UCL were noted in the nondominant arm of any thrower. Dominant arm UCL thickness and gapping under gravity were larger in subsequently injured players, but this did not reach statistical significance. Players who went on to injure the UCL during the following season (n = 7) did demonstrate a statistically significant increase in gapping of the dominant ulnohumeral joint under load as compared with those who did not sustain a subsequent UCL injury (6.5 vs 5.3 mm, P = .01). Specifically, professional pitchers with valgus ulnohumeral joint gapping ≥5.6 mm (AUC = 0.77, P = .02) (Figure 3) of the dominant arm were at 6-times greater risk of sustaining a UCL tear requiring reconstruction than were those below this threshold.
TABLE 2.
Comparisons Between Injured and Noninjured Pitchers: Elbow Gapping and UCL Propertiesa
| Dominant Arm | Nondominant Arm | ||||||
|---|---|---|---|---|---|---|---|
| n | Mean | SD | P Value | Mean | SD | P Value | |
| Resting joint opening, mm | |||||||
| Injured | 7 | 4.9 | 1.2 | .07 | 4.0 | 0.77 | .18 |
| Noninjured | 63 | 4.0 | 1.1 | 3.6 | 0.85 | ||
| Stressed joint opening, mm | |||||||
| Injured | 7 | 6.5 | 1.2 | .01 | 5.1 | 0.72 | .09 |
| Noninjured | 63 | 5.3 | 1.2 | 4.6 | 0.84 | ||
| UCL thickness, mm | |||||||
| Injured | 7 | 3.5 | 0.59 | .67 | 2.4 | 0.62 | .3 |
| Noninjured | 63 | 3.4 | 0.63 | 2.7 | 0.55 | ||
aValues are presented in millimeters unless indicated otherwise. UCL, ulnar collateral ligament.
Figure 3.
Receiver operating curve: dominant arm valgus loaded ulnohumeral opening.
Discussion
This study suggests that changes present in the UCL detectable on screening ultrasound may identify pitchers who are at higher risk for subsequent UCL injury. Specifically, professional pitchers who subsequently required UCL reconstruction had a wider gapped opening than that of their counterparts not requiring UCL reconstruction.
Overhand athletes exert large force throughout the medial elbow joint during the throwing motion. Fleisig et al13 showed that the highest valgus moment force occurs during the late cocking phase of throwing, where the elbow is close to 90° of flexion. At this moment, the amount of force to the medial aspect of the elbow can exceed 64 N·m and the tensile strength of the native ligament. This large distractive force can cause acute or chronic injuries to the anterior band of the UCL.
Injuries to the UCL were first described by Waris24 in 1946 in a study of javelin throwers. Over time, the injury to the UCL has gained attention in the medical literature and public press with regard to the professional baseball pitcher. An injury to the UCL was career ending for a professional baseball pitcher until the 1970s, when Dr Jobe popularized surgical reconstruction of the UCL. This landmark procedure has drastically improved careers and return to play in the professional pitching population; however, the recovery from a UCL reconstruction can take as long as 12 to 18 months.3,5,12,15 Prevention of this injury has received recent increased attention, with emphasis on proper throwing mechanics, core strength, and adequate rest, especially in younger populations.
Wright et al25 used plain radiographs for 56 asymptomatic professional baseball pitchers and found degenerative changes over time; however, these changes did not correlate with future injury. Another drawback to plain radiographs is the limited information about the structural integrity of the UCL or associated soft tissue structures. More recently, MRI has been the imaging modality of choice, and it provides enhanced visualization of the UCL and surrounding structures.14,16,23 The drawbacks of MRI studies, however, are that they do not provide a functional or dynamic assessment of the UCL and that the MRI is significantly more expensive than ultrasound imaging.
Ultrasound of the elbow is a fast, inexpensive, repeatable, and noninvasive tool that is effective at diagnosing partial- and full-thickness tears of the UCL.8,11,17,19 In a study of 30 collegiate baseball players, Sasaki et al22 showed that stress ultrasound can detect increased laxity and wider ulnohumeral joint space in the dominant throwing elbow as compared with the contralateral side at 90° of elbow flexion. Their testing protocol was similar to that of the present study in testing the elbow at 90° of flexion.
In the current study, we noted baseline anatomic changes within the dominant elbow of the professional baseball pitcher. We were also able to detect a significant difference in the magnitude of ulnohumeral gapping of the UCL among pitchers who eventually had a UCL injury. This study is the first, to our knowledge, to produce a modality that can indicate higher risk of future UCL injuries.
Ciccotti et al8 recently published their 10-year results using stress ultrasound in the evaluation of UCL injuries among professional pitchers. They found that the UCL in the dominant elbow of elite pitchers is thicker and more likely to have hypoechoic foci and/or calcifications as well as increased laxity over time. They were unable to find any significant relationship between the presence of these changes and subsequent UCL tearing. This is in contrast to the present study, where there was a significant correlation with stress ultrasound findings and future UCL injury. One potential explanation for the differences between the current study and that of Ciccotti et al8 was that their testing protocol utilized stress examination at 30° of flexion, as opposed to the 90° performed in the present study. Given that the highest valgus stress during the throwing motion occurs at around 90° of flexion in the late cocking stage,1,6,7,9 it may be that this angle allows for a more accurate approximation of stresses seen in live pitching. Outside the aforementioned article by Ciccotti et al,8 this is one of the largest study populations utilizing stress ultrasound among elite pitchers. The relatively high percentage of UCL injuries in the present cohort allowed for sufficient power to demonstrate a difference. In the Ciccotti et al8 study, 3.3% of pitchers in a sample of 368 sustained UCL injuries. Their post hoc analysis revealed that with potentially 17 (4.6%) UCL injuries, their results would have achieved significance.8
This study has several limitations. First, our follow-up was 1 season, and while we did note that 10% of our cohort sustained UCL injuries in this season, longer term follow-up may influence our results. Second, we did not collect pitch counts, pitching level, or pitching position (reliever vs starter) as a component of the study. It may be that our results were confounded by these other factors. Presumably, pitchers at lower levels of competition may attempt to pitch through elbow soreness to try to impress coaches and baseball organization personnel to move up a level of competition, thereby placing themselves more at risk for injury. Pitching position and pitch counts could influence UCL injury, as most relievers pitch with less time off as compared with starting pitchers, who typically pitch after a 4- to 5-day rest period. Further studies accounting for these factors with the use of stress ultrasound have potential benefits. Finally, while our results were significant, our overall injury numbers were low. One should be cautious of any cause-and-effect relationship based on a small cohort of injuries. This study is the first, however, to demonstrate that increased gapping of the dominant arm of professional pitchers leads to a significantly increased risk of subsequent UCL tear, and further study is certainly warranted.
Conclusion
We have shown that stress ultrasound is a potentially helpful tool in estimation of high-injury risk to the UCL in the professional baseball pitcher population. Professional pitchers with valgus stress ulnohumeral joint gapping ≥5.6 mm (AUC = 0.77, P = .02) of the dominant arm were at a 6-times greater risk of suffering a UCL tear requiring reconstruction as compared with those with <5.6 mm of valgus ulnohumeral joint gapping. Further study with longer follow-up and a larger cohort will be necessary to determine if these results hold true in a larger setting.
Acknowledgment
The authors acknowledge the support of the Colorado Rockies organization and medical staff.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: M.S. has received hospitality payments from DePuy Synthes. B.K.M. has received a grant from DePuy Orthopaedics and hospitality payments from DePuy Synthes and Stryker. J.M.T. is a consultant for Arthrex, DePuy Mitek, and Zimmer; has received hospitality payments from Peerless Surgical, DePuy, Arthrex, and Zimmer; has received educational support from Peerless Surgical; is a paid speaker/presenter for Arthrex and Mitek; and receives royalties from Arthrex. M.J.K. is a consultant for Arthrex; has received educational support from Arthrex; has received hospitality payments from Arthrex, Peerless Surgical, and Pacira Pharmaceuticals; and is a paid speaker/presenter for Pacira Pharmaceuticals and Arthrex. T.J.N. is a consultant for Stryker and Histogenics, has received hospitality payments from Stryker, and has received research support from Histogenics.
Ethical approval for this study was obtained from Greenville Health System.
References
- 1. Aguinaldo AL, Chambers H. Correlation of throwing mechanics with elbow valgus load in adult baseball pitchers. Am J Sports Med. 2009;37(10):2043–2048. [DOI] [PubMed] [Google Scholar]
- 2. Bowerman JW, McDonnell EJ. Radiology of athletic injuries: baseball. Radiology. 1975;116(3):611–615. [DOI] [PubMed] [Google Scholar]
- 3. Bowers AL, Dines JS, Dines DM, Altchek DW. Elbow medial ulnar collateral ligament reconstruction: clinical relevance and the docking technique. J Shoulder Elbow Surg. 2010;19 (suppl 2):110–117. [DOI] [PubMed] [Google Scholar]
- 4. Brunton LM, Anderson MW, Pannunzio ME, Khanna AJ, Chhabra AB. Magnetic resonance imaging of the elbow: update on current techniques and indications. J Hand Surg. 2006;31(6):1001–1011. [DOI] [PubMed] [Google Scholar]
- 5. Cain EL, Jr, Andrews JR, Dugas JR, et al. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: results in 743 athletes with minimum 2-year follow-up. Am J Sports Med. 2010;38(12):2426–2434. [DOI] [PubMed] [Google Scholar]
- 6. Cain EL, Jr, Dugas JR, Wolf RS, Andrews JR. Elbow injuries in throwing athletes: a current concepts review. Am J Sports Med. 2003;31(4):621–635. [DOI] [PubMed] [Google Scholar]
- 7. Chen FS, Rokito AS, Jobe FW. Medial elbow problems in the overhead-throwing athlete. J Am Acad Orthop Surg. 2001;9(2):99–113. [DOI] [PubMed] [Google Scholar]
- 8. Ciccotti MG, Atanda A, Jr, Nazarian LN, Dodson CC, Holmes L, Cohen SB. Stress sonography of the ulnar collateral ligament of the elbow in professional baseball pitchers: a 10-year study. Am J Sports Med. 2014;42(3):544–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ciccotti MG, Jobe FW. Medial collateral ligament instability and ulnar neuritis in the athlete’s elbow. Instr Course Lect. 1999;48:383–391. [PubMed] [Google Scholar]
- 10. Cotten A, Jacobson J, Brossmann J, et al. Collateral ligaments of the elbow: conventional MR imaging and MR arthrography with coronal oblique plane and elbow flexion. Radiology. 1997;204(3):806–812. [DOI] [PubMed] [Google Scholar]
- 11. De Smet AA, Winter TC, Best TM, Bernhardt DT. Dynamic sonography with valgus stress to assess elbow ulnar collateral ligament injury in baseball pitchers. Skeletal Radiol. 2002;31(11):671–676. [DOI] [PubMed] [Google Scholar]
- 12. Dines JS, Jones KJ, Kahlenberg C, Rosenbaum A, Osbahr DC, Altchek DW. Elbow ulnar collateral ligament reconstruction in javelin throwers at a minimum 2-year follow-up. Am J Sports Med. 2012;40(1):148–151. [DOI] [PubMed] [Google Scholar]
- 13. Fleisig GS, Barrentine SW, Escamilla RF, Andrews JR. Biomechanics of overhand throwing with implications for injuries. Sports Med. 1996;21(6):421–437. [DOI] [PubMed] [Google Scholar]
- 14. Fritz RC, Steinbach LS, Tirman PF, Martinez S. MR imaging of the elbow: an update. Radiol Clin North Am. 1997;35(1):117–144. [PubMed] [Google Scholar]
- 15. Hechtman KS, Zvijac JE, Wells ME, Botto-van Bemden A. Long-term results of ulnar collateral ligament reconstruction in throwing athletes based on a hybrid technique. Am J Sports Med. 2011;39(2):342–347. [DOI] [PubMed] [Google Scholar]
- 16. Kaplan LJ, Potter HG. MR imaging of ligament injuries to the elbow. Radiol Clin North Am. 2006;44(4):583–594. [DOI] [PubMed] [Google Scholar]
- 17. Kijowski R, De Smet AA. The role of ultrasound in the evaluation of sports medicine injuries of the upper extremity. Clin Sports Med. 2006;25(3):569–590. [DOI] [PubMed] [Google Scholar]
- 18. Miller TT, Adler RS, Friedman L. Sonography of injury of the ulnar collateral ligament of the elbow-initial experience. Skeletal Radiol. 2004;33(7):386–391. [DOI] [PubMed] [Google Scholar]
- 19. Nazarian LN, McShane JM, Ciccotti MG, O’Kane PL, Harwood MI. Dynamic US of the anterior band of the ulnar collateral ligament of the elbow in asymptomatic major league baseball pitchers. Radiology. 2003;227(1):149–154. [DOI] [PubMed] [Google Scholar]
- 20. Perry J. Anatomy and biomechanics of the shoulder in throwing, swimming, gymnastics, and tennis. Clin Sports Med. 1983;2(2):247–270. [PubMed] [Google Scholar]
- 21. Popovic N, Ferrara MA, Daenen B, Georis P, Lemaire R. Imaging overuse injury of the elbow in professional team handball players: a bilateral comparison using plain films, stress radiography, ultrasound, and magnetic resonance imaging. Int J Sports Med. 2001;22(1):60–67. [DOI] [PubMed] [Google Scholar]
- 22. Sasaki J, Takahara M, Ogino T, Kashiwa H, Ishigaki D, Kanauchi Y. Ultrasonographic assessment of the ulnar collateral ligament and medial elbow laxity in college baseball players. J Bone Joint Surg Am. 2002;84(4):525–531. [DOI] [PubMed] [Google Scholar]
- 23. Schwartz ML, al-Zahrani S, Morwessel RM, Andrews JR. Ulnar collateral ligament injury in the throwing athlete: evaluation with saline-enhanced MR arthrography. Radiology. 1995;197(1):297–299. [DOI] [PubMed] [Google Scholar]
- 24. Waris W. Elbow injuries of javelin-throwers. Acta Chir Scand. 1946;93(6):563–575. [PubMed] [Google Scholar]
- 25. Wright RW, Steger-May K, Klein SE. Radiographic findings in the shoulder and elbow of Major League Baseball pitchers. Am J Sports Med. 2007;35(11):1839–1843. [DOI] [PubMed] [Google Scholar]