Abstract
Background
Dementia is currently incurable, irreversible and a major cause of disability for the world's older population. The association between mental health difficulties, such as post-traumatic stress disorder (PTSD) and major depressive disorder (MDD), and dementia has a long history within the civilian population. Despite the increased importance of this link within the military veteran population, who suffer a greater propensity of mental health difficulties and consist largely of over 65s, attention is only recently being paid to the salience of such an association for this group. This paper aims to explore the relationship between PTSD and MDD with dementia within the military veteran population.
Method
A systematic review was conducted on articles from 1990 to July 2016 on MEDLINE, EMBASE, EBSCO and Web of Science electronic databases with an update conducted in February 2017.
Results
Six empirical studies were identified from the review, the majority of which originated from the USA. Five of the studies asserted that veterans with a diagnosis of either PTSD or MDD are at a significantly greater risk of developing dementia than ‘healthy’ controls. The final study, conducted in Australia, found only a small, but non-significant, correlation between earlier MDD and future dementia, but no concurrent correlation.
Conclusions
While causality cannot be determined, it is likely that PTSD and depressive disorders are related to an increased risk of dementia in military veterans. Potential pathological explanations and risk factors are reviewed and the clinical and neuroscience implications of these findings are explored.
Key words: Dementia, major depressive disorder depression, mental health disorders, military, post-traumatic stress disorder, review, veterans
Introduction
Dementia
Dementia is caused by degeneration of the brain and is characterised by symptoms such as memory loss, language difficulties and reduced problem solving ability (Alzheimer's Society, 2014). Dementia is irreversible and progressive meaning that symptoms continue to worsen throughout the patient's life (Alzheimer's Society, 2014). There are many types of dementia but this paper will focus on the four most common types. These along with the associated neurodegenerative pathways are highlighted in Table 1 below (Alzheimer's Society, 2014; NHS, 2015; British Medical Journal, 2017a, b, c, d):
Table 1.
Neurodegenerative pathways to dementia
| Dementia Label | Biological Pathway |
|---|---|
| Alzheimer's Disease | Deposits of amyloid protein plaques and neurofibrillary tangles; brain atrophy; and neuronal degeneration |
| Vascular Dementia | A stroke or fatty deposits interrupt the blood supply to the brain interfering with the normal functioning; neuronal degeneration |
| Lewy Body Dementia | Deposits of proteins develop inside brain cells impacting neurotransmitters carrying messages between brain cells |
| Frontotemporal Dementia | Temporal and frontal lobe damage, typically caused by a genetic mutation, causing the neuronal degeneration |
Alzheimer's disease is by far the most common form of dementia, estimated to account for up to 70% of dementia cases (World Health Organisation, 2015). According to the Alzheimer's Society (2014) rates of dementia in the UK general population are estimated to be about 850 000, affecting 1 in every 14 people over the age of 65. Age is the biggest risk factor for dementia with the risk doubling every 5 years after the age of 65 (Alzheimer's Society, 2014).
Dementia prevalence is increasing with the number of people living with dementia in the UK estimated to reach over 1 million by 2025, and over 2 million by 2050 (Lewis et al. 2014). This increase comes at both a personal cost to people with dementia and their families and carers, but also a huge economic cost to the UK. The current financial cost of dementia to the UK economy is over £24 billion a year, this is a combination of health and care costs and the vast contribution made by informal carers (Lewis et al. 2014). We also know that people with dementia have a lower self-reported quality of life than both the general population as a whole and those over 65 (Lewis et al. 2014).
Major depressive disorder (MDD), post-traumatic stress disorder (PTSD) and dementia
The relationship between MDD and dementia has been discussed within the civilian literature for many years, according to Mahendra (1985) potentially back to the ninth century AD. A 2006 meta-analyses within the civilian population suggests that for those with a diagnosis of MDD there is an odds ratio (OR) of between 2.03 [95% confidence interval (CI) 1.73–2.38] and 1.90 (95% CI 1.55–2.33) for dementia, depending on whether case control or cohort studies are examined (Ownby et al. 2006). In addition to this, a recent review of the risk factors for dementia identified depression at any age, as well as late life depression, as two of the four core risk factors for dementia along with benzodiazepines use and frequency of social contact (Bellou et al. 2017).
Whilst no comparable review exists exploring the relationship between PTSD and dementia within the civilian literature, empirical evidence is amassing, which stresses the importance of this association across a range of populations. A study of 9/11 survivors found that current PTSD, as well as MDD diagnosis, was associated with a twofold increase in cognitive impairment (Clouston et al. 2016). 12.8% of those screened displayed a level of cognitive impairment with 1.2% diagnosed with dementia, from a participant pool with an average age of only 53 these results are surprisingly high (Clouston et al. 2016). Holocaust survivors with PTSD have been shown to demonstrate accelerated aging compared with both holocaust survivors without PTSD and ‘healthy’ controls (Golier et al. 2002). A study exploring Swiss child labourers with PTSD indicated reduced cognitive function when compared with those without PTSD (Burri et al. 2013).
Potential pathways linking MDD/PTSD and dementia
Butters et al. (2008) and Greenberg et al. (2014) provide concise overviews of the potential pathways between MDD and PTSD (respectively) with dementia. The following section will summarise the complimentary pathways discussed in these reviews, supplemented by evidence from the wider literature. It must be stressed that these are not the only potential pathways, but rather they represent a number of pathways commonly discussed in the literature. It is also worth highlighting that the pathways are not mutually exclusive.
Increased activation of the HPA
MDD, PTSD and dementia are associated with hyperactivity of the hypothalamic–pituitary–adrenal (HPA) axis, and resultant increases in cortisol (Qureshi et al. 2010; Yaffe et al. 2010; Veitch et al. 2013; Weiner et al. 2013; Byers & Yaffe, 2014; Meziab et al. 2014). Increases in cortisol are shown to impact cognitive ability at the time of release as well as lead to cognitive impairment in later life (Meziab et al. 2014) with prolonged exposure to high levels of cortisol resulting in neurodegeneration (Qureshi et al. 2010; Yaffe et al. 2010; Veitch et al. 2013; Weiner et al. 2013; Byers & Yaffe, 2014; Meziab et al. 2014).
Increased cytokines and resultant inflammation
The HPA axis also controls the release of cytokines, proteins that impact certain neurotransmitters in the brain (Passmore, 2015). Increased levels of cytokines, seen in both MDD and PTSD, can cause inflammation, which damages the brain and increases the risk of dementia (Yaffe et al. 2010; Veitch et al. 2013; Byers & Yaffe, 2014).
Increase in amyloid beta (Aβ) plaques
The Aβ plaques are a diagnostic feature of Alzheimer's dementia (Weiner et al. 2013; Byers & Yaffe, 2014). Research indicates that MDD is also associated with an increase in Aβ deposition and that patients with both Alzheimer's dementia and MDD have an increased rate of Aβ deposition than those with Alzheimer's dementia alone (Veitch et al. 2013; Byers & Yaffe, 2014). PTSD has also been proposed to be caused by alterations of hormones, which control the production and deposition of Aβ plaques (Sibener et al. 2014).
Cognitive reserve
The cognitive reserve theory states that PTSD and MDD may diminish cognitive reserve, which may increase the risk, or speed up the process, of dementia (Qureshi et al. 2010; Yaffe et al. 2010; Apfel et al. 2011; Veitch et al. 2013). Higher levels of cognitive reserve, developed via factors such as higher socio-economic status and educational attainment may ‘protect’ an individual from developing dementia (Dent et al. 1998).
Potential unifying hypotheses
Inflammatory neurodegeneration
The theory of inflammatory neurodegeneration is gaining traction as a potential explanation for the impacts of psychiatric conditions such as MDD and PTSD. This theory ties each of the above mechanisms together in a prospective ‘unifying hypothesis’. When the body is exposed to stress it triggers an inflammatory response as a form of protection (Boorman et al. 2015; Franklin et al. 2015). Acute or prolonged stress can lead to increased inflammation and can result in neurodegeneration (Boorman et al. 2015; Franklin et al. 2015). The inflammatory response is controlled by the HPA axis and involves an increase in pro-inflammatory cytokines, which in turn activate microglia (Boorman et al. 2015; Franklin et al. 2015). Among other processes, microglia activation leads to an increase in release of NLRP3 and inhibition of brain-derived neurotrophic factor (BDNF) both of which can result in neurodegeneration (Boorman et al. 2015; Franklin et al. 2015). Dementia is characterised by neurodegeneration and both lower levels of BDNF and higher levels of NLRP3, stimulated by increased levels of Aβ plaques, are found in dementia (Boorman et al. 2015; Franklin et al. 2015). This suggests that such inflammatory markers may represent the mediatory factor between MDD/PTSD and dementia (Boorman et al. 2015; Franklin et al. 2015).
Brain reserve
Butters et al. (2008) describe the theory of brain reserve in relation to dementia. Brain reserve theory is based on the notion that individuals can tolerate more or less cell loss before clinical symptoms are observed, based on their level of cell redundancy. Indeed a meta-analysis by Valenzuela & Sachdev (2006) found that higher levels of brain reserve were associated with a lower risk of dementia, OR 0.54 (CI 0.49–0.59). Butters et al. (2008) suggest that such a hypothesis may also act as a ‘unifying hypothesis’ for each of the mechanisms described above, whereby each leads to an increasing level of reduction in brain reserve and therefore an increasing risk of dementia.
In line with this theory Greenberg et al. (2014) highlight that it is important to remember that not everyone who is diagnosed with MDD or PTSD will develop dementia, rather it appears that conditions such as PTSD ‘play an ancillary role among numerous factors that are involved in pathogenesis of dementia’ (pp. S163, Greenberg et al. 2014). The next section will explore how military veterans may represent a population at an increased risk of the pathogenesis of dementia due to a number of additional such factors.
Increased risk of dementia for military veterans
Increased prevalence of MDD and PTSD
Common mental health disorders are reported to occur at an increased rate in military personnel compared with the general population. Indeed, within the UK (Goodwin et al. 2015) found that the risk of common mental health disorders is approximately doubled in the military population as compared with the general population in employment (OR of 1 v. an OR of 2.4, respectively). Rates of PTSD are also reported at higher rates in military personnel from the USA (12.6%) and Australia (8.3%) (Hunt et al. (2014). Although the rate of PTSD in the UK Armed Forces is approximate to that in the general population (~4%), when military personnel deployed in combat roles are singled out prevalence rates increase to 5.7% (Fear et al. 2010). Therefore if, as civilian literature suggests, mental health conditions such as MDD and PTSD do represent risk factors for dementia, then military personnel, particularly those who have deployed, may represent a population with an increased vulnerability.
Substantial ageing population
In addition to this, due to the influx of recruitment from World War II and National Service, 46% of the UK's veteran population is over the age of 75, compared with only 10% of the general population (Royal British Legion, 2014). As mentioned earlier, age is the most significant risk factor for dementia, illustrating a further heightened risk factor for the veteran community over the general population.
Metabolic syndrome
Metabolic syndrome is a combination of obesity, high blood pressure and diabetes. Both hypertension and diabetes are postulated to interfere with Aβ clearance (Yaffe et al. 2014). As with obesity, although the prevalence of metabolic syndrome is not higher in the military population when compared with the general population, the rate does increase in those in the military population with a mental health diagnosis (Yaffe et al. 2014).
Physical inactivity
Physical activity is also described as a potential preventative factor for dementia since it both increases neurogenesis, as well as decreasing the risk of vascular disease and reducing inflammation (Yaffe et al. 2014). It has also been tentatively linked to lower levels of Aβ deposition in the brain (Yaffe et al. 2014). Again, Yaffe et al. (2014) propose that although the rates of physical activity in the veteran population is similar to the general population, there is some evidence of ‘retirement obesity’ for veterans who have previously held high levels of physical activity that are suddenly reduced when transitioning out of the military.
Alcohol and smoking
Alcohol and smoking are also identified as risk factors of dementia that are more common in the veteran population than the general population (Veitch et al. 2013; Yaffe et al. 2014). Smoking presents an increased risk of dementia in many ways including: vascular disease; inflammation; accelerated reductions in the cerebral blood flow; cerebral atrophy and the formation of white matter lesions and can roughly double the risk of Alzheimer's dementia (Veitch et al. 2013). For alcohol, although a low intake may be protective against dementia, excessive alcohol intake can be neurotoxic thus increasing the risk of dementia (Yaffe et al. 2014).
Traumatic brain injury (TBI)
One co-morbid condition that is frequently mentioned throughout the literature is TBI. TBI, is defined as ‘an external force to the head causes injury and results in alteration or loss or consciousness’ (Sibener et al. 2014) and is said to increase the risk of dementia by between a two- and fourfold rate (Sibener et al. 2014). The rate of TBI is projected to be much higher in the military population compared with the general population due to the risk of TBI from improvised explosive devices (IEDs) (Veitch et al. 2013; Weiner et al. 2013; Byers & Yaffe, 2014; Sibener et al. 2014). Rates of TBI after the recent Iraq and Afghanistan conflicts are assessed to be about 7% in US troops, although rates as high as 22% have been proposed, compared with about 0.5% in the general US population (Veitch et al. 2013). TBI has been proposed to interact with PTSD in three main ways: deposition of Aβ plaques and tau pathology; reduction in cognitive reserve; and ischaemic lesions (Veitch et al. 2013).
A link between mental health conditions such as MDD and PTSD with dementia holds a great deal of importance, especially for the veteran population who may be at an increased risk due the amplified prevalence of mental health problems as well as the heightened impact of a number of additional risk factors. This paper sets out to identify scientific literature examining the association between MDD, PTSD and dementia in the older veteran population.
Method
Search strategy
Relevant articles were identified by performing searches of the bibliographic databases MEDLINE, EMBASE, EBSCO, Web of Science and Google Scholar. Searches included keywords: Dementia, Alzheimer disease, depression, anxiety, PTSD, common mental disorders, alcohol & drug misuse, stress, military personnel, armed forces and veterans. Searches were limited to studies in articles published between 1990 and July 2016, in the English language, exploring the relationship between dementia and mental health in military veterans'. The full search strategy can be found in online Supplementary Appendix S1.
Selection strategy
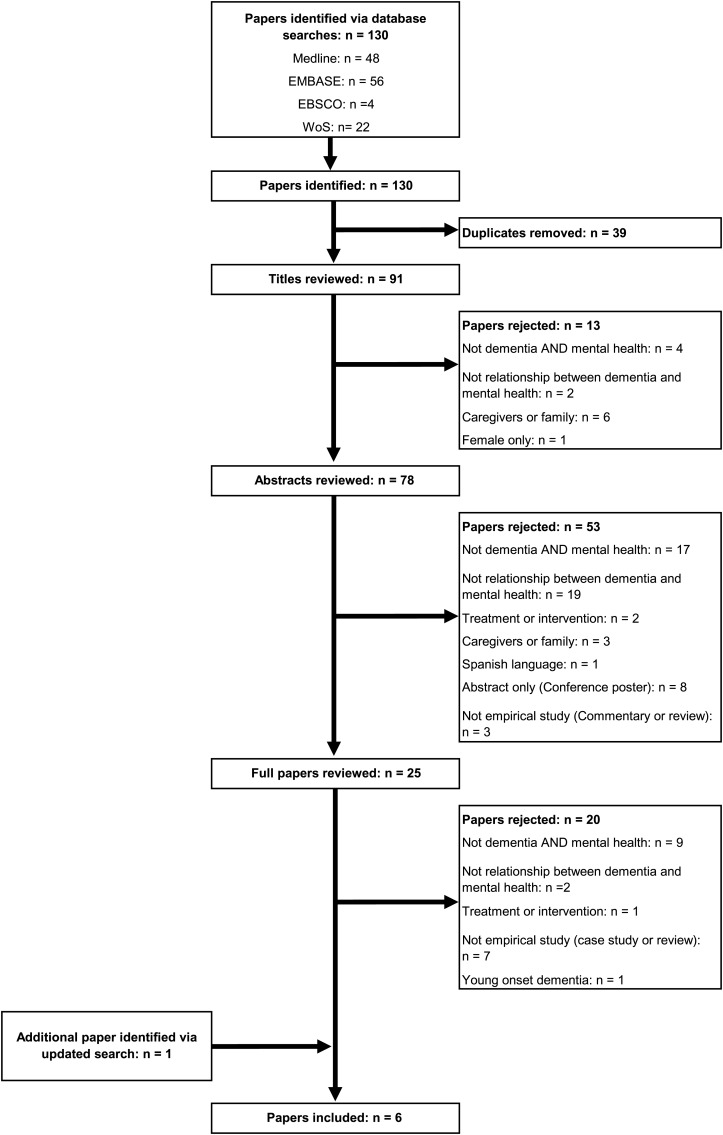
A total of 130 articles were retrieved from bibliographic searches. 39 papers were removed as duplicates and a further 13 were rejected after reviewing paper titles. Abstract reviews were then conducted on the remaining 78 papers, removing a further 53 as irrelevant. The final 25 papers were read in full, of which five papers were deemed to be relevant to the search criteria. Hand searching was also conducted of all references cited in articles. This process was conducted by LAR with a 10% sample of abstracts and full papers blind reviewed by SAMS with any discrepancies discussed and resolved. An updated search, following the same protocol, was conducted in February 2017, which identified an additional paper for inclusion. The inclusion process is outlined below in Fig. 1.
Fig. 1.
Inclusion process.
Quality appraisal
A quality criteria assessment tool for cohort studies was used to rate the methodological quality of the studies (http://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools). LAR and SAMS rated the studies independently according to the quality criteria given. Any discrepancies were discussed and resolved. After scoring all the criteria, the different ratings were listed and a final overall rating for each study was given jointly (see online Supplementary Appendix S2).
Study characteristics
Five of the papers included in this review were retrospective cohort studies based on data drawn from the Department of Veteran's Affairs medical care system in the USA. The studies identified eligible participants either aged 55 and over (Yaffe et al. 2010; Byers et al. 2012; Meziab et al. 2014), aged 56 and over (Mawanda et al. 2017) or aged 65 and over (Qureshi et al. 2010). Each of the studies utilised the existing definitions for dementia and mental health diagnosis, namely the ICD-9 Clinical Modification, with information about the diagnoses drawn from medical records. The remaining paper was conducted in Australia with randomly selected veterans from World War II taking part in a prospective cohort study, aged between 65 and 85 years at the second phase (Dent et al. 1998). Depression and dementia were explored via a clinical interview, focused on the DSM criteria for MDD, and the DSM criteria for dementia, along with the Mini Mental State exam (Dent et al. 1998). The number of study participants ranged from 209 (Dent et al. 1998) to 417 172 (Mawanda et al. 2017). All of the studies report that there were mental health diagnoses of either MDD or PTSD at a baseline point and then subsequent dementia diagnoses at a follow-up point. Only the Australian study specifies that the diagnosis of PTSD/MDD was still current at the follow-up phase. Table 2 below contains details of the characteristics of each paper reviewed and Table 3 provides information on the dementia types explored within each study.
Table 2.
Characteristics of included papers
| Author | Study design | Sample | Size | Mental Health Classification | Mental Health Diagnosis | Mental Health Diagnosis Data Source | Association |
|---|---|---|---|---|---|---|---|
| Byers et al. (2012) | Retrospective Cohort Study | US veterans 55 years & over |
n = 281 540 | ICD-9 Clinical Modification | Major Depression Disorder Dysthymia |
Department of Veteran's Affairs | HR: 2.18 (95% CI 2.08–2.28) HR: 1.96 (95% CI 1.71–2.25) |
| Dent et al. (1998) | Prospective Cohort Study | Australian veterans 56 years & over |
n = 209 | DSM Criteria Zung Depression Scale |
Major Depressive Disorder/Other Depression Depressive symptoms |
Clinical Interview | R: 0.13 (95% CI 0.00–0.26) R: 0.16 (95% CI 0.02–0.29) |
| Mawanda et al. (2017) | Retrospective Cohort Study | US veterans 56 years & over |
n = 417 172 | ICD-9 Clinical Modification | PTSD PTSD + Psychotropic Medication (SSRI) PTSD + Psychotropic Medication (SNRI) PTSD + Psychotropic Medication (AAI) |
Department of Veteran's Affairs | HR: 1.35 (95% CI 1.27–1.43) HR: 1.99 (95% CI 1.72–2.29) HR: 2.02 (95% CI 1.78–2.30) HR: 4.21 (95% CI 3.72–4.76) |
| Meziab et al. (2014) | Retrospective Cohort Study | US veterans 55 years & over |
n = 484 | ICD-9 Clinical Modification | PTSD PTSD + POW |
Department of Veteran's Affairs | HR: 1.52 (95% CI 1.41–1.64) HR: 2.24 (95% CI 1.72–2.92) |
| Qureshi et al. (2010) | Retrospective Cohort Study | US veterans 65 years & over |
n = 10 481 | ICD-9 Clinical Modification | PTSD PTSD + Purple Heart |
Department of Veteran's Affairs | OR 2.2 (95% CI 1.8–2.6) OR 1.4 (95% CI 0.7–2.7) |
| Yaffe et al. (2010) | Retrospective Cohort Study | US veterans 55 years & over |
n = 181 093 | ICD-9 Clinical Modification | PTSD | Department of Veteran's Affairs | HR: 2.31 (95% CI 2.24–2.39) |
Table 3.
Types of dementia explored in included papers
| Byers et al. (2012) | Dent et al. (1998) | Mawanda et al. (2017) | Meziab et al. (2014) | Qureshi et al. (2010) | Yaffe et al. (2010) | |
|---|---|---|---|---|---|---|
| Alzheimer's disease | ||||||
| Vascular dementia | ||||||
| Lewy body dementia | ||||||
| Frontotemporal dementia | ||||||
| Senile dementia | ||||||
| Dementia not otherwise specified | ||||||
| Alcohol-induced dementia | ||||||
| Drug-induced dementia | ||||||
| Parkinsons | ||||||
| Other degenerative diseases of the basal ganglia | ||||||
| Dementia due to Huntingtons disease | ||||||
| Dementia due to Jakob–Creutzfeldt disease | ||||||
| Dementia due to Multifocal leukoencephalopathy (Encephalitis) | ||||||
| Dementia in conditions classified elsewhere, e.g. physical condition |
The majority of papers focused on the four most common types of dementia, as illustrated in Table 1, as well as a more generic dementia category (Yaffe et al. 2010; Byers et al. 2012; Meziab et al. 2014; Mawanda et al. 2017). Qureshi et al. (2010) provide the most comprehensive categorisation of dementia covering a far broader range of dementia types than the other studies reviewed (Table 3).
Findings
Dementia and MDD
Byers et al. (2012) explored both MDD and dysthymia, which they defined as a depressive spectrum diagnosis, in veterans with no evidence of dementia at a study baseline point between 1997 and 2000 (n = 281 540). At a follow-up point between 2001 and 2007, after adjusting for demographics and comorbidities, veterans diagnosed with dysthymia or MDD were twice as likely to develop dementia compared with those with no dysthymia or MDD (Byers et al. 2012). The research of Byers et al. (2012) provides evidence for an association between the larger spectrum of depressive disorders and an increased risk of dementia in older veterans.
Dent et al. (1998) also explored the relationship between MDD and dementia, as well as investigating lower levels of depressive symptoms and cognitive decline. Veterans from World War II, living in Sydney, were tested in 1982 and again in a follow-up session in 1991 (n = 209). The results of the study found that the association between depressive symptoms and poor cognitive performance could be explained by the impact of verbal intelligence, a measure deemed resistant to the effects of brain pathology. Although a small correlation was found between MDD in 1982 and dementia in 1991, this was not statistically significant (r = 0.13, CI 0.00–0.26) and no concurrent correlation was found between MDD in 1991 and dementia in 1991. The lack of a significant difference in the prevalence of dementia in those with and without MDD at baseline led the authors to conclude that MDD was not a predictor of dementia (Dent et al. 1998).
Dementia and PTSD
Exploring the relationship between PTSD and dementia Yaffe et al. (2010) found that US veterans (n = 181 093) with a diagnosis of PTSD at baseline were significantly more likely to have a diagnosis of dementia at a follow-up period (roughly 7 years later), than those without a diagnosis of PTSD.
Qureshi et al. (2010) explored the association between dementia and PTSD in US veterans over the age of 65 (n = 10 481). Four groups of participants were identified: (1) a control group; (2) a group with a PTSD diagnosis; (3) a group with a Purple Heart (a medal presented to veterans physically wounded in combat, which they used as a proxy for combat exposure); and (4) a group with both PTSD and a Purple Heart. Veterans with PTSD and no Purple Heart were twice as likely as those without PTSD and no Purple Heart, or those without PTSD and a Purple Heart to develop dementia. This study allows the distinction to be made between the impact of combat exposure and PTSD, showing PTSD to represent the more substantial risk for dementia (Qureshi et al. 2010).
Meziab et al. (2014) investigated the relationship between PTSD and dementia as well as the impact Prisoner-of-war (POW) status may have on this relationship (n = 484). Adjusting for demographics, medical and psychiatric comorbidities, period of service and the competing risk of death, there was an increased risk of more than 50% for dementia in POWs, an increased risk of more than 50% for dementia in those with PTSD and those veterans with both PTSD and POW status were twice as likely to develop dementia (Meziab et al. 2014). Meziab et al. (2014) suggest that the additive effect of PTSD and POW status found in their study may indicate that the underlying mechanisms behind the impact of each status on dementia are different, presenting POW status as an additional risk factor pertinent to the veteran community.
Mawanda et al. (2017) examined the association between PTSD and dementia, as well as the potential impact of psychotropic medication use on this relationship in US veterans (n = 417 172). Those veterans with a diagnosis of PTSD at baseline (2002–2003) were significantly more likely to have a diagnosis of dementia during the follow-up period (2004–2012) (Mawanda et al. 2017). The authors found that psychotropic medication use impacted this association, specifically those veterans with a diagnosis of PTSD and a history of specific psychotropic medication use [SSRIs, serotonin–norepinephrine reuptake inhibitors (SNRIs), and atypical antipsychotics (AAs)] were significantly more at risk of dementia than those with a diagnosis of PTSD and no history of psychotropic medication use (Mawanda et al. 2017). In addition to this, Mawanda et al. (2017) found that use of specific psychotropic medication at baseline [benzodiazepines (BZAs) or SNRIs] lead to a significantly increased risk of dementia at follow up, independent of PTSD diagnosis. This suggests that use of specific psychotropic medications may act as an additional risk factor for dementia (Mawanda et al. 2017).
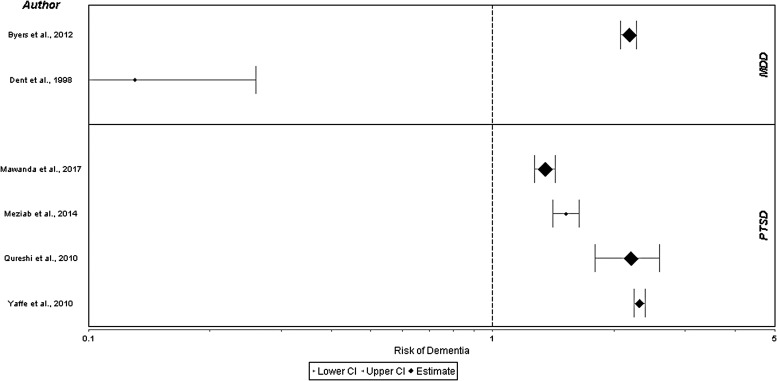
As indicated in Fig. 2 the relationship between PTSD and dementia appears to be supported by the papers included in this review. Further research is required to ascertain the relationship between MDD and dementia and to understand the different results in the papers included in this review.
Fig. 2.
Forest plots of MDD, PTSD and dementia.
Discussion
Overview of results
The review identified six papers, which discussed either MDD or PTSD, and dementia in military veterans, published in peer reviewed journals. Despite the studied participants originating from the US or Australian military, given the neurobiological nature of dementia, the results should hold relevance to the Armed Forces worldwide.
The initial hypothesis for this paper was that suffering MDD/PTSD resulted in an increased risk of dementia in military veterans. This review found a significant association between PTSD and a later diagnosis of dementia, which supports the assertion that a diagnosis of PTSD increases the risk of dementia in military veterans. The relationship between MDD and dementia illustrates conflicting results with one study supporting the relationship (Byers et al. 2012) and another denying it (Dent et al. 1998).
Dent et al. (1998) is the only paper, which does not support the relationship between MDD/PTSD and dementia. There are a number of potential reasons for this variation. The Dent et al. (1998) study is the only study, which employs a prospective as opposed to retrospective design. Prospective designs are thought to provide more accurate measures of risk, with less potential bias and confounding variables, so it may be that the non-significant relationship between MDD and dementia found in the Dent et al. (1998) study represents the more accurate finding. The Dent et al. (1998) study is also the only study that utilised clinical interviews to diagnose both MDD and dementia and thus its results may well be more valid than those drawing diagnoses from medical records. However, the Dent et al. (1998) study employed a comparatively small sample size of 209, compared with sample sizes in the 100 000s for the majority of the VA studies potentially impacting the power of its findings. The Dent et al. (1998) study is also the only study which was conducted outside of the USA suggesting that there may be a cultural confounder at play, possibly in terms of the application of diagnostic criteria.
Within the civilian literature an OR of between 1.90 (95% CI 1.55–2.33) and 2.03 (95% CI 1.73–2.38) was identified in Ownby et al. (2006) meta-analyses for MDD and dementia. This is comparable with results of Byers et al. (2012) where a hazard ratio of 2.18 (95% CI 2.08–2.28) was found. The outlier is Dent et al. (1998) study where no significant risk was identified.
Proposed explanations for findings
The research studies included in the review provided limited potential explanations for the mechanisms behind the association between MDD/PTSD and dementia. Table 4 below illustrates the pathways discussed within the papers.
Table 4.
Neurobiological pathways
Although there is limited discussion in the reviewed papers on the pathways that may link MDD/PTSD and dementia, what discussion there is supports both the inflammatory neurodegeneration hypothesis and the notion of brain reserve.
Evidence supporting both hypotheses is also present in the majority of papers included in the review. Byers et al. (2012) illustrate that dysthymia, as well as MDD, increases the risk of dementia. Mawanda et al. (2017) found that psychotropic medications also increase the risk of dementia. Since both dysthymia, and psychotropic medications, also impact neuroinflammation this provides further support for the theory that inflammation is at the root of the association between MDD/PTSD and dementia.
Additional risk factors that separately increase the risk of dementia in military veterans are found in three of the papers reviewed here. Meziab et al. (2014) conclude that POW status increases the risk of dementia, Mawanda et al. (2017) illustrate that psychotropic medications can increase the risk of dementia and Qureshi et al. (2010) show that Purple Heart status, indicative of combat exposure, also increased the risk of dementia. Each of these additional risk factors supports the notion that dementia risk may steadily increase as each additional risk factor depletes individuals' brain reserve.
It could be assumed that from the plethora of additional risk factors the military veteran population face that their risk of dementia should be heightened over the civilian population. Although current rates of dementia in the military population appear to be no higher than the general population, at least with regard to the US military population (Sibener et al. 2014), it would be expected that increasing rates of PTSD and MDD with recent deployments would lead to an increased ‘future’ rate of dementia in the future veteran population. In line with the work of Butters et al. (2008), it may be that each of these risk factors reduces the veterans' brain reserve, continuing to steadily increase their risk of dementia. If we take a similar stance then the risk for military veterans is not only dramatic but also highly complex. We suggest that future research should aim to unpack the pathways and mechanisms involved, as well as identify if and how these pathways are inter-related, in order to begin to understand the increased risk for this population.
Limitations
Retrospective cohort studies
The research presented here cannot identify causality; no conclusions can be drawn as to whether MDD and PTSD cause dementia or whether another factor causes both mental health conditions. As mentioned earlier, prospective studies are needed to provide more accurate measures of risk, with less potential bias and confounding variables.
Diagnostic method variability
As Meziab et al. (2014) highlight, studies that draw data from VA records draw from records kept for medical and billing purposes and as such may hold some misrepresentations. Dent et al. (1998) is the only study where the reader is provided details of how the diagnoses were made. As such we are unable to ascertain, but may assume, that there is a degree of diagnostic method variability between the studies, at least between the Dent et al. (1998) study and the VA studies.
Relevance to UK military veterans
The limited available evidence supports an association between PTSD and MDD with dementia within military veterans in the USA. All of the retrospective cohort studies reviewed in this paper were based on data from the Department of Veteran's Affairs medical care system in the USA and as such are limited to those who utilise this service (Krishnan et al. 2005; Qureshi et al. 2010; Yaffe et al. 2010; Byers et al. 2012; Meziab et al. 2014). Such research may hold questionable salience in the UK where rates of mental health difficulties in military personnel vary substantially from the USA. Empirical evidence exploring this association within UK military veterans, as well as the causal pathways underlying this relationship, is needed.
Potential confounding variables
Qureshi et al. (2010) also highlights that VA studies are unable to collect additional data that may have been influential, such as the duration, severity, or treatment of PTSD/MDD, which may have impacted the dementia diagnosis.
Lack of neurological data
The studies based on the VA were unable to collect any neurobiological information, such as inflammatory markers (Krishnan et al. 2005; Qureshi et al. 2010; Yaffe et al. 2010; Byers et al. 2012; Meziab et al. 2014).
Systematic review process
Although a 10% sample of the abstracts for review were also screened by an independent author, the robustness of the review could have been improved if the entire review process was conducted by two independent authors.
Implications
Research implications
We are still unable to prove, or explain, whether PTSD or MDD are risk factors for dementia within the UK, or worldwide, military veteran population. A large-scale cohort study is needed to assess UK military veterans' MDD/ PTSD and dementia status over a significant period of time, including the capturing of neurobiological markers and the use of brain imaging to understand the mechanisms underlying such an association. Such studies should be replicated to enable an appreciation of the risk to veterans worldwide. In addition to this further, small scale studies could be conducted to both measure neurobiological markers and test the potential impact of additional risk factors on the prevalence of dementia.
Military implications
It is understandable that much of the military mental ill-health research carried out to date is conducted with a focus on the here and now, and near future. However, the findings of this review support taking a longer-term view, and the mental well-being of older veterans, especially in terms of dementia/Alzheimer's disease, should be considered. Whilst the onset of dementia cannot be currently predicted with any great accuracy (aside possibly from the genetic factors), nor the inevitable slow decline in cognitive functioning associated with the condition be alleviated, it may be possible to highlight veterans who may be at higher risk, and hence provide timely and measured support accordingly.
The evidence available to date which indicates that the veteran population is at heightened risk of developing dementia over the general population is highly relevant for the future care of military veterans. Should this potential increased risk be confirmed, then care provisions for veterans with dementia will need to be prioritised to some degree to ensure consistency with the Military covenant promise (Ministry of Defence, 2015). Further research is therefore required to identify whether the findings in this review of mainly US papers, hold true for UK veterans and indeed veterans worldwide.
Clinical implications
The inflammatory neurodegeneration hypothesis cites inflammation at the centre of the association between MDD/PTSD and dementia. If proven this would have far-reaching clinical implications for the treatment of all three conditions. In addition to this anti-inflammatory medication may in fact help to mediate any potential relationship between conditions reducing the risk of dementia.
Conclusion
This review concludes that current evidence suggests that the military veteran community are at an increased risk of dementia due to the increased prevalence of mental health conditions such as PTSD and MDD within this population, as well as the supplementary impact of other military risk factors on this association. With the myriad of potential risk factors faced by military veterans it seems likely that the additive, complex interaction of all these factors impacts the development of dementia. Both the theory of inflammatory neurodegeneration and the brain reserve hypothesis hold potential in explaining this multifaceted relationship.
Acknowledgements
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Declaration of Interest
None.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0033291717001386.
click here to view supplementary material
References
- Alzheimer's Society (2014) What is Dementia? Available at https://www.alzheimers.org.uk/site/scripts/documents_info.php?documentID=106 (Accessed 18 February 2016).
- Apfel BA, Ross J, Hlavin J, Meyerhoff DJ, Metzler TJ, Marmar CR et al. (2011) Hippocampal volume differences in Gulf War Veterans with current versus lifetime posttraumatic stress disorder symptoms. Biological Psychiatry 69, 541–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellou V, Belbasis L, Tzoulaki I, Middleton LT, Ioannidis JP and Evangelou E (2017) Systematic evaluation of the associations between environmental risk factors and dementia: an umbrella review of systematic reviews and meta-analyses. Alzheimers & Dementia 13, 406–418. [DOI] [PubMed] [Google Scholar]
- Boorman E, Romano GF, Russell A, Mondelli V and Pariante CM (2015) Are mood and anxiety disorders inflammatory diseases? Psychiatric Annals 45, 240–248. [Google Scholar]
- British Medical Journal (2017a) BMJ Best Practice: Alzheimer's Dementia. Available at http://bestpractice.bmj.com/best-practice/monograph/317.html?g=w_bmj_bp (Accessed 18 April 2017).
- British Medical Journal (2017b) BMJ Best Practice: Dementia with Lewy Bodies. Available at http://bestpractice.bmj.com/best-practice/monograph/320.html?g=w_bmj_bp (Accessed 18 April 2017).
- British Medical Journal (2017c) BMJ Best Practice: Frontotemporal Dementia. Available at http://bestpractice.bmj.com/best-practice/monograph/968.html?g=w_bmj_bp (Accessed 18 April 2017).
- British Medical Journal (2017d) BMJ Best Practice: Vascular Dementia. Available at http://bestpractice.bmj.com/best-practice/monograph/319.html?g=w_bmj_bp (Accessed 18 April 2017).
- Burri A, Maercker A, Krammer S and Simmen-Janevska K (2013) Childhood trauma and PTSD symptoms increase the risk of cognitive impairment in a sample of former indentured child laborers in old age. PLoS ONE 8, e57826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butters MA, Young JB, Lopez O, Aizenstein HJ, Mulsant BH, Reynolds CF III et al. (2008) Pathways linking late-life depression to persistent cognitive impairment and dementia. Dialogues in Clinical Neuroscience 10, 345–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byers AL, Covinsky KE, Barnes DE and Yaffe K (2012) Dysthymia and depression increase risk of dementia and mortality among older veterans. The American Journal of Geriatric Psychiatry 20, 664–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byers AL and Yaffe K (2014) Depression and dementias among military veterans. Alzheimers & Dementia 10, S166–S173. [DOI] [PubMed] [Google Scholar]
- Clouston SA, Kotov R, Pietrzak RH, Luft BJ, Gonzalez A, Richards M et al. (2016) Cognitive impairment among World Trade Center responders: long-term implications of re-experiencing the 9/11 terrorist attacks. Alzheimers & Dementia (Amst) 4, 67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dent OF, Jorm AF, Tennant C, Fairley MJ, Sulway MR, Creasey H et al. (1998) Association between depression and cognitive impairment in aged male war veterans. Aging & Mental Health 2, 306–312. [Google Scholar]
- Fear NT, Jones M, Murphy D, Hull L, Iversen A, Coker B et al. (2010) What are the consequences of deployment to Iraq and Afghanistan on the mental health of the UK armed forces? A cohort study. The Lancet 375, 1783–1797. [DOI] [PubMed] [Google Scholar]
- Franklin TC, Wohleb ES and Duman RS (2015) The role of immune cells in the brain during physiological and pathological conditions. Psychiatric Annals 45, 232–239. [Google Scholar]
- Golier JA, Yehuda R, Lupien SJ, Harvey PD, Grossman R and Elkin A (2002) Memory performance in holocaust survivors with posttraumatic stress disorder. American Journal of Psychiatry 159, 1682–1688. [DOI] [PubMed] [Google Scholar]
- Goodwin L, Wessely S, Hotopf M, Jones M, Greenberg N, Rona RJ et al. (2015) Are common mental disorders more prevalent in the UK serving military compared to the general working population? Psychological Medicine 45, 1881–1891. [DOI] [PubMed] [Google Scholar]
- Greenberg MS, Tanev K, Marin MF and Pitman RK (2014) Stress, PTSD, and dementia. Alzheimers & Dementia 10, S155–S165. [DOI] [PubMed] [Google Scholar]
- Hunt EJ, Wessely S, Jones N, Rona RJ and Greenberg N (2014) The mental health of the UK Armed Forces: where facts meet fiction. European Journal of Psychotraumatology 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnan LL, Petersen NJ, Snow AL, Cully JA, Schulz PE, Graham DP et al. (2005) Prevalence of dementia among Veterans Affairs medical care system users. Dementia and Geriatric Cognitive Disorders 20, 245–253. [DOI] [PubMed] [Google Scholar]
- Lewis F, Karlsberg Schaffer S, Sussex J, O'Neill P and Cockcroft L (2014) The Trajectory of Dementia in the UK – Making a Difference. (ed. O. o. H. E. Consulting). Alzheimer's Research, UK. [Google Scholar]
- Mahendra B (1985) Depression and dementia: the multi-faceted relationship. Psychological Medicine 15, 227–236. [DOI] [PubMed] [Google Scholar]
- Mawanda F, Wallace RB, McCoy K and Abrams TE (2017) PTSD, psychotropic medication use, and the risk of dementia among US veterans: a retrospective cohort study. The Journal of the American Geriatric Society 65, 1043–1050. [DOI] [PubMed] [Google Scholar]
- Meziab O, Kirby KA, Williams B, Yaffe K, Byers AL and Barnes DE (2014) Prisoner of war status, posttraumatic stress disorder, and dementia in older veterans. Alzheimers & Dementia 10, S236–S241. [DOI] [PubMed] [Google Scholar]
- Ministry of Defence (2015) Armed Forces Covenant: 2015 to 2020. Available at https://www.gov.uk/government/publications/armed-forces-covenant-2015-to-2020/armed-forces-covenant (Accessed 18 April 2017).
- NHS (2015) Causes of Dementia. Available at http://www.nhs.uk/conditions/dementia-guide/pages/causes-of-dementia.aspx (Accessed 22 February 2016).
- Ownby RL, Crocco E, Acevedo A, John V and Loewenstein D (2006) Depression and risk for Alzheimer disease: systematic review, meta-analysis, and metaregression analysis. The Archives of General Psychiatry 63, 530–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Passmore P (2015) Behavioural and psychological symptoms in Alzheimer's disease. The Journal of Quality Research in Dementia 29, 1–13. [Google Scholar]
- Qureshi SU, Kimbrell T, Pyne JM, Magruder KM, Hudson TJ, Petersen NJ et al. (2010) Greater prevalence and incidence of dementia in older veterans with posttraumatic stress disorder. The Journal of the American Geriatric Society 58, 1627–1633. [DOI] [PubMed] [Google Scholar]
- Royal British Legion (2014) A UK Household Survey of the Ex-Service Community. Available at https://www.britishlegion.org.uk/media/2275/2014householdsurveyreport.pdf (Accessed 23 February 2016).
- Sibener L, Zaganjor I, Snyder HM, Bain LJ, Egge R and Carrillo MC (2014) Alzheimer's Disease prevalence, costs, and prevention for military personnel and veterans. Alzheimers & Dementia 10, S105–S110. [DOI] [PubMed] [Google Scholar]
- Valenzuela MJ and Sachdev P (2006) Brain reserve and cognitive decline: a non-parametric systematic review. Psychological Medicine 36, 1065–1073. [DOI] [PubMed] [Google Scholar]
- Veitch D, Friedl K and Weiner M (2013) Military risk factors for cognitive decline, dementia and Alzheimer's disease. Current Alzheimer Research 10, 907–930. [DOI] [PubMed] [Google Scholar]
- Weiner MW, Friedl KE, Pacifico A, Chapman JC, Jaffee MS, Little DM et al. (2013) Military risk factors for Alzheimer's disease. Alzheimers & Dementia 9, 445–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organisation (2015) Dementia. Available at http://www.who.int/mediacentre/factsheets/fs362/en/ (Accessed 22 February 2016).
- Yaffe K, Hoang TD, Byers AL, Barnes DE and Friedl KE (2014) Lifestyle and health-related risk factors and risk of cognitive aging among older veterans. Alzheimers & Dementia 10, S111–S121. [DOI] [PubMed] [Google Scholar]
- Yaffe K, Vittinghoff E, Lindquist K, Barnes D, Covinsky KE, Neylan T et al. (2010) Posttraumatic stress disorder and risk of dementia among US veterans. Archives of General Psychiatry 67, 608–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0033291717001386.
click here to view supplementary material