Abstract
Nursing professional development practitioners are encouraged to consider incorporating preferred learning styles into professional development programs. However, conclusive evidence about preferred learning styles does not exist. This study describes the preferred learning styles of nursing staff. Results showed that learning style preferences existed and were correlated with satisfaction, years of experience, and gender. The results can be used to plan and deliver professional development opportunities that are engaging and promote retention of learning.
Keywords: index of learning styles, learning style preferences, registered nurses
Assessing learning needs is essential for designing nursing professional development activities that address educational gaps and lead to safe patient care and positive patient outcomes. Resources for professional development can be limited and may compete with nurses’ other priorities for time, effort, and financial allocation. Considering learning style preferences of the intended learners is important for guiding nursing professional development practitioners (NPDPs) in developing effective education plans (McCrow, Yevchak, & Lewis, 2014). NPDPs have the opportunity to help learners identify individual learning style preferences, design educational initiatives in a way that supports various learning style preferences, and provide opportunities for learning to occur in a way that matches preferred learning styles (Hawkes & Hendricks-Jackson, 2017).
Literature Review
Learning styles represent “habitual cognitive and affective behaviors which determine how each individual interacts in learning situations or environments” (Andreou, Papastavrou, & Merkouris, 2014, p. 363). Learning styles are one part of the comprehensive approach to be considered in facilitating learning. Learning styles do not indicate one’s suitability for a particular education topic, how one will approach learning, or one’s intellectual ability (Felder & Brent, 2005). Additionally, the best method of instruction for a given topic may or may not fit with identified preferred learning styles of the target audience. The way one prefers to learn may not fit with the most effective modality for that topic (Kirschner, 2017).
Within nursing and health care, a variety of instruments have been utilized to assess learning style preferences, most predominately Kolb’s learning model and associated Learning Styles Inventory. The Learning Styles Inventory is a 12-item instrument that classifies learners as having a preference in one of four categories based on how individuals perceive and process information. Accommodators prefer doing and feeling, assimilators watching and thinking, divergers watching and feeling, and convergers thinking and doing (Kolb, 1984). Kolb’s Learning Styles Inventory has not identified a predominant category of learning style among nurses and nursing students. Divergers, accommodators, and convergers have been reported as dominant learning styles (Andreou et al., 2014; McKenna, Copnell, Butler, & Lau, 2018; Rassin, Kurzweil, & Maoz, 2015; Robinson, Scollan-Koliopoulos, Kamienski, & Burke, 2012; Shinnick & Woo, 2015; Smith, 2010; Tutticci, Lewis, & Coyer, 2016; Vizeshfar & Torabizadeh, 2018).
Information regarding learning style preferences specific to licensed nurses is limited to a small subset of nurses and was self-reported or variable regarding instrument type and sample. Two studies used the Learning Styles Inventory. A study by Smith (2010) indicated that registered nurses who were enrolled in online bachelor’s or master’s degree programs were predominately accommodators, and Rassin et al (2015) found that the most common learning style of nurses working in Israel was converger. Pilcher (2013) showed that a defined group of neonatal and maternal/child nurses self-reported that most enjoyed learning through lecture, followed by simulation, self-study, webinars, and finally audio-only podcasts. A study using the Visual Auditory Kinesthetic questionnaire found that nursing staff prefer visual learning over kinesthetic and auditory learning (Frankel, 2009). Finally, a study conducted by McCrow, Yevchak, and Lewis (2014) determined the preferred learning styles of 142 Australian acute care nurses using the Index of Learning Styles (ILS). The results of this study indicated that registered nurses were balanced on the active-reflective and sequential-global scales, but they had a preference of sensing over intuitive and visual over verbal. Table 1 provides a description of the ILS scales.
Table 1.
Index of Learning Styles
| Type of Learner | Description |
|---|---|
| Sensing | Concrete thinker |
| Practical | |
| Oriented toward facts and procedures | |
| Intuitive | Abstract thinker |
| Innovative | |
| Oriented toward theories and underlying meanings | |
| Visual | Prefer visual representations of presented material such as pictures, diagrams, and flow charts |
| Verbal | Prefer written and spoken explanations |
| Active | Learn by trying things out |
| Enjoy working in groups | |
| Reflective | Learn by thinking things through |
| Prefer working alone or with a single, familiar partner | |
| Sequential | Linear thinking process |
| Learn in small incremental steps | |
| Global | Holistic thinking process |
| Learn in large leaps |
Modified from Felder & Spurlin (2005). Used with permission.
Critics of learning styles theories identify a number of concerns. These include the difference between preferred learning and the learning method that will best lead to effective learning, classification of preference into distinct groups (not addressing that a continuum of learning styles may exist), weak explanatory frameworks for learning styles, and inadequate reliability and validity of tools used to determine learning style (An & Carr, 2017; Kirschner, 2017). NPDPs must consider instrumentation when assessing learning styles and utilize learning styles as one factor in designing and delivering professional development activities. Learning style profile results cannot be overinterpreted and may best be used with a group of learners to indicate preference distribution (Index of Learning Styles, n.d.).
Purpose of Current Research
Nursing professional development can be enhanced by determining nurses’ preferred learning styles; this knowledge can help ascertain how information is learned and retained (Dickerson, 2017). The NPDPs alignment of preferred learning styles with a type of instruction that best fits the educational need could promote learning. Including preferred learning styles with identification of learning needs from a variety of sources may help NPDPs develop, implement, and evaluate a comprehensive continuing professional development program for nurses at all levels of the organization. In addition to the learning styles assessment described here, the needs assessment should also include various internal sources (e.g., committees, strategic plan) and external sources (e.g., accreditation and regulatory trends, American Nurses Association, boards of nursing, professional organizations). This article describes one organization’s multifaceted approach to conducting an evaluation of learning needs in a Southwestern United States medical center.
Theoretical Framework
The Felder-Silverman Model guided the ILS assessment (Felder & Spurlin, 2005). This model was developed to describe the differences in learning styles among engineering students; the results were used to inform a teaching approach that encompassed the needs of all students. The model classifies learners along a continuum in four dimensions. Where a learner falls on the continuum for each dimension provides information about how he or she engages with learning materials and applies and retains information. The four dimensions are sensing-intuitive, visual-verbal, active-reflective, and sequential-global (Felder & Spurlin, 2005) and are described in Table 1.
Methods
Design
The purpose of this study was to describe the dominant patterns of learning for nursing staff as well as correlate preferred learning styles to demographic data and self-reported satisfaction with professional development activities. The organization’s institutional review board deemed the study exempt.
Sample and Setting
A total of 2,071 members of the nursing staff at a tertiary and quaternary academic medical center in the Southwestern United States with adult inpatient, ambulatory, procedural, and emergency services were eligible for the study. Nursing staff at all levels of the organization were invited to participate. Staff of all other types were excluded.
Instrument and Data Collection
Various tools that assess learning styles were identified with the support of medical librarians; the tools varied widely in relation to reliability, validity, length, and cost. The team chose the ILS (Felder & Spurlin, 2005) because of this tool’s reliability and validity, cost, ease of self-administration, and recent use in nursing (Brannan, White, & Long, 2016; McCrow et al., 2014). Another important consideration is that scoring of the ILS for each dimension is along a continuum, showing the range of responses and not locking learners or groups into one type. This is particularly important for NPDPs who are striving to create learning experiences that accommodate diverse learners. The ILS is a 44-item questionnaire that has four subscales (active-reflective, sensing-intuitive, visual-verbal, and sequential-global). A score of 1 to 3 in a dimension indicates that the individual is relatively well balanced and can learn well in an environment that is focused in either dimension of the subscale. A score of 5 to 7 indicates a moderate preference for learning, and learning will be easier if the environment favors that dimension. A score of 9 to 11 points to a strong preference for learning, and the learner will have considerable difficulty if the learning environment does not favor that dimension. The ILS has acceptable test-retest reliability, factor structure, internal consistency reliability, total-item correlation, interscale correlation, and construct validity (Felder & Spurlin, 2005; Litzinger, Lee, Wise, & Felder, 2007; Zywno, 2003). A demographic questionnaire and the ILS were administered to participants. Data were collected from January 2017 to March 2017 via an anonymous online survey tool or paper survey tool.
Data Analysis
Data analysis was conducted using SAS Studio statistical software (Version 4.1, SAS Institute Inc., Cary, NC) and R via RStudio (Version 0.99.891, RStudio, Inc., Boston, MA). Descriptive statistics were analyzed for demographic variables of interest. ILS results were analyzed using the scoring key provided by the tool author and Poisson regression, with relevant post hoc analyses done to evaluate relationships between ILS results and demographic and satisfaction variables.
Results
Demographic Variables
Overall, 67.55% (1,399/2,071) of nursing staff recruited completed the survey. The response rate varied on the basis of work area: Inpatient staff had a response rate of 83.62%; ambulatory staff, 74.87%; procedural/emergency department, 50.85%; advanced practice nurses, 56.79%; and nurse leaders, 67.00%. Nurse leaders included the chief nursing officer, nurse administrators, nurse managers, nurse supervisors, house supervisors, and nursing administrative specialists. All nurse leaders were RNs. Most respondents were women (86.37%) and were white/non-Hispanic (78.41%); most had a baccalaureate degree (61.85%). Details of these variables and years of experience are shown in Table 2. In addition, most nursing staff were satisfied with the current education provided (84.53%) compared with those reporting neutral or dissatisfied (Table 2).
Table 2.
Demographic Variables
| Variable | No. (%)a |
|---|---|
| Sex | |
| Female | 1,179 (86.37) |
| Male | 186 (13.63) |
| Race/ethnicity | |
| Asian/Pacific Islander | 105 (7.51) |
| Black/African American | 33 (2.36) |
| Hispanic/Latina(o) | 104 (7.43) |
| White/non-Hispanic | 1,097 (78.41) |
| American Indian | 11 (0.79) |
| Other/mixed | 49 (3.50) |
| Highest level of nursing education | |
| Diploma | 59 (4.63) |
| Associate degree | 228 (17.90) |
| Baccalaureate degree | 788 (61.85) |
| Master’s degree | 194 (15.23) |
| Doctorate degree | 5 (0.39) |
| Years of nursing/health care experience | |
| ≤5 | 342 (24.68) |
| 6–10 | 341 (24.60) |
| 11–25 | 437 (31.53) |
| ≥26 | 266 (19.19) |
| Satisfaction with education provided | |
| Satisfied | 1,169 (84.53) |
| Neutral | 154 (11.14) |
| Dissatisfied | 60 (4.34) |
Denominators vary depending on number of responses per category.
Index of Learning Styles
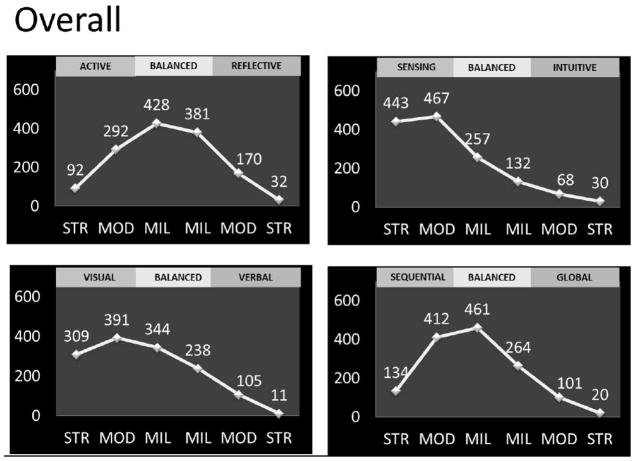
Analysis of learning style preference based on responses to items on each of the four dimensions of the ILS showed that nurses were well balanced overall on the active-reflective scale (i.e., provided similar responses on each end of the continuum from active to reflective), preferred sensing over intuitive learning and visual over verbal learning, and were fairly well balanced on the sequential-global scale with a slight shift towards sequential learning items. Table 3 provides results at each point on the continuums, and Figure 1 graphically represents these results.
Table 3.
Rates of Item Endorsement for the Index of Learning Styles
| Dimension | No. (%)a |
|---|---|
| Active-reflective | |
| Strong active | 92 (6.59) |
| Moderate active | 292 (20.93) |
| Weak active | 428 (30.68) |
| Weak reflective | 381 27.31 |
| Moderate reflective | 170 (12.19) |
| Strong reflective | 32 (2.29) |
| Sensing-intuitive | |
| Strong sensing | 443 (31.71) |
| Moderate sensing | 467 (33.43) |
| Weak sensing | 257 (18.40) |
| Weak intuitive | 132 (9.45) |
| Moderate intuitive | 68 (4.87) |
| Strong intuitive | 30 (2.15) |
| Visual-verbal | |
| Strong visual | 309 (22.10) |
| Moderate visual | 391 (27.97) |
| Weak visual | 344 (24.61) |
| Weak verbal | 238 (17.02) |
| Moderate verbal | 105 (7.51) |
| Strong verbal | 11 (0.79) |
| Sequential-global | |
| Strong sequential | 134 (9.63) |
| Moderate sequential | 412 (29.60) |
| Weak sequential | 461 (33.12) |
| Weak global | 264 (18.97) |
| Moderate global | 101 (7.26) |
| Strong global | 20 (1.44) |
Denominators vary depending on number of responses per category.
Dimension data from Felder & Spurlin (2005).
Figure 1. Index of Learning Styles Results.
The rate continuum of selected responses is shown for each point on the continuum for each subscale.
- Upper Left: Active-Reflective Scale
- Upper Right: Sensing-Intuitive Scale
- Lower Left: Visual-Verbal Scale
- Lower Right: Sequential-Global Scale
Key: STR indicates strong; MOD, moderate; MIL, mild.
Correlation of Learning Styles and Demographic Variables
The results of the Poisson regression analyses showed that satisfied respondents had an 11% stronger preference than neutral respondents for visual learning over verbal learning (exp[.104]=1.11; 95% confidence interval [CI] [1.04–1.18]; P<.01). Additionally, significant differences were found in visual learning by years of experience between those with ≥26 years and all other experience groups. Those with <26 years of experience had a 6% to 13% stronger preference for visual learning over verbal learning than those with >26 years of experience: <5 vs ≥26 years (exp[.12]=1.13; 95% CI [1.07–1.20]; P<.001); 6 to 10 vs ≥26 years (exp[.11]=1.11; 95% CI [1.05–1.18]; P<.001); and 11 to 25 vs ≥26 years (exp[.06]=1.07; 95% CI [1.01–1.13]; P=.033). Finally, significant differences in sensing and visual learning were found by gender; men had a 24% stronger preference for intuitive learning than women (exp[.22]=1.24; 95% CI [1.14–1.35]; P<.001) and a 17% stronger preference for visual learning (exp[.16]=1.17; 95% CI [1.11–1.24]; P<.001). Results did not show significant differences in learning profile by work area (i.e., hospital floor, specialty, or work unit).
Discussion
NPDPs are facing a demographic shift in the population they serve: 50% of registered nurses are now reported to be over 50 years and considering retirement in the coming years (Budden, Moulton, Harper, Brunell, & Smiley, 2016). With this shift, it is important to consider identifying learning style preferences of the workforce and provide professional development opportunities that support identified preferences. Technology and innovation will continue to transform the nursing world, and meaningful education will be imperative for providing quality patient care. The findings of this study support the need to understand the differences in learning styles of nurses and tailor education to support those preferences. Although limited information is available in the literature, this study supports learning activities that implement educational mediums for visual and sensing learners.
Similar to results from the study of McCrow, Yevchak, and Lewis (2014), the results indicated that sensing and visual were preferred learning styles among those surveyed regardless of gender, age, or experience. These preferred styles could be related to the job requirements and work environments of professional nurses. Identifying these styles, particularly on a work unit level, can allow for education that supports an identified area or group of nurses (McCrow et al., 2014).
Important findings related to the visual-verbal scales were identified. Satisfied respondents had a 10% stronger preference for visual learning than neutral respondents, which may be due to such a large majority of respondents (74.68%) with a preference for visual learning. Additionally, those with the most experience (≥26 years) had a stronger preference for verbal learning than those in all other experience categories. This finding shows a shift toward visual learning of more recent employment cohorts. Satisfaction is a self-reported but important variable because it helps identify how well training was received and can influence the reputation of professional development activities. The difference in visual-verbal learning by gender may be attributed to differences in sample size between the two genders, but this finding is important to consider when NPDPs are serving a diverse workforce. In our study, men had a 17% stronger preference for visual learning than women. Correlations of satisfaction, years of experience, and gender with the ILS visual-verbal scale bring notice to the NPDP to utilize visual learning tactics whenever possible.
Limitations
Limitations of this study relate to the sample of nurses recruited to complete the ILS; respondents were from one organization and may not represent the general population of nurses. The ILS tool was also originally designed for engineers, although it is gaining use in nursing and health care. The consistency of results to those of McCrow, Yevchak, and Lewis (2014) further validate the ILS tool for use in the nursing profession.
Implications for NPD Practice
Stakeholder engagement helped the team overcome traditional challenges involved in assessing learning needs, including interest in the process and target audience representation. The project plan was endorsed by the Department of Nursing’s research and education subcommittees and supported by leadership. These groups were able to promote participation in the process with colleagues and provide valuable recommendations. It was suggested that the ILS be offered both online and on paper, allowing each area to choose the best method for their team. As a result of this suggestion, the overall response rate was 67.55%, an increase of 37% from a prior assessment of learning needs in 2015. A higher response rate was noted for those using the paper tool (97.41%) than for those using the online method (58.2%). Therefore, NPDPs can consider the appropriate methods and available resources for gathering learning needs assessments and other data to potentially increase staff engagement and provide a broader sample. Resources for this project also included medical librarians assisting with the literature review and tool identification, a biostatistician for data analysis, and a volunteer from the research department to assist with data entry.
Although tailoring all education to individual preferences would be impossible, the ILS results allow for the NPDP to design and deliver professional development activities with these preferences in mind. It is essential to note that the results also support delivering education in multiple formats to allow learners to choose which method is most conducive for them. Learning style preference information can be considered by all NPDPs throughout the education process to provide an engaging experience that promotes understanding and retention of content. Knowledge of learning style preferences allowed NPDPs to be innovative and advocate for resources to facilitate learning in unique ways. Understanding learning style profiles challenged the team to think globally when a learning need is identified. Learning style preferences, available resources, and the optimal modality are now considered early in the education planning stage.
Practice changes have been made at the institution on the basis of the study results. For example, the organizers of the organization’s annual nursing conference incorporated a panel discussion with audience participation for the topic of “Safe Patient Handling.” Attendees conversed with the experts on the panel about utilization and best practices. The panel questions were displayed on the screen. This method incorporated active learning, augmented a verbal style with visual aids, and provided practical tips to meet the learning style preferences of the sensing learner. The results of this study have also led to the development of a Department of Nursing Education Fair. This fair allows for hands-on learning for a variety of topics identified as learning needs in an environment that is experiential and practical.
Facilitating learning at the point of care has also been implemented. The central venous catheter workgroup used the results of the study to design walking rounds at the point of care. Actual catheters and dressing change kits were used in the education so that staff could handle the equipment, identify errors, and be rewarded for correct answers. This method allowed for engagement of clinical nurses and promoted adherence to policies and protocols, which has the potential to support positive patient outcomes.
Finally, the results of the study led the NPDPs to consider the best methods to promote evidence-based practice and research. Journal clubs are being started in the Department of Nursing as a method to provide for active learning through interaction, collaboration, and discussion. Although outcomes of these initiatives are pending, initial feedback from participants has been favorable. Future research is needed to evaluate teaching methods to fit specific learning style preferences.
Conclusion
Learning style preferences exist among practicing nurses. The need for education in various formats is essential to the success of nurses in the ever-changing health care environment. The NPDP needs to be efficient and innovative in preparing professional development opportunities related to onboarding, competency, and continuing education in order to engage and retain the nursing staff. Knowledge of preferred styles of learning of the organization’s nursing staff can inform the planning delivery, resource utilization, and evaluation of learning activities.
Acknowledgments
The authors would like to acknowledge Diana Almader-Douglas, Noel M. Arring, Dennis Fitz-Patrick, Jennifer M. Lutz, Lisa A. Marks, and Bridget A. Tippins for their support in this research study.
Study data were collected and managed using REDCap electronic data capture tools hosted at Mayo Clinic.1 REDCap (Research Electronic Data Capture) is a secure, web-based application designed to support data capture for research studies, providing 1) an intuitive interface for validated data entry; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages; and 4) procedures for importing data from external sources.
Abbreviations
- CI
confidence interval
- ILS
Index of Learning Styles
- NPDPs
nursing professional development practitioners
Biographies
Kara L. Mangold, DNP, MS, RN is an Assistant Professor in Nursing and a Nursing Education Specialist at Mayo Clinic Hospital, Phoenix, Arizona.
Katie L. Kunze, PhD is a Biostatistician I in Biostatistics at Mayo Clinic, Scottsdale, Arizona.
Michelle M. Quinonez, MSN, RN, OCN is an Instructor of Nursing and a Nursing Education Specialist at Mayo Clinic, Scottsdale, Arizona
Lorna M. Taylor, MS, RN is a Nursing Education Specialist at Mayo Clinic Hospital, Phoenix, Arizona.
Ashley Tenison, MSN, RN, CMSRN is a Nursing Education Specialist at Mayo Clinic Hospital, Phoenix, Arizona.
Footnotes
Paul A. Harris, Robert Taylor, Robert Thielke, Jonathon Payne, Nathaniel Gonzalez, Jose G. Conde. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009 Apr;42(2):377-81.
Conflicts of Interest and Source of Funding: None declared. This project was supported by Grant Number UL1 TR002377 from the National Center for Advancing Translational Sciences (NCATS). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. Support for this research study was also provided by the Anne L. Bronfman Mayo Clinic in Arizona Nursing Excellence Fund.
Publisher: To expedite proof approval, send proof via scipubs@mayo.edu.
References
- An D, Carr M. Learning styles theory fails to explain learning and achievement: Recommendations for alternative approaches. Personality and Individual Differences. 2017;116:410–416. doi: 10.1016/j.paid.2017.04.050. [DOI] [Google Scholar]
- Andreou C, Papastavrou E, Merkouris A. Learning styles and critical thinking relationship in baccalaureate nursing education: a systematic review. Nurse Education Today. 2014;34(3):362–371. doi: 10.1016/j.nedt.2013.06.004. [DOI] [PubMed] [Google Scholar]
- Brannan JD, White A, Long J. Learning Styles: Impact on Knowledge and Confidence in Nursing Students in Simulation and Classroom. International Journal of Nursing Education Scholarship. 2016;13(1) doi: 10.1515/ijnes-2015-0052. [DOI] [PubMed] [Google Scholar]
- Budden JS, Moulton P, Harper KJ, Brunell M, Smiley RS. The 2015 National Nursing Workforce Survey. Journal of Nursing Regulation. 2016;7(1):S1–S90. doi: 10.1016/S2155-8256(16)31055-9. [DOI] [Google Scholar]
- Dickerson P. Core curriculum for nursing professional development. 5. Chicago, IL: Association for Nursing Professional Development; 2017. [Google Scholar]
- Felder RM, Brent R. Understanding Student Differences. Journal of Engineering Education. 2005;94(1):57–72. doi: 10.1002/j.2168-9830.2005.tb00829.x. [DOI] [Google Scholar]
- Felder RM, Spurlin J. Applications, Reliability and Validity of the Index of Learning Styles. International Journal of Engineering Education. 2005;21(1):103–112. [Google Scholar]
- Frankel A. Nurses’ learning styles: promoting better integration of theory into practice. Nursing Times. 2009;105(2):24–27. [PubMed] [Google Scholar]
- Hawkes B, Hendricks-Jackson L. Nursing professional development : review and resource manual. 4. Silver Spring, MD: American Nurses Credentialing Center/American Nurses Association; 2017. [Google Scholar]
- Index of Learning Styles (ILS) n.d Retrieved from http://www4.ncsu.edu/unity/lockers/users/f/felder/public/ILSpage.html.
- Kirschner PA. Stop propagating the learning styles myth. Computers & Education. 2017;106:166–171. doi: 10.1016/j.compedu.2016.12.006. [DOI] [Google Scholar]
- Kolb DA. Experiential Learning: Experience as the Source of Learning and Development. Englewood Cliffs, NJ: Prentice-Hall, Inc; 1984. [Google Scholar]
- Litzinger TA, Lee SH, Wise JC, Felder RM. A Psychometric Study of the Index of Learning Styles. Journal of Engineering Education. 2007;96(4):309–319. doi: 10.1002/j.2168-9830.2007.tb00941.x. [DOI] [Google Scholar]
- McCrow J, Yevchak A, Lewis P. A prospective cohort study examining the preferred learning styles of acute care registered nurses. Nurse Education in Practice. 2014;14(2):170–175. doi: 10.1016/j.nepr.2013.08.019. [DOI] [PubMed] [Google Scholar]
- McKenna L, Copnell B, Butler AE, Lau R. Learning style preferences of Australian accelerated postgraduate pre-registration nursing students: A cross-sectional survey. Nurse Education in Practice. 2018;28:280–284. doi: 10.1016/j.nepr.2017.10.011. [DOI] [PubMed] [Google Scholar]
- Pilcher J. Learning preferences among neonatal and maternal child nurses. Neonatal Network. 2013;32(2):117–119. doi: 10.1891/0730-0832.32.2.117. [DOI] [PubMed] [Google Scholar]
- Rassin M, Kurzweil Y, Maoz Y. Identification of the Learning Styles and “On-the-Job” Learning Methods Implemented by Nurses for Promoting Their Professional Knowledge and Skills. International Journal of Nursing Education Scholarship. 2015;12 doi: 10.1515/ijnes-2015-0006. [DOI] [PubMed] [Google Scholar]
- Robinson JA, Scollan-Koliopoulos M, Kamienski M, Burke K. Generational differences and learning style preferences in nurses from a large metropolitan medical center. Journal for Nurses in Staff Development. 2012;28(4):166–172. doi: 10.1097/NND.0b013e31825dfae5. [DOI] [PubMed] [Google Scholar]
- Shinnick MA, Woo MA. Learning style impact on knowledge gains in human patient simulation. Nurse Education Today. 2015;35(1):63–67. doi: 10.1016/j.nedt.2014.05.013. [DOI] [PubMed] [Google Scholar]
- Smith A. Learning styles of registered nurses enrolled in an online nursing program. Journal of Professional Nursing. 2010;26(1):49–53. doi: 10.1016/j.profnurs.2009.04.006. [DOI] [PubMed] [Google Scholar]
- Tutticci N, Lewis PA, Coyer F. Measuring third year undergraduate nursing students' reflective thinking skills and critical reflection self-efficacy following high fidelity simulation: A pilot study. Nurse Education in Practice. 2016;18:52–59. doi: 10.1016/j.nepr.2016.03.001. [DOI] [PubMed] [Google Scholar]
- Vizeshfar F, Torabizadeh C. The effect of teaching based on dominant learning style on nursing students' academic achievement. Nurse Education in Practice. 2018;28:103–108. doi: 10.1016/j.nepr.2017.10.013. [DOI] [PubMed] [Google Scholar]
- Zywno MS. A Contribution to Validation of Score Meaning for Felder Soloman’s Index of Learning Styles. Paper presented at the Proceedings of the 2003 American Society for Engineering Education Annual Conference & Exposition; Nashville, TN. 2003. [Google Scholar]