Abstract
Context:
Assessing global, regional, and fear-of-reinjury outcomes in individuals with chronic ankle instability (CAI) is critical to understanding the effectiveness of clinical interventions.
Objective:
To determine the improvement of patient-reported outcomes after balance- and strength-training and control protocols among participants with CAI.
Design:
Randomized controlled clinical trial.
Setting:
Athletic training research laboratory.
Patients or Other Participants:
Thirty-nine volunteers with CAI who scored 11 or greater on the Identification of Functional Ankle Instability questionnaire were randomly assigned to 1 of 3 groups: balance-training protocol (7 males, 6 females; age = 23.5 ± 6.5 years, height = 175.0 ± 8.5 cm, mass = 72.8 ± 10.9 kg), strength-training protocol (8 males, 5 females; age = 24.6 ± 7.7 years, height = 173.2 ± 9.0 cm, mass = 76.0 ± 16.2 kg), or control (6 males, 7 females; age = 24.8 ± 9.0 years, height = 175.5 ± 8.4 cm, mass = 79.1 ± 16.8 kg).
Intervention(s):
Each group met for 20 minutes, 3 times each week, for 6 weeks. The control group completed a mild to moderately strenuous bicycle workout.
Main Outcome Measure(s):
Global patient-reported outcomes, regional ankle function, and perceived instability were measured using the Disablement in the Physically Active Scale, the Fear-Avoidance Beliefs Questionnaire, the Foot and Ankle Ability Measure, and a visual analog scale for perceived instability. Participants completed the questionnaires at pretest and 6 weeks posttest. A multivariate repeated-measures analysis of variance with follow-up univariate analysis was conducted. The α level was set a priori at .05.
Results:
No time-by-group interaction was found (P = .78, η2 = 0.09). However, we observed a main effect for time (P = .001, η2 = 0.49). Follow-up univariate analyses revealed differences between the pretest and posttest for the Disablement in the Physically Active Scale (P = .02, η2 = 0.15), Fear-Avoidance Beliefs Questionnaire (P = .001, η2 = 0.27), Foot and Ankle Ability Measure–Activities of Daily Living subscale (P = .003, η2 = 0.22), Foot and Ankle Ability Measure–Sport subscale (P = .001, η2 = 0.36), and visual analog scale (P = .008, η2 = 0.18).
Conclusions:
Statistically, after the 6-week intervention, all groups improved in global and regional health-related quality of life. Clinicians should compare patient-reported outcomes with clinical measures to have a better understanding of progression during rehabilitation.
Key Words: rehabilitation, questionnaires, health-related quality of life, disability
Key Points
After a 6-week intervention, participants in both the balance- and strength-training–protocol and control groups improved in global and regional health-related quality of life.
The balance-training–protocol group had a meaningful improvement in global and regional health-related quality of life.
Clinicians should compare patient-reported outcomes with clinical and laboratory measures to gain a better understanding of progression during rehabilitation.
Rehabilitation protocols should incorporate the entire lower extremity to improve global and regional patient-reported outcomes.
Lateral ankle sprains are the most common musculoskeletal injuries in sports and among the physically active.1 Sixty percent of high school and collegiate athletes have experienced at least 1 ankle sprain,2 and 73% of all college-aged students have experienced an ankle sprain.3 These injuries are also responsible for the highest proportion of total weeks missed from sport participation.4 Many long-term problems can occur after an ankle sprain, including degenerative changes in the joint,5 decreased quality of life, reduced physical activity levels across the lifespan, development of chronic ankle instability (CAI), and increased risk of ankle osteoarthritis.6 The term CAI is associated with these prolonged symptoms that can occur after an initial ankle sprain.
Many researchers7–9 have focused on pathologic concerns, such as degenerative changes, arthrokinematic restrictions, and impairments in strength and neuromuscular control, to treat the mechanical and functional deficits of CAI. However, according to the paradigm of Hiller et al,10 perceived instability plays an equal role in the long-term deficits and potential decrease in physical activity that often occur in patients with CAI. Therefore, obtaining the patient's perspective can help in assessing the effectiveness of the treatment on perceived ankle-joint function, overall feelings of stability, and general quality of life.11
Arnold et al12 reported that individuals with CAI had a decreased health-related quality of life (HRQOL) because of their functional limitations. Those with a history of ankle sprain not only had functional limitations but also a heightened fear of reinjury.13 A heightened fear of reinjury, avoidance of activity, or a disability can lead to decreased physical activity.14,15 Assessing local, global, and fear-of-reinjury outcomes in individuals with CAI is critical to understanding the effectiveness of clinical interventions.13 Therefore, the purpose of our study was to assess patient-reported outcomes after a balance-training protocol (BTP), strength-training protocol (STP), or control (sham) protocol (CON) among participants with CAI.
METHODS
Participants
Participants were 39 volunteers with CAI. We presented the participants' demographics and the flow diagram, inclusion and exclusion criteria, CAI status, and physical activity levels in part I of this study.16 All participants provided written informed consent, and the research was approved by Indiana University's Institutional Review Board for the Protection of Human Subjects.
Procedures
All questionnaires were completed using online survey software (Qualtrics, Provo, UT). Time to complete all questionnaires ranged from 10 to 20 minutes. We assessed global patient-reported outcomes using the Disablement in the Physically Active Scale (DPA) and fear of reinjury using the Fear-Avoidance Beliefs Questionnaire (FABQ). Regional ankle function was measured using the Foot and Ankle Ability Measure (FAAM) and a visual analog scale (VAS) for perceived ankle instability. Participants completed the questionnaires at baseline (pretest) and 6 weeks posttest.
Disablement in the Physically Active Scale
The DPA is a 16-item global-outcome instrument designed by athletic trainers for physically active individuals. This multidimensional scale is based on current disablement and HRQOL paradigms.17 Scores for each item are on a 5-point Likert scale, with the anchors of 1 (no problem) and 5 (severe). After the recommended subtraction of 16 points,18 overall scores for the DPA range from 0 to 64, with higher scores indicating increased disablement. This instrument has good test-retest reliability (intraclass correlation coefficient [ICC] = 0.94),18 the minimal detectable change (MDC) is 4.2, and the minimal clinically important difference (MCID) is 9.0 points.18
Fear-Avoidance Beliefs Questionnaire
The FABQ is a 16-item questionnaire (11 scored items)19 designed to assess fear-avoidance beliefs postinjury.20 Scores for each item are based on a 7-point Likert scale, with the anchors of 0 (completely disagree) and 6 (completely agree). The overall score for the FABQ ranges from 0 to 66, with a higher score indicating increased fear-avoidance beliefs.19 This questionnaire has demonstrated high test-retest reliability (ICC = 0.77 for the Physical Activity scale and ICC = 0.90 for the Work scale).20
Foot and Ankle Ability Measure
The FAAM is a questionnaire with 21-item activities of daily living (ADL; FAAM-ADL) and 8-item sport (FAAM-Sport) subscales. Each item is scored on a 5-point Likert scale anchored by 0 (unable to do) and 4 (no difficulty at all).21 The FAAM-ADL subscale scores range from 0 to 84, and the FAAM-Sport subscale scores range from 0 to 32. These scores are transformed into standardized percentages based on the questions applicable to the participant. A higher score represents a higher level of function for each subscale. At the end of each subscale, participants are also instructed to rate their function from 0% to 100%. Zero percent indicates the inability to perform ADL or sports tasks, whereas 100% indicates a preinjury level of function. Both the FAAM-ADL and -Sport subscales have good test-retest reliability (ICC [2,1] = 0.89 and 0.87, respectively).22 Researchers22 have determined that the MDC and MCID values for the FAAM-ADL are 5.7% and 8.0%, respectively. The MDC and MCID values for the FAAM-Sport are 12.3% and 9.0%, respectively.22
Visual Analog Scale
For the VAS, participants were instructed to rate their overall perceived ankle instability at that moment by sliding the scale from 0 to 100. The VAS is commonly used for pain and has high validity and good test-retest reliability (ICC = 0.97).23 The VAS for perceived ankle instability is also valid in identifying individuals with CAI.24 Investigators25–27 have reported that the MCID on the VAS is an 11- to 20-mm change in pain severity.
Rehabilitation Procedures
Each participant was randomly assigned to 1 of 3 groups: BTP, STP, or CON. This study was part of a larger study, and the procedures for each protocol have been described in detail.16 Each participant met with a researcher (E.A.H.) 3 times each week for 6 weeks for his or her protocol.
Statistical Analysis
A multivariate repeated-measures analysis of variance was conducted for the dependent variables: DPA, FABQ, FAAM-ADL, FAAM-Sport, and VAS. On findings that were different, follow-up univariate analyses were performed for each dependent variable. The analysis consisted of 1 within-subjects factor (time at 2 levels: pretest, posttest) and 1 between-subjects factor (group at 3 levels: BTP, STP, CON). Finally, we calculated the MDC score with 95% confidence interval (MDC95%) and mean difference. The MDC95% equation is 1.96 × standard error of measurement ×  .28,29 The standard error of measurement was calculated by multiplying the pooled standard deviation from the CON group by
.28,29 The standard error of measurement was calculated by multiplying the pooled standard deviation from the CON group by 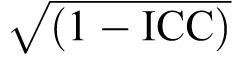 .29 The ICC used was the reliability estimate for each questionnaire.18,20,22,23 The α level was set a priori at .05. We used SPSS (version 23; IBM Corp, Armonk, NY) to analyze the statistics.
.29 The ICC used was the reliability estimate for each questionnaire.18,20,22,23 The α level was set a priori at .05. We used SPSS (version 23; IBM Corp, Armonk, NY) to analyze the statistics.
RESULTS
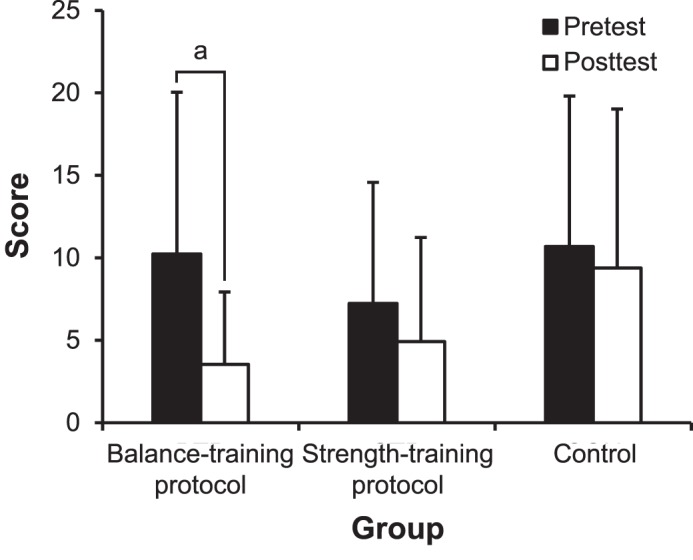
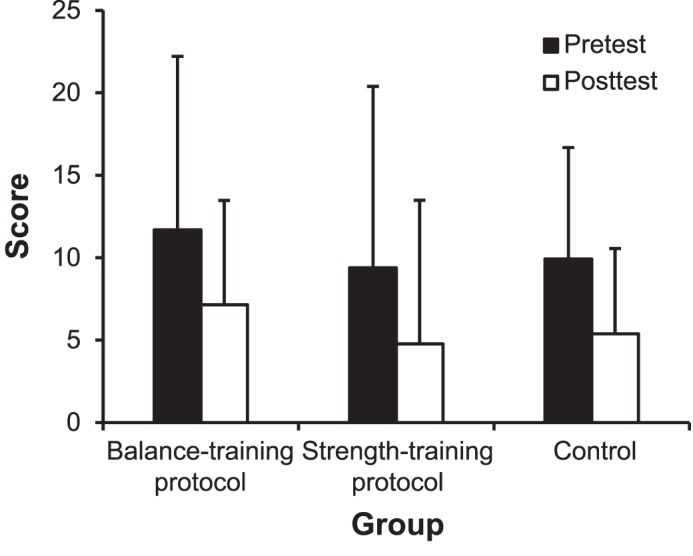
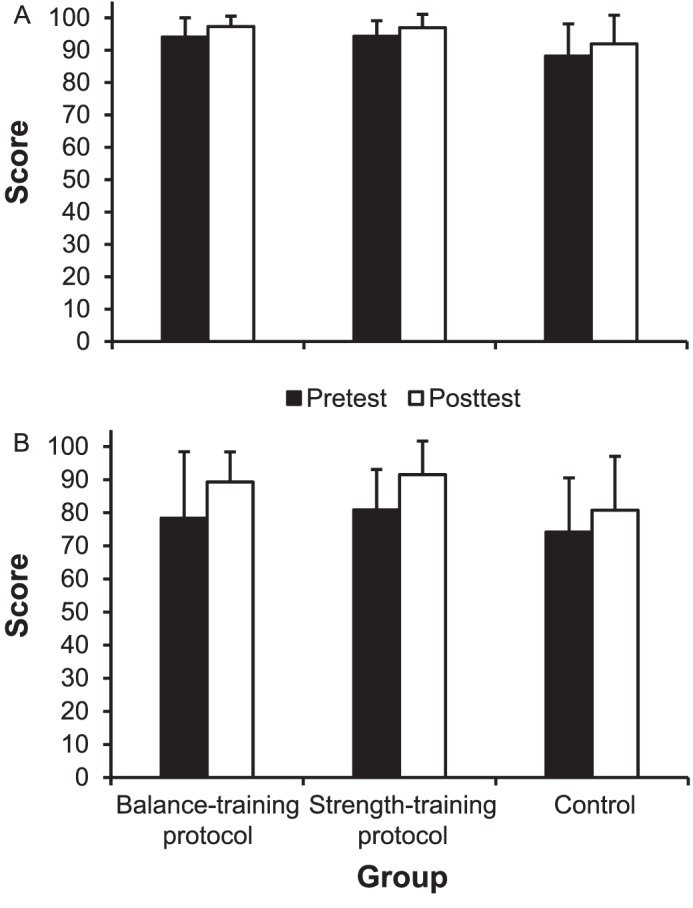
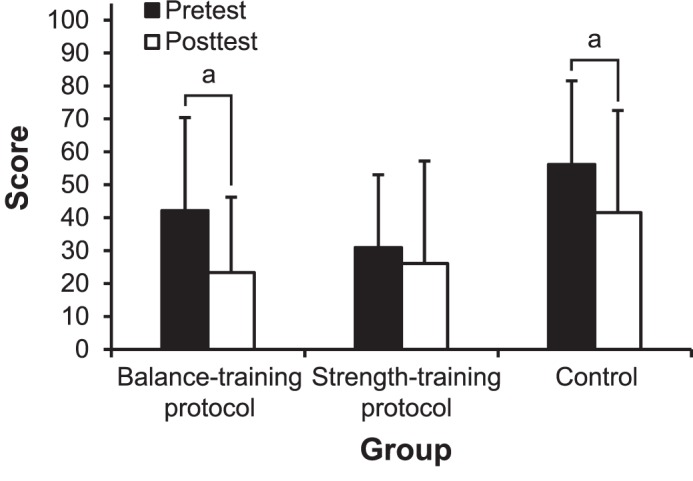
The multivariate analysis of variance with repeated measures did not reveal a time-by-group interaction (P = .78, η2 = 0.09). However, we observed a main effect for time (P = .001, η2 = 0.49). Follow-up univariate analyses revealed differences between pretest and posttest for each measure: DPA (P = .02, η2 = 0.15; Figure 1), FABQ (P = .001, η2 = 0.27; Figure 2), FAAM-ADL (P = .003, η2 = 0.22; Figure 3A), FAAM-Sport (P = .001, η2 = 0.36; Figure 3B), and VAS (P = .008, η2 = 0.18; Figure 4). In each measure, all participants, regardless of group, improved from pretest to posttest. The comparisons of the MDCs and mean differences are presented in the Table.
Figure 1.
Bar graph of the Disablement in the Physically Active questionnaire representing the average ± standard deviation scores in each group between the pretest and posttest. A higher score indicates a greater disability. a Exceeded the minimal detectable change.
Figure 2.
Bar graph of the Fear-Avoidance Beliefs Questionnaire representing the average ± standard deviation scores in each group between the pretest and posttest. A higher score indicates a greater fear of reinjury.
Figure 3.
Bar graph of the Foot and Ankle Ability Measure, A, Activities of Daily Living and, B, Sport subscales representing the average ± standard deviation scores in each group between the pretest and posttest. A lower score indicates a lower level of function.
Figure 4.
Bar graph of the visual analog scale for perceived instability representing the average ± standard deviation scores in each group between pretest and posttest. A higher score indicates greater instability. a Exceeded the minimal detectable change.
Table.
Comparison of the 95% Minimal Detectable Change Score and the Mean Difference
| Questionnaire |
Group |
Mean Difference |
95% Minimal Detectable Change Scorea |
| Disablement in the Physically Active | BTP | 6.69b | 6.37 |
| STP | 2.31 | ||
| Control | 1.31 | ||
| Fear-Avoidance Beliefs | BTP | 4.54 | 5.28 |
| STP | 4.61 | ||
| Control | 4.54 | ||
| Foot and Ankle Ability Measure | |||
| Activities of Daily Living subscale | BTP | 3.24 | 8.66 |
| STP | 2.64 | ||
| Control | 3.79 | ||
| Sport subscale | BTP | 10.94 | 16.32 |
| STP | 10.65 | ||
| Control | 6.59 | ||
| Visual analog scale | BTP | 18.84b | 13.61 |
| STP | 4.84 | ||
| Control | 14.61b | ||
Abbreviations: BTP, balance-training protocol; STP, strength-training protocol.
Calculated as 1.96 × standard error of measurement ×  .
.
Indicates that the mean difference exceeded the 95% minimal detectable change.
DISCUSSION
Our results indicated that, regardless of intervention group, patient-reported outcomes improved from pretest to posttest. To our knowledge, we are the first to use a sham intervention in a randomized controlled trial of ankle rehabilitation. For this study, our CON participants completed a 20-minute bicycle workout at mild to moderate intensity. The purpose of the sham treatment was to bring the CON participants into the laboratory to learn how simple patient interaction might provide a perceived benefit. Commonly used in pharmacologic and therapeutic modality studies,30–32 sham-controlled trials are beneficial for determining if the effect of the intervention is superior to the sham treatment. Participants were informed that they were in the bicycle group, and if they asked the investigator about the effectiveness of the protocol, they were told that continuous passive motion on the bicycle might affect the dependent variables.
Authors of previous rehabilitation studies33–37 have incorporated more patient-oriented outcome measures based on the guidelines of McKeon et al.38 However, many researchers have included only regional questionnaires in their rehabilitation studies33–37 without examining the global and psychological constraints as Houston et al13 recommended. Houston et al13 reported global, regional, and psychological HRQOL deficits in participants with CAI. We followed this recommendation13 and used the same questionnaires: the DPA for the global outcome, the FAAM-ADL and -Sport subscales for the regional outcomes, the VAS for perceived ankle instability, and the FABQ for the psychological outcome. Investigators have found improvements in scores on the FAAM and other region-specific questionnaires, but either their comparison was with a CON group that pursued no intervention33–36 or no CON group was included.37 Our study was unique because we included the CON group.
Evaluation of the MDC also provided an interesting opportunity to interpret the clinical meaningfulness of the change from pretest to posttest in each group. The change from pretest to posttest in the BTP group exceeded the MDC for both the DPA (mean difference = 6.69; MDC95% = 6.37) and the VAS (mean difference = 18.84; MDC95% = 13.61). The mean difference from pretest to posttest of the CON group also exceeded the MDC for the VAS. None of the groups exceeded the MDC for the FABQ or FAAM-ADL and -Sport subscales. Our MDC95% values were generally greater than those reported in previous research because we calculated the MDC95% based on our CON group's pooled standard deviation from the pretest and posttest. Our CON group had a greater standard deviation that affected the MDC because the intervention of a mild to moderately strenuous bicycle workout improved outcomes compared with doing nothing. Changes in patient-reported outcomes should be used as only one of many factors in measuring improvements after a rehabilitation protocol. Some improvement may represent a subtle change in the participant's abilities; therefore, even if a change does not reach the level of the MDC, it may still be an important milestone to document when making progression decisions.
To our knowledge, we are the first to evaluate the DPA after a rehabilitation protocol. We identified clinically meaningful improvements from pretest to posttest in the BTP group. The DPA is an HRQOL questionnaire that evaluates the patient's physical and emotional wellbeing. It also determines the level of disablement that the patient's injury has on physical activity.17 Whereas the STP and CON groups did not achieve clinically meaningful improvements according to the MDC, we still observed improvements, as indicated by the multivariate analysis of variance. This suggests that all groups improved in global function over time on the DPA.
Researchers13 have determined that individuals with CAI have a heightened fear of reinjury when assessed using the FABQ. Therefore, providing an intervention that could decrease the fear of reinjury would be beneficial for the participant to return to physical activity. Based on the mean differences between pretest and posttest, all participants experienced decreases in their fear of ankle reinjury by an average score of 4.6 after all interventions. Although our values did not exceed the MDC of 5.28, the improvement is important because, if the goal is to decrease the patient's fear in a rehabilitation program, then providing any intervention will be beneficial. Investigators should continue to use the FABQ when assessing psychological outcomes after injury and throughout the rehabilitation process.
The FAAM-ADL subscale scores showed small improvements (2.6% to 3.3%) in all groups after the 6-week intervention period. These limited improvements may be attributed to the higher level of function of our participants at baseline. The average baseline for all 3 groups was 92.2%, compared with 78.3% in a previous study.37 However, on the FAAM-Sport subscale, our BTP and STP groups had average improvements of 10.9% and 10.7%, respectively. These scores are similar to the results of Wright et al,36 who found 12.1% and 6.0% improvements after wobble-board and resistance-tubing training, respectively. Our CON group also had a 6.6% improvement after the 6-week intervention. Therefore, the bicycle workout appeared to be an effective intervention for improving the patients' perceptions of regional ankle function. No group exceeded the MDC to demonstrate clinical meaningfulness, but all groups improved statistically.
When evaluating the mean differences, we noted the VAS for perceived ankle instability was lower after the BTP. Thus, participants believed they were more stable after the BTP intervention. Researchers34 examining the VAS after 2 strength-training programs found improvements compared with a CON group that received no intervention. In that study, the CON group stayed the same from pretest to posttest, whereas our CON group using the bicycle intervention had some improvement. A possible explanation for the improvement in our CON group was that the continuous passive motion resulted in patients self-assessing functional improvement.
The improvement in our CON group implies a benefit from continuous passive motion at the ankle. Høiness et al39 found improvements in functional performance, strength, and subjective function in participants with residual ankle instability after high-intensity bicycle training. However, the pedal used was bidirectional, tilting 20° in the frontal plane.39 When unidirectional (sagittal-plane motion) bicycle training was used, no improvement in subjective function was reported.39 Our participants performed motion only in the unidirectional sagittal plane, but improvements occurred in global disability, regional ankle function, fear avoidance, and perceived instability. Based on our results, incorporating a 20-minute bicycle warm-up in a rehabilitation protocol may be beneficial. Researchers should further investigate the effect of bicycling or other low-complexity programs on patient-reported outcome measures.
LIMITATIONS
A limitation to our study was the lack of validity between the online questionnaire and the original format of each questionnaire. We also did not counterbalance the order of the questionnaires. Another limitation was the small sample size, which could have contributed to the lack of interaction between time and study group. Investigators should determine long-term patient-reported outcomes after rehabilitation.
CONCLUSIONS
Statistically, all groups improved in global and regional HRQOL questionnaire scores after the 6-week intervention. Our results introduce an interesting phenomenon for patient-reported outcomes: regardless of the intervention, improvements in these variables could still occur. However, when we further evaluated the mean differences from pretest to posttest, the BTP resulted in meaningful improvements on both global and regional questionnaires. Clinicians should compare patient-reported outcomes with clinical and laboratory measures to obtain a more complete picture of progression during rehabilitation. To improve both global and regional patient-reported outcomes, rehabilitation protocols should incorporate the entire lower extremity and not just the ankle.
REFERENCES
- 1.Yeung MS, Chang KM, So CH, Yuan WY. An epidemiological survey on ankle sprain. Br J Sports Med. 1994;28(2):112–116. doi: 10.1136/bjsm.28.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tanen L, Docherty CL, Van Der Pol B, Simon J, Schrader J. Prevalence of chronic ankle instability in high school and Division I athletes. Foot Ankle Spec. 2014;7(1):37–44. doi: 10.1177/1938640013509670. [DOI] [PubMed] [Google Scholar]
- 3.Donahue M, Simon J, Docherty CL. Critical review of self-reported functional ankle instability measures. Foot Ankle Int. 2011;32(12):1140–1146. doi: 10.3113/FAI.2011.1140. [DOI] [PubMed] [Google Scholar]
- 4.McKay G, Goldie P, Payne W, Oakes B, Watson L. A prospective study of injuries in basketball: a total profile and comparison by gender and standard of competition. J Sci Med Sport. 2001;4(2):196–211. doi: 10.1016/s1440-2440(01)80030-x. [DOI] [PubMed] [Google Scholar]
- 5.Löfvenberg R, Kärrholm J, Lund B. The outcome of nonoperated patients with chronic lateral instability of the ankle: a 20-year follow-up study. Foot Ankle Int. 1994;15(4):165–169. doi: 10.1177/107110079401500401. [DOI] [PubMed] [Google Scholar]
- 6.Gribble PA, Bleakley CM, Caulfield BM, et al. 2016 consensus statement of the International Ankle Consortium: prevalence, impact and long-term consequences of lateral ankle sprains. Br J Sports Med. 2016;50(24):1493–1495. doi: 10.1136/bjsports-2016-096188. [DOI] [PubMed] [Google Scholar]
- 7.Hertel J. Sensorimotor deficits with ankle sprains and chronic ankle instability. Clin Sports Med. 2008;27(3):353–370. doi: 10.1016/j.csm.2008.03.006. vii. [DOI] [PubMed] [Google Scholar]
- 8.Hubbard TJ, Kramer LC, Denegar CR, Hertel J. Correlations among multiple measures of functional and mechanical instability in subjects with chronic ankle instability. J Athl Train. 2007;42(3):361–366. [PMC free article] [PubMed] [Google Scholar]
- 9.Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train. 2002;37(4):364–375. [PMC free article] [PubMed] [Google Scholar]
- 10.Hiller CE, Kilbreath SL, Refshauge KM. Chronic ankle instability: evolution of the model. J Athl Train. 2011;46(2):133–141. doi: 10.4085/1062-6050-46.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wikstrom EA, Hubbard-Turner T, McKeon PO. Understanding and treating lateral ankle sprains and their consequences: a constraints-based approach. Sports Med. 2013;43(6):385–393. doi: 10.1007/s40279-013-0043-z. [DOI] [PubMed] [Google Scholar]
- 12.Arnold BL, Wright CJ, Ross SE. Functional ankle instability and health-related quality of life. J Athl Train. 2011;46(6):634–641. doi: 10.4085/1062-6050-46.6.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Houston MN, Van Lunen BL, Hoch MC. Health-related quality of life in individuals with chronic ankle instability. J Athl Train. 2014;49(6):758–763. doi: 10.4085/1062-6050-49.3.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beynnon BD, Vacek PM, Murphy D, Alosa D, Paller D. First-time inversion ankle ligament trauma: the effects of sex, level of competition, and sport on the incidence of injury. Am J Sports Med. 2005;33(10):1485–1491. doi: 10.1177/0363546505275490. [DOI] [PubMed] [Google Scholar]
- 15.Finch C, Owen N, Price R. Current injury or disability as a barrier to being more physically active. Med Sci Sports Exerc. 2001;33(5):778–782. doi: 10.1097/00005768-200105000-00016. [DOI] [PubMed] [Google Scholar]
- 16.Hall EA, Chomistek AK, Kingma JJ, Docherty CL. Balance- and strength-training protocols to improve chronic ankle instability deficits, part I: assessing clinical outcome measures. J Athl Train. 2018;53(6):568–577. doi: 10.4085/1062-6050-385-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vela LI, Denegar C. Transient disablement in the physically active with musculoskeletal injuries, part I: a descriptive model. J Athl Train. 2010;45(6):615–629. doi: 10.4085/1062-6050-45.6.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vela LI, Denegar CR. The Disablement in the Physically Active Scale, part II: the psychometric properties of an outcomes scale for musculoskeletal injuries. J Athl Train. 2010;45(6):630–641. doi: 10.4085/1062-6050-45.6.630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A. Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52(2):157–168. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 20.Jacob T, Baras M, Zeev A, Epstein L. Low back pain: reliability of a set of pain measurement tools. Arch Phys Med Rehabil. 2001;82(6):735–742. doi: 10.1053/apmr.2001.22623. [DOI] [PubMed] [Google Scholar]
- 21.Carcia CR, Martin RL, Drouin JM. Validity of the Foot and Ankle Ability Measure in athletes with chronic ankle instability. J Athl Train. 2008;43(2):179–183. doi: 10.4085/1062-6050-43.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martin RL, Irrgang JJ, Burdett RG, Conti SF, Van Swearingen JM. Evidence of validity for the Foot and Ankle Ability Measure (FAAM) Foot Ankle Int. 2005;26(11):968–983. doi: 10.1177/107110070502601113. [DOI] [PubMed] [Google Scholar]
- 23.Bijur PE, Silver W, Gallagher EJ. Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med. 2001;8(12):1153–1157. doi: 10.1111/j.1553-2712.2001.tb01132.x. [DOI] [PubMed] [Google Scholar]
- 24.Hiller CE, Refshauge KM, Bundy AC, Herbert RD, Kilbreath SL. The Cumberland Ankle Instability Tool: a report of validity and reliability testing. Arch Phys Med Rehabil. 2006;87(9):1235–1241. doi: 10.1016/j.apmr.2006.05.022. [DOI] [PubMed] [Google Scholar]
- 25.Todd KH, Funk KG, Funk JP, Bonacci R. Clinical significance of reported changes in pain severity. Ann Emerg Med. 1996;27(4):485–489. doi: 10.1016/s0196-0644(96)70238-x. [DOI] [PubMed] [Google Scholar]
- 26.Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP) Arthritis Care Res (Hoboken) 2011;63(suppl 11):S240–S252. doi: 10.1002/acr.20543. [DOI] [PubMed] [Google Scholar]
- 27.Stauffer ME, Taylor SD, Watson DJ, Peloso PM, Morrison A. Definition of nonresponse to analgesic treatment of arthritic pain: an analytical literature review of the smallest detectable difference, the minimal detectable change, and the minimal clinically important difference on the pain visual analog scale. Int J Inflam. 2011;2011:231926. doi: 10.4061/2011/231926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Donoghue D, Stokes EK. How much change is true change? The minimum detectable change of the Berg Balance Scale in elderly people. J Rehabil Med. 2009;41(5):343–346. doi: 10.2340/16501977-0337. [DOI] [PubMed] [Google Scholar]
- 29.Schwenk M, Gogulla S, Englert S, Czempik A, Hauer K. Test-retest reliability and minimal detectable change of repeated sit-to-stand analysis using one body fixed sensor in geriatric patients. Physiol Meas. 2012;33(11):1931–1946. doi: 10.1088/0967-3334/33/11/1931. [DOI] [PubMed] [Google Scholar]
- 30.Bjordal JM, Johnson MI, Iversen V, Aimbire F, Lopes-Martins RA. Low-level laser therapy in acute pain: a systematic review of possible mechanisms of action and clinical effects in randomized placebo-controlled trials. Photomed Laser Surg. 2006;24(2):158–168. doi: 10.1089/pho.2006.24.158. [DOI] [PubMed] [Google Scholar]
- 31.Bjordal JM, Johnson MI, Lopes-Martins RA, Bogen B, Chow R, Ljunggren AE. Short-term efficacy of physical interventions in osteoarthritic knee pain: a systematic review and meta-analysis of randomised placebo-controlled trials. BMC Musculoskelet Disord. 2007;8:51. doi: 10.1186/1471-2474-8-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gemmell H, Hilland A. Immediate effect of electric point stimulation (TENS) in treating latent upper trapezius trigger points: a double blind randomised placebo-controlled trial. J Bodyw Mov Ther. 2011;15(3):348–354. doi: 10.1016/j.jbmt.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 33.Hale SA, Hertel J, Olmsted-Kramer LC. The effect of a 4-week comprehensive rehabilitation program on postural control and lower extremity function in individuals with chronic ankle instability. J Orthop Sports Phys Ther. 2007;37(6):303–311. doi: 10.2519/jospt.2007.2322. [DOI] [PubMed] [Google Scholar]
- 34.Hall EA, Docherty CL, Simon J, Kingma JJ, Klossner JC. Strength-training protocols to improve deficits in participants with chronic ankle instability: a randomized controlled trial. J Athl Train. 2015;50(1):36–44. doi: 10.4085/1062-6050-49.3.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McKeon PO, Ingersoll CD, Kerrigan DC, Saliba E, Bennett BC, Hertel J. Balance training improves function and postural control in those with chronic ankle instability. Med Sci Sports Exerc. 2008;40(10):1810–1819. doi: 10.1249/MSS.0b013e31817e0f92. [DOI] [PubMed] [Google Scholar]
- 36.Wright CJ, Linens SW, Cain MS. A randomized controlled trial comparing rehabilitation efficacy in chronic ankle instability. J Sport Rehabil. 2017;26(4):238–249. doi: 10.1123/jsr.2015-0189. [DOI] [PubMed] [Google Scholar]
- 37.Hoch MC, Andreatta RD, Mullineaux DR, et al. Two-week joint mobilization intervention improves self-reported function, range of motion, and dynamic balance in those with chronic ankle instability. J Orthop Res. 2012;30(11):1798–1804. doi: 10.1002/jor.22150. [DOI] [PubMed] [Google Scholar]
- 38.McKeon PO, McKeon JM, Mattacola CG, Lattermann C. Finding context: a new model for interpreting clinical evidence. Athl Ther Today. 2011;16(5):10–13. [Google Scholar]
- 39.Høiness P, Glott T, Ingjer F. High-intensity training with a bi-directional bicycle pedal improves performance in mechanically unstable ankles: a prospective randomized study of 19 subjects. Scand J Med Sci Sports. 2003;13(4):266–271. doi: 10.1034/j.1600-0838.2003.10140.x. [DOI] [PubMed] [Google Scholar]


