Abstract
Aims
To estimate short-term mortality rates for individuals with type 1 or type 2 diabetes diagnosed before age 20 years from the SEARCH for Diabetes in Youth study.
Methods
We included 8358 individuals newly-diagnosed with type 1 (n=6840) or type 2 (n= 1518) diabetes from 1/1/2002–12/31/2008. We searched the National Death Index through 12/31/2010. We calculated standardized mortality ratios (SMRs) as observed divided by expected numbers of deaths based on age, sex, and race for the comparable US population in the geographic areas of the SEARCH study.
Results
Mean age at diabetes diagnosis was 10.7 years. During 44,893 person-years (PY) of observation (median follow-up=5.3 years), 41 individuals died (91.3 deaths/100,000 PY); 26 with type 1 (70.6 deaths/100,000 PY) and 15 with type 2 (185.6 deaths/100,000 PY) diabetes. The expected mortality rate was 70.9 deaths/100,000 PY. The overall SMR (95% CI) was 1.3 (1.0, 1.8) and was high among individuals with type 2 diabetes 2.4 (1.3, 3.9), females 2.2 (1.3, 3.3), 15–19 year olds 2.7 (1.7–4.0), and non-Hispanic blacks 2.1 (1.2, 3.4).
Conclusions
Compared to the state populations of similar age, sex, and race, our results show excess mortality in individuals with type 2 diabetes, females, older youth, and non-Hispanic blacks. We did not observe excess short-term mortality in individuals with type 1 diabetes. Studies of longer-term mortality in individuals with youth-onset diabetes are warranted.
Keywords: Type 1 Diabetes, Type 2 Diabetes, Mortality, Epidemiology, Youth
1. Introduction
Population-based studies in the US and territories,1–4 as well as other countries 5–13 have reported increased mortality for individuals with youth-onset type 1 diabetes compared to the general population, with standardized mortality ratios (SMRs) varying from 1.7 to 12.9 5, 8. Although few studies have evaluated mortality risk among individuals with youth-onset type 2 diabetes, it has been suggested that their mortality experience is worse than the general population and worse than those with youth-onset type 1 diabetes.7, 14
There is a paucity of data from contemporary populations in the US that can be used to identify people with youth-onset diabetes and evaluate their mortality risk. Most published studies have been limited to persons with type 1 diabetes. Further, few studies have examined cause-specific mortality among youth-onset type 2 diabetes. Using data from the SEARCH for Diabetes in Youth (SEARCH) study, we sought to estimate all-cause and cause-specific mortality in individuals with incident type 1 and type 2 diabetes diagnosed before 20 years of age (“youth-onset”) and to determine if the short-term mortality experience among SEARCH study participants differs from that of the comparable US population in the geographic areas of the SEARCH study.
2. Participants
SEARCH is a multicenter, population-based observational study of youth with incident diabetes who are followed longitudinally. A detailed description of study methods has been published.15 In brief, incident cases of physician-diagnosed diabetes in individuals aged <20 years were identified beginning in 2002. Diabetes type is based on physician report around the time of diabetes and categorized as type 1 (including type 1, type 1a, or type 1b) and type 2 diabetes. Cases were ascertained from geographically defined populations at sites in Ohio, Colorado, South Carolina and Washington, among enrollees in one health plan in California (Kaiser Permanente Southern California), and among Indian Health Service beneficiaries from American Indian populations in Arizona and New Mexico. Cases were identified through networks of pediatricians and endocrinologists, other healthcare providers, hospitals, community health centers, and health plans.Eligible cases were registered anonymously with the coordinating center at the Wake Forest School of Medicine. Case ascertainment has been >90% for both type 1 and type 2 diabetes for the duration of the study.15, 16
Local institutional review boards with jurisdiction over local study populations approved the study.
3. Materials and Methods
3.1 Mortality ascertainment
Vital status (living, deceased, unknown) and underlying and contributing causes of death were determined from linkages of all registered diabetes cases with the National Death Index (NDI) Plus database 17 from the date of diabetes diagnosis through 12/31/2010 unless cases were known to be alive on or after that date. Records where cases were known to be deceased were submitted to the NDI to obtain cause of death. NDI records were searched for all years for which vital status could not be confirmed. Deaths were verified by matching name, social security number (if available), date of birth, and sex. Death certificates and reports of deaths by immediate family members or healthcare providers were also considered definitive evidence of death.
Cause of death was derived from the NDI file and classified per International Classification Diseases, Tenth Revision (ICD-10). “Underlying cause of death” was used for cause-specific mortality. “Contributing cause of death” was used to identify deaths where diabetes was a significant condition contributing to death but not the underlying cause.
All 9213 individuals with incident type 1 or type 2 diabetes diagnosed between 1/1/2002 and 12/31/2008 were eligible for mortality surveillance. We excluded 855 (9.3%) cases because their vital status was unknown and we did not have sufficient individual-level data for NDI linkage, leaving 8358 for mortality surveillance. The excluded cases were older at diagnosis, more likely to have type 2 than type 1 diabetes and to be non-Hispanic black or of unknown race/ethnicity compared to cases who were known alive or whose data were submitted to the NDI.
3.2 Statistical Analysis
Person-years (PY) of follow-up were calculated from date of diabetes diagnosis to either 12/31/2010 or date of death, whichever occurred first. Age-, sex-, and race-standardized mortality rates were calculated using respective US state populations of the SEARCH study sites. Standardized mortality ratios (SMRs) were calculated as observed numbers of deaths in the SEARCH study divided by expected numbers of deaths based on age, sex, and race distributions for comparable US state populations of the study sites. For each year, we obtained population sizes and deaths in the corresponding US state populations from the Centers for Disease Control and Prevention (CDC) Wide-ranging Online Data for Epidemiologic Research (WONDER) online tool, which contains mortality and population counts for all US counties.18 Poisson regression was used to model death rates and calculate 95% confidence intervals (CIs). Cause-specific mortality rates were not calculated because the numbers of deaths were too small for reliable estimates. Statistical analyses were performed using SAS software, version 9.3 (SAS Institute, Cary, NC).
4. Results
Demographic characteristics of the 8358 SEARCH cases stratified by diabetes type are shown in Table 1. Follow-up time was similar among those with type 1 and type 2 diabetes.
Table 1.
Characteristics of the 8,358 Diabetes Cases in the SEARCH for Diabetes in Youth Study, Overall and by Type, 2002–2008
| Characteristics | Total (N=8,358) | Diabetes Type | |
|---|---|---|---|
| Type 1 (N=6,840) | Type 2 (N=1,518) | ||
| Age at diabetes diagnosis (years) | 10.7±4.7 | 9.8±4.5 | 14.7±2.8 |
| Age group at diagnosis (years), N (%) | |||
| 0–4 | 1228 (14.7) | 1224 (17.9) | 4 (0.3) |
| 5–9 | 2221 (26.6) | 2155 (31.5) | 66 (4.3) |
| 10–14 | 3230 (38.6) | 2517 (36.8) | 713 (47.0) |
| 15–19 | 1679 (20.1) | 944 (13.8) | 735 (48.4) |
| Sex, N (%) | |||
| Female | 4186 (50.1) | 3278 (47.9) | 908 (59.8) |
| Male | 4172 (49.9) | 3562 (52.1) | 610 (40.2) |
| Race/Ethnicity, N (%) | |||
| Non-Hispanic White | 5132 (61.4) | 4812 (70.4) | 320 (21.1) |
| Non-Hispanic Black | 1296 (15.5) | 781 (11.4) | 515 (33.9) |
| Hispanic | 1360 (16.3) | 908 (13.3) | 452 (29.8) |
| Other/Unknown | 570 (6.8) | 339 (5.0) | 231 (15.2) |
| Year of diagnosis, N (%) | |||
| 2002 | 1132 (13.5) | 924 (13.5) | 208 (13.7) |
| 2003 | 1087 (13.0) | 888 (13.0) | 199 (13.1) |
| 2004 | 1102 (13.2) | 910 (13.3) | 192 (12.6) |
| 2005 | 1196 (14.3) | 990 (14.5) | 206 (13.6) |
| 2006 | 1249 (14.9) | 1021 (14.9) | 228 (15.0) |
| 2007 | 1286 (15.4) | 1047 (15.3) | 239 (15.7) |
| 2008 | 1306 (15.6) | 1060 (15.5) | 246 (16.2) |
| Follow-up time from diagnosis, years* | 5.3 (0–9) | 5.3 (0–9) | 5.2 (0–9) |
| Age at death/censor (years) | 16.0±5.0 | 15.2± 4.9 | 20.0±3.5 |
| Age group at death/censor (years), N (%) | |||
| < 14 | 3449 (41.3) | 3328 (48.6) | 121 (8.0) |
| 15–19 | 2904 (34.7) | 2295 (33.6) | 609 (40.1) |
| 20–24 | 1795 (21.5) | 1121 (16.4) | 674 (44.4) |
| 25–29 | 210 (2.5) | 96 (1.4) | 114 (7.5) |
Data are means ± standard deviation, N (%), or median (range), as appropriate.
Time is from diabetes diagnosis to death or censoring on 12/31/2010.
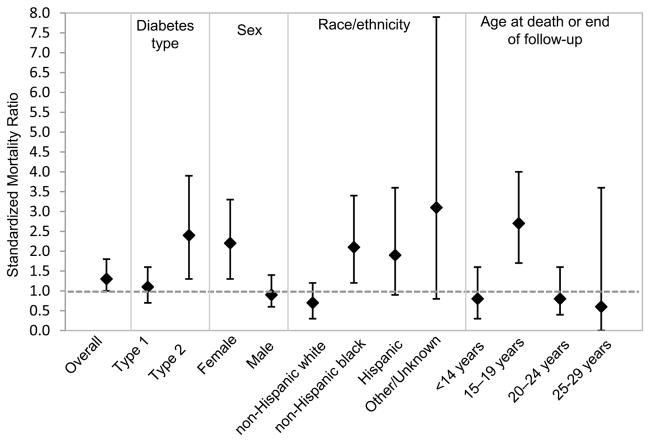
During a median follow-up of 5.3 years (44,893 PY of observation), 41 deaths occurred (crude rate of 91.3 deaths/100,000 PY); 26 with type 1 (70.6 deaths/100,000 PY) and 15 with type 2 diabetes (185.6 deaths/100,000 PY) (Table 2). The expected mortality rate was 70.9 deaths/100,000 PY. Mortality for all groups combined was slightly higher than that of the comparable age-, sex-, and race-specific US state populations of the SEARCH study sites (SMR=1.3, 95% CI=1.0, 1.8), and was not statistically significant (p=0.08) (Figure 1). Mean (SD) age at death among individuals with type 1 and type 2 diabetes was 15.2 (4.9) and 20.0 (3.5) years, respectively. The crude mortality rate was higher for type 2 versus type 1 diabetes. Compared to the US state populations, mortality in the SEARCH study was significantly higher than expected for individuals with type 2 diabetes (SMR=2.4, 95% CI=1.3, 3.9; p=0.001) but not for individuals with type 1 diabetes (SMR=1.1, 95% CI=0.7, 1.6; p=0.84) (Figure 1). Females had higher mortality rates than males, and non-Hispanic Blacks and Hispanics had higher mortality rates than non-Hispanic whites. Individuals aged 15–19 years at the time of death had the highest mortality rates compared to other age groups (Table 2). No deaths occurred among the 320 non-Hispanic whites with type 2 diabetes (data not shown). Compared to the US state populations, mortality in the SEARCH study was significantly higher than expected for females (SMR=2.2, 95% CI=1.3, 3.3; p<0.001), non-Hispanic blacks (SMR=2.1, 95% CI=1.2, 3.4; p=0.004) and those aged 15–19 years (SMR=2.7, 95% CI=1.7, 4.0; p<0.001) at the time of death or end of follow-up (Figure 1).
Table 2.
Crude Mortality Rates among 8,358 Diabetes Cases in the SEARCH for Diabetes in Youth Study, 2002–2008 and the 2014 Comparable State Populations
| Number of Deaths | Crude Mortality Rate | ||||
|---|---|---|---|---|---|
| Number of Person-Years | Observed | Expected | SEARCH* | US* | |
|
| |||||
| Overall | 44,893 | 41 | 31 | 91.3 | 70.9 |
|
| |||||
| Diabetes type | |||||
|
| |||||
| Type 1 | 36,810 | 26 | 25 | 70.6 | 70.9 |
|
| |||||
| Type 2 | 8,083 | 15 | 6 | 185.6 | 70.9 |
|
| |||||
| Sex | |||||
|
| |||||
| Female | 22,489 | 22 | 10 | 97.8 | 48.1 |
|
| |||||
| Male | 22,404 | 19 | 21 | 84.8 | 91.8 |
|
| |||||
| Race/Ethnicity | |||||
|
| |||||
| Non-Hispanic White | 27,766 | 12 | 17 | 43.2 | 63.9 |
|
| |||||
| Non-Hispanic Black | 6,897 | 16 | 8 | 232.0 | 127.9 |
|
| |||||
| Hispanic | 7,138 | 9 | 5 | 126.1 | 67.8 |
|
| |||||
| Other/Unknown | 3,091 | 4 | 1 | 129.4 | 46.3 |
|
| |||||
| Age at death/censor (years) | |||||
|
| |||||
| < 14 | 16,436 | 8 | 10 | 48.7 | 62.6 |
|
| |||||
| 15–19 | 15,481 | 23 | 9 | 148.6 | 58.3 |
|
| |||||
| 20–24 | 11,283 | 9 | 11 | 79.8 | 89.7 |
|
| |||||
| 25–29 | 1,693 | 1 | 2 | 59.1 | 87.4 |
per 100,000 person-years
Figure 1.
Age-, Sex-, and Race-Standardized Mortality Ratios Overall and by Diabetes Type, Sex, Race/Ethnicity, and Age at Death or End of Follow-up
Among decedents with type 1 diabetes, diabetes was the most frequent underlying cause of death followed by accidental injury and intentional self-harm (Table 3). Diabetes was listed as the contributing cause of death for 2 of the 26 deaths among individuals with type 1 diabetes. Using the underlying or contributing cause of death due to diabetes, 50% of deaths among those with type 1 diabetes were related to their diabetes. Among decedents with type 2 diabetes, the leading underlying cause of death was attributed to transport/motor vehicle accidents followed by accidental poisoning and intentional self-harm. Among individuals with type 2 diabetes, diabetes was not listed as contributing cause of death for any of the deaths but it was the underlying cause of death for 1 individual.
Table 3.
Underlying and Contributing Cause of Death by Diabetes Type among 8,358 Diabetes Cases in the SEARCH for Diabetes in Youth Study, 2002–2008
| Cause of Death | ICD-10 Code | Total No. (%) | Type 1 Diabetes No. (%) | Type 2 Diabetes No. (%) |
|---|---|---|---|---|
| Total number of deaths | 41 (100.0) | 26 (63.4) | 15 (36.6) | |
| Underlying cause of death | ||||
| Infection and parasitic disease | A00-B99 | 1 (2.4) | 0 | 1 (6.7) |
| Diseases of the blood | D50-D89 | 1 (2.4) | 0 | 1 (6.7) |
| Endocrine, nutritional and metabolic diseases | ||||
| Diabetes mellitus (DM) | E00-E69 | 12 (29.3) | 11 (42.3) | 1 (6.7) |
| Insulin-dependent DM, with ketoacidosis | E10.1 | 2 | 2 | 0 |
| Insulin-dependent DM, without complications | E10.9 | 1 | 1 | 0 |
| Unspecified DM, with coma | E14.0 | 1 | 0 | 1 |
| Unspecified DM, with ketoacidosis | E14.1 | 6 | 6 | 0 |
| Unspecified DM, without complications | E14.9 | 2 | 2 | 0 |
| Metabolic disorders | E70-E89 | 1 (2.4) | 1 (3.8) | 0 |
| Mental and behavioral disorders | F01-F99 | 1 (2.4) | 0 | 1 (6.7) |
| Diseases of the nervous system | G00-G98 | 3 (7.3) | 2 (7.7) | 1 (6.7) |
| Diseases of the circulatory system | I00-I99 | 2 (4.9) | 1 (3.8) | 1 (6.7) |
| Diseases of the respiratory system | J00-J98 | 2 (4.9) | 2 (7.7) | 0 |
| Diseases of the digestive system | K00-K92 | 0 | 0 | 0 |
| Pregnancy, childbirth and puerperium | O00-O99 | 0 | 0 | 0 |
| Congenital malformations | Q00-Q99 | 0 | 0 | 0 |
| External causes of morbidity and mortality | V00-Y89 | |||
| Transport/motor vehicle accidents | V13-V89 | 5 (12.2) | 2 (7.7) | 3 (20.0) |
| Other external causes of accidental injury | W00-X59 | 3 (7.3) | 3 (11.5) | 0 |
| Accidental poisoning | X40-X49 | 2 (4.9) | 0 | 2 (13.3) |
| Intentional self-harm | X60-X84 | 5 (12.2) | 3 (11.5) | 2 (13.3) |
| Sequelae of motor vehicle accident | Y85 | 1 (2.4) | 0 | 1 (6.7) |
| Unknown | 2 (4.9) | 1 (3.8) | 1 (6.7) | |
| Contributing cause of death | ||||
| Diabetes | E10-E14 | 2 (4.9) | 2 (7.7) | 0 |
| Underlying or contributing cause of death* | ||||
| Diabetes | E10-E14 | 14 (34.1) | 13 (50.0) | 1 (6.7) |
Underlying cause of death when diabetes mellitus is a contributing cause: Other external causes of accidental injury and Transport/motor vehicle accident
5. Discussion
In the SEARCH study, mortality for both types of diabetes together did not differ significantly from the comparable general US population in the geographic areas of the SEARCH study. However, compared to the general population, mortality was two-fold higher among those with type 2 diabetes, females, non-Hispanic Blacks, and those aged 15–19 years at the time of death.
We identified 41 deaths during 44,893 person-years (91.3 deaths/100,000 PY) of observation over a median follow-up of 5.3 years; 26 deaths occurred in youth-onset type 1 diabetes (70.6 deaths/100,000 PY) and 15 deaths occurred in youth-onset type 2 diabetes (185.6 deaths/100,000 PY). The mortality rates we observed were substantially lower than what has been reported in other studies in the US 1, 19 and many other countries.10 However, few studies have reported on short-term mortality risk in youth-onset diabetes and comparisons of our findings to previous studies should be made with caution, due to differences in methods, study populations (including type of diabetes, age at diagnosis, diabetes duration, and historical versus contemporary cohorts), and the background population mortality. During 7.8 years of follow-up in the Chicago Diabetes Registry of 1238 individuals with diabetes onset before age 18 between 1985–2000, 30 individuals were reported to have died (250 deaths/100,000 PY).1 In the population-based Western Australia Children’s Diabetes Database, mortality among individuals with type 1 diabetes diagnosed before age 18 between 1987–2011 was 74.5 deaths/100,000 PY during 7.6 years of follow-up.8 The lower mortality rates seen in the Western Australia Children’s Database and the SEARCH cohort could be due to a shorter duration of diabetes as well as the focus on more contemporary cohorts, which may have benefited from advances in diabetes treatment.
After a median 5.3 years of follow-up, we found that the crude mortality rate was higher for individuals with type 2 versus type 1 diabetes. Further, mortality for youth-onset type 2 diabetes was higher than expected compared to the similar age, sex, and race state populations of the SEARCH study sites. Several studies have suggested that youth-onset type 2 diabetes is associated with more severe chronic diabetes complications and greater mortality.7, 20–22 Over a median 21 years of follow-up in the Royal Prince Alfred Hospital Diabetes Clinical Database in Australia, the adjusted hazard ratio for mortality was two-fold higher in type 2 versus type 1 diabetes (diabetes onset between ages 15–30 years).7
Mortality was higher in females compared to males in the SEARCH study and higher than expected in females compared with the general population (SMR=2.2; 95% CI: 1.3, 3.3). Similarly, the Western Australian Children’s Diabetes Database study found that mortality for females with type 1 diabetes was 10 times that of the general population, while no statistically significant elevated mortality risk was observed in males 8. Similar observations have been reported from studies conducted in Japan 23, Europe 6, and the US;19 however, some studies have observed higher mortality in males compared to females.24 The higher SMR among females may reflect the death rate in the general population for this age group where young males have a two-fold higher death rate than females.
We found that mortality in non-Hispanic blacks in the SEARCH study was 2.1 times higher than the mortality in the similar age, sex, and race state populations of the SEARCH study sites. These findings are supported by other studies in the US and territories.1, 25, 26 We previously reported that a substantial proportion of non-Hispanic black youth with diabetes have adverse socioeconomic profiles,27 which may be associated with barriers to care and contribute to the increased mortality.
There are several limitations to our study. We could not conduct detailed cause-specific mortality analyses due to the small number of deaths. Therefore, although it is interesting to note that only one death was attributed to diabetes in those with youth-onset type 2 diabetes, we were unable to determine whether this is related to socioeconomic, psychosocial or other risk factors of acute deaths. The mortality estimates for youth-onset type 2 diabetes are based on a very small number of deaths over a very short time period and may not reflect the true mortality rates across the US. In addition, we could not ascertain vital status for 9.3% of the cohort. These individuals were older at diabetes diagnosis, more likely to have type 2 diabetes and to be non-Hispanic black; therefore, it is possible that our mortality findings are underestimated in these populations and the SMRs are higher than reported here. Further, we were unable to confirm cause of death through medical record review or death certificates. However, previous studies have demonstrated that the NDI is an accurate source for ascertaining vital status even in the absence of social security numbers. Sensitivity of the NDI ranges from 87% to 98% 28 and use of different combinations of personal identifiers can correctly identify 83% to 92% of decedents and 92% to 99% of living individuals.29 Strengths of our study include the large sample size and racial/ethnic and geographic diversity, which makes our findings generalizable, although not necessarily generalizable to the entire US. Moreover, SEARCH is a unique and valuable resource for conducting mortality surveillance since it includes individuals with youth-onset type 1 and type 2 diabetes. Few contemporary cohorts of incident type 1 and type 2 diabetes in children and young adults in the US are available; therefore, these results likely provide the most comprehensive and current estimates of the mortality experience of youth-onset diabetes in the US.
6. Conclusions
Among individuals with type 1 or type 2 diabetes, our results show excess short-term mortality risk in individuals with type 2 diabetes, non-Hispanic blacks, females and those aged 15–19 years compared to youth of similar age, sex, and race in the corresponding US states. We did not observe excess mortality in individuals with type 1 diabetes. Our findings begin to shed light on the epidemiology of short-term risk of mortality of youth-onset type 1 and type 2 diabetes in the US. A longer follow-up in this well-characterized and contemporary cohort would allow for further examination of cause-specific mortality outcomes, which could help in developing focused strategies aimed to increase survival in youth-onset diabetes.
Acknowledgments
The SEARCH for Diabetes in Youth Study is indebted to the many youth and their families, and their health care providers, whose participation made this study possible.
Funding: The SEARCH for Diabetes in Youth Cohort Study (1UC4DK108173-01) is funded by the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases and supported by the Centers for Disease Control and Prevention.
The Population Based Registry of Diabetes in Youth Study (RFP DP15-002) is funded by the Centers for Disease Control and Prevention and supported by the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases.
Sites: Kaiser Permanente Southern California (U18DP006133, U48/CCU919219, U01 DP000246, and U18DP002714), University of Colorado Denver (U18DP006139, U48/CCU819241-3, U01 DP000247, and U18DP000247-06A1), Cincinnati’s Children’s Hospital Medical Center (U18DP006134, U48/CCU519239, U01 DP000248, and 1U18DP002709), University of North Carolina at Chapel Hill (U18DP006138, U48/CCU419249, U01 DP000254, and U18DP002708), Seattle Children’s Hospital (U18DP006136, U58/CCU019235-4, U01 DP000244, and U18DP002710-01), Wake Forest University School of Medicine (U18DP006131, U48/CCU919219, U01 DP000250, and 200-2010-35171)
The authors wish to acknowledge the involvement of the South Carolina Clinical & Translational Research Institute, at the Medical University of South Carolina, NIH/National Center for Advancing Translational Sciences (NCATS) grant number UL1 TR001450; Seattle Children’s Hospital and the University of Washington, NIH/NCATS grant number UL1 TR00423; University of Colorado Pediatric Clinical and Translational Research Center, NIH/NCATS grant Number UL1 TR000154; the Barbara Davis Center at the University of Colorado at Denver (DERC NIH grant number P30 DK57516); the University of Cincinnati, NIH/NCATS grant number UL1 TR001425; and the Children with Medical Handicaps program managed by the Ohio Department of Health. This study includes data provided by the Ohio Department of Health, which should not be considered an endorsement of this study or its conclusions.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention and the National Institute of Diabetes and Digestive and Kidney Diseases.
Declarations of Interest. No potential conflicts of interest relevant to this article were reported.
Prior presentation. Parts of this study were presented as an abstract at the 75th Annual Scientific Sessions of the American Diabetes Association, 5–9 June 2015, in Boston, MA.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Burnet DL, Cooper AJ, Drum ML, Lipton RB. Risk factors for mortality in a diverse cohort of patients with childhood-onset diabetes in Chicago. Diabetes Care. 2007;30(10):2559–2563. doi: 10.2337/dc07-0216. [DOI] [PubMed] [Google Scholar]
- 2.Secrest AM, Becker DJ, Kelsey SF, LaPorte RE, Orchard TJ. All-cause mortality trends in a large population-based cohort with long-standing childhood-onset type 1 diabetes: the Allegheny County type 1 diabetes registry. Diabetes Care. 2010;33(12):2573–2579. doi: 10.2337/dc10-1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Washington RE, Orchard TJ, Arena VC, LaPorte RE, Secrest AM, Tull ES. All-cause mortality in a population-based type 1 diabetes cohort in the U.S. Virgin Islands. Diabetes Res Clin Pract. 2014;103(3):504–509. doi: 10.1016/j.diabres.2013.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dorman JS, Laporte RE, Kuller LH, et al. The Pittsburgh insulin-dependent diabetes mellitus (IDDM) morbidity and mortality study. Mortality results. Diabetes. 1984;33(3):271–276. doi: 10.2337/diab.33.3.271. [DOI] [PubMed] [Google Scholar]
- 5.Asao K, Sarti C, Forsen T, et al. Long-term mortality in nationwide cohorts of childhood-onset type 1 diabetes in Japan and Finland. Diabetes Care. 2003;26(7):2037–2042. doi: 10.2337/diacare.26.7.2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bruno G, Cerutti F, Merletti F, et al. Short-term mortality risk in children and young adults with type 1 diabetes: the population-based Registry of the Province of Turin, Italy. Nutr Metab Cardiovasc Dis. 2009;19(5):340–344. doi: 10.1016/j.numecd.2008.03.010. [DOI] [PubMed] [Google Scholar]
- 7.Constantino MI, Molyneaux L, Limacher-Gisler F, et al. Long-Term Complications and Mortality in Young-Onset Diabetes: Type 2 diabetes is more hazardous and lethal than type 1 diabetes. Diabetes Care. 2013 doi: 10.2337/dc12-2455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cooper MN, de Klerk NH, Jones TW, Davis EA. Clinical and demographic risk factors associated with mortality during early adulthood in a population-based cohort of childhood-onset type 1 diabetes. Diabet Med. 2014;31(12):1550–1558. doi: 10.1111/dme.12522. [DOI] [PubMed] [Google Scholar]
- 9.Jorgensen ME, Almdal TP, Carstensen B. Time trends in mortality rates in type 1 diabetes from 2002 to 2011. Diabetologia. 2013;56(11):2401–2404. doi: 10.1007/s00125-013-3025-7. [DOI] [PubMed] [Google Scholar]
- 10.Morgan E, Cardwell CR, Black CJ, McCance DR, Patterson CC. Excess mortality in Type 1 diabetes diagnosed in childhood and adolescence: a systematic review of population-based cohorts. Acta Diabetol. 2015;52(4):801–807. doi: 10.1007/s00592-014-0702-z. [DOI] [PubMed] [Google Scholar]
- 11.Patterson CC, Dahlquist G, Harjutsalo V, et al. Early mortality in EURODIAB population-based cohorts of type 1 diabetes diagnosed in childhood since 1989. Diabetologia. 2007;50(12):2439–2442. doi: 10.1007/s00125-007-0824-8. [DOI] [PubMed] [Google Scholar]
- 12.Evans-Cheung TC, Bodansky HJ, Parslow RC, Feltbower RG. Mortality and acute complications in children and young adults diagnosed with Type 1 diabetes in Yorkshire, UK: a cohort study. Diabet Med. 2018;35(1):112–120. doi: 10.1111/dme.13544. [DOI] [PubMed] [Google Scholar]
- 13.Morgan E, Black CR, Abid N, Cardwell CR, McCance DR, Patterson CC. Mortality in type 1 diabetes diagnosed in childhood in Northern Ireland during 1989–2012: A population-based cohort study. Pediatr Diabetes. 2017 doi: 10.1111/pedi.12539. [DOI] [PubMed] [Google Scholar]
- 14.Pavkov ME, Bennett PH, Knowler WC, Krakoff J, Sievers ML, Nelson RG. Effect of youth-onset type 2 diabetes mellitus on incidence of end-stage renal disease and mortality in young and middle-aged Pima Indians. JAMA. 2006;296(4):421–426. doi: 10.1001/jama.296.4.421. [DOI] [PubMed] [Google Scholar]
- 15.Hamman RF, Bell RA, Dabelea D, et al. The SEARCH for Diabetes in Youth study: rationale, findings, and future directions. Diabetes Care. 2014;37(12):3336–3344. doi: 10.2337/dc14-0574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dabelea D, Mayer-Davis EJ, Saydah S, et al. Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA. 2014;311(17):1778–1786. doi: 10.1001/jama.2014.3201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. National Center for Health Statistics: National Death Index (NDI), NDI Plus Searches. http://www.cdc.gov/nchs/ndi/index.htm.
- 18.Centers for Disease Control and Prevention, National Center for Health Statistics. Underlying Cause of Death 1999–2014 on CDC WONDER Online Database. Data are from the Multiple Cause of Death Files, 1999–2014, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. Accessed at: http://wonder.cdc.gov/ucd-icd10.html.
- 19.Secrest AM, Becker DJ, Kelsey SF, Laporte RE, Orchard TJ. Cause-specific mortality trends in a large population-based cohort with long-standing childhood-onset type 1 diabetes. Diabetes. 2010;59(12):3216–3222. doi: 10.2337/db10-0862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rhodes ET, Prosser LA, Hoerger TJ, Lieu T, Ludwig DS, Laffel LM. Estimated morbidity and mortality in adolescents and young adults diagnosed with Type 2 diabetes mellitus. Diabet Med. 2012;29(4):453–463. doi: 10.1111/j.1464-5491.2011.03542.x. [DOI] [PubMed] [Google Scholar]
- 21.Amutha A, Anjana RM, Venkatesan U, et al. Incidence of complications in young-onset diabetes: Comparing type 2 with type 1 (the young diab study) Diabetes Res Clin Pract. 2017;123:1–8. doi: 10.1016/j.diabres.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 22.Dart AB, Martens PJ, Rigatto C, Brownell MD, Dean HJ, Sellers EA. Earlier onset of complications in youth with type 2 diabetes. Diabetes Care. 2014;37(2):436–443. doi: 10.2337/dc13-0954. [DOI] [PubMed] [Google Scholar]
- 23.Morimoto A, Onda Y, Nishimura R, et al. Cause-specific mortality trends in a nationwide population-based cohort of childhood-onset type 1 diabetes in Japan during 35 years of follow-up: the DERI Mortality Study. Diabetologia. 2013;56(10):2171–2175. doi: 10.1007/s00125-013-3001-2. [DOI] [PubMed] [Google Scholar]
- 24.Waernbaum I, Blohme G, Ostman J, et al. Excess mortality in incident cases of diabetes mellitus aged 15 to 34 years at diagnosis: a population-based study (DISS) in Sweden. Diabetologia. 2006;49(4):653–659. doi: 10.1007/s00125-005-0135-x. [DOI] [PubMed] [Google Scholar]
- 25.Bosnyak Z, Nishimura R, Hagan Hughes M, et al. Excess mortality in Black compared with White patients with Type 1 diabetes: an examination of underlying causes. Diabet Med. 2005;22(12):1636–1641. doi: 10.1111/j.1464-5491.2005.01671.x. [DOI] [PubMed] [Google Scholar]
- 26.Tull ES, Barinas E. A twofold excess mortality among black compared with white IDDM patients in Allegheny county, Pennsylvania. Pittsburgh DERI Mortality Study Group. Diabetes Care. 1996;19(12):1344–1347. doi: 10.2337/diacare.19.12.1344. [DOI] [PubMed] [Google Scholar]
- 27.Mayer-Davis EJ, Beyer J, Bell RA, et al. Diabetes in African American youth: prevalence, incidence, and clinical characteristics: the SEARCH for Diabetes in Youth Study. Diabetes Care. 2009;32(Suppl 2):S112–122. doi: 10.2337/dc09-S203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cowper DC, Kubal JD, Maynard C, Hynes DM. A primer and comparative review of major US mortality databases. Ann Epidemiol. 2002;12(7):462–468. doi: 10.1016/s1047-2797(01)00285-x. [DOI] [PubMed] [Google Scholar]
- 29.Williams BC, Demitrack LB, Fries BE. The accuracy of the National Death Index when personal identifiers other than Social Security number are used. Am J Public Health. 1992;82(8):1145–1147. doi: 10.2105/ajph.82.8.1145. [DOI] [PMC free article] [PubMed] [Google Scholar]