Abstract
Introduction
Step climbing is a potentially useful modality for testing exercise capacity. However, there are significant variations between test protocols and lack of consistent validation against gold standard cycle ergometry cardiopulmonary exercise testing (CPET). The purpose of the study was to validate a novel technique of exercise testing using a dedicated device.
Methods
We built a step oximetry device from an adapted aerobics step and pulse oximeter connected to a computer. Subjects performed lung function tests, a standard incremental cycle CPET and also a CPET while stepping on and off the step oximetry device to maximal exertion. Data from the step oximetry device were processed and correlated with standard measurements of pulmonary function and cycle CPET.
Results
We recruited 89 subjects (57 years, 50 men). Oxygen uptake (VO2) was 0.9 mL/kg/min (95% CI −3.6 to 5.4) higher in the step test compared with the gold standard cycle CPET, p<0.001. VO2 in the two techniques was highly correlated (R=0.87, p<0.001). Work rate during stair climbing showed the best correlation with VO2 (R=0.69, p<0.0001). Desaturation during step climbing correlated negatively with diffusion capacity for carbon monoxide (r=−0.43, p<0.005). No adverse events occurred.
Conclusions
The step oximetry test was a maximal test of exertion in the subjects studied, achieving slightly higher VO2 than during the standard test. The test was safe to perform and well tolerated by the patients. Parameters derived from the step oximetry device correlated well with gold standard measurements. The step oximetry test could become a useful and standardisable exercise test for clinical settings where advanced testing is not available or appropriate.
Keywords: exercise
Introduction
Difficulty in climbing stairs is a frequent complaint in patients with exercise intolerance from any cause. It is also a familiar and necessary form of exercise for all patients, as opposed to treadmill walking or pedalling on a stationary exercise bicycle. In spite of this, there are only a small number of studies evaluating the physiology of stair climbing. These studies vary in terms of testing protocols, step height, total height climbed (usually limited by the size of the hospital building), the factor determining end of test (height, time) and the endpoint evaluated (height gained, climbing time, velocity, power). Step testing is a reproducible test across different protocols.1–5 In general, step climbing performance correlates well with the gold standard peak oxygen uptake (VO2peak), both in height-limited and time-limited tests, although in most cases VO2peak was not measured during the step climbing itself.2–11 In two recent studies, VO2 was measured directly during step climbing and cycle ergometry, with conflicting results regarding the relationship between VO2 with the different tests.1 12
The aim of this study was to measure VO2 during a standardised, laboratory-based step climbing test using a dedicated device and compare performance with the gold standard test of cycle ergometry. In addition, we explored several novel parameters derived from the technique.
Methods
The study protocol was approved by the Rabin Medical Center Ethics Committee. All subjects gave written informed consent.
Subject selection
Subjects were invited to participate in the study if they had been referred for cycle ergometry cardiopulmonary exercise testing (CPET) by their physician. Patients with significant neurological or musculoskeletal limitation which could affect their step climbing ability were excluded.
Patient testing and data collection
All patients attending for CPET performed spirometry and single breath diffusion capacity for carbon monoxide (DLCO) as a part of their workup, according to standard guidelines (ZAN-500 system, nSpire Health, Longmont, CO).13 14 The cycle ergometry CPET was performed in accordance with established guidelines (CardiO2Max, Medical Graphics, St Paul, MN).15 In brief, patients rested on the cycle ergometer for 2 min, then 2 min of unloaded cycling at 60 rpm followed by a 15 W/min ramp. All parameters measured during CPET were averaged over 30 s. End of test was defined by the earliest occurrence of patient exhaustion or failure to maintain 60 rpm pedalling, achievement of VO2peak predicted, respiratory exchange ratio >1.15 or heart rate (HR) >90% predicted.15 Anaerobic threshold was determined with the V-slope technique.15 Following the test, patients rested on a chair for at least 90 min before doing the step oximetry test, as detailed below.
Step oximetry test: patient monitoring/data collection
Step testing was performed while the subject was monitored with the metabolic cart of the cycle ergometry CPET device. The step oximetry device was built by the investigators from a 17 cm high ‘aerobics’ step, adapted with pressure sensors that transmit a signal to the computer when the subject mounts the step with both feet. A pulse oximeter (Radical 7, Massimo, Irvine, CA) outputted HR and SpO2 data every 6 s to the computer. Integration of time, step count, HR and SpO2 were performed by a computer program. Before the step test, the subject read a standard written instruction, stating that they should climb for as long as possible at a constant rate (20 per min) until their self-perceived limit was reached. A brief demonstration of stepping was performed by the study physician. During the step test the subject mounted and dismounted from the step with one foot after the other until he/she reached their self-perceived maximal exertion or an arbitrary limit of 200 steps (34 m vertical climb). Other than a verbal confirmation that the subject was climbing correctly, the test was performed unencouraged. Subjects were not aware of the 200 steps limit and were not allowed to view the computer monitor during the test.4 At the end of the step test the subject rested on a chair while monitoring of HR/SpO2 continued until recovery (HR within 5% of baseline and SpO2 with 2% of baseline value).
Postprocessing of the data was performed by a computer algorithm developed by the investigators, based on equations from classical Newtonian physics. A graphical representation of a typical test is shown in figure 1. Exercise performance indices were: total height gained; climbing time; mean vertical climbing velocity; total work against gravity (energy: mass*total height gained*g where mass was body weight in kg); and work rate (energy divided by climbing time). We also derived the ’Climb Index' from velocity and height gained. From the HR data we calculated the per cent use of predicted heart rate reserve (220-age) and the slope of HR recovery regression line. Desaturation indices were defined as: maximum absolute drop in SpO2 from baseline value (desaturation); desaturation area (the integration of time with SpO2 values below 95%); and the mean deviation of SpO2 below 95% (saturation deviation). In patients with >2% absolute desaturation we calculated the time to recovery of SpO2 to within 2% of baseline values (resaturation time).
Figure 1.
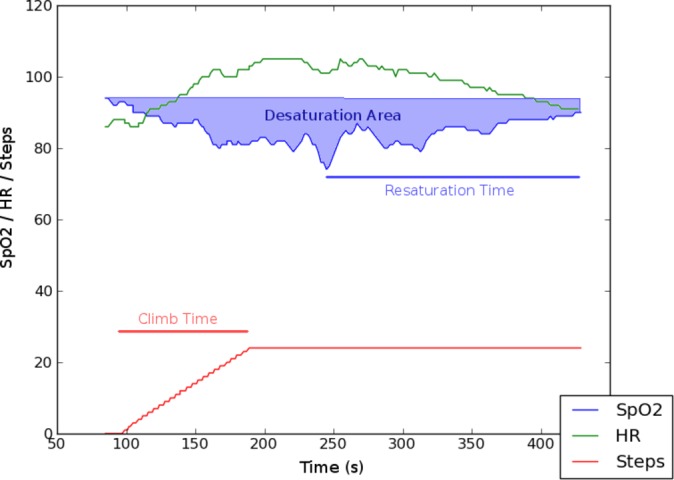
Representative plot from step oximetry device, annotated to demonstrate some of the step oximetry parameters.
Data analysis
The primary outcome of interest was the agreement between VO2 on both tests, assessed by the Bland-Altman technique.16 Secondary endpoints were the correlations between VO2 and the derived exercise performance indices generated by the step oximetry algorithm, or DLCO and the desaturation indices. Categorical data were summarised and analysed using the Χ2 test. Continuous data were summarised as mean (95% CIs) or median (IQR) as appropriate. Parameters with significant right skew were log transformed and analysed and mean, 95% CI reported in their original units after an anti-log transformation.17 The correlation between parameters of interest was by Pearson’s R or Spearman’s rho as appropriate. Given the large number of possible comparisons, we applied the Holm-Bonferroni correction and reported the uncorrected p values that remained significant after correction.18 All tests were two tailed and the predetermined level of significance was p<0.05.
Results
Eighty-nine patients were recruited (table 1). In the step test, mean height gained was 4.72 m (95% CI 4.04 to 5.52), equivalent to 28 steps. No patients reached the maximal limit of 200 steps (34 m ascent). Vertical velocity was 3.18 m/s (95% CI 3.01 to 3.35). No adverse events occurred during the study.
Table 1.
Study participants (n=89). Continuous data shown as mean (95% CI)
| Age (years) | 57.7 (54.3 to 60.2) |
| Sex (M:F) | 50:39 |
| Weight (kg) | 74.4 (70.7 to 78.2) |
| Body mass index (kg/m) | 27.5 (26.5 to 29.1) |
| Principal diagnosis | Lung transplant recipient, 28 |
| Chronic obstructive pulmonary disease, 17 | |
| Pulmonary arterial hypertension, 10 | |
| Cardiac failure, 7 | |
| Interstitial lung disease, 5 | |
| Others, 22 | |
| FVC (% predicted) | 68 (53 to 65) |
| FEV1 (% predicted) | 59 (53 to 64) |
| DLCO (% predicted) | 48 (42 to 54) |
DLCO, diffusion capacity for carbon monoxide; FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity.
Primary endpoint: agreement between VO2 on step oximetry and cycle ergometry
Oxygen uptake was 0.9 mL/kg/min (95% CI −3.6 to 5.4) higher on the step oximetry test compared with the cycle CPET (table 2, figure 2). These higher levels of VO2 were achieved at a significantly shorter exercise time and lower use of cardiac/respiratory reserves than on the cycle CPET (table 2). VO2 in the two techniques was highly correlated, R=0.87; 95% CI (0.81 to 0.92), p<0.001. Of note it was difficult to establish the VO2 at anaerobic threshold during the step climbing test and so this comparison was excluded from the analysis.
Table 2.
Comparison of CPET results with two techniques, the lower section of the table presents data available only from the step test
| Cycle CPET | Step test CPET | MD (step cycle) | |
| Exercise time (s) | 307 (285 to 329) | 114 (98 to 130) | −194 (−380 to −9)**** |
| Work rate (W) | 63 (58 to 69) | 38 (35 to 41) | NA |
| VO2 (mL/kg/min) | 11.9 (11.2 to 12.7) | 12.8 (11.9 to 13.7) | 0.9 (−3.6 to 5.4)*** |
| VO2 (% predicted) | 54 (50 to 57) | 58 (54 to 62) | 5 (−17 to 26)*** |
| Heart rate (bpm) | 115 (111 to 120) | 114 (109 to 118) | −2 (−32 to 28) |
| Cardiac reserve (%) | 71 (69 to 74) | 68 (64 to 72) | 4 (−35 to 28)* |
| O2 pulse (mL/beat) | 7.5 (7.0 to 8.0) | 8.1 (7.5 to 8.7) | 0.7 (− 2.7 to 4.1)*** |
| VE (L/min) | 35.2 (32.7 to 37.8) | 32.8 (30.3 to 35.5) | −2.2 (−16.4 to 11.9)** |
| Breathing reserve (%) | 63 (60 to 67) | 60 (56 to 64) | −3 (−25 to 19)** |
| RER | 1.07 (1.04 to 1.09) | 0.86 (0.84 to 0.88) | −0.21 (−0.45 to 0.03) **** |
| Absolute desaturation | 3 (2 to 4) | 5 (4 to 7) | −2 (4 to −9)**** |
| Steps/min | 19 (18 to 20) | ||
| Total energy (kJ) | 3.35 (2.84 to 3.95) | ||
| Climb index | 2.77 (2.60 to 2.95) | ||
| Height gained (m) | 4.72 (4.04 to 5.52) | ||
| Velocity (m/min) | 3.19 (3.01 to 3.35) | ||
| Saturation deviation | 0.6 (0.0 to 2.4) | ||
| Desaturation area | 48 (0 to 356) | ||
| Resaturation time (s) | 39 (13.5 to 70.0) |
Data presented as mean (95% CI) or median (IQR). Mean difference (MD) between the groups is calculated by the Bland-Altman technique.
Differences in work rate are not compared since the step oximetry system calculates only ascending work.
Significant difference between results in paired t-test:
*P<0.05; **P<0.01; ***P<0.001; ****P<0.0001.
CPET, cardiopulmonary exercise testing; NA, not applicable; RER, respiratory exchange ratio; VE, minute ventilation; VO2, peak oxygen uptake.
Figure 2.
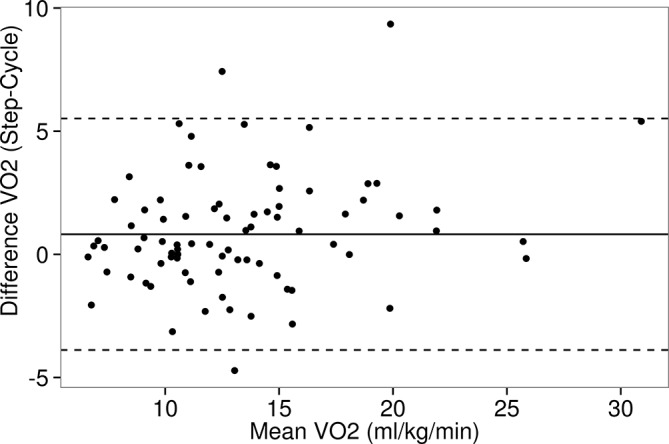
Bland-Altman plot of oxygen uptake (VO2) during cycle ergometry and step oximetry. HR, heart rate.
Secondary endpoint: correlations between step oximetry parameters and VO2 and DLCO
In all comparisons, step oximetry exercise performance indices correlated closely with VO2 achieved on both cycle ergometry and step oximetry, with good CIs (table 3). The closest correlation was observed for the work rate (W) calculated by the step oximetry algorithm (R=0.69) (figure 3). After applying the Bonferroni-Holms correction, all correlations remained statistically significant. Pearson’s R was similar between the two tests for each parameter.
Table 3.
Correlation table for step oximetry exercise performance indices—Pearson’s R (95% CIs)
| Parameter | VO2 (cycle) | VO2 (step) |
| Work rate (W) | 0.69 (0.57 to 0.78) | 0.69 (0.56 to 0.78) |
| Total energy (kJ) | 0.65 (0.51 to 0.75) | 0.67 (0.54 to 0.77) |
| Climb index | 0.57 (0.42 to 0.70) | 0.60 (0.45 to 0.72) |
| Height gained (m) | 0.54 (0.37 to 0.67) | 0.57 (0.40 to 0.70) |
| Velocity (m/min) | 0.47 (0.29 to 0.62) | 0.49 (0.31 to 0.63) |
| Climb time (s) | 0.41 (0.22 to 0.57) | 0.41 (0.22 to 0.57) |
Parameters listed in descending order of R. All correlations reached statistical significance (p<0.0001) after Bonferroni-Holms correction.
Figure 3.
Correlation plot between work rate on the step climber and VO2 on the cycle ergometer.
We also correlated DLCO with the step oximetry desaturation indices (table 4). Saturation deviation, desaturation area and absolute desaturation all showed a significant negative linear correlation with DLCO, after applying the Bonferroni-Holms correction. Of note, absolute desaturation during cycle CPET also correlated negatively with DLCO.
Table 4.
Correlation table for step oximetry oxygenation indices—Spearman’s r test
| Parameter | DLCO |
| Saturation deviation | −0.43* |
| Absolute desaturation | −0.42* |
| Desaturation area | −0.40* |
| Resaturation time | −0.14 |
| Cycle absolute desaturation | −0.47* |
Parameters listed in descending order of r.
*Indicates statistical significance (p<0.005) after Bonferroni-Holms correction.
DLCO, diffusion capacity for carbon monoxide.
Discussion
We report the validation of a computerised laboratory-based step oximetry test on a dedicated device, compared with the gold standard cycle ergometry. We showed that VO2peak on the step test typically exceeds that on the cycle ergometer, and that novel step oximetry exercise performance indices correlate well with VO2peak.
Our step climbing protocol is a potentially attractive form of exercise testing for several reasons. The test appears to be a maximal exercise challenge for most patients, as demonstrated by the higher VO2compared with the gold standard cycle CPET with similar increases in HR and ventilation. Furthermore, no patients in this cohort reached 200 steps in this study, and only 19% in a previous study.4 The protocol has previously been validated against WHO functional class and the 6 min walk (6 MW) test.4 Our results are consistent with those of Dal Corso et al, who demonstrated slightly higher VO2 during step climbing among patients with chronic obstructive pulmonary disease compared with walking.1 Hansen et al studied healthy subjects and found that VO2 was 85% of that obtained during cycle ergometry.12 However, the healthy subjects in Hansen’s group completed the test at submaximal HRs, strongly suggesting that step climbing may have not represented maximal exertion over the time limit or step limit used in the step test. In healthy controls doing the step oximetry test, we have shown a similar phenomenon.4 The set-up costs of the test are also modest compared with the cost of purchasing a full CPET device, and with a standardised protocol, test results can be compared between centres and potentially within clinical trials. Step climbing testing outside a laboratory setting is potentially hazardous since the patient is not always monitored, and could sustain significant trauma if she/he becomes dizzy or slips. By confining the testing to a laboratory or office setting with a maximum height gain of 17 cm and continuously monitoring pulse oximetry, we believe that this technique may be safer for patients. Other forms of ‘low-technology’ exercise testing such as 6 MW require only a long corridor and relatively straightforward training of staff and patients.19 However, 6 MW is regarded as a submaximal test of exercise capacity, since the anaerobic threshold is not typically exceeded in during the test.20 21
As well as demonstrating good agreement between ‘gold-standard’ parameters of exercise capacity (VO2), we also developed and validated novel parameters of exercise performance from the device (3). Previous reports of step climbing have either not recorded or processed detailed data for HR and oxygen saturation during the step test. Clearly it is intuitive and expected that work rate, for example, is correlated closely with VO2. The clinical relevance of this finding is that clinicians are able to objectively quantify exercise capacity without the full CPET device and obtain relevant and valid information.
We demonstrated significant correlation between step climbing desaturation indices and diffusion capacity of the lung (DLCO), replicating the results of a previous study.4 The best correlations with DLCO were seen with derived measurements of SpO2 such as saturation deviation and desaturation area where the extent of desaturation is averaged or integrated over time, respectively. The simple calculation of absolute desaturation (baseline SpO2− nadir SpO2) was less well correlated with DLCO. The step climbing test therefore also gives the clinician some insight into the gas transfer capacity of the lung, which could be useful in an office setting lacking full lung function tests.
Although there are advantages to a stationary step test as discussed above, there are important differences between this test and a step test performed on a staircase. During normal step climbing, the subject performs work against gravity with each sequential upward step. In our test, most of the antigravity work occurs when lifting the lower foot up onto the step. There is also a step-down phase in the step oximetry test, which is less energy consuming (eccentric muscle contraction) than continuing a sequential upward climb. The subject therefore has regular ‘rest’ during the test. Energy expenditure and work rate in our step test are calculated only for the ascending work via classical physics equations. These differences in technique probably explain the relatively low work rates reported by our technique, relative to those reported during hospital staircase-based climbing experiments.2 We note that despite these limitations, the step test work rate parameter had the best correlation with VO2 (table 3). Another potential limitation is that this study was performed on patients with lung disease, although this should not affect the reliability of results since the study simply checked agreement between the two tests in the same patient. At the present time, we also have no data available to give ‘normal ranges’ for the various parameters over a large and varied population. Therefore, at this time, the step climbing test and device should be considered a research tool only.
In summary, we provide the first study of laboratory-based, semiautomated and standardised step test using a dedicated device in a cohort of subjects presenting for exercise testing. We believe that step oximetry testing could become a useful functional test in clinical practice.
Footnotes
Contributors: BDF conceived the study, built the device, analysed the data and drafted the manuscript. NS collected the data, analysed the data and drafted the manuscript. BV and LF collected the data and revised the manuscript. MRK conceived the study, built the device, analysed the data and revised the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data sharing is possible. Please contact the corresponding author.
References
- 1.Dal Corso S, de Camargo AA, Izbicki M, et al. A symptom-limited incremental step test determines maximum physiological responses in patients with chronic obstructive pulmonary disease. Respir Med 2013;107:1993–9. 10.1016/j.rmed.2013.06.013 [DOI] [PubMed] [Google Scholar]
- 2.Cataneo DC, Cataneo AJ. Accuracy of the stair climbing test using maximal oxygen uptake as the gold standard. J Bras Pneumol 2007;33:128–33. [DOI] [PubMed] [Google Scholar]
- 3.Dal Corso S, Duarte SR, Neder JA, et al. A step test to assess exercise-related oxygen desaturation in interstitial lung disease. Eur Respir J 2007;29:330–6. 10.1183/09031936.00094006 [DOI] [PubMed] [Google Scholar]
- 4.Fox BD, Langleben D, Hirsch A, et al. Step climbing capacity in patients with pulmonary hypertension. Clin Res Cardiol 2013;102:51–61. 10.1007/s00392-012-0495-4 [DOI] [PubMed] [Google Scholar]
- 5.Swinburn CR, Wakefield JM, Jones PW. Performance, ventilation, and oxygen consumption in three different types of exercise test in patients with chronic obstructive lung disease. Thorax 1985;40:581–6. 10.1136/thx.40.8.581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brunelli A, Xiumé F, Refai M, et al. Peak oxygen consumption measured during the stair-climbing test in lung resection candidates. Respiration 2010;80:207–11. 10.1159/000279331 [DOI] [PubMed] [Google Scholar]
- 7.Koegelenberg CF, Diacon AH, Irani S, et al. Stair climbing in the functional assessment of lung resection candidates. Respiration 2008;75:374–9. 10.1159/000116873 [DOI] [PubMed] [Google Scholar]
- 8.Kramer MR, Krivoruk V, Lebzelter J, et al. Quantitative 15 steps exercise oximetry as a marker of disease severity in patients with chronic obstructive pulmonary disease. Isr Med Assoc J 1999;1:165–8. [PubMed] [Google Scholar]
- 9.Pollock M, Roa J, Benditt J, et al. Estimation of ventilatory reserve by stair climbing. A study in patients with chronic airflow obstruction. Chest 1993;104:1378–83. [DOI] [PubMed] [Google Scholar]
- 10.Rusanov V, Shitrit D, Fox B, et al. Use of the 15-steps climbing exercise oximetry test in patients with idiopathic pulmonary fibrosis. Respir Med 2008;102:1080–8. 10.1016/j.rmed.2007.12.031 [DOI] [PubMed] [Google Scholar]
- 11.Starobin D, Kramer MR, Yarmolovsky A, et al. Assessment of functional capacity in patients with chronic obstructive pulmonary disease: correlation between cardiopulmonary exercise, 6 minute walk and 15 step exercise oximetry test. Isr Med Assoc J 2006;8:460–3. [PubMed] [Google Scholar]
- 12.Hansen D, Jacobs N, Bex S, et al. Are fixed-rate step tests medically safe for assessing physical fitness? Eur J Appl Physiol 2011;111:2593–9. 10.1007/s00421-011-1886-3 [DOI] [PubMed] [Google Scholar]
- 13.Macintyre N, Crapo RO, Viegi G, et al. Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur Respir J 2005;26:720–35. 10.1183/09031936.05.00034905 [DOI] [PubMed] [Google Scholar]
- 14.Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J 2005;26:319–38. 10.1183/09031936.05.00034805 [DOI] [PubMed] [Google Scholar]
- 15.American Thoracic Society, American College of Chest Physicians. ATS/ACCP Statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med 2003;167:211–77. 10.1164/rccm.167.2.211 [DOI] [PubMed] [Google Scholar]
- 16.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;1:307–10. [PubMed] [Google Scholar]
- 17.Bland JM, Altman DG. Transformations, means, and confidence intervals. BMJ 1996;312:1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Holm S. A simple sequentially rejective multiple test procedure. Scand J Statistics 1979;6:65–70. [Google Scholar]
- 19.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002;166:111–7. 10.1164/ajrccm.166.1.at1102 [DOI] [PubMed] [Google Scholar]
- 20.Deboeck G, Niset G, Vachiery JL, et al. Physiological response to the six-minute walk test in pulmonary arterial hypertension. Eur Respir J 2005;26:667–72. 10.1183/09031936.05.00031505 [DOI] [PubMed] [Google Scholar]
- 21.Oudiz RJ, Barst RJ, Hansen JE, et al. Cardiopulmonary exercise testing and six-minute walk correlations in pulmonary arterial hypertension. Am J Cardiol 2006;97:123–6. 10.1016/j.amjcard.2005.07.129 [DOI] [PubMed] [Google Scholar]



