Abstract
Background
Limited comparative data are available on the efficacy of cryoablation versus radiofrequency ablation in patients with atrial fibrillation. This study aimed to compare radiofrequency ablation and cryoablation with regard to clinical outcomes and the restoration of sinus rhythm or atrial contractility.
Methods
A total of 239 patients who underwent surgical ablation between August 2003 and December 2016 at our institution were included. The patients were divided into 2 groups according to the energy device that was used (group A: n=140, radiofrequency ablator; group B: n=99, cryoablator). Echocardiographic data, overall survival, and major cardiovascular and cerebrovascular event (MACCE)-free survival were compared between the 2 groups.
Results
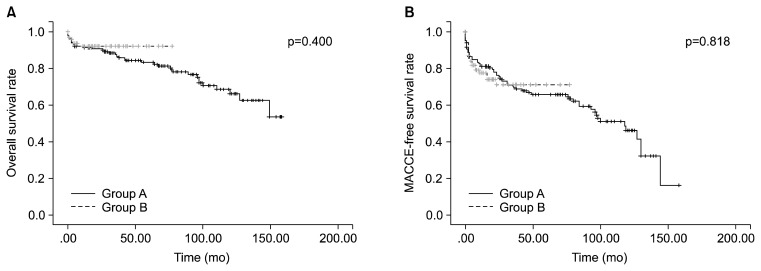
At 1 year of follow-up, the atrial contractility recovery rate was 32.2% (19 of 59) in group A and 48.8% (21 of 44) in group B. In addition, cryoablation was found to be a predictive factor for the recovery of atrial contractility (cryoablation vs. radiofrequency ablation: odds ratio, 2.540; 95% confidence interval, 1.063–6.071; p=0.036). The left ventricular ejection fraction was significantly higher in group B (53.1%±11.5% vs. 59.1%±6.3%, p=0.001). The median follow-up duration was 36 months. The 5-year overall survival rate was 80.1%±3.6% in group A and 92.1%±2.9% in group B (p=0.400). The 5-year MACCE-free survival rate was 70.3%±4.0% in group A and 70.9%±5.6% in group B (p=0.818).
Conclusion
Cryoablation was associated with a higher atrial contractility restoration rate and better left ventricular function than radiofrequency ablation. However, no significant relationship was observed between the energy source and overall or MACCE-free survival.
Keywords: Cox-maze procedure, Atrial contraction, Radiofrequency, Ablation, Cryoablation
Introduction
Atrial fibrillation (AF) is the most common type of arrhythmia. It is associated with several long-term risks, including increased risks of stroke, heart failure, and all-cause mortality [1]. Performing a maze procedure for the treatment of AF concomitantly with other cardiac procedures can prolong the operation time, cardiopulmonary bypass (CPB) time, and cardiac arrest time. In addition, surgical ablation increases the risk of postoperative bleeding and the need for permanent pacemaker (PPM) insertion [2,3]. However, the substantial benefits from regaining sinus rhythm and atrial contractility warrant the potential risks [3]. Thus, performing surgical ablation concomitantly with other cardiac procedures is recommended in patients with AF [4]. Although the original ‘cut-and-sew’ Cox maze III procedure had higher efficacy, it was widely substituted with ablation using radiofrequency and cryothermal energy to overcome its technical complexity and to reduce the risk of postoperative bleeding [5–7]. However, few studies have compared the efficacy of radiofrequency ablation with that of cryoablation. The purpose of this study was to compare radiofrequency ablation and cryoablation with regard to clinical outcomes, including overall survival, major cardiovascular and cerebrovascular event (MACCE)-free survival, sinus rhythm restoration, atrial contractility, and overall cardiac function.
Methods
This study was approved by the Institutional Review Board of Seoul National University Bundang Hospital, which waived the need for informed consent (IRB approval no., B-1711-432-107).
1) Study population
A total of 239 consecutive patients who underwent surgical ablation at our institution with or without other cardiac procedures between August 2003 and December 2016 were included. Patients were divided into 2 groups according to the device utilized as an energy source for surgical ablation. Radiofrequency ablators were either monopolar (Cardioblate; Medtronic Inc., Minneapolis, MN, USA) or bipolar (Cardioblate, Medtronic Inc.) and were used in 140 patients (group A), whereas cryoablators ([Cardioblate, Medtronic Inc.] or [cryoICE; AtriCure Inc., Mason, OH, USA]) were used in 99 patients (group B). The preoperative characteristics of the patients are described in Table 1. A history of previous cardiac surgery was more common in group A patients. Most of the patients had persistent AF, except for 7 (2.9%) who had paroxysmal AF.
Table 1.
Preoperative characteristics
| Characteristic | Group A (n=140) | Group B (n=99) | p-value |
|---|---|---|---|
| Demographics | |||
| Age (yr) | 60.5±12.2 | 61.7±10.9 | 0.420 |
| Male | 67 (47.9) | 42 (42.4) | 0.406 |
| Smoker | 0.257 | ||
| Never smoker | 83 (59.3) | 67 (67.7) | |
| Ex-smoker | 33 (23.6) | 22 (22.2) | |
| Current smoker | 24 (17.1) | 10 (10.1) | |
| Diabetes | 26 (18.6) | 11 (11.1) | 0.116 |
| Hypertension | 46 (32.9) | 43 (43.4) | 0.096 |
| Dyslipidemia | 9 (6.4) | 12 (12.1) | 0.126 |
| History of stroke | 17 (12.1) | 12 (12.1) | 0.996 |
| Chronic kidney disease | 5 (3.6) | 3 (3.0) | 0.819 |
| Acute renal failure | 1 (0.7) | 1 (1.0) | >0.999 |
| Chronic obstructive pulmonary disease | 13 (9.3) | 9 (9.1) | 0.959 |
| Previous cardiac surgery | 8 (5.7) | 0 | 0.022 |
| Infective endocarditis | 4 (2.9) | 3 (3.0) | 0.999 |
| Type of atrial fibrillation | 0.999 | ||
| Persistent | 136 (97.1) | 96 (97.0) | |
| Paroxysmal | 4 (2.9) | 3 (3.0) | |
| Preoperative echocardiography | |||
| Left ventricle ejection fraction (%) | 55.0±9.4 | 56.2±10.4 | 0.338 |
| Left atrial dimension (mm) | 55.8±10.0 | 55.4±9.8 | 0.775 |
| Left ventricle end-diastolic dimension (mm) | 54.6±10.8 | 52.47±9.7 | 0.119 |
Values are presented as mean±standard deviation for continuous variables and frequency (%) for categorical variables.
2) Operative strategy and surgical ablation lesion set
The operative characteristics of the patients are described in Table 2. Replacement or repair of the valve was most frequently combined with surgical ablation. Concomitant coronary artery bypass grafting was more common in group A patients. Decisions on performing surgical ablation, the energy source, and the lesion set were made at the surgeon’s discretion. Radiofrequency ablators were available and used from the beginning of the study period, whereas cryoablators were used starting in November 2009. The bilateral lesion sets did not change based on the choice of ablator. Radiofrequency ablation lesion sets were replaced by cryoablation lesion sets. The right atrial auricle was resected. A longitudinal line between the superior and inferior vena cava, a vertical line at the inferior vena cava, and an atrial septal line were cut and sewn. The lines of the tricuspid annulus, coronary sinus, pulmonary vein box, mitral annulus, left atrial auricle, and left atrial auricle to the mitral valve were ablated. When surgical ablation was conducted under CPB, the bypass and aortic cross-clamp time were recorded and compared between the patients in the 2 groups.
Table 2.
Operative characteristics and maze lesion set
| Characteristic | Group A (n=140) | Group B (n=99) | p-value |
|---|---|---|---|
| Urgency/emergency operation | 0.037 | ||
| Elective | 131 (93.6) | 99 (100.0) | |
| Urgency | 8 (5.7) | 0 | |
| Emergency | 1 (0.7) | 0 | |
| Concomitant procedure | |||
| Valve | 122 (87.1) | 86 (86.9) | 0.950 |
| Coronary artery bypass graft surgery | 17 (12.1) | 2 (2.0) | 0.004 |
| Aorta | 11 (8.0) | 5 (5.1) | 0.377 |
| Othera) | 13 (9.3) | 9 (9.1) | 0.959 |
| Cardiopulmonary bypass time (min) | 157.4±59.6 | 160.7±44.4 | 0.679 |
| Aortic cross-clamping time (min) | 120.6±48.9 | 129.4±143.6 | 0.551 |
| Ablation lesion set | 0.011 | ||
| Bilateral | 123 (87.9) | 98 (99.0) | |
| Right-side | 10 (7.1) | 0 | |
| Left-side | 4 (2.9) | 0 | |
| Pulmonary vein isolation | 3 (2.1) | 1 (1.0) | |
Values are presented as frequency (%) for categorical variables or mean±standard deviation for continuous variables.
Repair of atrial septal defect, repair of ventricular septal defect, and tumor excision.
3) Clinical outcomes and echocardiography findings
Operative and anesthetic records of heart rhythm were reviewed at the end of each operation. The rhythm was assessed using a 12-lead electrocardiogram (ECG) or a 24-hour Holter monitor and compared between the groups at discharge and at a 1-year follow-up. Additionally, echocardiographic (echoCG) data were collected at discharge and at the 1-year follow-up. Measurements of the left ventricle ejection fraction (LVEF), left atrium anteroposterior dimension (LAD), and left ventricle end-diastolic dimension (LVEDD) were recorded. Atrial contractility was assessed by the presence of the A-wave (1: positive velocity from the left atrium to left ventricle was observed using Doppler echoCG after observing the p-wave on ECG or 2: atrial contraction was observed using tissue Doppler echoCG after observing the p-wave on ECG). Survival data were collected from outpatient clinical visits, telephone calls, or records of the Korean Ministry of the Interior and Safety. A MACCE was defined as the occurrence of any of the following: all-cause death, myocardial infarction, cardiac reoperation/reintervention, stroke, transient ischemia attack, or readmission for congestive heart failure.
4) Statistical analysis
IBM SPSS Statistics ver. 22.0.0 (IBM Corp., Armonk, NY, USA) was used for statistical analyses. Continuous variables are presented as mean±standard deviation. The Student t-test was used to compare the results of continuous variables. The results for categorical variables are presented as frequency (%), and categorical variables were analyzed using the chi-square test or the Fisher exact test. Prognostic factors for atrial contractility were evaluated using multivariate logistic regression analysis. All p-values <0.05 were considered to indicate statistical significance. Survival data were depicted using a Kaplan-Meier curve and tested using the log-rank test.
Results
1) Sinus conversion and restoration of atrial contractility
Apart from 1 case of early death in group B, all patients had records of their immediate postoperative rhythm status and ECG before discharge. In the immediate postoperative period, the group A patients had a higher rate of AF, while the group B patients had a higher rate of abnormal sinus rhythm (Table 3). At discharge, the group A patients had a higher rate of AF, whereas the group B patients had a higher rate of restoration of atrial contractility, which was less than half that of sinus conversion.
Table 3.
Sinus conversion and restoration of atrial contractility
| Variable | Group A | Group B | p-value |
|---|---|---|---|
| Immediate postoperative rhythm | <0.001 | ||
| Atrial fibrillation | 30 (21.4) | 8 (8.2) | |
| Sinus rhythm | 100 (71.4) | 66 (67.3) | |
| Sick sinus syndrome | 10 (7.1) | 24 (24.5) | |
| Rhythm at discharge | 0.002 | ||
| Atrial fibrillation | 69 (49.3) | 27 (27.6) | |
| Sinus rhythm | 65 (46.4) | 68 (69.4) | |
| Sick sinus syndrome | 6 (4.3) | 3 (3.1) | |
| Atrial contractility at discharge | 14 (10.8) | 20 (20.4) | 0.043 |
| Rhythm at 1 year | 0.186 | ||
| Atrial fibrillation | 31 (30.7) | 12 (19.7) | |
| Sinus rhythm | 66 (65.3) | 48 (78.7) | |
| Sick sinus syndrome | 4 (4.0) | 1 (1.6) | |
| Atrial contractility at 1 year | 19 (32.2) | 21 (48.8) | 0.089 |
| Left ventricle ejection fraction at 1 year (%) | 53.1±11.5 | 59.1±6.3 | 0.001 |
| Left atrial dimension at 1 year (mm) | 48.3±8.5 | 52.0±17.7 | 0.164 |
| Left ventricle end-diastolic dimension at 1 year (mm) | 50.4±7.5 | 49±5.9 | 0.298 |
| Permanent pacemaker insertion | 8 (5.7) | 2 (2.0) | 0.202 |
Values are presented as frequency (%) for categorical variables or mean±standard deviation for continuous variables.
When rhythm and atrial contractility were compared at the 1-year follow-up using the available ECG and echoCG data, sinus rhythm and atrial contractility were more frequently found in the group B patients; however, no statistical significance was observed. In addition to atrial contractility, the LVEF was significantly higher in the group B patients, and was comparable with the preoperative data. The PPM insertion rate was higher in the group A patients. However, these differences were not statistically significant.
2) Predictive factors for restoration of atrial contractility
To assess the impact of the energy source used in the maze procedure on atrial contractility, logistic regression analysis was performed, with possible confounding factors including LAD, surgical ablation lesion set, and persistence of AF (Table 4). At discharge, it was found that the use of a cryoablator rather than a radiofrequency ablator contributed to the restoration of atrial contractility, which remained consistent at the 1-year follow-up (Table 5). Moreover, a smaller LAD was a predictive factor for restoration of atrial contractility at discharge (Table 4).
Table 4.
Predictive factor analysis for atrial contractility at discharge
| Variable | Odds ratio (95% confidence interval) | p-value |
|---|---|---|
| Cryoablation (vs. radiofrequency) | 2.603 (1.151–5.885) | 0.022 |
| Preoperative left atrial dimension | 0.950 (0.910–0.991) | 0.017 |
| Bilateral ablation lesion set | 0.550 (0.118–2.574) | 0.448 |
| Paroxysmal atrial fibrillation (vs. persistent) | 0.544 (0.056–5.332) | 0.602 |
| Concomitant coronary artery bypass graft surgery | 1.381 (0.306–6.236) | 0.675 |
Multivariate logistic regression analysis.
Table 5.
Predictive factor analysis for atrial contractility at 1-year follow-up
| Variable | Odds ratio (95% confidence interval) | p-value |
|---|---|---|
| Cryoablation (vs. radiofrequency) | 2.540 (1.063–6.071) | 0.036 |
| Preoperative left atrial dimension | 0.964 (0.925–1.005) | 0.084 |
| Bilateral ablation lesion set | 0.350 (0.041–2.986) | 0.337 |
| Paroxysmal atrial fibrillation (vs. persistent) | 2.886 (0.226–36.796) | 0.414 |
| Concomitant coronary artery bypass graft | 2.105 (0.127–34.834) | 0.603 |
Multivariate logistic regression analysis.
3) Survival analysis according to the energy source
There were 3 cases of early (30-day) mortality in both group A (3 of 140 [2.1%]) and group B (3 of 99 [3.0%]). At a median follow-up duration of 36 months (group A: 76.9 months; interquartile range [IQR], 33.2–111.5 months; group B: 18.6 months; IQR, 10.0–28.6 months), there were 44 overall mortalities. There was no significant difference in overall survival between the 2 groups (Fig. 1A). The 1-year, 3-year, and 5-year overall survival rates were 91.4%±2.4%, 87.5%±2.8%, and 80.1%±3.6% in group A, respectively, and 95.9%±2.0%, 92.1%±2.9%, and 92.1%± 2.9% in group B, respectively.
Fig. 1.
Overall survival (A) and MACCE-free survival (B) of group A and group B. There was no significant difference in overall survival (p=0.400) or MACCE-free survival (p=0.818) between the 2 groups. MACCE, major cardiovascular and cerebrovascular event.
MACCE-free survival was not significantly different between the 2 groups (Fig. 1B). In group A, the 1-year, 3-year, and 5-year MACCE-free survival rates were 91.4%±2.4%, 80.2%±3.4%, and 70.3%±4.0%, respectively, while in group B, they were 92.8%±2.6%, 78.9%±4.3%, and 70.9%±5.6%, respectively.
Discussion
1) Sinus conversion
Both radiofrequency ablation and cryoablation are known to be safe and effective for restoring sinus rhythm in AF patients [5–12]. The sinus rhythm restoration rate has been reported to be between 61% and 85% [6–13], which is slightly lower than that reported for the standard ‘cut-and-sew’ Cox maze III procedure [5–12]. However, it has been argued that the restoration rate of the standard Cox-maze III has been overestimated, with the real restoration rate being approximately 80% [13].
Few studies have compared the results of the maze procedure according to the energy source used [8,9,12]. In the current study, the frequency of sinus rhythm was higher in the cryoablation group, whereas that of AF was higher in the radiofrequency ablation group at discharge. Similar to previous studies, the frequency of sinus rhythm at the 1-year follow-up increased in both groups [14]; however, this difference was not statistically significant.
2) Atrial contractility
The rate of restoration of atrial contractility, which has been reported to be 23%–76% [10,15,16], was found to be approximately 20% lower than that of sinus rhythm [9,14–16]. Theoretically, because of the atrial ‘kick,’ restoration of atrial contractility may be associated with increased ventricular preload, increased LVEF, reduced LAD, and reduced risk of stroke. However, its predictors have not yet been established [15,16]. In the current study, atiral contractility restoration rate at discharge was significantly higher in the cryoablation group than in the radiofrequency ablation group. And, the rate was associated with smaller preoperative LAD. In contrast, the only predictor of restoration of atrial contractility at the 1-year follow-up was cryoablation.
3) Clinical outcomes
There was no statistically significant difference in the overall survival and MACCE-free survival (including stroke) rates between the 2 groups. Owing to the restoration of atrial contractility, which was shown to be associated with the energy source used, the incidence of stroke or readmission for heart failure was expected to be lower in group B. However, because of the small number of patients and the short follow-up period, those clinical outcomes were not found to be significantly different between the 2 groups.
4) Echocardiographic
There were no significant differences in preoperative echoCG parameters between the 2 groups, while the group A patients showed higher LVEF, smaller LAD, and smaller LVEDD at the 1-year follow-up than the group B patients. The results of this study may be limited due to loss to follow-up and variations in the echoCG follow-up period. Accordingly, these outcomes should be interpreted with caution. However, these results imply that restoration of atrial contractility may be associated with good left heart function.
5) Permanent pacemaker insertion
According to the literature, the incidence of PPM insertion after the maze procedure is 7%–11% [2,5]. In this study, the incidence of PPM insertion was 5.7% in group A and 2.0% in group B; these rates are consistent with those reported in previous studies [2,5].
6) Limitation
This study was a retrospective single-center study. This center started performing surgical ablation in 2004. The energy sources and equipment used in surgical ablation have changed over time. Atrial contractility was only assessed by the presence of the A-wave in trans-mitral flow, rather than the A-wave in trans-tricuspid flow. In some studies, the clinical manifestations differed according to left and right atrial contractility [10,15,16]. In addition, although surgical ablation is known to affect the functional class of patients [3], our study did not include functional class assessments.
7) Conclusion
In the maze procedure, compared with radiofrequency ablation, cryoablation may be associated with improved atrial contractility recovery and left ventricular function, as observed on echoCG. However, no relationship between the energy source used in the maze procedure and overall or MACCE-free survival was observed.
Acknowledgments
The authors give special thanks to Hyun Jeong Han, RN, as a clinical research specialist, for her tremendous support in collecting, maintaining, and analyzing our data.
This study was supported by a Grant of the Samsung Vein Clinic Network (Daejeon, Anyang, Cheongju, Cheonan; Fund no. KTCS04-106).
Footnotes
This paper was presented in the 49th Annual Meeting of Korean Society of Thoracic and Cardiovascular Surgery, 2017.
Conflict of interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Stewart S, Hart CL, Hole DJ, McMurray JJ. A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Am J Med. 2002;113:359–64. doi: 10.1016/S0002-9343(02)01236-6. [DOI] [PubMed] [Google Scholar]
- 2.Ad N, Holmes SD, Ali R, Pritchard G, Lamont D. A single center’s experience with pacemaker implantation after the Cox maze procedure for atrial fibrillation. J Thorac Cardiovasc Surg. 2017;154:139–46. doi: 10.1016/j.jtcvs.2016.12.047. [DOI] [PubMed] [Google Scholar]
- 3.Kawaguchi AT, Kosakai Y, Sasako Y, Eishi K, Nakano K, Kawashima Y. Risks and benefits of combined maze procedure for atrial fibrillation associated with organic heart disease. J Am Coll Cardiol. 1996;28:985–90. doi: 10.1016/S0735-1097(96)00275-6. [DOI] [PubMed] [Google Scholar]
- 4.Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur J Cardiothorac Surg. 2016;50:e1–e88. doi: 10.1093/ejcts/ezw313. [DOI] [PubMed] [Google Scholar]
- 5.Ad N, Barnett S, Lefrak EA, et al. Impact of follow-up on the success rate of the cryosurgical maze procedure in patients with rheumatic heart disease and enlarged atria. J Thorac Cardiovasc Surg. 2006;131:1073–9. doi: 10.1016/j.jtcvs.2005.12.047. [DOI] [PubMed] [Google Scholar]
- 6.Ghavidel AA, Javadpour H, Shafiee M, Tabatabaie MB, Raiesi K, Hosseini S. Cryoablation for surgical treatment of chronic atrial fibrillation combined with mitral valve surgery: a clinical observation. Eur J Cardiothorac Surg. 2008;33:1043–8. doi: 10.1016/j.ejcts.2008.03.019. [DOI] [PubMed] [Google Scholar]
- 7.Sie HT, Beukema WP, Misier AR, et al. Radiofrequency modified maze in patients with atrial fibrillation undergoing concomitant cardiac surgery. J Thorac Cardiovasc Surg. 2001;122:249–56. doi: 10.1067/mtc.2001.114633. [DOI] [PubMed] [Google Scholar]
- 8.Ad N, Holmes SD, Rongione AJ, Massimiano PS, Fornaresio LM. Does surgical ablation energy source affect long-term success of the concomitant Cox maze procedure? Ann Thorac Surg. 2017;104:29–35. doi: 10.1016/j.athoracsur.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 9.Chen MC, Guo GB, Chang JP, Yeh KH, Fu M. Radiofrequency and cryoablation of atrial fibrillation in patients undergoing valvular operations. Ann Thorac Surg. 1998;65:1666–72. doi: 10.1016/S0003-4975(98)00230-6. [DOI] [PubMed] [Google Scholar]
- 10.Chen MC, Chang JP, Chang HW. Preoperative atrial size predicts the success of radiofrequency maze procedure for permanent atrial fibrillation in patients undergoing concomitant valvular surgery. Chest. 2004;125:2129–34. doi: 10.1378/chest.125.6.2129. [DOI] [PubMed] [Google Scholar]
- 11.Jeong DS, You JH, Jeon CS, et al. Impact of ablation duration on rhythm outcome after concomitant maze procedure using cryoablation in patients with persistent atrial fibrillation. J Cardiothorac Surg. 2017;12:60. doi: 10.1186/s13019-017-0620-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee KH, Min J, Kim KH, Hwang HY, Kim JS. Efficacy of Cox maze IV procedure using argon-based cryoablation: a comparative study with N2O-based cryoablation. Korean J Thorac Cardiovasc Surg. 2014;47:367–72. doi: 10.5090/kjtcs.2014.47.4.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ad N, Henry L, Hunt S, Barnett S, Stone L. The Cox-maze III procedure success rate: comparison by electrocardiogram, 24-hour holter monitoring and long-term monitoring. Ann Thorac Surg. 2009;88:101–5. doi: 10.1016/j.athoracsur.2009.04.014. [DOI] [PubMed] [Google Scholar]
- 14.Jeon CS, Shim MS, Park SJ, et al. The absence of atrial contraction as a predictor of permanent pacemaker implantation after maze procedure with cryoablation. Korean J Thorac Cardiovasc Surg. 2017;50:163–70. doi: 10.5090/kjtcs.2017.50.3.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim YJ, Sohn DW, Park DG, et al. Restoration of atrial mechanical function after maze operation in patients with structural heart disease. Am Heart J. 1998;136:1070–4. doi: 10.1016/S0002-8703(98)70165-6. [DOI] [PubMed] [Google Scholar]
- 16.Loardi C, Alamanni F, Galli C, et al. Surgical treatment of concomitant atrial fibrillation: focus onto atrial contractility. Biomed Res Int. 2015;2015:274817. doi: 10.1155/2015/274817. [DOI] [PMC free article] [PubMed] [Google Scholar]