Abstract
Background
Affective instability is a facet of emotion dysregulation that characterizes various mental disorders, including Major Depressive Disorder (MDD). However, it is unclear as to how affective instability predicts the course of MDD. It is also unknown whether affective instability is a relevant predictor of MDD in later adulthood, a period when there is a decrease in both affective instability and MDD prevalence. Thus, we investigated the role of affective instability in the course of MDD in a sample of late middle-age and older adults.
Methods
Using a longitudinal design over six years, 1,630 adults aged 55–64 years (M = 59.60, SD = 2.70) completed a baseline assessment of affective instability (self-report, informant-report, interviewer-report), three assessments of MDD (computerized interview), and eight assessments of depressive symptoms (self-report).
Results
Baseline affective instability positively predicted the likelihood of having lifetime major depressive episodes (MDE) and first-time MDEs, as well as depressive symptoms up to six years later. However, affective instability did not predict remission or having more depressive symptoms over time. These findings held when controlling for neuroticism.
Limitations
We only assessed affective instability at the baseline, did not investigate specific mechanisms or recurrence, and focused on middle-age and older adults.
Conclusions
Our findings replicate and extend prior work by showing that affective instability is differentially related to multiple aspects of MDD’s course and remains an important predictor of MDD even in older age. We discuss implications for the role of affective instability in MDD across the lifespan.
Keywords: affective instability, emotion dysregulation, depression course, older adulthood, risk factors
Introduction
Emotion dysregulation is highly characteristic of Major Depressive Disorder (MDD), one of the world’s most common and debilitating psychiatric disorders (Kessler et al., 2003). Existing emotion research has largely focused two key facets of emotion dysregulation in MDD: aberrant levels of positive and negative affect (e.g., Brown, Chorpita, & Barlow, 1998; Hofmann, Sawyer, Fang, & Asnaani, 2012) and emotion regulation strategy use (e.g., Ehring, Tuschen-Caffier, Schnulle, Fischer, & Gross, 2010, Garnefski & Kraaij, 2006). However, elevated affective instability, intense and frequent shifts (i.e., variability) in emotional experience (e.g., Larsen & Diener, 1987), is another facet of emotion dysregulation that characterizes various mental health disorders, such as bipolar disorder (Henry et al., 2001) and borderline personality disorder (Koeningsberg, 2010; Trull et al., 2008). Affective instability is also relevant for MDD (e.g., Peeters, Berkhof, Delespaul, Rottenberg, & Nicolson, 2006). Individuals with a lifetime history of MDD have higher affective instability than do those without a lifetime history of MDD (Angst, Gamma, & Endrass, 2003; Thompson, Berenbaum, & Bredemeir, 2011), and a meta-analysis found that individuals with MDD have greater affective instability than do individuals without MDD (Houben, Van Den Noortgate, & Kuppens, 2015). There is also empirical support for the temporal association between affective instability and depression; greater affective instability prospectively predicted changes in depressive symptoms in young adult women (Thompson et al., 2011).
One period of life that is especially important to consider when examining the course of MDD is older adulthood since MDD prevalence is lower during this life stage. Decreased prevalence may be partly due to the normative age-related decrease in affective instability (e.g., Brose, De Roover, Cuelemans, & Kuppens, 2015; Carstensen et al., 2011). Thus, older adults who do not improve in emotion regulation and show a decrease in affective instability, may be more likely to experience MDEs and have greater depressive symptoms. Indeed, although MDD is more common in younger adults than in older adults, it is still the most prevalent of all the psychiatric disorders among older adults (Fiske, Wetherell, & Gatz, 2010). Furthermore, older adults with MDD have a worse prognosis than younger adults with MDD, such as a reduced likelihood of going into remission and higher suicide rates (Rodda, Walker, & Carter, 2011).
A growing number of studies indicate that affective instability consistently plays a critical role in MDD. However, most studies that have examined the relevance of affective instability in MDD have largely focused on how affective instability corresponds to MDEs at one time point (e.g., Angst et al., 2003). Thus, it is not clear how affective instability may be relevant for changes in MDD over time (i.e., remission). Addressing this question is important because MDD is a highly complex and recurrent disorder (Monroe & Harkness, 2011). Further, most studies on this topic have used younger adult or middle-aged adult samples (e.g., Peeters et al., 2006; Thompson et al., 2012). And although a meta-analysis on affective variability and psychological well-being (Houben et al., 2016) suggests that affective instability remains a relevant predictor of MDD later in life, these samples consisted of few older adults. Thus, it is unclear whether affective instability continues to predict MDD later in life. This knowledge is critical because both affective instability (e.g., Brose et al., 2015; Carstensen et al., 2000) and MDD prevalence (e.g., Fiske et al., 2010) decrease with age.
The Present Research
In the present research, we extend prior work in two important ways. First, we examine how affective instability prospectively predicts the course of MDD, including the onset and remission of major depressive episodes (MDE). Second, we investigate whether affective instability remains a key risk factor later in life by examining it as a predictor of MDD in late middle-age and older adults. We address these gaps in the literature by investigating how affective instability predicts MDD’s course in a 6-year longitudinal study with a large sample of late middle-aged and early older adults, and evaluate MDEs and depressive symptoms. Based on studies showing a positive association between affective instability and MDD (e.g., Thompson et al., 2011), we hypothesize that middle-aged and older adults who have greater affective instability will be more likely to have lifetime and first-time MDEs and less likely to recover from MDEs. We hypothesize that they will also report more depressive symptoms over time.
To isolate the unique effect of affective instability on MDD, we controlled for neuroticism and the other remaining Borderline Personality Disorder (BPD) symptoms. Neuroticism is key a risk factor of MDD (e.g., Kendler, Kuhn, & Prescott, 2004) that is largely characterized by negative affectivity (e.g., Watson, Wiese, Vaidya, & Tellegen, 1999). Although neuroticism is related to affective instability (Miller & Pilkonis, 2006; Miller, Vachon, & Lynam, 2009), it has been shown to be a broader, distinct construct (Peeters et al., 2006). We controlled for BPD symptoms because BPD is highly comorbid with MDD (Grant et al., 2008).
Methods
Participants and Procedure
A community-based sample of 1,630 late middle-aged and early old age adults were recruited as part of a larger longitudinal study for the St. Louis Personality and Aging Network (see Oltmanns and Gleason [2011] for details regarding recruitment and assessment). To focus on MDD, we excluded participants who experienced a manic episode (2.3% of the sample), as assessed by the Computerized Screening Version of the Diagnostic Interview Schedule (C-DIS-IV; Robins, Helzer, Croughan, & Ratcliff, 1981) at baseline. This left us with a sample of 1,592 adults.
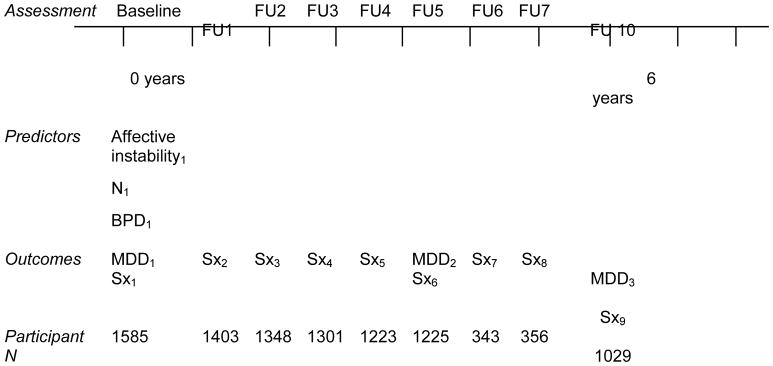
At baseline, participants were ages 55–64 years (M = 59.60, SD = 2.70), showed a relatively equal gender distribution (55% female), and were mostly Caucasian (65%) or African American (33%). About half of the participants had a bachelor’s degree or higher (54%). In addition to completing measures at baseline, participants were involved in subsequent follow-ups every six months. Relevant to the current paper, self-, informant-, and interviewer-reported affective instability were collected at baseline, MDD diagnosis was obtained at three time points (baseline, follow-up five [FU5], follow-up ten [FU10]), and depressive symptoms were collected at nine time points (baseline and all follow-ups [FU1-FU7; FU10]). Depressive symptoms were not assessed at FU8, and only 20 participants completed the measure during FU9 due to a gap in funding; thus, we excluded these time points from the paper. Figure 1 shows the study design and number of participants at each time point.
Figure 1.
Study design timeline and number of participants at each time point. Each tic mark represents six months. FU = follow-up. Affective instability = self-, informant-, and interviewer-reported affective instability; N = neuroticism; BPD = Borderline Personality Symptoms. MDD = MDD diagnosis; Sx = self-reported depressive symptoms. Small subscripts reflect assessment number for a given measure.
Measures
Affective instability
We assessed affective instability using self, informant-, and interviewer-reports. Following Miller and Pilkonis (2006), we made a composite score of affective instability from ratings on four diagnostic criteria. The four items were as follows: “perceives attacks on his or her character or reputation that are not apparent to others and is quick to react angrily or to counterattack (paranoid personality disorder; PPD);” “displays rapidly shifting and shallow expression of emotions (histrionic personality disorder; HPD);” “affective instability due to a marked reactivity of mood (e.g., intense episodic dysphoria, irritability, or anxiety usually lasting a few hours and only rarely more than a few days [borderline personality disorder; BPD]);” “inappropriate, intense anger or difficulty controlling anger (e.g., frequent displays of temper, constant anger, recurrent physical fights; BPD).
Self- and informant-reports of affective instability were assessed using the Multisource Assessment of Personality Pathology (MAPP; Okada & Oltmanns, 2009). The MAPP items translate the DSM-IV criteria to language that is accessible to lay people. “I become angry quickly when I am criticized (PPD);” “I am not afraid to show my emotions and my emotions can change quickly (HPD);” “I have sudden, intense outbursts of anger (BPD);” “I have strong mood swings in response to events (BPD).” Participants rated each of these items about themselves, and informants rated these items about the participant (e.g., “He/she becomes angry quickly when they are criticized”) using a 5-point scale (0 = I/he is never like this; 4 = I/she is always like this). Interviewer-reported affective instability was assessed using the Semi-Structured Interview for DSM-IV Personality (SIDP-IV; Pfohl, Blum, & Zimmerman, 1997). This is a diagnostic interview in which the interviewer asks open-ended questions that map onto the DSM-IV criteria for personality disorders. We included the scores from the four relevant diagnostic criteria of PPD, HPD, or BPD. The interviewers were trained clinical graduate students and research assistants. Although the interviewers used participants’ answers to determine their scoring, they also relied on behavioral observations (e.g., facial expressions) and made a clinical judgment. Scoring was calculated using a 4-point scale (0 = not present; 3 = strongly present). Cronbach’s alphas were as follows: .67 for self-report, .80 for informant-report, and .48 for interviewer-report. Correlations between each pair was as follows: r = .25 (informant and interviewer), r = .35 (self and informant), and r = .38 (self and interviewer).
MDD diagnosis
We assessed MDD using the C-DIS-IV (Robins et al., 1981). This computerized interview is designed to assess all major DSM-IV psychiatric diagnoses. That is, it does not involve a clinical interviewer, but instead participants answer a series of yes or no questions that are administered via on a computer. As part of the C-DIS-IV, participants report on their experience of MDD symptom criteria from the DSM-IV. If applicable, the program administers additional questions to determine whether the symptoms are linked to another diagnosis or a medical condition. Its algorithm uses participants’ responses to calculate whether they met criteria for a current or past MDD diagnosis. It is highly valid, reliable, and has been used in numerous studies (e.g., Blouin, Perez, & Blouin, 1998; Greist et al., 1987).
Depressive symptoms
We used the 21-item Beck Depression Inventory-II (BDI-II; Beck, Steer, & Garbin, 1988) to measure depressive symptoms over the past two weeks. It is a widely used self-report measure of depressive symptoms. Participants rated the severity level of each symptom on a 4-point scale (e.g., 0 = “I do not feel sad,” 3 = I am so sad or unhappy that I can’t stand it”). We summed all items to create a depression score. Cronbach’s alphas across baseline and subsequent follow-ups ranged from .91 to .93.
Covariates
Neuroticism
We used the 48-item neuroticism subscale of the Neuroticism-Extraversion-Openness Personality Inventory-Revised (Neo-PI-R; Costa & McCrae, 2002) to assess self-reported neuroticism (e.g., “I am easily frightened,” “I am known as hot-blooded and quick-tempered”). Cronbach’s alpha was .92.
Borderline personality disorder symptoms
We used the MAPP (Okada & Oltmanns, 2009) to assess self-reported (e.g., “I am impulsive and have done things that could be dangerous to me”) and informant-reported symptoms (e.g., “He/she is impulsive and has done things that could be dangerous to him/her”). We used the SIDP-IV (Pfohl et al., 1997) to assess interviewer-reported symptoms (e.g., “impulsivity in at least two areas that are potentially self-damaging [e.g., spending, sex, substance abuse, reckless driving, binge eating]”). Cronbach’s alphas were .63 for self-report, .73 for informant-report, and .60 for interviewer-report. Correlations between each pair was as follows: r = .20 (self and informant), r = .31 (informant and interviewer), and r = .35 (self and interviewer).
Results
Analysis Plan
We examined how affective instability predicts four indices of depression: lifetime MDE at any time point (baseline, FU5, FU10), first-time MDE (at FU5 or FU10), remission from an MDE (from baseline to FU5, baseline to FU10, or FU5 to FU10), and depressive symptoms. We used baseline MDD diagnosis to identify individuals who experienced a first-time MDE or recovered from an MDE during the study (at FU5 or FU10). We used the following dummy codes: diagnosis (0 = No MDE; 1 = MDE), first-time MDE (0 = No first-time MDE; 1 = first-time MDE), and remission (0 = Not remitted; 1 = In remission).
We conducted multi-level growth curve modeling (GCM) to estimate the impact of affective instability variability on depressive symptoms over time. GCM is appropriate because the dependent variable is a continuous measure, participants have at least three repeated observations, and our sample is at least N = 100 (Curran, Obeidat, & Losardo, 2010). We coded time as 0 = baseline, 1 = 6 months (FU1), 2 = 1 year (FU2), 3 = 1.5 years (FU3), 4 = 2 years (FU4), 5 = 2.5 years (FU5), 6 = 3 years (FU6), 7 = 3.5 years, and 11 = 5.5 years (FU10). We included time, affective instability, and the interaction between time and affective instability as predictors. We only report linear effects of time because there was no non-linear change (i.e., quadratic effect of time) in depressive symptoms. We computed semi-partial R2 values as our index of effect size, which is used for multi-level modeling analyses and represents the proportion of variance explained by a variable (Edwards et al., 2008).
In all analyses, we controlled for neuroticism and BPD symptoms, as well as demographics, including gender (0 = Men, 1 = Women) and race (0 = White, 1 = Black). Although affective instability did not vary by demographics (gender: β = .03; race: β = −.02, ps > .24), we tested for these demographics as potential moderators. We also controlled for lifetime MDD at baseline when predicting depressive symptoms (r = .21, p < .001) to separate the effect of affective instability on symptoms from its effect on diagnosis. Neuroticism was positively correlated with symptoms (r = .30, p < .001). It was also positively correlated with lifetime MDD (r = .12, p < .001), but this correlation was weak. We ran all analyses in R Version 3.4.3.
Does Affective Instability Predict the Course of Depression Later in Life?
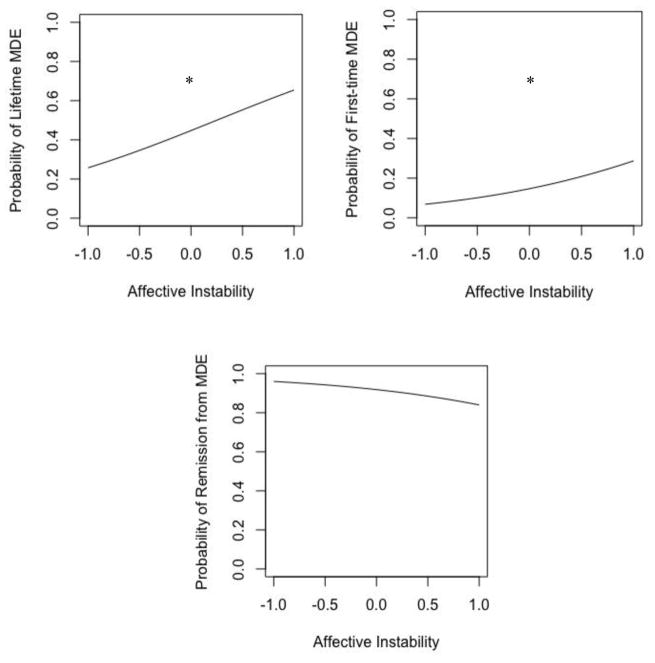
Table 1 and Figure 2 show results from the logistic regression analyses, and Table 2 shows results from the GCM analyses.
Table 1.
Logistic Regression Analyses for Affective Instability Predicting the Course of MDD Diagnosis
| Predictors | Lifetime MDE | First-time MDE | Remission from MDE | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| B (SE) | OR | 95% CI | B (SE) | OR | 95% CI | B (SE) | OR | 95% CI | |
| Intercept | −.166(.12) | −2.10(.24) | 4.87(2.54) | ||||||
| Affective instability | |||||||||
| Self-report | .138(.09) | 1.14 | [.958,1.37] | .080(.14) | 1.08 | [.811,.1.44] | −.115(.24) | .891 | [.548,1.43] |
| Informant-report | .180(.09)† | 1.19 | [.990,1.45] | .096(.16) | 1.10 | [.795,1.51] | .118(.29) | 1.12 | [.641,2.02] |
| Interviewer-report | .146(.08)† | 1.15 | [.984,1.36] | .310(.12)* | 1.36 | [1.05,1.75] | −.191(.18) | .825 | [.573,1.22] |
| Gender | −.206(.14) | .813 | [.614,1.07] | .130(.26) | 1.13 | [.683,1.94] | .573(.45) | 1.77 | [.714,4.39] |
| Race | −.024(.15) | .976 | [.721,1.31] | .458(.24)† | 1.58 | [.969,2.55] | .295(.56) | 1.34 | [.470,4.56] |
| Neuroticism | .152(.07)* | 1.16 | [1.00,1.35] | −.037(.12) | .962 | [.762,1.22] | −.027(.02) | .972 | [.922,1.02] |
| Borderline Personality Disorder | |||||||||
| Self-report | .067(.09) | 1.06 | [.892,1.28] | .293(.14)* | 1.34 | [1.01,1.78] | −.312 (.27) | .731 | [.423,1.27] |
| Informant-report | .204(.09)* | 1.22 | [1.02,1.47] | .356(.15)* | 1.42 | [1.05,1.92] | −.595(.26)* | .551 | [.318,.919] |
| Interviewer-report | .325(.09)* | 1.38 | [1.16,1.66] | .204(.14) | 1.22 | [.922,1.61] | .215(.20) | 1.24 | [.856,1.90] |
Note. B(SE) = unstandardized fixed effects with standard errors in parentheses. OR = odds ratio. 95% CI = 95% confidence intervals. Gender: 0 = Male; 1 = Female. Race: 0 = White; 1 = Black.
Borderline Personality Disorder includes relevant symptoms without the affective instability items.
p < .10,
p < .05.
Figure 2.
This figure illustrates probability curves for affective instability averaged across sources predicting lifetime (top left panel), a first-time MDE (top right panel), and remission from an MDE (bottom panel).
*p < .05.
Table 2.
Multi-level Growth Curve Analyses for Affective Instability Predicting the Course of Depressive Symptoms
| Parameters | Depressive symptoms | ||
|---|---|---|---|
|
| |||
| γ (SE) | 95% CI | Rβ2 | |
| Intercept | 3.79(24) | ||
| Time | .040(.01)* | [.010,.067] | .001 |
| Affective instability | |||
| Self-report | .943(.16)* | [.626,1.26] | .009 |
| Informant-report | .022(.16) | [−.301,.346] | <.001 |
| Interviewer-report | .064 (.14) | [−.220,.350] | <.001 |
| Gender | .222(.25) | [−.274,.719] | <.001 |
| Race | 2.49(.26)* | [1.99,2.99] | .04 |
| Neuroticism | .861(.13)* | [.602,1.12] | .02 |
| Baseline lifetime MDD | 1.82(.27)* | [1.28,2.37] | .02 |
| Borderline Personality Disorder | |||
| Self-report | .837(.15)* | [.537,1.12] | .01 |
| Informant-report | .781(.15)* | [.479,1.08] | .01 |
| Interviewer-report | 1.07(.14)* | [.792,1.34] | .03 |
| Affective instability x time | |||
| Self-report | −.027(.01) | [−.059,.004] | <.001 |
| Informant-report | .022(.01) | [−.009,.054] | <.001 |
| Interviewer-report | .016(.01) | [−.016,.048] | <.001 |
| ICC | 0.67 | ||
Note. γ (SE) = unstandardized fixed effects with standard errors in parentheses. Rβ2 = semi-partial R2. 95% CI = 95% confidence intervals. Time: 0 = baseline, 1 = 6 months (FU1), 2 = 1 year (FU2), 3 = 1.5 years (FU3), 4 = 2 years (FU4), 5 = 2.5 years (FU5), 6 = 3 years (FU6), 7 = 3.5 years, and 11 = 5.5 years (FU10). Gender: 0 = Male, 1 = Female. Race: 0 = White, 1 = Black.
Borderline Personality Disorder includes relevant symptoms without the affective instability items. ICC = intra-class correlation coefficient.
p < .05.
MDD diagnosis
Approximately 43.7% (n = 501/1147) of participants had experienced a past or current MDE at any time point: 25.4% (n = 405/1585) at baseline, 12.2% (n = 151/1237) at FU5 and 10.4% (n = 106/1015) at FU10. At baseline, people in a current MDE had greater affective instability than did those (a) without lifetime MDD at any time point (self-report: t(687) = 6.89, p < .001, 95%CI[.304, 2.70]; informant-report: t(689) = 5.99, p < .001, 95% CI[−3.07, −1.55]; interviewer-report: t(689) = 6.87, p < .001, 95% CI[−1.18, −.65]), and (b) those whose MDDs were in remission, (self-report: t(308) = 2.71, p < .01, 95% CI[.32, 2.07]; informant-report: t(310) = 2.20, p = .02, 95% CI[−.04, 2.45]; interviewer-report: t(310) = 2.63, p < .01, 95% CI[.15, 1.05]). Participants whose MDD was in remission had greater affective instability than did those without lifetime MDD at any time point (self-report: t(706) = 4.59, p < .001, 95% CI[−1.70, −.682]; informant-report: t(708) = 2.30, p = .02, 95% CI−1.41, −.112]; interviewer-report: t(708) = 3.81, p < .001, 95% CI−.670, −.215]).
In terms of first-time MDEs, 14.8% (n = 112/758) of the sample experienced their first-time MDE at FU5 (7%; n = 65/923) or FU10 (5.5%; n = 47/850). Individuals with greater baseline affective instability based on informant and interviewer reports were more likely to experience a lifetime MDE before or during the study. Based on interviewer reports, individuals with greater baseline affective instability also had a greater likelihood of experiencing a first-time MDE.
In terms of remission, 90.7% (n =283/312) of participants who had a current MDE at any time point were in remission at either FU5 or FU10; 72.5% (n = 224/309) of participants who had an MDE at baseline were in remission at FU5 and 76.2% (n = 192/252) were in remission at FU10. No measure of affective instability predicted the likelihood of remission. Race moderated the effect of informant-rated (B = −.395, SE = .17, p = .02, 95% CI[−.740, −.052]) and interviewer-rated (B = .295, SE = .17, p = .09, 95% CI[−.046, .649]) affective instability on lifetime MDE. Specifically, informant-rated (B = .285, SE = .11, p = .01, 95% CI[.057, .515]) affective instability predicted a greater overall likelihood of having a lifetime MDE (as assessed across the study) in Whites, but not in interviewer-rated affective instability predicted a greater likelihood of having a lifetime MDE in Blacks (B = .430, SE = .15, p < .01, 95% CI[.135, .742]). Gender did not moderate the effects of affective instability on lifetime number of MDEs (ps > .27) and neither race nor gender moderated the effects of affective instability on first-time MDEs (ps > .12) or remission (ps > .06).
Depressive symptoms
The stability correlations for depressive symptoms were strong (baseline and FU5: r = .60; baseline and FU10: r = .62; FU5 and FU10: r = .66, p < .001). Growth curve analyses revealed that depressive symptoms increased over the six years (γ = .046, SE = .01, 95% CI[.013, .068], p < .01). Aggregated across time, individuals who reported greater affective instability had greater depressive symptoms. Gender and race did not moderate this effect (ps > .06). Meanwhile, affective instability did not predict the trajectory of depressive symptoms over time. That is, individuals higher in affective instability did not necessarily have worse symptoms six years later. However, there was a significant three-way interaction between self-reported affective instability, time, and gender (γ = −.077, SE = .03, 95% CI[−.148, −.006], p = .03). Simple effects analyses revealed that although self-reported affective instability did not predict the trajectory of depressive symptoms in men (γ = .017, SE = .03, 95% CI[−.043,.079], p = .57), it did in women (γ = −.044, SE = .01, 95% CI[−.083, −.005], p = .02), such that women with greater affective instability showed a decline in depressive symptoms over time. There were no other significant three-way interactions between informant- or interview-reported, affective instability, time, and gender or race (ps > .06).
Discussion
Major Depressive Disorder (MDD) is one of society’s most prevalent and economically burdensome psychiatric disorders (Kessler, 2003). The goals of our study were to (1) investigate how affective instability is associated with the course of MDD and (2) determine its relevance for MDD in later life. Building on previous research (e.g., Peeters et al., 2006), we found that baseline affectively instability positively predicted a greater likelihood of experiencing a first-time MDE as well as depressive symptoms six years later. In addition, we replicated past research that found that those with MDD in remission had greater affective instability than those without a lifetime MDD diagnosis (Thompson et al., 2011); importantly, we also found that those with current MDD have greater affective instability than those whose MDD is in remission. Notably, our findings held even after controlling for neuroticism, one of the most common risk factors for MDD (e.g., Kendler et al., 2004). Thus, there is a distinct utility of affective instability in predicting the course of MDD above and beyond neuroticism. Furthermore, our findings held when taking into account MDD history, demonstrating that the association between affective instability and depressive symptoms was not simply an artifact of having a lifetime MDD diagnosis.
Although our hypotheses that affective instability is positively associated with lifetime MDEs, first-time MDEs, and depressive symptoms were supported, some of our hypotheses were not. In particular, affective instability did not predict an increase in depressive symptoms over time. Thus, even though individuals higher in baseline affective instability still had more depressive symptoms many years later than those lower in affective instability, their symptoms did not get any more worse. Affective instability was also unrelated to remission, such that individuals higher in affective instability were also not less likely to recover from an MDE. These findings highlight the importance of distinguishing between factors that predict distinct aspects of MDD’s course (Hardeveld et al., 2010). Our findings would suggest that affective instability is a risk factor for the onset and reoccurrence of MDD. Thus, affective instability would best be targeted in MDD prevention, as well as secondary prevention efforts, where psychotropic medication remains the primary option (Geddes et al., 2003). In contrast, other affective constructs besides affective instability, such as attention to emotion, may be more important for predicting remission (e.g., Thompson et al., 2013).
Another major contribution of this work is that despite MDD’s decreased prevalence in older adults, affective instability is still linked to MDD later in life. Thus, affective instability may be a key risk factor across adulthood. This is important because the risk factors for MDD often vary by age (Rodda et al., 2011). Another possibility is that rather than being a risk factor, affective instability is a core feature of MDD that is shared by younger and older adults. This kind of work is critical for understanding how MDD manifests across the lifespan. Some studies indicate that older adults are less likely to report affective symptoms than younger adults (Henderson et al., 1993). Affective instability could also be a transdiagnostic factor that explains the comorbidity between MDD and BPD (Shea, Widiger, & Klein, 1992). Furthermore, although examining gender was not our primary focus, the typical gender differences in MDD (Nolen-Hoeksema & Girgus, 1994) did not emerge in this older sample; women were not more likely to have an MDE than men. In general, there were few moderating effects of gender, indicating that affective instability similarly impacts MDD in men and women, at least in older adulthood.
Future Directions and Limitations
A key strength of our study was that we examined how affective instability predicts changes in MDD over time. We assessed affective instability using a variety of measures (self, informant, interviewer) and adopted diagnostic criteria from prior research (Miller & Pilkonis, 2006). Any existing associations showed that MDD was consistently linked to elevated affective instability. This supports prior research, that regardless of the methods used to assess affective instability (e.g., trait-level versus daily-level assessments), there is a positive association with MDD (see meta-analysis by Houben et al. 2016). However, some of our findings were not present for all reporters and for all aspects of MDD. Thus, we recommend that future studies investigate why there might sometimes be discrepancies. Consider the fact that interviewer-reports predicted experiencing a first-time MDE, whereas informant-reports did not. This might be because interviewers are not as influenced by personal experiences with participants and might be more objectively in their assessment. Meanwhile, given that both MDD diagnosis and symptoms were assessed via self-report, future research should use clinical interviews for assessing MDD since this is the gold standard. Furthermore, it will be useful to test whether certain aspects of affective instability are driving the association between affective instability and MDD’s course. A study by Thompson et al. (2011) would suggest that specific facets of affective instability, such as affective variability as opposed to intensity, may be especially relevant.
In addition to including diverse measures of affective instability and clinical interviews for assessing MDD, we also recommend that future studies include repeated assessments. This will help determine whether fluctuations in affective instability correspond to fluctuations in MDD. If affective instability is a symptom of MDD as opposed to a risk factor, then affective instability and MDD should increase and decrease together. Including multiple assessments will also allow for a test of whether decreased affective instability is a reason why MDD is less prevalent in older adulthood. Furthermore, researchers should consider using momentary assessments to capture how affective instability unfolds on a daily basis. This can help capture the mechanisms driving the association between affective instability and MDD.
In addition, while we were one of the first to investigate how affective instability is related to multiple aspects of MDD’s course, we only examined first-time onset, remission, and symptoms. Understanding affective instability’s role in other aspects, such as recurrence will be especially critical because MDD is highly recurrent (Monroe & Harkness, 2010). It will also be important for future studies to replicate our findings in a sample with a wide age range. While affective instability predicted first-time MDEs, the factors that predict first-time MDEs early in life can differ from those that predict first-time MDEs later in life (Rodda et al., 2011).
Lastly, while we examined the association between affective instability and MDD, we did not examine specific mechanisms. For example, compared to healthy controls, individuals with MDD have more negative cognitive biases, such that they are more likely to attend to, interpret, and remember negative stimuli (e.g., Gotlib & Joormann, 2010; Mathews & MacLeod, 2005), which can lead to greater intensity and changes in emotional experience (Thompson et al., 2012). Individuals with MDD (Aldao, Nolen-Hoeksema, & Schweizer, 2010; Liu & Thompson, 2017) and greater affective instability (Kokkonen & Pullkinen, 2001) also tend to use putatively maladaptive emotion regulation strategies, such as rumination (Liu & Thompson, 2017; Nolen-Hoeksema, Wisco, & Lyubomirsky, 2008), that can increase negative emotion (e.g., Gross, 1998). It will be important for future studies to test these and other mechanisms to better understand why affective instability is related to MDD course. Given that people increase in their positive cognitive biases in older adulthood (e.g., Reed, Chan, & Mikels, 2014; Mather & Carstensen, 2005) and have better control over their emotions (English & Carstensen, 2014; Gross et al., 1997; Lawton, Kleban, Rajagopal, & Dean, 1992), it will be especially important to take a lifespan approach when evaluating mechanisms.
Conclusions
Our findings demonstrate that affective instability is predictive of MDD even in older age. Notably, affective instability was related to multiple aspects of MDD’s course, including experiencing a lifetime MDE, a first-time MDE, and greater depressive symptoms, but not to all aspects, such as remission. These findings have important implications for understanding the risk factors associated with MDD and its course across the lifespan.
Highlights.
Affective instability predicts multiple aspects of depression’s course.
Affective instability does not predict remission from depressive episodes.
Affective instability remains a key predictor of depression in older adults.
Acknowledgments
Role of the Funding Source
Funding: This work was supported by the National Institutes of Health (grant numbers R01 MH077840-05, T32 AG00030-32).
We would like to thank Michael Boudreaux, Merlyn Rodrigues, Christina Noel White, and the dozens of other lab members and research assistants who worked hard on this project. We would also like to thank the hundreds of participants who have graciously provided data for the project.
Footnotes
Author Disclosure
Contributors
Lameese Eldesouky (L.E.), Renee J. Thompson (R.J.T.), and Tammy English (T.E.) developed the study concept. Thomas F. Oltmanns (T.F.O.) designed the study and collected the data. L.E. performed the data analysis and interpretation under the supervision of R.J.T, T.F.O, and T.E.. L.E. also drafted the paper and all authors provided critical revisions. All authors contributed to and have approved the final manuscript.
Institutional Review Board
The study presented in this paper was approved by the Institutional Review Board at Washington University in St. Louis.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, … Wang PS. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 2.Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. J Abnormal Psychol. 1998;107:179–192. doi: 10.1037//0021-843x.107.2.179. [DOI] [PubMed] [Google Scholar]
- 3.Hofmann SG, Sawyer AT, Fang A, Asnaani A. Emotion dysregulation model of mood and anxiety disorders. Depress Anxiety. 2012;29:409–416. doi: 10.1002/da.21888. [DOI] [PubMed] [Google Scholar]
- 4.Ehring T, Tuschen-Caffier B, Schnülle J, Fischer S, Gross JJ. Emotion regulation and vulnerability to depression: spontaneous versus instructed use of emotion suppression and reappraisal. Emotion. 2010;10:563–572. doi: 10.1037/a0019010. [DOI] [PubMed] [Google Scholar]
- 5.Garnefski N, Kraaij V. Relationships between cognitive emotion regulation strategies and depressive symptoms: A comparative study of five specific samples. Pers Individ Dif. 2006;40:1659–1669. [Google Scholar]
- 6.Larsen RJ, Diener E. Affect intensity as an individual difference characteristic: A review. J Res Pers. 1987;21:1–39. [Google Scholar]
- 7.Henry C, Mitropoulou V, New AS, Koenigsberg HW, Silverman J, Siever LJ. Affective instability and impulsivity in borderline personality and bipolar II disorders: similarities and differences. J Psychiatr Res. 2001;35:307–312. doi: 10.1016/s0022-3956(01)00038-3. [DOI] [PubMed] [Google Scholar]
- 8.Koenigsberg HW. Affective instability: Toward an integration of neuroscience and psychological perspectives. J Pers Disord. 2010;24:60–82. doi: 10.1521/pedi.2010.24.1.60. [DOI] [PubMed] [Google Scholar]
- 9.Trull TJ, Solhan MB, Tragesser SL, Jahng S, Wood PK, Piasecki TM, Watson D. Affective instability: measuring a core feature of borderline personality disorder with ecological momentary assessment. J Abnormal Psychol. 2008;117:647–661. doi: 10.1037/a0012532. [DOI] [PubMed] [Google Scholar]
- 10.Peeters F, Berkhof J, Delespaul P, Rottenberg J, Nicolson NA. Diurnal mood variation in major depressive disorder. Emotion. 2006;6:383–391. doi: 10.1037/1528-3542.6.3.383. [DOI] [PubMed] [Google Scholar]
- 11.Angst J, Gamma A, Endrass J. Risk factors for the bipolar and depression spectra. Acta Psychiatr Scand. 2003;108:15–19. doi: 10.1034/j.1600-0447.108.s418.4.x. [DOI] [PubMed] [Google Scholar]
- 12.Thompson RJ, Berenbaum H, Bredemeier K. Cross-sectional and longitudinal relations between affective instability and depression. J Affect Disord. 2011;130:53–59. doi: 10.1016/j.jad.2010.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Houben M, Van Den Noortgate W, Kuppens P. The relation between short-term emotion dynamics and psychological well-being: A meta-analysis. Psychol Bull. 2015;141:901–930. doi: 10.1037/a0038822. [DOI] [PubMed] [Google Scholar]
- 14.Brose A, de Roover K, Ceulemans E, Kuppens P. Older adults’ affective experiences across 100 days are less variable and less complex than younger adults’. Psychol Aging. 2015;30:194–208. doi: 10.1037/a0038690. [DOI] [PubMed] [Google Scholar]
- 15.Carstensen LL, Pasupathi M, Mayr U, Nesselroade JR. Emotional experience in everyday life across the adult life span. J Pers Soc Psychol. 2000;79:644–655. [PubMed] [Google Scholar]
- 16.Fiske A, Wetherell JL, Gatz M. Depression in older adults. Annu Rev Clin Psychol. 2009;5:363–389. doi: 10.1146/annurev.clinpsy.032408.153621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rodda J, Walker Z, Carter J. Depression in older adults. Br J Med Res. 2011;343:683–687. doi: 10.1136/bmj.d5219. [DOI] [PubMed] [Google Scholar]
- 18.Monroe SM, Harkness KL. Recurrence in major depression: a conceptual analysis. Psychol Rev. 2011;118:655–674. doi: 10.1037/a0025190. [DOI] [PubMed] [Google Scholar]
- 19.Thompson RJ, Mata J, Jaeggi SM, Buschkuehl M, Jonides J, Gotlib IH. The everyday emotional experience of adults with major depressive disorder: Examining emotional instability, inertia, and reactivity. J Abnormal Psychol. 2012;121:819–829. doi: 10.1037/a0027978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kendler KS, Kuhn J, Prescott CA. The interrelationship of neuroticism, sex, and stressful life events in the prediction of episodes of major depression. Am J Psychiatry. 2004;161:631–636. doi: 10.1176/appi.ajp.161.4.631. [DOI] [PubMed] [Google Scholar]
- 21.Watson D, Wiese D, Vaidya J, Tellegen A. The two general activation systems of affect: Structural findings, evolutionary considerations, and psychobiological evidence. J Pers Soc Psychol. 1999;76:820–838. [Google Scholar]
- 22.Miller JD, Pilkonis PA. Neuroticism and affective instability: The same or different? Am J Psychiatry. 2006;163:839–845. doi: 10.1176/ajp.2006.163.5.839. [DOI] [PubMed] [Google Scholar]
- 23.Miller DJ, Vachon DD, Lynam DR. Neuroticism, negative affect, and negative affect instability: Establishing convergent and discriminant validity using ecological momentary assessment. Pers Individ Dif. 2009;47:873–877. doi: 10.1016/j.paid.2009.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, … Ruan WJ. Prevalence, correlates, disability, and comorbidity of DSM-IV Borderline Personality Disorder: Results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69:533–545. doi: 10.4088/jcp.v69n0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oltmanns TF, Gleason MEJ. Personality, health, and social adjustment in later life. In: Cottler LB, editor. Mental health in public health: The next 100 years. Oxford University Press; New York: 2011. pp. 151–179. [Google Scholar]
- 26.Robins LN, Helzer JE, Croughan J, Ratcliff KS. National Institute of Mental Health diagnostic interview schedule: Its history, characteristics, and validity. Arch Gen Psychiatry. 1981;38:381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- 27.Okada M, Oltmanns TF. Comparison of three self-report measures of personality pathology. J Psychopathol Behav Assess. 2009;31:358–367. doi: 10.1007/s10862-009-9130-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pfohl B, Blum N, Zimmerman M. Structured Interview for DSM-IV Personality: SIDP-IV. American Psychiatric Pub; 1997. [Google Scholar]
- 29.Greist JH, Klein MH, Erdman HP, Bires JK, Bass SM, Machtinger PE, Kresge DG. Comparison of computer-and interviewer-administered versions of the Diagnostic Interview Schedule. Psychiatr Serv. 1987;38:1304–1311. doi: 10.1176/ps.38.12.1304. [DOI] [PubMed] [Google Scholar]
- 30.Blouin AG, Perez EL, Blouin JH. Computerized administration of the diagnostic interview schedule. Psychiatry Res. 1988;23:335–344. doi: 10.1016/0165-1781(88)90024-8. [DOI] [PubMed] [Google Scholar]
- 31.Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- 32.Costa PT, Jr, McCrae RR. Revised NEO Personality Inventory (NEO–PI– R) and NEO Five-Factor Inventory (NEO–FFI) professional manual. Odessa, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- 33.Curran PJ, Obeidat K, Losardo D. Twelve frequently asked questions about growth curve modeling. J Cogn Dev. 2010;11:121–136. doi: 10.1080/15248371003699969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Edwards LJ, Muller KE, Wolfinger RD, Qaqish BF, Schabenberger O. An R2 statistic for fixed effects in the linear mixed model. Stat Med. 2008;27:6137–6157. doi: 10.1002/sim.3429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hardeveld F, Spijker J, De Graaf R, Nolen WA, Beekman ATF. Prevalence and predictors of recurrence of major depressive disorder in the adult population. Acta Psychiatr Scand. 2010;122:184–191. doi: 10.1111/j.1600-0447.2009.01519.x. [DOI] [PubMed] [Google Scholar]
- 36.Geddes JR, Carney SM, Davies C, Furukawa TA, Kupfer DJ, Frank E, Goodwin GM. Relapse prevention with antidepressant drug treatment in depressive disorders: a systematic review. Lancet. 2003;361:653–661. doi: 10.1016/S0140-6736(03)12599-8. [DOI] [PubMed] [Google Scholar]
- 37.Thompson RJ, Mata J, Jaeggi S, Buschkuehl M, Jonides J, Gotlib IH. The role of attention to emotion in recovery from Major Depressive Disorder. Depress Res Treat. 2013;2013:1–6. doi: 10.1155/2013/540726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Henderson AS, Jorm AF, Mackinnon A, Christensen H, Scott LR, Korten AE, Doyle C. The prevalence of depressive disorders and the distribution of depressive symptoms in later life: a survey using Draft ICD-10 and DSM-III-R. Psychol Med. 1993;23:719–729. doi: 10.1017/s0033291700025496. [DOI] [PubMed] [Google Scholar]
- 39.Shea MT, Widiger TA, Klein MH. Comorbidity of personality disorders and depression: implications for treatment. J Consult Clin Psychol. 1992;60:857–868. doi: 10.1037//0022-006x.60.6.857. [DOI] [PubMed] [Google Scholar]
- 40.Nolen-Hoeksema S, Girgus JS. The emergence of gender differences in depression during adolescence. Psychol Bull. 1994;115:424–443. doi: 10.1037/0033-2909.115.3.424. [DOI] [PubMed] [Google Scholar]
- 41.Gotlib IH, Joormann J. Cognition and depression: Current status and future directions. Annu Rev Clin Psychol. 2010;6:285–312. doi: 10.1146/annurev.clinpsy.121208.131305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mathews A, MacLeod C. Cognitive vulnerability to emotional disorders. Annu Rev Clin Psychol. 2005;1:167–195. doi: 10.1146/annurev.clinpsy.1.102803.143916. [DOI] [PubMed] [Google Scholar]
- 43.Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clin Psychol Rev. 2010;30:217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 44.Liu DY, Thompson RJ. Selection and implementation of emotion regulation strategies in major depressive disorder: An integrative review. Clin Psychol Rev. 2017;57:183–194. doi: 10.1016/j.cpr.2017.07.004. [DOI] [PubMed] [Google Scholar]
- 45.Kokkonen M, Pulkkinen LEA. Extraversion and neuroticism as antecedents of emotion regulation and dysregulation in adulthood. Eur J Pers. 2001;15:407–424. [Google Scholar]
- 46.Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking rumination. Perspect Psychol Sci. 2008;3:400–424. doi: 10.1111/j.1745-6924.2008.00088.x. [DOI] [PubMed] [Google Scholar]
- 47.Reed AE, Chan L, Mikels JA. Meta-analysis of the age-related positivity effect: Age differences in preferences for positive over negative information. Psychol Aging. 2014;29:1–15. doi: 10.1037/a0035194. [DOI] [PubMed] [Google Scholar]
- 48.Mather M, Carstensen LL. Aging and motivated cognition: the positivity effect in attention and memory. Trends Cogn Sci. 2005;9:496–502. doi: 10.1016/j.tics.2005.08.005. [DOI] [PubMed] [Google Scholar]
- 49.English T, Carstensen LL. Selective narrowing of social networks across adulthood is associated with improved emotional experience in daily life. Int J Behav Dev. 2014;38:195–202. doi: 10.1177/0165025413515404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gross JJ, Carstensen LL, Pasupathi M, Tsai J, Götestam Skorpen C, Hsu AYC. Emotion and aging: Experience, expression, and control. Psychol Aging. 1997;12:590–599. doi: 10.1037//0882-7974.12.4.590. [DOI] [PubMed] [Google Scholar]
- 51.Lawton MP, Kleban MH, Rajagopal D, Dean J. Dimensions of affective experience in three age groups. Psychol Aging. 1992;7:171–184. doi: 10.1037//0882-7974.7.2.171. [DOI] [PubMed] [Google Scholar]