Abstract
Plant-based diets, defined in terms of low frequency of animal food consumption, have been increasingly recommended for their health benefits. Numerous studies have found plant-based diets, especially when rich in high quality plant foods such as whole grains, fruits, vegetables, and nuts, to be associated with lower risk of cardiovascular outcomes and intermediate risk factors. This review summarizes the current evidence base examining the associations of plant-based diets with cardiovascular endpoints, and discusses the potential biological mechanisms underlying their health effects, practical recommendations and applications of this research, and directions for future research. Healthful plant-based diets should be recommended as an environmentally sustainable dietary option for improved cardiovascular health.
The potentially beneficial role of plant-based diets in cardiovascular health has been increasingly recognized, with a vast and accumulating evidence-base documenting their health effects (1, 2). Complementary findings from studies of individual plant and animal foods as well as their constituent nutrients lend further support to the potential cardio-protective effects of plant-based diets. Most recently, based on a comprehensive review of these studies, the Dietary Guidelines for Americans 2015–2020 (3) included a healthy vegetarian-style dietary pattern in its recommendations of dietary patterns that can be adopted for improved health. In the present review, we will provide an overview of the cardiovascular benefits associated with plant-based diets, while discussing the biological pathways potentially involved, as well as clinical applications and public health implications of these findings.
Definition of plant-based diets
Plant-based diets consist of a diverse family of dietary patterns, defined in terms of low frequency of consumption of animal foods (4). Vegetarian diets are a subset of plant-based diets which exclude intake some or all animal foods entirely. On the extreme end, vegan diets exclude consumption of all animal products. Lacto-vegetarians consume dairy products but no other animal foods, and lacto-ovo-vegetarians consume eggs and dairy products while excluding other animal foods. Pesco-vegetarians or pescetarians consume fish in addition to eggs and dairy, but exclude poultry and red meat from their diet. Some studies have also examined semi-vegetarian diets, which are sometimes defined in terms of exclusion of just red meat (4), and at others times as infrequent intake of poultry and red meat (5).
Instead of defining plant-based diets in terms of the complete exclusion of some or all animal foods as is the case with studies of vegetarianism, a few recent investigations have examined gradations of adherence to a predominantly plant-based diet. The first of these, the pro-vegetarian diet score, was defined by Martinez-Gonzalez et al. (6) as a diet which positively weighs plant foods while negatively weighing animal foods. They conceptualized such a diet as “a progressive and gentle approach to vegetarianism… that incorporates a range of progressively increasing proportions of plant-derived foods and concomitant reductions in animal-derived foods” (6)(p2S). The advantage of such a definition is its wider applicability, as recommendations of moderate dietary changes, such as gradual reductions in animal food intake may be easier to adopt and adhere to than more extreme recommendations, such as complete exclusion of animal foods.
Plant-based diets are usually defined in terms of the proportion and frequency animal foods consumed in the diet, with little consideration given to the types and frequencies of plant foods consumed. However, not all plant foods are the same, and a wide diversity of plant-based diets exists based on the quality of plant foods included in the diet, each with potentially distinct cardio-metabolic effects. We examined two such variations of graded plant-based diets: a healthful plant-based index which positively weighs healthy plant foods (e.g. whole grains, fruits, vegetables, nuts, legumes) (7–10) and negatively weighs less healthy plant foods (e.g. refined grains, potatoes, sugar-sweetened beverages [SSBs]) (11–15) and animal foods; and an unhealthful plant-based diet index, which positively weighs less healthy plant foods and negatively weighs healthy plant foods and animal foods. We found varying cardio-metabolic effects of these diet indices (16, 17), pointing to the importance of defining plant-based diets in terms of the quality of plant foods they emphasize.
Associations with cardiovascular endpoints and intermediate risk factors
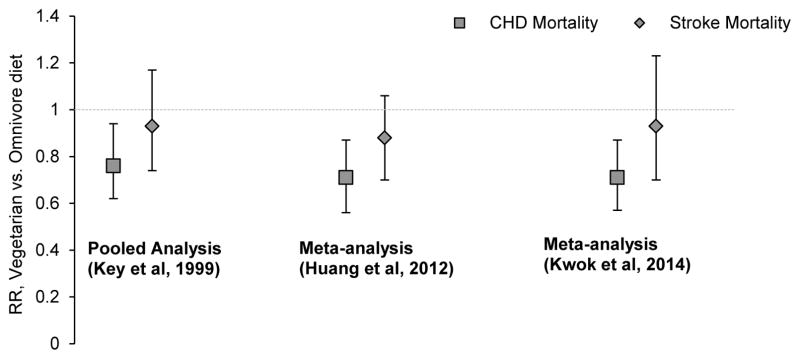
Despite the wide variation in the definitions of plant-based diets in the literature, their associations with cardiovascular endpoints in prospective cohort studies have been fairly consistent. Most studies of vegetarian diets have been carried out in Europe, with one study in Japan, and three studies among Seventh Day Adventists in the US. In a pooled analysis of 5 of the above cohorts, Key et al. (18) found a 24% (95% Confidence Interval [CI]: 6%–38%) lower rate of coronary heart disease (CHD) mortality among vegetarians relative to omnivores, although they didn’t find any association with stroke mortality; two recent meta-analyses which included more studies found similar results (Figure 1) (19, 20). In many of these studies, the inverse associations were stronger among younger participants, among participants with a longer duration of adherence to a vegetarian diet, and among men relative to women. In particular, the most recent meta-analysis found a 22% (95% CI: 12%–31%) lower rate of stroke mortality among vegetarian men relative to their omnivore counterparts, but the association was not significant among women (20).
Figure 1.
Summary effect estimates (95% CI) of pooled and meta-analyses of vegetarian diets in relation to CHD or stroke mortality7–9
CHD, Coronary Heart Disease; CI, Confidence Interval; RR, Relative Risk
Studies of graded plant-based diet indices have also found similar results. Comparing the highest with the lowest category of adherence, Martinez-Gonzalez et al. (6) found a pro-vegetarian diet score to be associated with a lower rate of cardiovascular mortality (Hazard Ratio [HR]: 0.47; 95% CI: 0.21 to 1.04; p-trend=0.039) over a median follow-up of 5 years in the PREDIMED trial in Spain. Over a longer duration of follow-up (median=12.8 years) in a large European cohort, Lassale et al. (21) found a 20% (95% CI: 7%–30%) lower cardiovascular death rate comparing extreme categories. Recently, we conducted a similar analysis in more than 200,000 male and female health professionals in the Nurses Health Studies and the Health Professionals Follow-up Study in the US (Figure 2) (17). An overall plant-based diet index (similar to the pro-vegetarian diet score) was modestly inversely associated with incident CHD (HR comparing extreme deciles: 0.92; 95% CI: 0.83 to 1.01; p-trend=0.003). This inverse association was substantially stronger for a healthful version of this graded plant-based diet index (HR comparing extreme deciles: 0.75; 95% CI: 0.68 to 0.83; p-trend<0.001). However, the association was positive for an unhealthful version of the index (HR comparing extreme deciles: 1.32; 95% CI: 1.20 to 1.46; p-trend<0.001).
Figure 2.
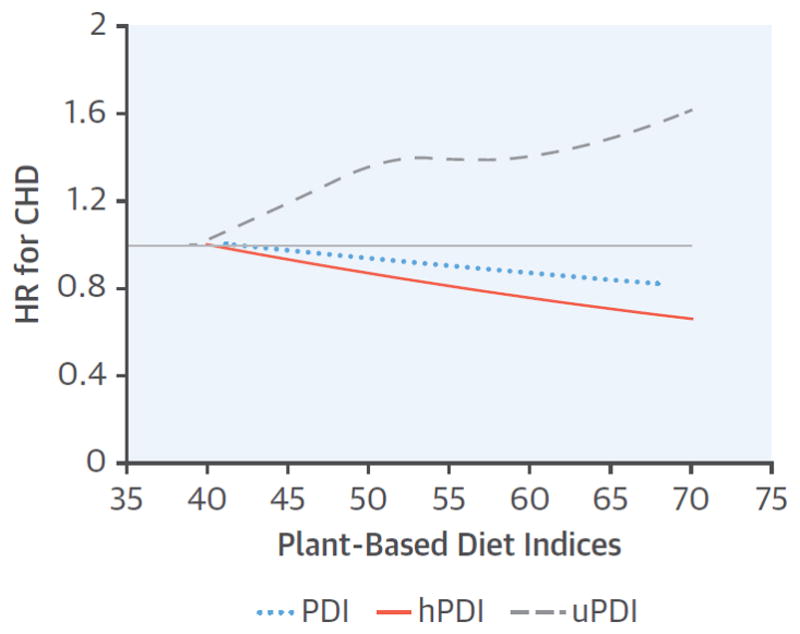
Dose-response relationship of plant-based diet indices with CHD incidence6
CHD, Coronary Heart Disease; HR, Hazard Ratio; PDI, Overall Plant-based Diet Index; hPDI, Healthful Plant-based Diet Index; uPDI, Unhealthful Plant-based Diet Index
For uPDI, p for test of curvature = 0.01 and p for nonlinear association <0.001. The p values for test of curvature for PDI = 0.25, and for hPDI = 0.82. The p values for linearity = 0.001 for PDI, and <0.001 for hPDI.
Reprinted from J Am Coll Cardiol, 70, Satija et al., Healthful and Unhealthful Plant-Based Diets and the Risk of Coronary Heart Disease in U.S. Adults, 411–422, Copyright (2017), with permission from Elsevier
Given the likely long induction periods of cardiovascular diseases, especially with respect to their dietary etiology, plant-based diets have not been examined in randomized controlled trials (RCTs) of hard cardiovascular endpoints. Nevertheless, several RCTs have examined the effect of vegetarian diets on intermediate risk factors of cardiovascular diseases (Table 1). In a meta-analysis of RCTs, Wang et al. (22) found vegetarian diets to significantly lower blood concentrations of total, LDL, HDL, and non-HDL cholesterol relative to a range of omnivorous control diets. Other meta-analyses have found vegetarian diets to lower blood pressure, enhance weight loss, and improve glycemic control to greater extent than omnivorous comparison diets (23–25). Taken together, the beneficial effects of such diets on established proximal determinants of cardiovascular diseases found in RCTs, and their inverse associations with hard cardiovascular endpoints found in prospective cohort studies provide strong support for the adoption of healthful plant-based diets for cardiovascular disease prevention.
Table 1.
Summary effect estimates of meta-analyses of RCTs examining the effects vegetarian diets on cardiovascular risk factors
| Author (year) | Endpoint | Types of control diets | Summary effect estimate comparing vegetarian with control diets |
|---|---|---|---|
| Wang (2015) (22) | Total cholesterol | Usual diet, ADA diet, Prudent diet with lean meat, Low fat diet, Diabetic diet | −0.36 mmol/L (−0.55, −0.17)* |
| LDL cholesterol | −0.34 mmol/L (−0.57, −0.11)* | ||
| HDL cholesterol | −0.10 mmol/L (−0.14, −0.06)* | ||
| Triglycerides | 0.04 mmol/L (−0.05, 0.13) | ||
| Non-HDL cholesterol | −0.30 mmol/L (−0.50, −0.10)* | ||
| Yokoyama (2014) (23) | Systolic blood pressure† | Usual diet, Prudent diet with lean meat, Low fat diet | −4.8 mmHg (−6.6, −3.1)* |
| Diastolic blood pressure† | −2.2 mmHg (−3.5, −1.0)* | ||
| Huang (2015) (24) | Body weight | Usual diet, Diabetic diet, Low fat diet, NCEP diet, Low carb diet, High carb diet, High protein (from meat) diet | −2.02 kg (−2.80, −1.23)* |
| Yokoyama (2014) (25) | HbA1c†† | Usual diet, ADA diet, Low fat diet, Diabetic diet | −0.39% (−0.62, −0.15)* |
| Fasting blood glucose | −0.36 mmol/L (−1.04, 0.32) |
RCT, Randomized Controlled Trial; LDL, Low-Density Lipoprotein; HDL, High-density lipoprotein; HbA1c, glycated hemoglobin; ADA, American Diabetes Association; NCEP, National Cholesterol Education Program
P value<0.05
1 trial out of 7 trials was non-randomized
2 trials out of 5 trials were non-randomized
Potential biological mechanisms
A healthful plant-based diet, which emphasizes intake of whole grains, fruits, vegetables, nuts and legumes, tea and coffee, and non-hydrogenated vegetable oils, might affect cardiovascular health through numerous potential biological pathways (Figure 3). Such a diet is likely to be low in energy density due to its low saturated fat and high fiber content, which could help with weight loss and long-term weight maintenance. In particular, dietary fiber might lower energy intake by triggering satiety cues such as increased gastric distention, likely caused by the augmented chewing of fibrous foods, together with gel formation due to water absorption by soluble fiber (26). The viscous gel formation by soluble fiber may also delay gastric emptying and prolong nutrient absorption, further promoting satiety and moderating post-prandial insulinemic and glycemic responses (26). Another key mechanism through which dietary fiber may improve cardiovascular health is through its potential cholesterol lowering effect. In a meta-analysis of RCTs, a 2–10 g/day increase in soluble fiber intake resulted in a modest but significant −0.057 mmol/L decrease in LDL cholesterol (95% CI: −0.070, −0.044 mmol/L) (27), probably mediated by lower cholesterol and fat absorption, altered cholesterol synthesis, increased bile acid synthesis, and decreased bile acid absorption (28).
Figure 3.
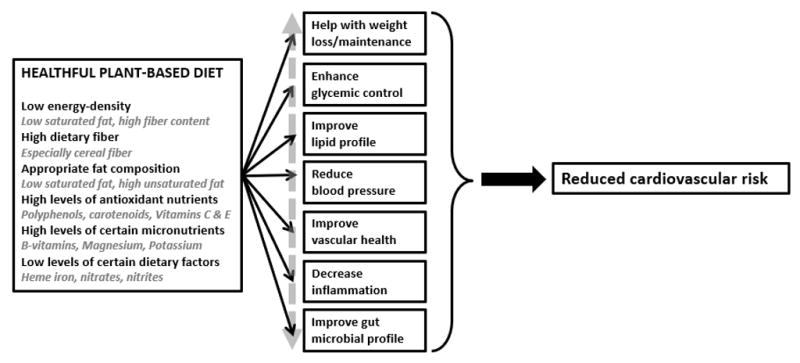
Potential mechanisms underlying the cardiovascular effects of healthful plant-based diets
The low saturated fat and high unsaturated fat contents of a healthful plant-based diet may lower CVD risk by improving the blood lipid profile. In meta-analyses of RCTs, replacing saturated fatty acids with polyunsaturated fatty acids lowered total:HDL cholesterol ratio (29), as well as CHD risk (30) in a dose response manner, with similar results observed in prospective cohort studies (31). In vitro studies have shown saturated fatty acids to activate the pro-inflammatory TLR4 signaling pathway (32). Saturated fatty acids may also interact with the gut microbiome to promote the translocation of lipopolysaccharide (LPS), a potent pro-inflammatory endotoxin, into the bloodstream (33). On the other hand, there is some evidence that polyunsaturated fatty acids activate anti-inflammatory pathways (34, 35). Thus, a high unsaturated fat and low saturated fat diet may also lower CVD risk through its potential anti-inflammatory effects. Replacing saturated fats with polyunsaturated and monounsaturated fats may also enhance insulin sensitivity and prevent type 2 diabetes, possibly through altering cell membrane fatty acid composition and hence cell membrane function, moderating gene expression and enzyme activity, and mediating the inflammatory response (32).
Plant foods such as whole grains, fruits, vegetables, vegetable oils, nuts, tea, coffee, and cocoa are also rich in polyphenols, natural bioactive compounds produced by plants as secondary metabolites essential for plant physiology (36). The numerous individual polyphenols are classified into four major classes based on structure, which account for most of the polyphenols found in human diet: flavonoids, lignans, phenolic acids, and stilbenes (37). The antioxidant capacity of such polyphenol compounds, largely through their role in scavenging and neutralizing free oxygen and nitrogen species and protecting against oxidative stress is known from in vitro studies (37). This antioxidant capacity, potentially together with their ability to modulate nitric oxide (NO) production, enables polyphenol compounds to help maintain vascular homeostasis (38). Polyphenols might also contribute to improved cardiovascular health through their roles in inhibiting platelet aggregation, reducing vascular inflammation, modulating apoptotic processes, limiting LDL oxidation, and improving lipid profile (38, 39). A healthful plant-based diet is also replete with numerous other antioxidant nutrients such as vitamins C and E and beta-carotene; potassium which has been shown to reduce blood pressure and lower stroke risk through its beneficial effects on endothelial function and vascular homeostasis (40, 41); and magnesium which has been associated with improved cardio-metabolic outcomes due to its effects on glucose metabolism and insulin sensitivity, and its anti-inflammatory, vasodilatory, and antiarrhythmic properties (42, 43).
On the other hand, several dietary factors that are abundant in animal foods have been associated with increased risk of cardiovascular endpoints. For instance, heme iron, found mainly in animal foods such as red meat, poultry, and seafood, has been associated with higher risk of cardiovascular endpoints in several prospective cohort studies (44–48). It is postulated that the oxidative potential of iron resulting in the production of reactive oxygen species and oxidative stress, couple with the higher absorption and bioavailability of heme iron could mediate this association (45). Other nutrients used to preserve processed meats, such as sodium, nitrates, and nitrites may also increase risk of cardiovascular outcomes through raised blood pressure, impaired insulin response, and endothelial dysfunction (49).
The gut microbiome represents another novel pathway through which a healthful plant-based diet may influence cardiovascular risk. The complex community of microorganisms that reside in the human gut metabolizes otherwise undigestible dietary substrates to potentially influence the cardiovascular health of the human host (50, 51). An example of this is the trimethylamine N-oxide (TMAO) pathway. Choline and L-carnitine, compounds derived mainly from animal foods such as red meat, poultry, and fish are broken down by gut microbes to generate trimethylamine (TMA), which is further broken down to TMAO in the liver (52). TMAO has been associated with a higher risk of cardiovascular events independent of traditional risk factors, and it is postulated that it influences cardiac health through its effects on cholesterol and sterol metabolism, inflammation, and thrombotic and atherosclerotic pathways (53). Given that a recent study found no correlation between TMAO and dietary factors (54), it is possible that associations of animal foods with cardiac risk through the TMAO pathway are modified by level of dietary intake of foods rich in TMAO precursors, as well as by gut microbial composition. Plant foods are also rich in certain TMAO precursors such as betaine. However, in animal models, certain plant compounds (e.g. resveratrol) have been found to potentially inhibit TMAO production (55, 56). Plant-based diets differ from animal-based diets with respect to many other microbe-dependent metabolic pathways as well, including increased metabolism of fiber and polyphenols, and decreased metabolism of bile acids and amino acids (57–59), which could mediate their inverse associations with cardiovascular endpoints. Larger studies with longer follow-up and repeat assessments of diet, the metabolome, and the microbiome are needed to clarify the likely complicated pathways through which diet interacts with the gut microbial environment to impact cardiovascular health.
Conclusions
Plant-based diets, defined in terms of varying degrees of restrictions on animal food consumption, have been associated with lower risk of cardiovascular diseases as well as an improved cardiovascular risk profile. In addition, numerous biological mechanisms exist through which healthful plant foods may exert their potentially cardio-protective effects. However, there has been some concern about the nutritional adequacy of vegetarian diets, especially vegan diets which completely exclude all animal foods. While the bioavailability of certain nutrients such as iron, zinc, and vitamin A (obtained from conversion of carotenoids) is lower in plant than animal foods, these nutrients can be obtained in the recommended amounts in well planned vegan diets which include a wide variety of healthful plant foods (60). Other nutrients such as vitamins B12 and D are mostly found in animal foods; however, use of supplements, consumption of fortified foods, and in the case of vitamin D, sunlight exposure can ensure adequate levels in vegans (60). The Academy of Nutrition and Dietetics (60), the American Heart Association (61), and the 2015–2020 Dietary Guidelines for Americans (3) recommend appropriately planned vegetarian diets for improved health.
The consistent beneficial associations observed with a wide variation of plant-based diets also allows for personalized and culturally relevant applications of dietary recommendations. For individuals who prefer not to consume certain or most animal foods, healthful and well-planned plant-based meals can provide adequate nutrition and cardiovascular benefits. For those who prefer a more moderate approach, health benefits may be observed even with gradual reductions in animal food intake when replaced with healthy plant foods. For all types of plant-based diets however, it is crucial that the choice of plant foods is given careful consideration. Individuals should choose whole grains over refined grains, whole fruits over fruit juices, unrefined vegetable oils over partially hydrogenated versions, and healthful and unsweetened beverages such as water, tea, and coffee over sweetened beverages, while reducing potatoes/French fries and foods with added sugar. A wider adoption of healthful plant-based diets and a decrease in intake of animal foods, in particular red meat, would also have favorable environmental impacts, as production of plant foods requires fewer natural resources with lower greenhouse gas emissions than that of animal foods (62–64).
In conclusion, considerable evidence supports the cardiovascular benefits of healthful plant-based diets, and these diets and their constituent foods are getting increasing recognition in dietary recommendations. Future research should examine policy strategies to translate the findings of these studies to the wider population, and further explore mechanistic pathways through which healthful plant-based diets may improve cardiovascular health.
Acknowledgments
Funding: AS was supported by American Heart Association Grant #16POST29660000. FBH is supported by NIH grants HL60712 and HL118264.
Footnotes
Conflicts of interest: The authors have no conflicts of interests to declare
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Patel H, Chandra S, Alexander S, Soble J, Williams KA. Plant-Based Nutrition: An Essential Component of Cardiovascular Disease Prevention and Management. Current Cardiology Reports. 2017;19(10):104. doi: 10.1007/s11886-017-0909-z. [DOI] [PubMed] [Google Scholar]
- 2.Kahleova H, Levin S, Barnard N. Cardio-Metabolic Benefits of Plant-Based Diets. Nutrients. 2017;9(8):848. doi: 10.3390/nu9080848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015 – 2020 Dietary Guidelines for Americans. 2015 Available from: http://health.gov/dietaryguidelines/2015/guidelines/
- 4.Li D. Effect of the vegetarian diet on non-communicable diseases. J Sci Food Agric. 2013 doi: 10.1002/jsfa.6362. [DOI] [PubMed] [Google Scholar]
- 5.Tonstad S, Stewart K, Oda K, Batech M, Herring RP, Fraser GE. Vegetarian diets and incidence of diabetes in the Adventist Health Study-2. Nutr Metab Cardiovasc Dis. 2013;23(4):292–9. doi: 10.1016/j.numecd.2011.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martinez-Gonzalez MA, Sanchez-Tainta A, Corella D, Salas-Salvado J, Ros E, Aros F, et al. A provegetarian food pattern and reduction in total mortality in the Prevencion con Dieta Mediterranea (PREDIMED) study. Am J Clin Nutr. 2014;100(Suppl 1):320S–8S. doi: 10.3945/ajcn.113.071431. [DOI] [PubMed] [Google Scholar]
- 7.Aune D, Giovannucci E, Boffetta P, Fadnes LT, Keum N, Norat T, et al. Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality-a systematic review and dose-response meta-analysis of prospective studies. Int J Epidemiol. 2017;46(3):1029–56. doi: 10.1093/ije/dyw319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miller V, Mente A, Dehghan M, Rangarajan S, Zhang X, Swaminathan S, et al. Fruit, vegetable, and legume intake, and cardiovascular disease and deaths in 18 countries (PURE): a prospective cohort study. Lancet. 2017;390(10107):2037–49. doi: 10.1016/S0140-6736(17)32253-5. [DOI] [PubMed] [Google Scholar]
- 9.Benisi-Kohansal S, Saneei P, Salehi-Marzijarani M, Larijani B, Esmaillzadeh A. Whole-Grain Intake and Mortality from All Causes, Cardiovascular Disease, and Cancer: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies. Adv Nutr. 2016;7(6):1052–65. doi: 10.3945/an.115.011635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Luo C, Zhang Y, Ding Y, Shan Z, Chen S, Yu M, et al. Nut consumption and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality: a systematic review and meta-analysis. Am J Clin Nutr. 2014 doi: 10.3945/ajcn.113.076109. [DOI] [PubMed] [Google Scholar]
- 11.Barclay AW, Petocz P, McMillan-Price J, Flood VM, Prvan T, Mitchell P, et al. Glycemic index, glycemic load, and chronic disease risk--a meta-analysis of observational studies. Am J Clin Nutr. 2008;87(3):627–37. doi: 10.1093/ajcn/87.3.627. [DOI] [PubMed] [Google Scholar]
- 12.Huang C, Huang J, Tian Y, Yang X, Gu D. Sugar sweetened beverages consumption and risk of coronary heart disease: a meta-analysis of prospective studies. Atherosclerosis. 2014;234(1):11–6. doi: 10.1016/j.atherosclerosis.2014.01.037. [DOI] [PubMed] [Google Scholar]
- 13.Yang Q, Zhang Z, Gregg EW, Flanders WD, Merritt R, Hu FB. Added sugar intake and cardiovascular diseases mortality among US adults. JAMA Intern Med. 2014;174(4):516–24. doi: 10.1001/jamainternmed.2013.13563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hu EA, Pan A, Malik V, Sun Q. White rice consumption and risk of type 2 diabetes: meta-analysis and systematic review. BMJ. 2012;344:e1454. doi: 10.1136/bmj.e1454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Muraki I, Rimm EB, Willett WC, Manson JE, Hu FB, Sun Q. Potato Consumption and Risk of Type 2 Diabetes: Results From Three Prospective Cohort Studies. Diabetes Care. 2016;39(3):376–84. doi: 10.2337/dc15-0547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Satija A, Bhupathiraju SN, Rimm EB, Spiegelman D, Chiuve SE, Borgi L, et al. Plant-Based Dietary Patterns and Incidence of Type 2 Diabetes in US Men and Women: Results from Three Prospective Cohort Studies. PLoS Med. 2016;13(6):e1002039. doi: 10.1371/journal.pmed.1002039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Satija A, Bhupathiraju SN, Spiegelman D, Chiuve SE, Manson JE, Willett W, et al. Healthful and Unhealthful Plant-Based Diets and the Risk of Coronary Heart Disease in U.S. Adults. J Am Coll Cardiol. 2017;70(4):411–22. doi: 10.1016/j.jacc.2017.05.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Key TJ, Fraser GE, Thorogood M, Appleby PN, Beral V, Reeves G, et al. Mortality in vegetarians and nonvegetarians: detailed findings from a collaborative analysis of 5 prospective studies. Am J Clin Nutr. 1999;70(3 Suppl):516S–24S. doi: 10.1093/ajcn/70.3.516s. [DOI] [PubMed] [Google Scholar]
- 19.Huang T, Yang B, Zheng J, Li G, Wahlqvist ML, Li D. Cardiovascular Disease Mortality and Cancer Incidence in Vegetarians: A Meta-Analysis and Systematic Review. Ann Nutr Metab. 2012;60(4):233–40. doi: 10.1159/000337301. [DOI] [PubMed] [Google Scholar]
- 20.Kwok CS, Umar S, Myint PK, Mamas MA, Loke YK. Vegetarian diet, Seventh Day Adventists and risk of cardiovascular mortality: a systematic review and meta-analysis. Int J Cardiol. 2014;176(3):680–6. doi: 10.1016/j.ijcard.2014.07.080. [DOI] [PubMed] [Google Scholar]
- 21.Lassale C, Beulens J, Van der Schouw Y, Roswall N, Weiderpass E, Romaguera D, et al. Abstract 16: A Pro-Vegetarian Food Pattern and Cardiovascular Mortality in the Epic Study (abstr) Circulation. 2015;131(Suppl 1):A16. [Google Scholar]
- 22.Wang F, Zheng J, Yang B, Jiang J, Fu Y, Li D. Effects of Vegetarian Diets on Blood Lipids: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Journal of the American Heart Association. 2015;4(10) doi: 10.1161/JAHA.115.002408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yokoyama Y, Nishimura K, Barnard ND, Takegami M, Watanabe M, Sekikawa A, et al. Vegetarian diets and blood pressure: A meta-analysis. JAMA Intern Med. 2014;174(4):577–87. doi: 10.1001/jamainternmed.2013.14547. [DOI] [PubMed] [Google Scholar]
- 24.Huang RY, Huang CC, Hu FB, Chavarro JE. Vegetarian Diets and Weight Reduction: a Meta-Analysis of Randomized Controlled Trials. J Gen Intern Med. 2016;31(1):109–16. doi: 10.1007/s11606-015-3390-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yokoyama Y, Barnard ND, Levin SM, Watanabe M. Vegetarian diets and glycemic control in diabetes: a systematic review and meta-analysis. Cardiovascular Diagnosis and Therapy. 2014;4(5):373–82. doi: 10.3978/j.issn.2223-3652.2014.10.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Howarth NC, Saltzman E, Roberts SB. Dietary fiber and weight regulation. Nutr Rev. 2001;59(5):129–39. doi: 10.1111/j.1753-4887.2001.tb07001.x. [DOI] [PubMed] [Google Scholar]
- 27.Brown L, Rosner B, Willett WW, Sacks FM. Cholesterol-lowering effects of dietary fiber: a meta-analysis. Am J Clin Nutr. 1999;69(1):30–42. doi: 10.1093/ajcn/69.1.30. [DOI] [PubMed] [Google Scholar]
- 28.Smith CE, Tucker KL. Health benefits of cereal fibre: a review of clinical trials. Nutr Res Rev. 2011;24(1):118–31. doi: 10.1017/S0954422411000023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mensink RP, Zock PL, Kester AD, Katan MB. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. The American Journal of Clinical Nutrition. 2003;77(5):1146–55. doi: 10.1093/ajcn/77.5.1146. [DOI] [PubMed] [Google Scholar]
- 30.Mozaffarian D, Micha R, Wallace S. Effects on coronary heart disease of increasing polyunsaturated fat in place of saturated fat: a systematic review and meta-analysis of randomized controlled trials. PLoS Med. 2010;7(3):e1000252. doi: 10.1371/journal.pmed.1000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jakobsen MU, O’Reilly EJ, Heitmann BL, Pereira MA, Balter K, Fraser GE, et al. Major types of dietary fat and risk of coronary heart disease: a pooled analysis of 11 cohort studies. Am J Clin Nutr. 2009;89(5):1425–32. doi: 10.3945/ajcn.2008.27124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Risérus U, Willett WC, Hu FB. Dietary fats and prevention of type 2 diabetes. Prog Lipid Res. 2009;48(1):44–51. doi: 10.1016/j.plipres.2008.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fritsche KL. The Science of Fatty Acids and Inflammation. Advances in Nutrition: An International Review Journal. 2015;6(3):293S–301S. doi: 10.3945/an.114.006940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Petersson H, Basu S, Cederholm T, Risérus U. Serum fatty acid composition and indices of stearoyl-CoA desaturase activity are associated with systemic inflammation: longitudinal analyses in middle-aged men. Br J Nutr. 2008;99(6):1186–9. doi: 10.1017/S0007114507871674. [DOI] [PubMed] [Google Scholar]
- 35.Willett WC. The role of dietary n-6 fatty acids in the prevention of cardiovascular disease. J Cardiovasc Med (Hagerstown) 2007;8(Suppl 1):S42–5. doi: 10.2459/01.JCM.0000289275.72556.13. [DOI] [PubMed] [Google Scholar]
- 36.Duthie GG, Gardner PT, Kyle JAM. Plant polyphenols: are they the new magic bullet? Proc Nutr Soc. 2007;62(3):599–603. doi: 10.1079/PNS2003275. [DOI] [PubMed] [Google Scholar]
- 37.Tangney C, Rasmussen HE. Polyphenols, Inflammation, and Cardiovascular Disease. Current atherosclerosis reports. 2013;15(5):324. doi: 10.1007/s11883-013-0324-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Quiñones M, Miguel M, Aleixandre A. Beneficial effects of polyphenols on cardiovascular disease. Pharmacol Res. 2013;68(1):125–31. doi: 10.1016/j.phrs.2012.10.018. [DOI] [PubMed] [Google Scholar]
- 39.Vita JA. Polyphenols and cardiovascular disease: effects on endothelial and platelet function. The American Journal of Clinical Nutrition. 2005;81(1):292S–7S. doi: 10.1093/ajcn/81.1.292S. [DOI] [PubMed] [Google Scholar]
- 40.Aaron KJ, Sanders PW. Role of Dietary Salt and Potassium Intake in Cardiovascular Health and Disease: A Review of the Evidence. Mayo Clin Proc. 2013;88(9):987–95. doi: 10.1016/j.mayocp.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Aburto NJ, Hanson S, Gutierrez H, Hooper L, Elliott P, Cappuccio FP. Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. BMJ. 2013;346:f1378. doi: 10.1136/bmj.f1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Volpe SL. Magnesium in disease prevention and overall health. Adv Nutr. 2013;4(3):378s–83s. doi: 10.3945/an.112.003483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kolte D, Vijayaraghavan K, Khera S, Sica DA, Frishman WH. Role of magnesium in cardiovascular diseases. Cardiol Rev. 2014;22(4):182–92. doi: 10.1097/CRD.0000000000000003. [DOI] [PubMed] [Google Scholar]
- 44.Ascherio A, Willett WC, Rimm EB, Giovannucci EL, Stampfer MJ. Dietary iron intake and risk of coronary disease among men. Circulation. 1994;89(3):969–74. doi: 10.1161/01.cir.89.3.969. [DOI] [PubMed] [Google Scholar]
- 45.Qi L, van Dam RM, Rexrode K, Hu FB. Heme Iron From Diet as a Risk Factor for Coronary Heart Disease in Women With Type 2 Diabetes. Diabetes Care. 2007;30(1):101–6. doi: 10.2337/dc06-1686. [DOI] [PubMed] [Google Scholar]
- 46.de Oliveira Otto MC, Alonso A, Lee D-H, Delclos GL, Bertoni AG, Jiang R, et al. Dietary Intakes of Zinc and Heme Iron from Red Meat, but Not from Other Sources, Are Associated with Greater Risk of Metabolic Syndrome and Cardiovascular Disease. The Journal of Nutrition. 2012;142(3):526–33. doi: 10.3945/jn.111.149781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.van der ADL, Peeters PHM, Grobbee DE, Marx JJM, van der Schouw YT. Dietary haem iron and coronary heart disease in women. Eur Heart J. 2005;26(3):257–62. doi: 10.1093/eurheartj/ehi027. [DOI] [PubMed] [Google Scholar]
- 48.Lee D-H, Folsom AR, Jacobs DR. Iron, zinc, and alcohol consumption and mortality from cardiovascular diseases: the Iowa Women’s Health Study. The American Journal of Clinical Nutrition. 2005;81(4):787–91. doi: 10.1093/ajcn/81.4.787. [DOI] [PubMed] [Google Scholar]
- 49.Micha R, Wallace SK, Mozaffarian D. Red and Processed Meat Consumption and Risk of Incident Coronary Heart Disease, Stroke, and Diabetes Mellitus: A Systematic Review and Meta-Analysis. Circulation. 2010;121(21):2271–83. doi: 10.1161/CIRCULATIONAHA.109.924977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Structure, function and diversity of the healthy human microbiome. Nature. 2012;486(7402):207–14. doi: 10.1038/nature11234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.De Filippo C, Cavalieri D, Di Paola M, Ramazzotti M, Poullet JB, Massart S, et al. Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc Natl Acad Sci U S A. 2010;107(33):14691–6. doi: 10.1073/pnas.1005963107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rak K, Rader DJ. Cardiovascular disease: the diet-microbe morbid union. Nature. 2011;472(7341):40–1. doi: 10.1038/472040a. [DOI] [PubMed] [Google Scholar]
- 53.Heianza Y, Ma W, Manson JE, Rexrode KM, Qi L. Gut Microbiota Metabolites and Risk of Major Adverse Cardiovascular Disease Events and Death: A Systematic Review and Meta-Analysis of Prospective Studies. Journal of the American Heart Association. 2017;6(7):e004947. doi: 10.1161/JAHA.116.004947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kuhn T, Rohrmann S, Sookthai D, Johnson T, Katzke V, Kaaks R, et al. Intra-individual variation of plasma trimethylamine-N-oxide (TMAO), betaine and choline over 1 year. Clin Chem Lab Med. 2017;55(2):261–8. doi: 10.1515/cclm-2016-0374. [DOI] [PubMed] [Google Scholar]
- 55.Chen ML, Yi L, Zhang Y, Zhou X, Ran L, Yang J, et al. Resveratrol Attenuates Trimethylamine-N-Oxide (TMAO)-Induced Atherosclerosis by Regulating TMAO Synthesis and Bile Acid Metabolism via Remodeling of the Gut Microbiota. mBio. 2016;7(2):e02210–15. doi: 10.1128/mBio.02210-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wang Z, Roberts AB, Buffa JA, Levison BS, Zhu W, Org E, et al. Non-lethal Inhibition of Gut Microbial Trimethylamine Production for the Treatment of Atherosclerosis. Cell. 2015;163(7):1585–95. doi: 10.1016/j.cell.2015.11.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Glick-Bauer M, Yeh MC. The health advantage of a vegan diet: Exploring the gut microbiota connection. Nutrients. 2014;6(11):4822–38. doi: 10.3390/nu6114822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Blaut M, Clavel T. Metabolic diversity of the intestinal microbiota: implications for health and disease. J Nutr. 2007;137(3 Suppl 2):751s–5s. doi: 10.1093/jn/137.3.751S. [DOI] [PubMed] [Google Scholar]
- 59.Hooper LV, Midtvedt T, Gordon JI. How host-microbial interactions shape the nutrient environment of the mammalian intestine. Annual review of nutrition. 2002;22:283–307. doi: 10.1146/annurev.nutr.22.011602.092259. [DOI] [PubMed] [Google Scholar]
- 60.Melina V, Craig W, Levin S. Position of the Academy of Nutrition and Dietetics: Vegetarian Diets. Journal of the Academy of Nutrition and Dietetics. 116(12):1970–80. doi: 10.1016/j.jand.2016.09.025. [DOI] [PubMed] [Google Scholar]
- 61.AHA. American Heart Association: Vegetarian Diets. Available from: http://www.heart.org/HEARTORG/HealthyLiving/HealthyEating/Vegetarian-Diets_UCM_306032_Article.jsp#.WinafkqnE2w.
- 62.Nelson ME, Hamm MW, Hu FB, Abrams SA, Griffin TS. Alignment of Healthy Dietary Patterns and Environmental Sustainability: A Systematic Review. Adv Nutr. 2016;7(6):1005–25. doi: 10.3945/an.116.012567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tilman D, Clark M. Global diets link environmental sustainability and human health. Nature. 2014;515(7528):518–22. doi: 10.1038/nature13959. [DOI] [PubMed] [Google Scholar]
- 64.Eshel G, Shepon A, Makov T, Milo R. Land, irrigation water, greenhouse gas, and reactive nitrogen burdens of meat, eggs, and dairy production in the United States. Proc Natl Acad Sci U S A. 2014;111(33):11996–2001. doi: 10.1073/pnas.1402183111. [DOI] [PMC free article] [PubMed] [Google Scholar]