Abstract
BACKGROUND
Childhood obesity is increasing in prevalence in developing countries. We conducted this study to assess the prevalence of overweight and obesity in primary school children age 7 to 13 years in central Iraq and to identify possible risk factors.
METHODS
The study was conducted in Babil governorate from October through March 2002. Eight thousand three hundred pupils (4100 girls and 4200 boys) randomly chosen primary schools were included in the study. BMI was measured and compared to standard tables. Information on possible risk factors was collected by questionnaire.
RESULTS
The prevalence of overweight and obesity was 6% and 1.3%, respectively. Significant associations were found between overweight and age, residency (urban-rural), birth rank, breast-feeding and certain dietary and lifestyle practices.
CONCLUSION
The prevalence of obesity and overweight is relatively high in children in central Iraq. Modern dietary habits are an important influence in the development of childhood obesity that should be watched carefully and controlled.
Childhood obesity is a growing problem and an increasing public health concern in the developed countries.1 Even more worrying is the increasing prevalence of obesity in developing countries.2,3 Childhood obesity is a well-recognized problem all over the world. Obseity can cause other medical problems in childhood, adolescence and adulthood.4
The objectives of this study were to assess the prevalence and possible risk factors for childhood obesity in Babil governorate (ancient Babylon), which is adjacent to the capital Baghdad (about 100 kilometers to the south). This 1.2 million population city is similar to Baghdad in terrain and climate and is of relatively similar or somewhat lower socio-economic status. For these reasons (and also because it is convenient and presumably representative of the population of Iraq), we chose this area for the survey.
Methods
A sample of schools was chosen by simple random technique from each of the five districts of the governorate. The sample was proportionate to the number of schools in each district. The sample involved 20 primary schools, including 14 with two shifts each day (boys and girls separately), 3 primary schools for boys and 3 schools for girls. These schools are distributed in rural and urban areas in each administrative sector, including 10 in the rural area and 10 in the urban area. The classification of rural and urban areas was according to census bureau distributions. The total number of schools included 47 (10%) primary schools for boys, 46 (10%) primary schools for girls and 361 (80%) primary schools for boys and girls (mixed).
All the pupils in the chosen schools were examined for weight and height. The sample size was 8300 pupils, which represented 4.5% of the total number of children in the primary schools. The sample involved 4200 boys and 4100 girls, representing (4.1%) and (5.1%) of the total, respectively. The age of the pupils involved in the study was 7 years to 13 years of age.
The study was divided into two main parts: a cross-sectional portion to measure the prevalence of overweight/obesity in children and a case-control study to explore differences in possible risk factors between obese and non-obese children. The study sample included the total number of obese and overweight children (n=499) as cases with four controls (normal weight) for each case from the same class (to match for demographic and social factors). The non-response rate for the questionnaire was 3% for the cases and 20% for the controls, so that we included 484 cases and 1600 controls in our analysis.
Weight was measured with a well-calibrated digital scale. All boys and girls in the school wore uniforms and were barefooted. Weight was measured in kilograms with an accepted error of 0.1 kg. Height was measured in centimeters with a stadiometer with an accepted error of 0.1 cm. The body mass index (BMI) was estimated from the equation: BMI = WT (kg)/ HT (m2). The definition of obesity is relatively arbitrary and is usually based on an approximation of body fat—the body mass index (BMI, Quetelet’s index = weight in kg/height in m2).5 Overweight and obesity were determined by international cut off points (Table 1).6
Table 1.
Definitions of overweight and obesity according to body mass index.
| Age (years) | BMI (overweight) | BMI (obesity) | ||
|---|---|---|---|---|
| Male | Female | Male | Female | |
| 7 | 17.9 | 17.8 | 20.6 | 20.5 |
|
| ||||
| 8 | 18.4 | 18.3 | 21.6 | 21.6 |
|
| ||||
| 9 | 19.1 | 19.1 | 22.8 | 22.8 |
|
| ||||
| 10 | 19.8 | 19.9 | 24.0 | 24.1 |
|
| ||||
| 11 | 20.6 | 20.7 | 25.1 | 25.4 |
|
| ||||
| 12 | 21.2 | 21.7 | 26.0 | 26.7 |
Risk factors were assessed by means of a questionnaire that included specific questions (answered by a family member). Birth rank was explored to study the possible effects of order of birth, whether being first or last child in birth order has any relation to the BMI. Type of feeding during infancy was recorded, including breast-feeding or bottle-feeding. Mixed feeding was not included. Other questions assessed current dietary pattern (number of meals/ day), eating outside the house (school, restaurant), eating between meals, current pattern of physical activity (playing outside the house more than 2 hours /day), watching TV (more than 3 hours/day), working after school time, and the educational levels of the parents.
The standard chi square test was used to test for association for categorical variables. The chi-square Mantel-Haenszel summary test was used for stratification of risk factors to control for confounding.2 The main limitation of the study was that feeding practices and habits are personal and miscellaneous, making that issue difficult to assess precisely.
Results
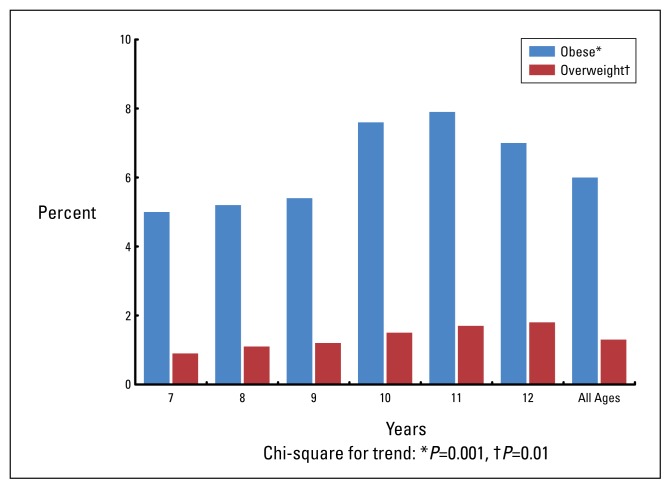
The prevalence of overweight in the study sample was 6% (499/8300) and the prevalence of obesity was 1.3% (111/8300) (obese included in the overweight group). Prevalence increased with age (Figure 1). The prevalence of overweight was greater in girls than in boys (6.1% vs. 5.8%), but the difference was not statistically significant.
Figure 1.
Prevalence of overweight and obese children by age.
The questionnaire was completed for 484 of 499 overweight pupils (97%), including 250 of 253 overweight girls (98.8%), 234 of 246 overweight boys (95.1%), and 1094 of 1600 normal weight pupils (68.3%). The urban-rural distribution of overweight children was 189 (4.4%) in rural areas and 310 (7.6%) in urban areas and the difference was highly significant (P<0.0001). There was no significant difference in the percentages of overweight boys and girls in either urban or rural areas.
In the analysis of possible risk factors, birth rank was a significant factor overall, with first-born children more frequently of normal weight than last-born children (odds ratio, 0.78, P=0.02) (Table 2). A history of breast-feeding during infancy was also significantly associated with normal weight (odds ratio, 0.73, P=0.03). The distribution of overweight and normal weight pupils according to educational level of their fathers as (primary or college) showed a significant difference, with more overweight children among those with fathers who had only a primary education (odds ratio, 1.58, P=0.001). Differences in playing outside and watching TV were not significant overall, but watching TV more than 3 hours was a highly significant factor for overweight in 7– to 9–year-old males (odds ratio, 2.98, P<0.001) and playing outside was a significant factor for normal weight in 10– to 12–year-old males (odds ratio, 0.47, P=0.004). Biking was not used as an indicator for physical activity for it is not a common exercise among children in our society.
Table 2.
Analysis of possible risk factors in overweight children.
| Possible risk factor | Chi-square | P value | Odds ratio (95% CI) | |
|---|---|---|---|---|
| First born (n=340) vs. last born (n=428) | ||||
| All | 5.03 | 0.02 | 0.78 (0.48–0.95) | |
| Female | 9.41 | 0.002 | 0.51 (0.33–7.9) | |
| Male | 0.01 | 0.92 | 1.05 (0.62–1.82) | |
| Breast fed (n=1076) vs. bottle fed (n=225) during infancy* | ||||
| All | 4.71 | 0.03 | 0.73 (0.52–0.97) | |
| Female | 10.77 | 0.001 | 0.47 (0.30–0.75) | |
| Male | 0.00 | 0.97 | 1.03 (0.65–1.63) | |
| Primary (n=288) vs college education (n=566) of fathers* | ||||
| All | 10.24 | 0.001 | 1.58 | |
| Female | 0.93 | 0.92 | 0.96 | |
| Male | 20.25 | <0.0001 | 2.36 | |
| Playing outside the house ≤2 h (n=1313) vs. >2 h (n=1032)* | ||||
| All | 0.40 | 0.52 | 0.96 (0.67–1.22) | |
| Female | 7–9 years | 2.66 | 0.10 | 2.13 (0.87–6.5) |
| 10–12 years | 0.90 | 0.34 | 1.53 (0.69–3.46) | |
| Male | 7–9 years | 0.02 | 0.87 | 0.93 (0.55–1.57) |
| 10–12 years | 8.25 | 0.004 | 0.47 (0.28–0.80) | |
| Time spent watching TV ≤3h (n=790) vs. >3h (n=556)* | ||||
| All | 3.12 | 0.07 | 1.28 (0.98–1.57) [†] | |
| Female | 7–9 years | 1.18 | 0.27 | 1.73 (0.80–2.34) |
| 10–12 years | 0.05 | 0.81 | 0.92 (0.57–1.49) | |
| Male | 7–9 years | 19.69 | <0.001 | 2.98 (1.79–4.97) |
| 10–12 years | 3.16 | 0.07 | 0.66 (0.41–1.04) | |
Mantel-Haenszel summary test
Excess calorie intake (represented by more than 3 meals/day) was not significant when compared with the control group (χ2=0.38, P=0.53). On the other hand, eating between meals was highly significant (χ2=8.66, P=0.003) and eating outside the house was also significant (χ2=4.36, P=0.03). The Mantel- Haenszel summary test for pooling showed significant differences, indicating the presence of a statistical association between these habits and high BMI (OR=1.21, 95% Cl=1.09–1.59, χ2=9.02, P=0.002).
The study showed that a significantly higher percent of working boys than girls (10.2% vs. 7.2%) (χ2=4.16, P=0.04). Comparing cases to controls regarding working after school showed a highly significant association with high values of BMI in working children than those not working (OR=1.81, 95% Cl=1.25–2.26, χ2=9.45, P=0.002).
Discussion
Childhood obesity is a serious public health problem with a rapidly increasing prevalence worldwide. The problem is surprisingly difficult to define.5 It is associated with several risk factors for later heart disease and other chronic diseases including hyperlipidaemia, hyperinsulinaemia, hypertension, and early atherosclerosis.7 The prevalence of overweight in our (presumably representative) sample of children was 6%, which is almost equal to the prevalence of obesity in the UK in 1984 (5.4%) and in Scotland (6.4%). The prevalence of obesity in the UK and Scotland in 1994 was (1.7%) and (2.1%) respectively. 8 By comparison, in our sample the prevalence of obesity was (1.3%), which is remarkably similar, taking into consideration the difference in developmental habits and prosperity between Iraq and these countries. Our study demonstrated that the prevalence of overweight and obesity significantly increased with age. The proportion of overweight and obesity increased from 5% and 0.9% at age 7 reaching 6.5 and 1.8%, respectively, at the age of 12 years. This may give the impression that obesity is a progressing phenomenon that once present, tends to increase with time. This is consistent with a study of children in primary schools in Leeds, which found a significant increase in the proportion of overweight and obese children at age 10. It is also in agreement with Sanjay et al, who found in 20 973 children aged 5–14 years that the prevalence of obesity increases with age, being almost double in the oldest age quarter, compared with youngest age quarter.10 In our study, although the prevalence of overweight was higher in girls than in boys, it was statistically not significant (6.1% vs. 5.8%). This finding does not coincide with Nicolas et al in their prospective study of African Americans, which concluded that female sex is an independent risk factor.11
The prevalence of overweight was significantly higher in urban areas than in rural areas (7.6% vs. 4.4%) in our study. This was in agreement with Zuguo et al12 in the USA, who observed an increase in the prevalence of overweight among both urban and rural children, although trends were more marked and consistent in the urban areas. Our results also agree with Fredrik et al,13 a study in the Netherlands, and with Behrman et al,14 which concluded that obesity is more prominent in urban than rural areas. This observation may be due to more food and less physical activity in urban areas. Studies relating infant feeding practices to childhood obesity unfortunately give inconclusive results. Some report a negative correlation between breastfeeding duration and late introduction of solid food with childhood obesity,15,16 while others found a positive correlation between breast-feeding and obesity17 or found no correlation between these two variables.18 Although little is known, some believe that there may be a connection between insufficient breast-feeding and a deficit of tryptophan associated with bottle-feeding. Tryptophan is necessary for the development of brain serotonin, a linkage that has been well documented by Professor Judith Wurtman at the MIT Clinical Research Centre.19
Although eating more than five meals per day was not significantly related to the BMI, the study demonstrated that the percentage of overweight children (eating more than five meals per day) was slightly more than those with normal weight (8.4% vs. 7.3%). Eating outside the house was significantly related to high BMI. The study showed that 73.5% of overweight children eat outside the house versus 68.3% of normal weight children. Underreporting also occurs among obese children and adults.20,21 The high BMI associated with these dietary habits in our sample does not agree with some studies, which concluded that obese children do not eat differently than their peers.9 Eating between meals was significantly related to high BMI. The study showed that 92.9% of overweight children eat between meals in comparison with 87.8% of normal weight children. The type of food was not recorded for it is difficult to assess.
The study showed a significant association between BMI and educational level of both mothers and fathers. Increased BMI in children seems to be associated with a low educational level of the parents. It seems that better educated people are more aware of this problem and more enthusiastic about protecting their children from the dangers of overweight and obesity. This assumption is in agreement with Fredrik et al,13 who found increased BMI values in children with less educated parents, but does not agree with a study done by Mihaela et al22 in the USA where mothers of obese children were not different from mothers of non-obese children in education.
Our study showed that 82.8% of overweight children play more than two hours outdoors versus 83.3% of normal weight children. BMI was not significantly associated with more time playing except in boys 10–12 years in whom more time of outdoors playing showed protective effect (OR=0.47). This may be due to the tribal custom that girls spend more time indoors and children less than 10 years were more (domestically) controlled by parents to avoid accidents. Watching TV more than 3 hours/ day was not associated with high BMI, which does not coincide with other studies23,24 where the BMI was significantly associated with more hours of TV viewing/day. This may be rationalized by the fact that in our culture the habit of eating while watching TV is not common.
We can conclude that the time has come for an effective and immediate effort to face this enemy; obesity is one of the frequently unrecognized deleterious effects of modern civilization in our society.
References
- 1.Nalina Robert M, Katzmarzyk Peter T. Validity of the body mass index as an indicator of the risk and presence of overweight in adolescents. Am J Clin Nutr. 1999;70:131S–136S. doi: 10.1093/ajcn/70.1.131s. [DOI] [PubMed] [Google Scholar]
- 2.Garrow JS. Obesity and related disease. London: Churchil Livingstone; 1988. p. 329. [Google Scholar]
- 3.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–1243. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ravussin Eric, Swindurn Boyd A. Pathophysiology of obesity. Lancet. 1992:340–404. doi: 10.1016/0140-6736(92)91480-v. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Report of a WHO consultation. Geneva: WHO; 1998. Obesity: preventing and managing the global epidemic. (WHO/ NUT/98.1.) [PubMed] [Google Scholar]
- 6.Kirkwood Bettyr. Essential of medical statistics. 1989;Chapter 14:94–105. [Google Scholar]
- 7.Berenson GS, Srinivasan SR, Bao W, Mewman WP. Obesity and Cardiovascular risk in children. Ann NY Acad Sci. 1993;699:93–103. doi: 10.1111/j.1749-6632.1993.tb18840.x. [DOI] [PubMed] [Google Scholar]
- 8.Chinn S, Rona RJ. Prevalence and trends in overweight and obesity in three cross sectional studies of British children, 1974–94. BMJ. 2001;322:24–26. doi: 10.1136/bmj.322.7277.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rudolf MGJ, Sahota P, Barth JH, Walker J. Incraesing prevalence of obesity in primary scool children: cohort study. BMJ. 2001;332:1094–1095. doi: 10.1136/bmj.322.7294.1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kinra Sanjay, Nelder Robert P, Lewendon Gill J. Deprevation and childhood obasity: a cross sectional study of 20973 children in plymouth, United Kingdom. J Epidemiol Community Health. 2000;54:456–460. doi: 10.1136/jech.54.6.456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stettler Nicolas, Tershakovec Andrew M, Zemel Babette S, et al. Early risk factors for increased adiposity: a cohort study of African American subjects followed from birth to young adulthood. Am J Clin Nur. 2000;72:378–83. doi: 10.1093/ajcn/72.2.378. [DOI] [PubMed] [Google Scholar]
- 12.Mei Zuguo, Scanlon Kelly S, Grummer-Strawn Laurence M, Freedman David S, Yip Ray, Trowbridge Frederick L. Increasing prevalence of overweight among US low-income preschool children: The center for disease control and prevention pediatric nutrition surviellance, 1983 to 1995. Pediatric. 1998;101:e 12. doi: 10.1542/peds.101.1.e12. [DOI] [PubMed] [Google Scholar]
- 13.Fredriks AM, van Buuren S, Burgmeijer RJF, et al. Continuing positive secular growth changes in the Netherlands 1955–1997. Pediatr Res. 2000 doi: 10.1203/00006450-200003000-00006. [In press] [DOI] [PubMed] [Google Scholar]
- 14.Behrman RE, Kliegman RM, Jenson HB. Obesity. Chap 16. W.B Saunders company; 2000. Nelson textbook of pediatrics; pp. 172–176. [Google Scholar]
- 15.Kumanyika S. Ethnicity and obesity development in children. Ann NY Acad Sci. 1993;29:81–92. doi: 10.1111/j.1749-6632.1993.tb18839.x. [DOI] [PubMed] [Google Scholar]
- 16.Von Kries R, Koletzko B, Sauerwald T, von Mutius E, Barnert D, Grunert V, von Voss H. Breast feeding and obesity: cross sectional study. Br Med J. 1999;319:147–150. doi: 10.1136/bmj.319.7203.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Agras WS, Kraemer HC, Berkowitz RI, Hammer LD. Influence of early feeding styles on adiposity at 6 years of age. J Pediatr. 1990;116:805–809. doi: 10.1016/s0022-3476(05)82677-0. [DOI] [PubMed] [Google Scholar]
- 18.Zive MM, McKay H, Frank-Spohrer GC, Broyles SL, Nelson JA, Nader PR. Infant-feeding practices and adiposity in 4 yr. old Anglo and Mexican- American. Am J Clin Nutr. 1992;55:1104–1108. doi: 10.1093/ajcn/55.6.1104. [DOI] [PubMed] [Google Scholar]
- 19.Wurtman, Suffes The serotonin solution, 1999. BMJ. 2002;321:1094–95. [Google Scholar]
- 20.Heitmann BL, Lissner L. Dietary under-reporting by obese individuals—Is it specific or nonspecific? BMJ. 1995;311:986–989. doi: 10.1136/bmj.311.7011.986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Johnson-Down L, O’Loughlin J, Koski KG, Gray-Donald K. High prevalence of obesity in low income and multiethnic school children: A diet and physical activity assessment. J Nut. 1997;127:2310–2315. doi: 10.1093/jn/127.12.2310. [DOI] [PubMed] [Google Scholar]
- 22.Tanasescu Mihaela, Ferris Ann M, Himmelgreen David A, Rodriguez Nancy, Perez-Escamilla Rafael. Biobehavioral factors are associated with obesity in Puerto Rican children. J of Nutr. 2000;130:1734–1742. doi: 10.1093/jn/130.7.1734. [DOI] [PubMed] [Google Scholar]
- 23.Andersen RE, crespo CJ, Bartlett SJ, et al. Relatioship of physical activity and television watching with body weight and level of fatness among children. Results from the third national health and nutrition examination survey. JAMA. 1998;25:938–942. doi: 10.1001/jama.279.12.938. [DOI] [PubMed] [Google Scholar]
- 24.Robinson TN. reducing children’s television viewing to prevent obesity: a randomized controlled trial. J Am Med Assoc. 1999;282:1561–1567. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]