Tuberculosis (TB), a common health problem in developing countries, is a specific multi-systemic infection that can lead protean manifestations in any organ system. Anemia and leukocytosis are the most frequent hematological findings at presentation and during the long clinical course of the disease. Coombs’-positive hemolytic anemia and immune thrombocytopenic purpura (ITP) are exceedingly rare and life-threatening complications of TB. We report two patients with Coombs’-positive hemolytic anemia and ITP that responded well to antituberculosis therapy.
Case 1
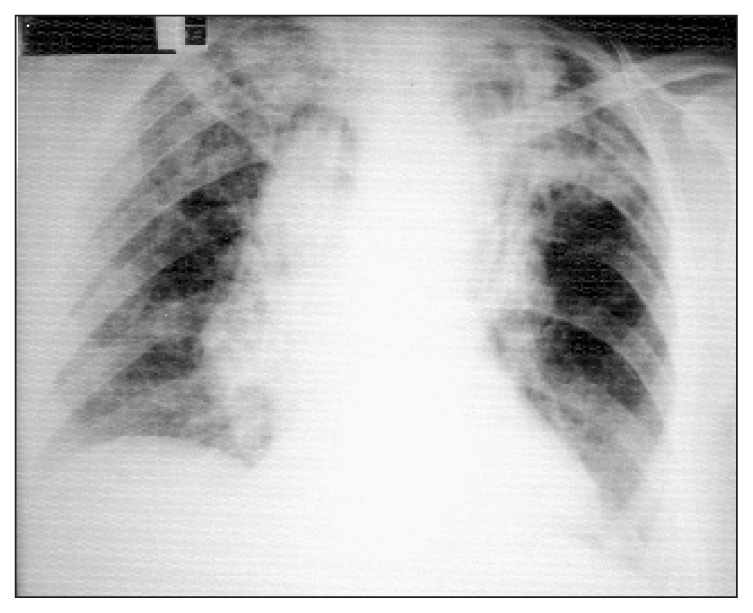
A 30-year-old previously healthy woman presented to the emergency department because of recent-onset jaundice and syncope. She had a one-month history of malaise, fatigue, non-productive cough and weight loss of 5 kg. Physical examination revealed a blood pressure of 80/55 mm Hg, pulse 112/min, respiration 30/min and body temperature 39.5°C orally. In the examination of the respiratory system, fine rales were heard in the left apical zone during inspiration and expiration together with a harsh bronchial noise. There was a systolic cardiac murmur of grade II heard all over the precordium. The laboratory findings on admission revealed a WBC of 6600/mm3, hemoglobin 4.6 g/dL, platelet count 175000/mm3 and reticulocytes 19.7%. Direct and indirect Coombs’ tests were positive without any transfusion. Erythrocyte morphology was polychromacytic together with macrocytosis, spherocytosis, anisopoikilocytosis and 6% normoblasts. Bone marrow examination disclosed significant erythroid hyperplasia and hypercellularity. No granuloma was observed in this biopsy. No drug history was obtained. Biochemical tests on admission were total bilirubin 6.0 g/dL, direct bilirubin 1.9 g/dL, AST 88 IU/L, ALT 37 IU/L, LDH 1902 U/L, ferritin 7685 ng/dL and haptoglobin 31 mg/dL. In the chest x-ray (Figure 1) there were bilateral apical reticulonodular infiltrations. Cavitary lesions were prominent in the posterior segments of the upper lobes in the high-resolution CT (Figure 2). Tests for ANA, anti-DNA, HIV and blood cultures were all negative. The bronchoalveolar lavage from the right upper lobe was positive for acid-fast bacilli, and M. tuberculosis was cultivated in Löwenstein-Jensen agar.
Figure 1.
Chest x-ray of case 1 at admission showing bilateral apical reticulonodular infiltration more prominent over the both apical lung fields.
Figure 2.
High resolution CT of case 1 showing bilateral upper lobe infiltration with multiple cavitary lesions over the posterior segments.
The drug regimen included isoniazid 300 mg/day, rifampicin 450 mg/day, pyrazinamide 1500 mg/day and streptomycin 750 mg/day, initiated on 8 April 2001. Fever subsided one week later. Since the liver enzymes were elevated on the tenth day of treatment (ALT 540 IU/L and AST 560 IU/L), all of the drugs except streptomycin were stopped and ethambutol 1500 mg/day was added to the treatment schema. When the enzymes (ALT and AST) were again 39 IU/L and 100 IU/L, respectively, isoniazid, pyrazinamide and rifampicin were added to the drug regimen with 5-day intervals. There were no increments in the enzymes following the re-initiation of treatment. After the first three months, streptomycin, pyrazinamide and ethambutol were stopped. Isoniazid and rifampicin were continued for nine months. We used no corticosteroids at any stage of the disease. Laboratory findings are shown in Table 1.
Table 1.
Consecutive laboratory findings of case 1.
| Parameters | On admission | 15 days after admission | 1 month later | 2 months later | 4 months later | 6 months later | 8 months later |
|---|---|---|---|---|---|---|---|
| Hemoglobin (g/dL) | 4.6 | 6.75 | 8 | 11.4 | 11.5 | 12.1 | 12.2 |
| Reticulocyte (%) | 19.7 | 17 | 1.05 | 0.98 | |||
| LDH (U/L) | 1902 | 1384 | 872 | 600 | 480 | 369 | 270 |
| Bilirubin (total/direct) (mg/dL) | 6.0/1.9 | 2.0/0.4 | 1.5/0.2 | 0.8/0.2 | 0.6/0.2 | 0.23/0.03 | 0.32/0.05 |
| AST (U/L) | 88 | 120 | 39 | 83 | 27 | 26 | 20 |
| ALT (U/L) | 37 | 368 | 100 | 90 | 15 | 20 | 18 |
| Haptoglobulin (mg/dL) (normal > 50) | 31 | 60 | 80 |
No blood or blood products were given to the patient and clinical symptoms gradually improved. The sputum examination made in June 2001 and at the end of treatment revealed no acid-fast bacilli and no M. tuberculosis in the control cultures. The control chest X-ray obtained at the end of treatment showed no abnormalities except the bilateral apical fibrotic opacities. She was free of disease and no recurrence was observed 14 months after completion of treatment.
Case 2
A 64-year-old previously healthy woman presented with a 4-day history of rash. She also complained of cough and a small amount of purulent sputum production for one month. No weight loss or other symptoms were reported. On physical examination, she had normal blood pressure and was afebrile with non-palpable purpuric lesions over the lower extremities and abdomen. The remainder of the physical examination was normal. The initial white and red blood cell count were normal and the platelet count was 6 × 109/L (normal range 125–400 × 109/L). LDH level was 700 U/L (normal rage <290 U/L). Total protein was 9.45 g/dL and globulin was 6 g/dL. The ESR was 70 mm/h and the coagulation profile was within normal limits. ANA, rheumatoid factor and HIV tests were all negative. A peripheral smear was remarkable for a paucity of platelets, and a bone marrow aspirate demonstrated increased cellularity and a number of megakaryocytes. No granulomas were detected. Detailed history disclosed no drug use before admission to our clinic. The chest x-ray demonstrated bilateral hilar and mediastinal widening with patchy opacities more pronounced over the left apical region (Figure 3). The patient received intravenous immunglobulins (400 mg/kg) for three days with a diagnosis of ITP. Although the platelet count showed a partial response to this treatment and increased to 79 × 109/L at the third day of treatment, it again fell to 20 × 109/L level one week later. Meanwhile, chest CT revealed multiple bilateral hilar, mediastinal adenopathy and a consolidation with “tree-in-bud” appearance over the posterior segment of the left upper lung (Figure 4 and 5). Bronchoscopy could not be instituted because of a low platelet level. Three sputum smears were found positive for acid-fast bacilli. Antituberculosis therapy consisting of isoniazid 300 mg/day, rifampicin 600 mg/day, ethambutol 2000 mg/day and pyrazinamide 2000 mg/day was started. The constitutional symptoms of the patient progressed day by day. The platelet count was increased to a normal level at the end of the first month of therapy. Ethambutol and pyrazinamide were stopped after two months and therapy was completed to one year with rifampicin and isoniazid. Mediastinal adenopathy (80% and cavitary lesions completely improved at the end of treatment (Figure 6 and 7). The patient was in good health and there was no recurrence after 12 months of treatment.
Figure 3.
Chest x- ray of case 2 at admission showing bilateral hilar and mediastinal widening and patchy opacities over both apical regions.
Figure 4.
Thorax CT of case 2 showing multiple paratracheal and subaortic adenopathy.
Figure 5.
High-resolution CT of case 2 showing bilateral apical consolidation with “tree-in-bud” appearance and a cavitary lesion over the posterior segment of left upper lobe.
Figure 6.
Control thorax CT of case 2 showing regressed paratracheal and subaortic adenopathy.
Figure 7.
Control high-resolution CT of case 2 showing complete resolution of lesions.
Discussion
A variety of hematological manifestations can be expected in TB due to its chronic inflammatory nature. Common manifestations are anemia and leukocytosis, which have been reported as having a frequency of 60% and 40%, respectively.1 Anemia of TB is usually due to nutritional deficiency, failure of iron utilization, malabsorption syndrome and bone marrow suppression. However, immune hemolytic anemia and ITP are exceedingly rare conditions in tuberculosis.
Infection-associated hemolytic anemia is mostly related to viral and mycoplasmal infection. Four hemolytic anemia cases due to TB were reported previously.2–5 As in our case, two of these cases responded successfully to antituberculosis therapy alone.3,5 In the third patient, prednisolone 60 mg for three weeks and splenectomy due to subcapsular hematoma preceded antituberculosis therapy.4 The fourth patient required prolonged steroid therapy to prevent the recurrence of hemolysis.2
Another complicated issue in the treatment of these patients is the hemolytic effects of antituberculosis drugs like rifampicin, streptomycin and para-aminosalicylic acid. We observed no hemolytic effects with rifampicin and streptomycin in our patients.
ITP usually occurs in two forms. The acute form is usually self-limited and is a post-viral disease of childhood. The adult form usually present in a more indolent way that may persist for many years and is referred as chronic ITP.6 The diagnosis of ITP is made by excluding other causes of thrombocytopenia. A secondary form of the disease occurs in association with systemic lupus erythematosus, the antiphospholipid syndrome, in immune deficiency states, in lymphoproliferative disorders, infections and certain drugs.7
An association between TB and ITP is exceedingly rare. To our knowledge, only 20 cases have been reported in the world literature.8–20 Pulmonary TB represents the most common clinical presentation, having occurred in 33% of cases, followed by disseminated TB and lymphadenitis. Platelet counts of these patients ranged from 1.0 to 46 × 109/L. All of the patients had a platelet count lower then 50 × 109 and 59% of cases had a platelet count under 10 × 109/L, as in our patient.
An immune basis for TB-induced ITP was supported by the presence either platelet antigen specific antibodies or platelet surface membrane IgG in two reports (12,14). The diagnosis of TB was not entertained initially in most of the ITP cases. The start of TB treatment changed from 1 week to 12 weeks when the poor response to steroid treatment was obvious and the manifestation of TB became more pronounced.
Disappearance of hematological abnormalities with antituberculosus therapy alone is important proof that TB is the underlying cause of a hematological abnormality. Recovery of hemoglobin, reticulocyte, haptoglobulin, and bilirubin levels and Cooombs’ negativity in a hemolytic anemia patient and a platelet level in an ITP patient after antituberculosis therapy are all strong evidence of an immune-mediated complication of TB.
In conclusion, severe hemolytic anemia and thrombocytopenia are life-threatening hematological complications of TB. As the incidence of TB is still high worldwide, TB should be recognized early in the course of the disease as a treatable and secondary cause of ITP and hemolytic anemia.
References
- 1.Glasser RM, Walker RI, Herion GE. The significance of hematologic abnormalities in patients with tuberculosis. Arch Intern Med. 1970;125(4):691–695. [PubMed] [Google Scholar]
- 2.Cameron SJ. Tuberculosis and the blood: a special relationship? Tubercle. 1974;55:55–72. doi: 10.1016/0041-3879(74)90067-1. [DOI] [PubMed] [Google Scholar]
- 3.Siribadana SH, Wijesundera A. Autoimmune hemolytic anemia responding to anti-tuberculous treatment. Trop Doct. 1997;27:243–244. doi: 10.1177/004947559702700424. [DOI] [PubMed] [Google Scholar]
- 4.Blanche P, Rigolet A, Massault PP, Bouscary D, Dreyfus F, Sicard D. Autoimmune haemolytic anaemia revealing miliary tuberculosis. J Infect. 2000;40(3):292. doi: 10.1053/jinf.1999.0530. [DOI] [PubMed] [Google Scholar]
- 5.Kuo PH, Yang PC, Kuo SS, Luh KT. Severe immune hemolytic anemia in disseminated tuberculosis with response to antituberculous therapy. Chest. 2001;119(6):1961–1963. doi: 10.1378/chest.119.6.1961. [DOI] [PubMed] [Google Scholar]
- 6.Cines DB, Blanchette VS. Immune thrombocytopenic purpura. New Engl J Med. 2002;346(13):995–1008. doi: 10.1056/NEJMra010501. [DOI] [PubMed] [Google Scholar]
- 7.Diz K, Hacıhanefioğlu A, Yenerel M, Turgut M, Keskin H, Nalcacı M, Inanc M. Antiphospholipid antibodies and antiphospholipid syndrome in patients presenting with immune thrombocytopenic purpura: a prospective cohort study. Blood. 2001;98(6):1760–1764. doi: 10.1182/blood.v98.6.1760. [DOI] [PubMed] [Google Scholar]
- 8.Perez de Liano LA, Soilan del Cerro JL, Garcia Pais MJ. Thrombocytopenic purpura as presenting form of miliary tuberculosis. Arch Bronho-Pneumol. 1998;34(8):411–412. [PubMed] [Google Scholar]
- 9.Talbot S, Dowling A, Dowling JP, Fuller A, Schwarz M. Mediastinal nodal tuberculosis presenting as immune thrombocytopenia. Aust NZ J Med. 1998;28(4):465–466. doi: 10.1111/j.1445-5994.1998.tb02084.x. [DOI] [PubMed] [Google Scholar]
- 10.Hernandez-Maraver D, Pelaez J, Pinilla J, Navarro FH. Immune thrombocytopenic purpura due to disseminated tuberculosis. Acta Haematol. 1996;96(4):266. doi: 10.1159/000203802. [DOI] [PubMed] [Google Scholar]
- 11.al- Majed SA, al-Momen AK, al-Kassimi FA, al-Zeer A, Kambal AM, Baagil H. Tuberculosis presenting as immune thrombocytopenic purpura. Acta Haematol. 1995;94(3):135–138. doi: 10.1159/000203995. [DOI] [PubMed] [Google Scholar]
- 12.Yasuda Y, Matsubara Y, Watanabe S, Hatakenaka R, Funarsu T. A case of intractable pulmonary tuberculosis complicated by idiopathic thrombocytopenic purpura. Nippon Kyobu Geka Gakki Zasshi. 1994;42(12):2301–2305. [PubMed] [Google Scholar]
- 13.Pavithran K, Vijayalekshmi N. Thrombocytopenic purpura with tuberculous adenitis. Indian J Med Sci. 1993;47(10):239–240. [PubMed] [Google Scholar]
- 14.Boots RJ, Roberts AW, McEvoy D. Immune thrombocytopenia complicating pulmonary tuberculosis. Case report and investigation of mechanism. Thorax. 1992;47(5):396–397. doi: 10.1136/thx.47.5.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singh SP, Misra GC, Prusty PK, Das RK. Tubercular lymphadenitis with purpura. J Indian Med Assoc. 1986;84(8):247–249. [PubMed] [Google Scholar]
- 16.Jurak SS, Aster R, Sawaf H. Immune thrombocytopenia associated with tuberculosis. Clin Pediatr. 1983;22(4):318–319. doi: 10.1177/000992288302200416. [DOI] [PubMed] [Google Scholar]
- 17.Chia YC, Machin SJ. Tuberculosis and severe thrombocytopenia. Br J Clin Pract. 1973;33(2):55–56. [PubMed] [Google Scholar]
- 18.Cockcroft DW, Donevan RE, Copland GM, Ibbott JW. Miliary tuberculosis presenting with hyponatremia and thrombocytopnia. Can Med Assoc J. 1976;115(9):871–873. [PMC free article] [PubMed] [Google Scholar]
- 19.Levy M, Cooper BA. Thrombocytopenic purpura associted with tuberculous lymphadenitis. Can Med Assoc J. 1964;90:373–374. [PMC free article] [PubMed] [Google Scholar]
- 20.Albornoz MA, Ghodrial MW. Immune thrombocytopenia: a rare presenting manifestation of tuberculosis. Am J Hem. 2001;67:139–143. doi: 10.1002/ajh.1093. [DOI] [PubMed] [Google Scholar]