Abstract
Aim
To identify the factors, risks, and mortality associated with unplanned out-of-hospital births.
Material and Methods
This observational, retrospective, case-control study was conducted between 2005 and 2013 through a review of medical records from the hospital network of a county of Brazil. Mother-child dyads were divided into in-hospital births and unplanned out-of-hospital births. For hypothesis testing involving quantitative variables, parametric and nonparametric methods (t-test or Mann–Whitney test, respectively) were used as appropriate after ascertaining normality of distribution via the Kolmogorov-Smirnov or Shapiro-Wilk tests. The chi-square test, Fisher’s exact test, odds ratios, and 95% confidence intervals were used to assess the relationship between categorical variables. A binary logistic regression was applied for pooled analysis of those variables that, when analyzed in isolation, had significant p-values on hypothesis testing. In all tests, p-values <0.05 were considered statistically significant.
Results
Of the 420 records, 117 corresponded to out-of-hospital births dyads. Mothers were predominantly nonwhite (p<0.001), with a history of inadequate antenatal care (p<0.001), multiparous (p<0.001), aged >25 years (p=0.031), and had more puerperal complications (p<0.001). Their newborns had low birth weight (Odds Ratios: 2.22; 95% CI: [1.4–3.4]; p<0.001), higher morbidity (p=0.009), a higher rate of admission to neonatal intensive care and stepdown units (p=0.030), and prolonged length of stay (p<0.001).
Conclusion
The risk of maternal and neonatal complications, as well as the neonatal mortality rate, were higher for unplanned out-of-hospital deliveries. It occurred predominantly in nonwhite, older, multiparous women who had received incomplete antenatal care and who lived far from perinatal care centers.
Keywords: Birth injuries, mortality, newborn, perinatal morbidity, out-of-hospital delivery
Introduction
Starting from the premise that delivery should take place in a well-prepared environment with qualified birth attendants, out-of-hospital (OOH) birth remains a universal event, although not all such deliveries are accidental. Despite the medical consensus that the best place for birth is a hospital (1), given the potential for maternal complications and need for neonatal resuscitation (2), many countries have decided to allow deliveries in OOH settings.
Out-of-hospital deliveries may be classified as planned or unplanned (accidental) (3). Several maternal and neonatal incidents have been reported in OOH births. These include hypothermia (in newborns abandoned after birth) (4), issues related to handling of the placenta and umbilical cord (5, 6), jaundice, tetanus, prematurity (4), asphyxia, higher rates of neonatal intensive care unit (NICU) admission (7), and higher odds of death (8, 9). A number of these problems could be avoided by proper handling at the time of delivery, based on principles of hygiene and basic care.
The literature has identified several socioeconomic factors associated with accidental or unplanned home birth, including single motherhood, maternal unemployment, low educational attainment, and multiparity (9). Neonatal characteristics include a higher prevalence of low birth weight and preterm birth (10).
In some reports from developed countries, the incidence of OOH ranges from 0.1 to 2% (11). According to the American College of Obstetrics and Gynecology (2015), in the United States, approximately 25,000 (0.6%) births per year occur at home, 25% of which are accidental (12, 13). Even in developed countries, under-registration of OOH is a well-known problem. In Brazil, despite some reports, published data on OOH are scarce. A study conducted in São Paulo reported a frequency of around 0.4%, which is comparable to rates recorded in urban Europe (14).
Despite advances in the Brazilian health care network in recent years, we believe clinical complication rates in mothers and their neonates remain higher when birth occurs outside an appropriate environment.
Within this context, the objectives of the present study were to identify the profile of mother-child dyads and their complications and verify whether associations existed between maternal and neonatal problems and delivery in inappropriate settings.
Material and Methods
Study design
This retrospective, observational case-control study was based on a review of medical records of newborns and their mothers, conducted from January 2005 through August 2013. Institutional review board approval was obtained at all participating hospitals for this retrospective study, and informed consent was waived. The project was approved by the Research Ethics Committee of Universidade Federal Fluminense (CAAE: 0082.0.258.258-11).
Study setting
We selected mother-child dyads admitted to three public facilities in the municipality of Niterói, state of Rio de Janeiro, Brazil: two high-complexity care units and one low-complexity facility. We also attempted to obtain information from private maternity hospitals in the municipality, but were unsuccessful, as some facilities had closed and others had moved. The hospitals are located in the Metropolitan 2 region of the state of Rio de Janeiro, Brazil, and serve a population of 2 million. Two of the study facilities are large hospitals (average 1,200–1,500 annual births) with maternal and neonatal intensive care units. The third facility is a low-complexity public maternity that handles approximately 800–1,200 births per year and is located geographically close to the other two units, which allows continuity of care for high-complexity patients. In Brazil, the vast majority of deliveries take place in a hospital setting, and there is no culture of planned OOH birth.
Sample size, target population, and group allocation
For this case-control study, mother-child dyads were divided into in-hospital births (IHB, control group) and unplanned out-of-hospital births (OOH, case group). The main study group was composed of mothers who gave birth OOH and were subsequently brought in by ambulance or self-presented to the study facilities. For its characterization, delivery room logs, medical records, and certificates of live birth were considered. For comparative analysis, we evaluated a randomly selected, threefold-sized sample of medical records of mothers and neonates born in the hospital setting (IHB). To ensure random selection, we used a randomized list and matched cases by date. Both in the case and control groups, the exclusion criteria were gestational age <22 weeks or birth weight <500 g, regardless of mode of delivery (vaginal or cesarian section). Patient files in both study groups (IHB and OOH) were requested from the Medical Records departments of each facility; subsequently, all data of interest were transcribed onto a specific form.
Only one of the authors was responsible for the systematic selection of records and data collection. A second researcher was responsible for auditing and checking the consistency of the data collected and the database. The categorical and continuous variables of the two groups were compared to prove the established hypothesis.
Categorical variables
Data were collected on maternal and neonatal parameters, birth conditions, and the setting in which delivery occurred. The main maternal variables were neighborhood and municipality of residence, skin color (classified as white or nonwhite), antenatal care (categorized as yes or no; complete [≥6 visits] or incomplete [<6 visits]), obstetric issues during the antenatal period (such as infection, bleeding, hypertension, or other), any antenatal treatment required (antibiotics, antihypertensives, or other), mode of delivery (vaginal or cesarian section), postpartum complications (bleeding, infection, hypertension, or other), and maternal treatment required in the postpartum period (e.g., antibiotics, antihypertensives, perineal surgery).
The neonatal variables of interest were birth weight (classified as low [<2500 g] or very low [<1500 g]), sex (female or male), weight-for-age status (small for gestational age, appropriate for gestational age, or large for gestational age), vitality at birth (yes or no), type of resuscitation required (tactile stimulation, bag-valve-mask + positive pressure ventilation, endotracheal intubation + positive pressure ventilation, other), crying at birth (yes or no, only for neonates in whom Apgar scores were not calculated), neonatal conditions (suspicion or evidence of infection, respiratory distress, jaundice, prematurity, or other), any neonatal treatment required (fluid resuscitation, antibiotics, phototherapy, infant formula, or other), setting of admission (rooming-in, stepdown unit, or NICU), and disposition (death, discharge, transfer, or discharge against medical advice).
The variables of interest regarding birth setting were place of birth (hospital, home, public thoroughfare, car/taxi/bus, ambulance, non-hospital health facility, or other), birth attendant (physician, the mother herself, relatives, neighbors/friends, Emergency Medical Service, Fire Rescue, or other), means of transport to hospital (self-transport, neighbors, or other), date and time of admission, and whether admission was diurnal (from 6:00 a.m. to 5:59 p.m.) or nocturnal (from 6:00 p.m. to 5:59 a.m.).
Quantitative variables
The quantitative variables of interest were maternal age (in years), parity (in absolute numbers), number of antenatal care visits (also as an absolute number), gestational age (as recorded in the certificates of live birth), birth weight (in grams), 5-minute Apgar score (0–10; IHB), and length of stay (in days).
Statistical Analysis
The data obtained were recorded in spreadsheets for subsequent analysis in IBM SPSS Statistics for Windows, version 22.0 (IBM Corp, Armonk, NY, USA) or R version 2.15.1 (The R Foundation for Statistical Computing).
Descriptive statistics [mean, median, range (min/max), and standard deviation (SD)] were used for analysis of continuous variables. For hypothesis testing involving quantitative variables, parametric and nonparametric methods (t-test or Mann–Whitney test, respectively) were used as appropriate after ascertaining normality of distribution via the Kolmogorov-Smirnov or Shapiro-Wilk tests. For all tests, a p-value <0.05 was considered significant.
The frequencies and cross-products of some categorical variables (health conditions during antenatal period, treatment required during antenatal period, maternal health conditions during puerperal period, maternal treatment during puerperal period, neonatal health conditions, and neonatal treatment) were analyzed by creating multiple-response sets. The percentage taken into consideration for between-group comparison (IHB vs. OOH) was that obtained from the total number of cases observed in each set. To test the relationship between these variables, the Chi-square method with Fisher’s exact test was used. Odds ratios (ORs) with 95% confidence intervals (CIs) were calculated using the Mantel–Haenszel procedure.
Binary logistic regression was used for pooled analysis of variables that, when analyzed in isolation with the dependent variable (birth setting, IHB vs. OOH), yielded a significant p-value (<0.05), except for those variables in which information bias was evident (health conditions during antenatal period, treatment required during antenatal period, mode of delivery, and neonatal resuscitation). Furthermore, to rule out multicollinearity between- predictor variables, we examined tolerance and the variance inflation factor, with reference values of >0.1 and <10, respectively. For regression, the dependent variable was the place of birth (IHB=0 vs. OOH=1). The IHB group was also analyzed separately without cesarean deliveries to eliminate the possibility of interference of this procedure on maternal and neonatal outcomes. The covariates considered for multiple regression analysis (binary independent variables) were maternal skin color, number of antenatal visits (≥6 or <6 visits), presence of maternal health conditions in the antenatal period (0, no; 1, yes), time of birth, weight <2500 g, infant sex, presence of maternal health conditions in the puerperal period (0, no; 1, yes), presence of neonatal health conditions (0, no; 1, yes) and neonatal treatment required (0, no; 1, yes). P-values were considered when <0.05, and ORs, when the 95% CI did not contain the number 1. A logistic function between birth setting (IHB=1; OOH=0) and the continuous variables was computed in R. A generalized linear model was used to estimate alpha (intercept) and beta and to plot the sigmoid curve.
Results
We analyzed a total of 420 records: 117 OOH and 303 IHB. Among the OOH group, there was an absolute predominance of women living in Niterói (n=76; 65.00%), most of whom lived in neighborhoods 30 km from the nearest maternity facility (n=12, 10.30%).
Most women were nonwhite (n=80; 68.40%) and had a striking lack of adequate antenatal care; only one-third of mothers (n=29; 24.80%) had attended six or more visits. The mean age was 25.43 years [range: 11–41; 95% CI: (24.19–26.67); SD: −6.73]. The mean number of pregnancies was 3.48 [95% CI: (3.10–3.86); SD: −2.03], the mean number of antenatal visits was 3.52 [95% CI: (2.77–4.26); SD: −3.50], and the mean gestational age was 38.08 weeks [95% CI: (37.48–38.69); SD: −3.27]. Of the women who had complications during the antenatal period (n=39; 33.30%), only 20 (17.10%) received any treatment. All deliveries were vaginal, and women were attended by relatives, friends or neighbors (n=34; 29.10%) or by their own mothers (n=32; 27.40%) in most cases. The home was the predominant place of birth (n=62; 53.00%), followed by a car/taxi/bus (n=23; 19.70%), and most occurred during the day (6:00 a.m. to 6:00 p.m.; n=62, 53.00%). The Emergency Medical System was the predominant means for transport of mother-infant dyads to maternity hospitals (n=36; 30.80%). The patient records revealed no maternal deaths.
The neonates had a mean birth weight of 2766.96 g [95% CI: (2652.10–2881.81); SD: −616.21]. On physical examination on arrival at the hospital, the vast majority of newborns were considered to have good vitality. Low-birth-weight (n=30; 25.6%) and very-low-birth- weight (n=5; 4.40%) deliveries were present in this group, and a minority required resuscitation (n=14; 12.00%). These were predominantly female (n=68; 58.10%). The rate of problems in the immediate puerperal period was high both in mothers (n=52; 44.40%) and in neonates (n=92; 78.60%). After delivery, neonates were most commonly discharged to rooming-in (n=89; 76.10%); a minority required admission to a stepdown unit (n=12; 10.30%) or NICU (n=10; 8.50%). Regarding disposition, most infants were discharged (n=101; 88.00%) after a mean length of stay of 5.75 days [95% CI: (3.95–7.55); SD: −9.56].
Analysis of continuous and categorical variables in the IHB and OOH groups clearly shows these differences (Tables 1, 2). When women who had a cesarean delivery (112/420) were withdrawn from the IHB group and the resulting data were compared with those for OOH births, analysis of quantitative variables showed that significance was maintained: age (p=0.06), number of pregnancies (p<0.001), number of antenatal visits (p<0.001), gestational age (p=0.011), weight (p<0.001), and hospital stay (p<0.001). The categorical variables also showed similar behavior, with nonsignificant differences in the following variables: antenatal problems (p=0.230), antenatal treatment (p=0.020), timing of birth (p=0.285), sex, and resuscitation (p=0.155 for each).
Table 1.
Description of continuous variables in the two study groupsa
| Continuous variable | Group | N | Mean | MIN | MAX | SD | p | 95% CI |
|---|---|---|---|---|---|---|---|---|
| Maternal age (years) | OOH | 116 | 25.43 | 11 | 41 | 6.736 | 0.031 | 24.19–26.67 |
| IHB | 299 | 23.91 | 13 | 43 | 6.111 | 23.22–24.61 | ||
| Total | 415 | |||||||
| Number of pregnancies | OOH | 113 | 3.48 | 1 | 13 | 2.031 | <0.001 | 3.10–3.86 |
| IHB | 301 | 2.25 | 1 | 12 | 1.648 | 2.06–2.44 | ||
| Total | 414 | |||||||
| Antenatal care visits | OOH | 87 | 3.52 | 0 | 12 | 3.507 | <0.001 | 2.77–4.26 |
| IHB | 242 | 7.1 | 0 | 17 | 3.159 | 6.70–7.50 | ||
| Total | 329 | |||||||
| Mean gestational age (weeks) | OOH | 116 | 38.088 | 22 | 42.1 | 3.275 | 0.02 | 37.48–38.69 |
| IHB | 302 | 38.787 | 24 | 42 | 2.394 | 38.51–39.05 | ||
| Total | 418 | |||||||
| Weight (g) | OOH | 113 | 2767 | 500 | 3970 | 616.21 | <0.001 | 2652.10–2881.81 |
| IHB | 301 | 3112 | 630 | 4700 | 613.2 | 3042.45–3181.56 | ||
| Total | 414 | |||||||
| Apgar (5-minute) | IHB | 290 | 9.05 | 2 | 10 | 1.021 | 8.93–9.17 | |
| Total | 309 | |||||||
| Length of stay (days) | OOH | 111 | 5.75 | 1 | 76 | 9.568 | <0.001 | 3.95–7.55 |
| IHB | 301 | 4.23 | 1 | 72 | 7.06 | 3.43–5.03 | ||
| Total | 412 |
CI; confidence interval;
IHB: in-hospital birth; MAX: maximum; MIN: minimum; N: frequency; aOOH: unplanned out-of-hospital birth; p: p-value (Mann–Whitney test); SD: standard deviation
Table 2.
Comparison of binary categorical variables
| Binary variables | OOH | IHB | p | OR | 95% CI | |
|---|---|---|---|---|---|---|
| Skin color | White | 15 (4.30%) | 90 (26.20%) | |||
| Nonwhite | 80 (23.30%) | 159 (46.20%) | <0.001 | 3.01 | 1.64–5.55 | |
| Antenatal care | Yes | 30 (8.60%) | 171 (49.10%) | |||
| No | 65 (18.70%) | 82 (23.60%) | <0.001 | 4.51 | 2.72–7.49 | |
| Problems during antenatal period | Yes | 43 (11.50%) | 136 (36.40%) | |||
| No | 39 (10.40%) | 156 (41.70%) | 0.382 | 0.79 | 0.48–1.29 | |
| Treatment during antenatal period | Yes | 20 (5.20%) | 114 (29.30%) | |||
| No | 74 (19.00%) | 181 (46.50%) | 0.002 | 2.33 | 1.34–4.02 | |
| Mode of delivery | Vaginal | 117 (27.90%) | 191 (45.40%) | |||
| Cesarean | 0 (0.00%) | 112 (26.70%) | <0.001 | 1.58 | 1.45–1.72 | |
| Timing of birth | Daytime | 62 (14.90%) | 192 (46.20%) | |||
| Nocturnal | 55 (13.20%) | 107 (25.70%) | 0.044 | 1.59 | 1.03–2.45 | |
| Weight <1500 g | Yes | 5 (1.20%) | 9 (2.20%) | |||
| No | 108 (26.00%) | 293 (70.60%) | 0.540 | 0.66 | 0.21–2.02 | |
| Weight <2500 g | Yes | 30 (7.20%) | 36 (8.70%) | |||
| No | 83 (20.00%) | 265 (64.10%) | <0.001 | 2.22 | 1.4–3.4 | |
| Sex | Female | 68 (16.80%) | 148 (36.70%) | |||
| Male | 43 (10.70%) | 144 (35.70%) | 0.056 | 1.53 | 0.98–2.40 | |
| Resuscitation | Yes | 14 (3.50%) | 78 (19.30%) | |||
| No | 89 (21.90%) | 224 (55.30%) | 0.011 | 2.21 | 1.19–4.11 | |
| Postpartum maternal problems | Yes | 52 (12.50%) | 46 (11.00%) | |||
| No | 63 (15.10%) | 256 (61.40%) | <0.001 | 2.96 | 2.12–4.14 | |
| Postpartum maternal treatment | Yes | 51 (12.10%) | 39 (9.30%) | |||
| No | 66 (15.70%) | 264 (62.90%) | <0.001 | 3.38 | 2.36–4.84 | |
| Neonatal problems | Yes | 92 (22.10%) | 155 (37.30%) | |||
| No | 22 (5.30%) | 147 (35.30%) | <0.001 | 1.57 | 1.36–1.81 | |
| Neonatal treatment | Yes | 49 (11.80%) | 81 (19.50%) | |||
| No | 64 (15.40%) | 221 (53.20%) | 0.001 | 1.61 | 1.22–2.14 | |
| Neonatal death | Yes | 5 (1.20%) | 2 (0.50%) | |||
| No | 110 (26.40%) | 299 (71.90%) | 0.009 | 6.54 | 1.28–33.2 |
CI: confidence interval;
IHB: in-hospital birth; aOOH: unplanned out-of-hospital birth; OR: odds ratio; p: p-value (Fisher’s exact test)
Multiple response testing revealed that that the main puerperal complications in the OOH group were perineal injury (n=47/55, 85.50%) and infection (n=4/55, 7.30%); the predominant treatments were corrective perineal surgery and antibiotic therapy, respectively. The most prevalent neonatal problems were suspected infection (n=74/187, 39.57%), confirmed infection (n=23/187, 12.29%), respiratory problems (n=15/187, 8.02%), jaundice (n=14/187, 7.28%), and prematurity (n=14/187, 7.28%). In the IHB group, the most prevalent problems were the same, but in a different order. In order of frequency, the most common problems were suspected infection, confirmed infection, jaundice, prematurity, and respiratory problems. Accordingly, therapeutic interventions also differed between the groups.
Regarding site of admission, there was also a significant difference between the groups (p=0.030): neonates in the OOH group were admitted to stepdown units and NICUs more often.
Regarding disposition after delivery, deaths, transfers, and discharges against medical advice were more frequent in the OOH group (p=0.020).
On multivariate analysis, computation of collinearity ruled out the hypothesis of a strong relationship between predictor variables, as the tolerance test and variance inflation factor yielded values >0.1 and <10, respectively.
Pooled analysis of dichotomous variables revealed that skin color, appropriate antenatal care, and neonatal problems in the puerperal period were significantly different (Table 3).
Table 3.
Binary logistic regression
| Variables in equation | B | S.E. | Wald | df | Sig. | Exp(B) | 95%CI for EXP(B) | ||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Lower | Upper | ||||||||
| Step1 | Skin color (1) | −1.378 | .447 | 9.506 | 1 | .002 | .252 | .105 | .605 |
| Antenatal care (1) | −1.179 | .376 | 9.847 | 1 | .002 | .308 | .147 | .642 | |
| Timing of admission (1) | −.545 | .369 | 2.187 | 1 | .139 | .580 | .281 | 1.194 | |
| Weight under 2.5 kg (1) | −.784 | .518 | 2.289 | 1 | .130 | .457 | .165 | 1.261 | |
| Sex (1) | .110 | .381 | .084 | 1 | .772 | 1.116 | .530 | 2.354 | |
| Postpartum complications (1) | −1.645 | .400 | 16.903 | 1 | .000 | .193 | .088 | .423 | |
| Neonatal conditions (1) | −1.187 | .427 | 7.718 | 1 | .005 | .305 | .132 | .705 | |
| Neonatal treatment (1) | −.184 | .437 | .177 | 1 | .674 | .832 | .353 | 1.960 | |
| Constant | 2.948 | .684 | 18.575 | 1 | .000 | 19.061 | |||
Variable(s) entered into step 1: Skin color (1); Neonatal conditions (1); Neonatal treatment (1); Antenatal care (1); Postpartum complications (1); Sex (1); Timing of admission (1); Weight under 2.5 kg (1)
Multivariate analysis also revealed clear, significant differences between the two groups, particularly regarding parity and birth weight (Figure 1).
Figure 1.
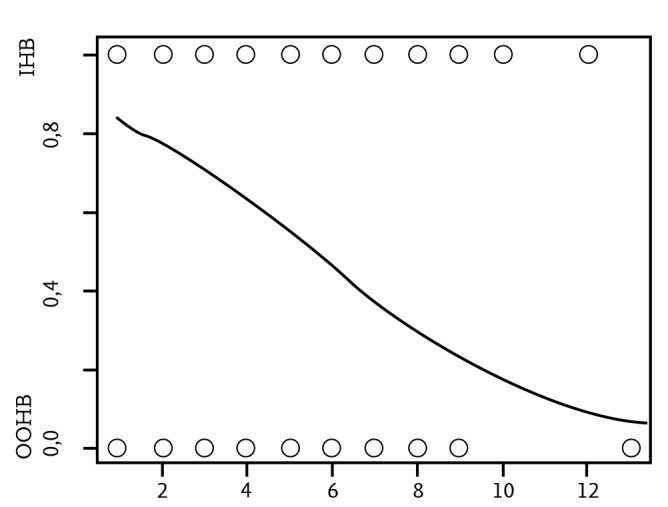
Multivariate analysis: parity
Discussion
The risk of maternal and neonatal complications, as well as the rate of infant mortality, were higher for unplanned out-of-hospital deliveries. This group exhibited a clearly-characterized, well-defined profile: multiparous, nonwhite women aged over 25 years who lived far from perinatal care centers and had received incomplete or no antenatal care. Mothers in this group had higher rates of perineal injury and treatment in the puerperal period, and their newborns had higher rates of complications in the neonatal period, such as low birth weight, infection, respiratory disorders, and jaundice.
Maternal problems occur when OOH is unplanned. A study conducted in Nigeria (15) showed that the most common reason was short duration of labor, that the preferred place of birth was the bedroom, and that 25.4% of deliveries were conducted by untrained persons. However, the social, political, and economic situation in Niterói is different because the city has a high Human Development Index as compared with other municipalities. In our sample, most OOH occurred at the mother’s home, with a smaller share occurring en route to the hospital, and most deliveries were attended by persons lacking the cognitive and motor skills required of birth attendants (relatives, neighbors or friends).
Mothers who delivered OOH were three times more likely to be nonwhite than mothers who delivered in-hospital, which is indicative of a striking – and historically well-known – social-racial difference in access to health care services (16). The relationship between lack of antenatal care and OOH is also well described. Mothers who had not received appropriate antenatal care were four times more likely to deliver OOH. There is consistent evidence that routine antenatal care prevents maternal and perinatal morbidity and mortality because it allows timely detection and treatment of diseases and reduces risk factors for complications to mother and child health (17).
As described elsewhere, the occurrence of unplanned or accidental delivery is associated with factors such as limited financial resources, living in remote areas, and limited years of schooling (9). One of the limitations of data assessment in the present study concerned maternal educational level and employment because these data were missing from medical records. The present study was conducted at three public health care facilities, which serve a more deprived population. Between 2013 and 2015, an Universidade Federal Fluminense undergraduate research project conducted with 227 postpartum women treated at the same perinatal care facilities revealed a predominance of low educational attainment, defined as <8 years of schooling; 73 of the 227 (32.2%) had not completed primary education, and 72 (31.7%) had completed secondary school (unpublished data - research project: IC144963). In the aforementioned Nigerian study, only 3.5% of mothers (n=14/400) received higher education (15). Educational attainment influences individual perceptions about the importance assigned to maternal and child health. Another limitation for the between-group comparison was the presence of complications during the antenatal period. The majority of pregnant women in the OOH group did not receive antenatal care, which made it difficult to interpret the difference found in absolute values of this variable, even after justifying for the greater frequency of therapeutic interventions in the IHB group during the antenatal period.
Women in the OOH group were three times more likely to have complications in the puerperal period, with perineal injury being the most common. A systematic review (18) showed that bleeding was the leading complication of accidental birth. Our review of records revealed no women with anemia or other related obstetric complications. The size of full-term neonates and inadequate posture during delivery may have influenced the rates observed. Perineal trauma at birth has been reported at undesirably high rates and is known to be associated with nulliparity, abnormal presentation, and perineal instrumentation during delivery (19).
It has long been known that neonates born OOH have a higher prevalence of complications. Several reports endorse higher rates of mortality(20–22), asphyxia (although under-registration of Apgar scores may lead to bias in such estimation) (23), NICU admission (9), prematurity (24), and hypothermia (24). Other complications have been described, and the present study confirms some data from the literature. In our sample, neonates were full-term and had higher odds of low birth weight. There was no difference in the rate of very low birth weight between the two groups. No cases of asphyxia were evident, nor was there a higher rate of preterm birth. However, neonates in the OOH group had more clinical complications, were more likely to require treatment and be admitted to NICU or stepdown units, and had a prolonged length of stay. This was clearly associated with increased expenditure to address the adverse events triggered by unplanned birth.
Upon analysis of the scenario described in this study, it is easy to speculate that Emergency Medical System and other prehospital responders should be methodologically prepared and trained to provide all necessary maternal and neonatal care procedures (25). Emphasis should be placed on continuous assessment of knowledge and training about these procedures, and further studies should focus on elucidating the optimal frequency and intensity of such training and its follow-up.
Perinatal outcomes are the result of a complex network of factors that include biologic, socioeconomic, and health care-related determinants (17). Joint action with particular emphasis on expanding supply and access to health care services and enhancing maternal education is essential for reducing social inequities and preventing complications in mothers and infants alike. By corroborating that birth in inappropriate settings is associated with maternal and neonatal complications, the present study creates the expectation that the public health system might be able to intervene in pregnancies with a profile of heightened risk for this event. Detection of such a profile should be regarded by health care providers responsible for antenatal care as a red flag of increased risk for unplanned hospital birth. This, in turn, should prompt a distinct approach to care, including providing information to the expectant patient about this possibility, and educating the patient on proper behavior and attitudes toward the healthcare network.
In conclusion, the risk of maternal and neonatal complications, as well as the neonatal mortality rate, were higher for accidental or otherwise unplanned deliveries that occurred in improper environments. Out-of-hospital deliveries occurred predominantly in nonwhite, older, multiparous women who had received incomplete or no antenatal care and who lived far from perinatal care centers.
What is already known on this topic
The prevalence of unplanned out-of-hospital birth is highly variable across different regions worldwide.
Delivery in unprepared settings can cause risk to the mother and to the fetus.
The frequency of low birth weight and prematurityand its consequences are not convergent.
What this study adds
Deliveries in the OOH group were unplanned and occurred in improper environments. This group was clearly characterized by incomplete or absent antenatal care, multiparity, nonwhite skin color, age>25 years, and living in areas remote from perinatal care centers.
There was a clear predominance of low-birth-weight and full-term deliveries, as well as a greater need for neonatal admission and treatment in the NICU setting, which led to longer hospital stay.
Living in neighborhoods far from maternity hospitals and perinatal care centers was closely associated with OOH delivery.
Regarding the sequence of care upon hospital arrival, this study showed a clear need for standardization of management of mother-child dyads presenting after OOH delivery.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Universidade Federal Fluminense (CAAE: 0082.0.258.258-11).
Informed Consent: Informed consent was not obtained from patients due to the retrospective nature of the study.
Peer-review: Externally peer-reviewed
Author Contributions: Concept - I.F.J., G.L.; Design - I.F.J., A.C., G.L.; Supervision - G.L., A.C., I.F.J.; - Funding D.L., A.C.;Data Collection and/or Processing - D.L., A.C.; Analysis and/or Interpretation - I.F.J., D.L., G.L. Literature Review - D.L.,G.L.; Writing - D.L., I.F.J., A.C., G.L.; Critical Review - I.F.J., D.L.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Wyckoff MH, Aziz K, Escobedo MB, et al. Part 13: Neonatal resuscitation: 2015 American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S543–60. doi: 10.1161/CIR.0000000000000267. [DOI] [PubMed] [Google Scholar]
- 2.Wasden SW, Chasen ST, Perlman JM, et al. Planned home birth and the association with neonatal hypoxic ischemic encephalopathy. J Perinat Med. 2017;45:1055–60. doi: 10.1515/jpm-2016-0292. [DOI] [PubMed] [Google Scholar]
- 3.Ovaskainen K, Ojala R, Gissler M, Luukkaala T, Tammela O. Out-of-hospital deliveries have risen involving greater neonatal morbidity: Risk factors in out-of-hospital deliveries in one University Hospital region in Finland. Acta Paediatr. 2015;104:1248–52. doi: 10.1111/apa.13117. [DOI] [PubMed] [Google Scholar]
- 4.Orimadegun AE, Akinbami FO, Tongo OO, Okereke JO. Comparison of neonates born outside and inside hospitals in a children emergency unit, southwest of Nigeria. Pediatr Emerg Care. 2008;24:354–8. doi: 10.1097/PEC.0b013e318177a73c. [DOI] [PubMed] [Google Scholar]
- 5.McDonald SJ, Middleton P. Effect of timing of umbilical cord clamping of term infants on maternal and neonatal outcomes. Cochrane Database Syst Rev. 2008;2:CD004074. doi: 10.1002/14651858.CD004074.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Neilson JP. Cochrane Update: Effect of timing of umbilical cord clamping at birth of term infants on mother and baby outcomes. Obstet Gynecol. 2008;112:177–8. doi: 10.1097/AOG.0b013e31817f2169. [DOI] [PubMed] [Google Scholar]
- 7.Gunnarsson B, Smarason AK, Skogvoll E, Fasting S. Characteristics and outcome of unplanned out-of-institution births in Norway from 1999 to 2013: a cross-sectional study. Acta Obstet Gynecol Scand. 2014;93:1003–10. doi: 10.1111/aogs.12450. [DOI] [PubMed] [Google Scholar]
- 8.McLelland G, McKenna L, Archer F. No fixed place of birth: unplanned BBAs in Victoria, Australia. Midwifery. 2013;29:e19–25. doi: 10.1016/j.midw.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 9.Renesme L, Garlantezec R, Anouilh F, Bertschy F, Carpentier M, Sizun J. Accidental out-of-hospital deliveries: a case-control study. Acta Paediatr. 2013;102:e174–77. doi: 10.1111/apa.12156. [DOI] [PubMed] [Google Scholar]
- 10.Boland RA, Davis PG, Dawson JA, Stewart MJ, Smith J, Doyle LW. Very preterm birth before arrival at hospital. Aust N Z J Obstet Gynaecol. 2017 doi: 10.1111/ajo.12690. [DOI] [PubMed] [Google Scholar]
- 11.Sheiner E, Ohel I, Hadar A. Out-of-hospital deliveries. In: Sir Arulkumaran S, Karoshi M, Keith LG, Lalonde AB, B-Lynch C, editors. A Comprehensive textbook of postpartum hemorrhage: an essential clinical reference for effective management. 2 ed. London, UK: The global library of women’s medicine by sapiens publishing; 2012. pp. 571–6. [Google Scholar]
- 12.Chervenak FA, McCullough LB, Arabin B. Obstetric ethics: an essential dimension of planned home birth. Obstet Gynecol. 2011;117:1183–7. doi: 10.1097/AOG.0b013e3182172a97. [DOI] [PubMed] [Google Scholar]
- 13.Grunebaum A, McCullough LB, Brent RL, Arabin B, Levene MI, Chervenak FA. Perinatal risks of planned home births in the United States. Am J Obstet Gynecol. 2015;212:350 e1–6. doi: 10.1016/j.ajog.2014.10.021. [DOI] [PubMed] [Google Scholar]
- 14.Almeida MF, Alencar GP, Novaes MH, et al. Accidental home deliveries in southern Sao Paulo, Brazil. Rev Saude Publica. 2005;39:366–75. doi: 10.1590/S0034-89102005000300006. [DOI] [PubMed] [Google Scholar]
- 15.Bukar M, Jauro YS. Home births and postnatal practices in Madagali, north-eastern Nigeria. Niger J Clin Pract. 2013;16:232–7. doi: 10.4103/1119-3077.110151. [DOI] [PubMed] [Google Scholar]
- 16.Yudell M, Roberts D, DeSalle R, Tishkoff S. Taking race out of human genetics. Science. 2016;351:564–5. doi: 10.1126/science.aac4951. [DOI] [PubMed] [Google Scholar]
- 17.Victora CG, Aquino EM, do Carmo Leal M, Monteiro CA, Barros FC, Szwarcwald CL. Maternal and child health in Brazil: progress and challenges. Lancet. 2011;377:1863–76. doi: 10.1016/S0140-6736(11)60138-4. [DOI] [PubMed] [Google Scholar]
- 18.McLelland GE, Morgans AE, McKenna LG. Involvement of emergency medical services at unplanned births before arrival to hospital: a structured review. Emerg Med J. 2014;31:345–50. doi: 10.1136/emermed-2012-202309. [DOI] [PubMed] [Google Scholar]
- 19.Ojule JD, Oriji VK, Georgewill KN. Perineal trauma in Port Harcourt, Souh-south Nigeria. Niger J Med. 2012;21:36–40. [PubMed] [Google Scholar]
- 20.Silva ZP, Almeida MF, Alencar GP. Accidental non-hospital birth as an indicator of risk of infant mortality. Rev Bras Saúde Matern Infant. 2014;14:155–63. doi: 10.1590/S1519-38292014000200005. [DOI] [Google Scholar]
- 21.Pilkington H, Blondel B, Drewniak N, Zeitlin J. Where does distance matter? Distance to the closest maternity unit and risk of foetal and neonatal mortality in France. Eur J Public Health. 2014;24:905–10. doi: 10.1093/eurpub/ckt207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grunebaum A, McCullough LB, Sapra KJ, et al. Early and total neonatal mortality in relation to birth setting in the United States, 2006–2009. Am J Obstet Gynecol. 2014;211:390 e1–7. doi: 10.1016/j.ajog.2014.03.047. [DOI] [PubMed] [Google Scholar]
- 23.Grunebaum A, McCullough LB, Brent RL, Arabin B, Levene MI, Chervenak FA. Justified skepticism about Apgar scoring in out-of-hospital birth settings. J Perinat Med. 2015;43:455–60. doi: 10.1515/jpm-2014-0003. [DOI] [PubMed] [Google Scholar]
- 24.Jones P, Alberti C, Jule L, et al. Mortality in out-of-hospital premature births. Acta Paediatr. 2011;100:181–7. doi: 10.1111/j.1651-2227.2010.02003.x. [DOI] [PubMed] [Google Scholar]
- 25.Nelissen E, Ersdal H, Mduma E, et al. Helping Mothers Survive Bleeding After Birth: retention of knowledge, skills, and confidence nine months after obstetric simulation-based training. BMC Pregnancy Childbirth. 2015;15:190. doi: 10.1186/s12884-015-0612-2. [DOI] [PMC free article] [PubMed] [Google Scholar]


